Weight Categories among Male Adolescents Linked to Risky Behaviors: High or Low BMI, Which Is Worse?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
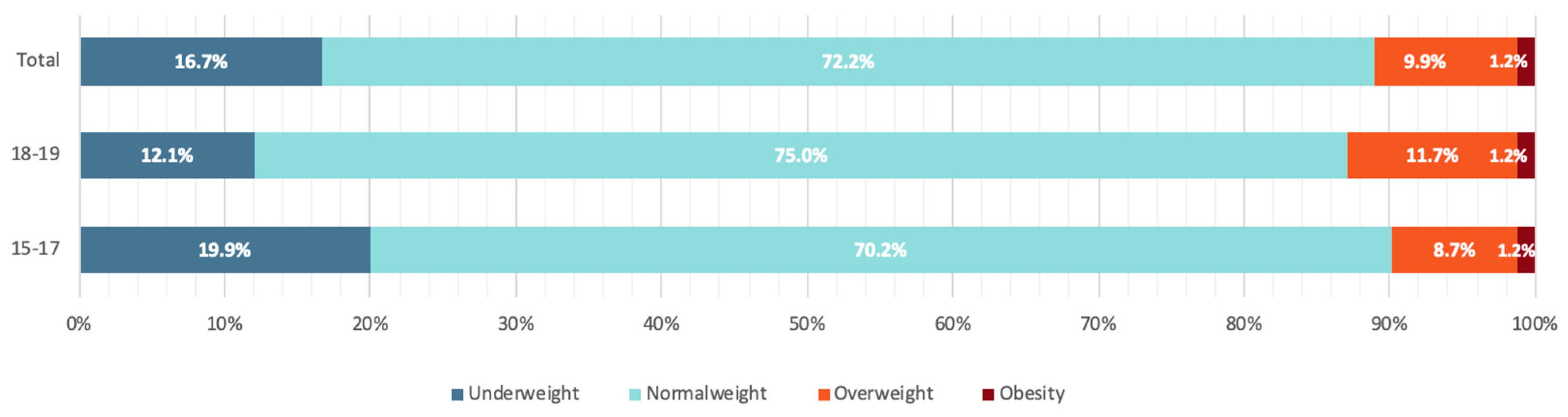
2.2. Participants
2.3. Measures
2.3.1. Dependent Variable
2.3.2. Independent Variables
2.4. Statistical Analysis
3. Results
Multinomial Logistic Regression Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. Clin. Ter. 2019, 170, e223–e230. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and Adolescent Obesity in the United States: A Public Health Concern. Glob. Pediatri. Health 2019, 6, 2333794X19891305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef] [Green Version]
- Luder, E.; Alton, I. The underweight adolescent. In Guidelines for Adolescent Nutrition Services; Stang, J., Story, M., Eds.; Center for Leadership, Education and Training in Maternal and Child Nutrition, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota: Minneapolis, MN, USA, 2005; pp. 93–100. [Google Scholar]
- Keys, A.; Fidanza, F.; Karvonen, M.J.; Kimura, N.; Taylor, H.L. Indices of relative weight and obesity. J. Chronic. Dis. 1972, 25, 329–343. [Google Scholar] [CrossRef]
- McMurray, R.G.; Harrell, J.S.; Deng, S.; Bradley, C.B.; Cox, L.M.; Bangdiwala, S.I. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes. Res. 2000, 8, 130–139. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Lim, H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int. Rev. Psychiatry 2012, 24, 176–188. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zhang, Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am. Clin. Nutr. 2006, 84, 707–716. [Google Scholar] [CrossRef] [Green Version]
- Haines, J.; Rifas-Shiman, S.L.; Horton, N.J.; Kleinman, K.; Bauer, K.W.; Davison, K.K.; Walton, K.; Austin, S.B.; Field, A.E.; Gillman, M.W. Family functioning and quality of parent-adolescent relationship: Cross-sectional associations with adolescent weight-related behaviors and weight status. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 68. [Google Scholar] [CrossRef] [Green Version]
- Vollmer, R.L.; Mobley, A.R. Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight. A review. Appetite 2013, 71, 232–241. [Google Scholar] [CrossRef]
- Zeller, M.H.; Reiter-Purtill, J.; Modi, A.C.; Gutzwiller, J.; Vannatta, K.; Davies, W.H. Controlled study of critical parent and family factors in the obesigenic environment. Obesity 2007, 15, 126-126. [Google Scholar] [CrossRef] [Green Version]
- Crossman, A.; Sullivan, D.A.; Benin, M. The family environment and American adolescents’ risk of obesity as young adults. Soc. Sci. Med. 2006, 63, 2255–2267. [Google Scholar] [CrossRef]
- Mirza, N.M.; Yanovski, J.A. Body dissatisfaction, self-esteem, and overweight among inner-city Hispanic children and adolescents. J. Adoles. Health 2005, 36, 267.e16. [Google Scholar] [CrossRef] [Green Version]
- Jebeile, H.; Lister, N.B.; Baur, L.A.; Garnett, S.P.; Paxton, S.J. Eating disorder risk in adolescents with obesity. Obes. Rev. 2021, 22, e13173. [Google Scholar] [CrossRef]
- Da Luz, F.Q.; Hay, P.; Touyz, S.; Sainsbury, A. Obesity with comorbid eating disorders: Associated health risks and treatment approaches. Nutrients 2018, 10, 829. [Google Scholar] [CrossRef] [Green Version]
- Agüera, Z.; Lozano-Madrid, M.; Mallorquí-Bagué, N.; Jiménez-Murcia, S.; Menchón, J.M.; Fernández-Aranda, F. A review of binge eating disorder and obesity. Neuropsychiatrie 2021, 35, 57–67. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Miranda-Olivos, R.; Agüera, Z.; Granero, R.; Vergeer, R.R.; Dieguez, C.; Jiménez-Murcia, S.; Gearhardt, A.N.; Fernández-Aranda, F. Food addiction and lifetime alcohol and illicit drugs use in specific eating disorders. J. Behav. Addict. 2022, in press. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Steiger, H.; Isräel, M.; Granero, R.; Prat, R.; Santamaría, J.J.; Fernández-Aranda, F. Pathological gambling in eating disorders: Prevalence and clinical implications. Compr. Psychiatry 2013, 54, 1053–1060. [Google Scholar] [CrossRef]
- Schreiber, L.R.; Odlaug, B.L.; Grant, J.E. The overlap between binge eating disorder and substance use disorders: Diagnosis and neurobiology. J. Behav. Addict. 2013, 2, 191–198. [Google Scholar] [CrossRef] [Green Version]
- Fouladi, F.; Mitchell, J.E.; Crosby, R.D.; Engel, S.G.; Crow, S.; Hill, L.; Steffen, K.J. Prevalence of alcohol and other substance use in patients with eating disorders. Eur. Eat. Disord. Rev. 2015, 23, 531–536. [Google Scholar] [CrossRef]
- Yohn, S.E.; Galbraith, J.; Calipari, E.S.; Conn, P.J. Shared Behavioral and Neurocircuitry Disruptions in Drug Addiction, Obesity, and Binge Eating Disorder: Focus on Group I mGluRs in the Mesolimbic Dopamine Pathway. ACS Chem. Neurosci. 2019, 10, 2125–2143. [Google Scholar] [CrossRef]
- Slane, J.D.; Burt, S.A.; Klump, K.L. Bulimic behaviors and alcohol use: Shared genetic influences. Behav. Genet. 2012, 42, 603–613. [Google Scholar] [CrossRef] [PubMed]
- Eskander, N.; Chakrapani, S.; Ghani, M.R. The risk of substance use among adolescents and adults with eating disorders. Cureus 2020, 12, e10309. [Google Scholar] [CrossRef] [PubMed]
- Barry, D.; Petry, N.M. Associations between body mass index and substance use disorders differ by gender: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addict. Behav. 2009, 34, 51–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, T.L.; Yen, J.Y.; Ko, C.H.; Huang, M.F.; Wang, P.W.; Yeh, Y.C.; Yen, C.F. Associations between substance use and body mass index: Moderating effects of sociodemographic characteristics among Taiwanese adolescents. Kaohsiung J. Med. Sci. 2010, 26, 281–289. [Google Scholar] [CrossRef] [Green Version]
- Audrain-McGovern, J.; Benowitz, N.L. Cigarette smoking, nicotine, and body weight. Clin. Pharmacol. Ther. 2011, 90, 164–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorgeirsson, T.E.; Gudbjartsson, D.F.; Sulem, P.; Besenbacher, S.; Styrkarsdottir, U.; Thorleifsson, G.; Walters, G.B.; TAG Consortium; Oxford-GSK Consortium; ENGAGE consortium; et al. A common biological basis of obesity and nicotine addiction. Transl. Psychiatry 2013, 3, e308. [Google Scholar] [CrossRef]
- National Research Council and Institute of Medicine. Preventing Mental, Emotional, and Behavioral Disorders among Young People. In Progress and Possibilities; The National Academies Press: Washington, DC, USA, 2009. [Google Scholar] [CrossRef]
- Blüml, V.; Kapusta, N.; Vyssoki, B.; Kogoj, D.; Walter, H.; Lesch, O.M. Relationship between substance use and body mass index in young males. Am. J. Addict. 2012, 21, 72–77. [Google Scholar] [CrossRef]
- Verdejo-Garcia, A.; Crossin, R. Nutritional and metabolic alterations arising from stimulant use: A targeted review of an emerging field. Neurosci. Biobehav. Rev. 2021, 120, 303–306. [Google Scholar] [CrossRef]
- Kantanista, A.; Osinski, W. Underweight in 14 to 16 year-old girls and boys: Prevalence and associations with physical activity and sedentary activities. Ann. Agric. Environ. Med. 2014, 21, 114–119. [Google Scholar]
- Pengpid, S.; Peltzer, K. Diabetes & Metabolic Syndrome: Clinical Research & Reviews Underweight and overweight or obesity and associated factors among school-going adolescents in five ASEAN countries. Diabetes. Metab. Syndr. Clin. Res. Rev. 2019, 13, 3075–3080. [Google Scholar] [CrossRef]
- Black, D.W.; Shaw, M.; McCormick, B.; Allen, J. Pathological gambling: Relationship to obesity, self-reported chronic medical conditions, poor lifestyle choices, and impaired quality of life. Compr. Psychiatry 2013, 54, 97–104. [Google Scholar] [CrossRef] [Green Version]
- Grant, J.E.; Derbyshire, K.; Leppink, E.; Chamberlain, S.R. Obesity and gambling: Neurocognitive and clinical associations. Acta Psychiatr. Scand. 2015, 131, 379–386. [Google Scholar] [CrossRef] [Green Version]
- Yip, S.W.; Desai, R.A.; Steinberg, M.A.; Rugle, L.; Cavallo, D.A.; Krishnan-Sarin, S.; Potenza, M.N. Health/functioning characteristics, gambling behaviors, and gambling-related motivations in adolescents stratified by gambling problem severity: Findings from a high school survey. Am. J. Addict. 2011, 20, 495–508. [Google Scholar] [CrossRef] [Green Version]
- Algren, M.H.; Ekholm, O.; Davidsen, M.; Larsen, C.V.; Juel, K. Health behaviour and body mass index among problem gamblers: Results from a nationwide survey. J. Gambl. Stud. 2015, 31, 547–556. [Google Scholar] [CrossRef]
- Ballard, M.; Gray, M.; Reilly, J.; Noggle, M. Correlates of video game screen time among males: Body mass, physical activity, and other media use. Eat. Behav. 2009, 10, 161–167. [Google Scholar] [CrossRef]
- Männikkö, N.; Billieux, J.; Kääriäinen, M. Problematic digital gaming behavior and its relation to the psychological, social and physical health of Finnish adolescents and young adults. J. Behav. Addict. 2015, 4, 281–288. [Google Scholar] [CrossRef]
- Männikkö, N.; Ruotsalainen, H.; Tolvanen, A.; Kääriäinen, M. Problematic gaming is associated with some health-related behaviors among Finnish vocational school students. Int. J. Ment. Health Addict. 2020, 18, 993–1007. [Google Scholar] [CrossRef] [Green Version]
- Ponce-Blandón, J.A.; Espejel-Hernández, I.; Romero-Martín, M.; Lomas-Campos, M.D.L.M.; Jiménez-Picón, N.; Gómez-Salgado, J. Videogame-related experiences among regular adolescent gamers. PLoS ONE 2020, 15, e0235327. [Google Scholar] [CrossRef]
- Stockdale, L.; Coyne, S.M. Video game addiction in emerging adulthood: Cross-sectional evidence of pathology in video game addicts as compared to matched healthy controls. J. Aaffect. Disord. 2018, 225, 265–272. [Google Scholar] [CrossRef]
- Vandewater, E.A.; Shim, M.S.; Caplovitz, A.G. Linking obesity and activity level with children’s television and video game use. J. Adolesc. 2004, 27, 71–85. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Carnell, S.; Haworth, C.M.; Plomin, R. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am. J. Clin. Nutr. 2008, 87, 398–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hibell, B.; Guttormsson, U.; Ahlström, S.; Balakireva, O.; Bjarnason, T.; Kokkevi, A.; Kraus, L. The ESPAD Report Substance Use among Students in 36 European Countries; The Swedish Council for Information on Alcohol and Other Drugs (CAN) and the Pompidou Group at the Council of Europe: Stockholm, Sweden, 2011; Available online: http://www.can.se/contentassets/8d8cb78bbd28493b9030c65c598e3301/the_2011_espad_report_full.Pdf (accessed on 13 December 2021).
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nashida, C.; Siekmann, J. Elaboración de un patrón OMS de crecimiento de escolares y adolescentes. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Langhinrichsen-Rohling, J.; Rohling, M.L.; Rohde, P.; Seeley, J.R. The SOGSRA vs. the MAGS-7: Prevalence estimates and the classification congruence. J. Gambl. Stud. 2004, 20, 259–281. [Google Scholar] [CrossRef]
- Colasante, E.; Gori, M.; Bastiani, L.; Scalese, M.; Siciliano, V.; Molinaro, S. Italian adolescent gambling behaviour: Psychometric evaluation of the South Oaks Gambling Screen: Revised for Adolescents (SOGS-RA) among a sample of Italian students. J. Gambl. Stud. 2014, 30, 789–801. [Google Scholar] [CrossRef]
- Rapporto Osservasalute 2016: Stato di Salute e Qualità Dell’assistenza Nelle Regioni Italiane. Osservatorio Nazionale Sulla Salute Nelle Regioni Italiane. Italia. Available online: https://www.osservatoriosullasalute.it/osservasalute/rapporto-osservasalute-2016 (accessed on 2 December 2021).
- Ceccarelli, G.; Bellato, M.; Zago, M.; Cusella, G.; Sforza, C.; Lovecchio, N. BMI and inverted BMI as predictors of fat mass in young people: A comparison across the ages. Ann. Hum. Biol. 2020, 47, 237–243. [Google Scholar] [CrossRef]
- Hills, A.P.; Andersen, L.B.; Byrne, N.M. Physical activity and obesity in children. Br. J. Sports Med. 2011, 45, 866–870. [Google Scholar] [CrossRef] [Green Version]
- Elinder, L.S.; Sundblom, E.; Rosendahl, K.I. Low physical activity is a predictor of thinness and low self-rated health: Gender differences in a Swedish cohort. J. Adolesc. Health 2011, 48, 481–486. [Google Scholar] [CrossRef]
- Jacobs, W.; Merianos, A.L.; Lee Smith, M.; Nabors, L.; Fajayan, A.; Valente, T.W. Examining the Role of Weight Status and Individual Attributes on Adolescent Social Relations. J. Adolesc. Health 2020, 67, 108–114. [Google Scholar] [CrossRef]
- Smarandescu, L.; Walker, D.; Wansink, B. Mindless drinking: How gender and BMI relate to the consumption of alcohol. Int. J. Drug Policy 2014, 25, 1131–1134. [Google Scholar] [CrossRef]
- Sayon-Orea, C.; Martínez-González, M.A.; Ruiz-Canela, M.; Bes-Rastrollo, M. Associations between yogurt consumption and weight gain and risk of obesity and metabolic syndrome: A systematic review. Adv. Nutr. 2017, 8, 146S–154S. [Google Scholar] [CrossRef]
- Traversy, G.; Chaput, J.P. Alcohol consumption and obesity: An update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y. Cross-national comparison of childhood obesity: The epidemic and the relationship between obesity and socioeconomic status. Int. J. Epidemiol. 2001, 30, 1129–1136. [Google Scholar] [CrossRef] [Green Version]
- French, S.A.; Tangney, C.C.; Crane, M.M.; Wang, Y.; Appelhans, B.M. Nutrition quality of food purchases varies by household income: The SHoPPER study. BMC Public Health 2019, 19, 231. [Google Scholar] [CrossRef] [Green Version]
- Biro, F.M.; Striegel-Moore, R.H.; Franko, D.L.; Padgett, J.; Bean, J.A. Self-esteem in adolescent females. J. Adolesc. Health 2006, 39, 501–507. [Google Scholar] [CrossRef]
- Tiggemann, M. Body dissatisfaction and adolescent self-esteem: Prospective findings. Body Image 2005, 2, 129–135. [Google Scholar] [CrossRef]
- Turner, H.M.; Rose, K.S.; Cooper, M.J. Schema and parental bonding in overweight and nonoverweight female adolescents. Int. J. Obes. 2005, 29, 381–387. [Google Scholar] [CrossRef] [Green Version]
- Yanovski, J.A. Trends in underweight and obesity—scale of the problem. Nat. Rev. Endocrinol. 2018, 14, 5–6. [Google Scholar] [CrossRef]
- Wilson, G.T. Eating disorders, obesity and addiction. Eur. Eat. Disord. Rev. 2010, 18, 341–351. [Google Scholar] [CrossRef]
- Esmaeelzadeh, S.; Moraros, J.; Thorpe, L.; Bird, Y. Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the US and Canada—A systematic review and meta-analysis. J. Clin. Med. 2018, 7, 543. [Google Scholar] [CrossRef] [Green Version]
- Li, G.; Hou, G.; Yang, D.; Jian, H.; Wang, W. Relationship between anxiety, depression, sex, obesity, and internet addiction in Chinese adolescents: A short-term longitudinal study. Addict. Behav. 2019, 90, 421–427. [Google Scholar] [CrossRef]
- Slobodin, O.; Crunelle, C.L. Mini review: Socio-cultural influences on the link between ADHD and SUD. Front. Public Health 2019, 7, 173. [Google Scholar] [CrossRef]
- Theule, J.; Hurl, K.E.; Cheung, K.; Ward, M.; Henrikson, B. Exploring the relationships between problem gambling and ADHD: A meta-analysis. J. Atten. Disord. 2019, 23, 1427–1437. [Google Scholar] [CrossRef]
- Horsager, C.; Færk, E.; Gearhardt, A.N.; Lauritsen, M.B.; Østergaard, S.D. Food addiction comorbid to mental disorders in adolescents: A nationwide survey and register-based study. Eat. Weight Disord. 2021, 1–15. [Google Scholar] [CrossRef]
- Lin, C.Y.; Potenza, M.N.; Ulander, M.; Broström, A.; Ohayon, M.M.; Chattu, V.K.; Pakpour, A.H. Longitudinal relationships between nomophobia, addictive use of social media, and insomnia in adolescents. Healthcare 2021, 9, 1201. [Google Scholar] [CrossRef]
- Ministry of Health. Quaderni del Ministrero Della Salute: Linee di Indirizzo Nazionali per la Riabilitazione Nutrizionale Nei Disturbi Dell’alimentazione n. 29-2017, ISSN 2038-Italy. Available online: http://www.quadernidellasalute.it/imgs/C_17_pubblicazioni_2636_allegato.pdf (accessed on 1 December 2021).
| Independent Variables | Questions | Codes |
|---|---|---|
| Psychosocial Variables | ||
| Physical activity = hardly ever/rarely | Think back over the last 12 month. How often did you exercise? | Hardly ever/rarely = Never; few times/year; 1–2 times/week vs. Often = 3–4 times/week; almost every day |
| Relationship with parents | In general, how satisfied are you with the relationship with your parents? | Very satisfied; satisfied vs. neither satisfied nor dissatisfied; not so satisfied; unsatisfied |
| Self-satisfaction | In general, how satisfied are you with yourself? | Very satisfied; satisfied vs. neither satisfied nor dissatisfied; not so satisfied; unsatisfied |
| Health satisfaction | In general, how satisfied are you with your health? | Very satisfied; satisfied vs. neither satisfied nor dissatisfied; not so satisfied; unsatisfied |
| Family’s financial situation | How well off is your family compared to other families in your country? | Medium/high financial situation = very much better off; much better off; better off; about the same vs. low financial family situation = less well off; much less well off; very much less well off |
| School performance | Which of the following best describes your average grade at the end of the last term? | Excellent; good = high vs. medium; low = on the average; below the average |
| Risk behaviors variable | ||
| Gambling | South Oaks Gambling Screen: Revised for Adolescents (SOGS-RA) | Non-problematic, at risk, and problematic profile |
| Gaming | “I think that I spend way too much time gaming” “My parents tell me that I spend way too much time gaming” | Agree = strongly agree; partly agree vs. not agree = neither nor, partly disagree; strongly disagree |
| Psychoactive: Illegal substance use—cannabis | During the last 30 days, on how many occasions (if any) have you used cannabis? | Less than 10 times vs. 10 or more times |
| Psychoactive: Illegal substance use | During the last 12 months, on how many occasions (if any) have you used:
| Use = one or more times vs. non-use = never |
| Psychoactive: Legal substance use—tobacco | Think back again over the last 30 days. How many cigarettes did you smoke per day? | Less than 6 = never, less than 1 cigarette/week, less than 1 cigarette/day, 1–5 cigarettes/day vs. 6 or more = 6–10 cigarettes/day, 11–20 cigarettes/day, 20 or more cigarettes/day |
| Psychoactive: Legal substance use—alcohol | Think back again over the last 30 days. On how many occasions (if any) have you had any alcoholic beverages to drink? | Less than 10 vs. more than 10 |
| Underweight | p-Value | Overweight | p-Value | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||
| Physical activity = hardly ever/rarely | 1.575 (1.358; 1.827) | *** | 1.602 (1.392; 1.843) | *** |
| Low financial family situation | n.s. | n.s. | 1.556 (1.259; 1.924) | *** |
| Dissatisfied with health | 1.460 (1.178; 1.809) | ** | 1.638 (1.354; 1.981) | *** |
| Dissatisfied with himself | n.s. | n.s. | 1.238 (1.055; 1.454) | ** |
| Dissatisfied with relationship with parents | n.s. | n.s. | n.s. | n.s. |
| High academic performance | n.s. | n.s. | 0.797 (0.694; 0.916) | ** |
| I think I spend way too much time gaming = I agree | 0.834 (0.702; 0.992) | * | n.s. | n.s. |
| My parents tell me, I spend way too much time gaming = I agree | n.s. | n.s. | 1.209 (1.025; 1.426) | * |
| Gambler’s profile = at risk | n.s. | n.s. | n.s. | n.s. |
| Gambler’s profile = problem | n.s. | n.s. | 1.656 (1.257; 2.181) | *** |
| Drinking 10 or more times in a month | n.s. | n.s. | 1.412 (1.161; 1.716) | ** |
| Smoking 6 or more cigarettes per day | 0.687 (0.519; 0.910) | * | n.s. | n.s. |
| Smoking cannabis 10 or more times in a month | n.s. | n.s. | n.s. | n.s. |
| Use of energy drinks during last year | 0.821 (0.709; 0.951) | ** | n.s. | n.s. |
| Use of anabolic/testosterone during last year | n.s. | n.s. | n.s. | n.s. |
| Use of any other illegal substances during last year | n.s. | n.s. | n.s. | n.s. |
| Underweight | ||
| OR (95% CI) | p-Value | |
| Being under 18 | 0.633 (0.569; 0.705) | *** |
| Physical activity = hardly ever/rarely | 1.627 (1.228; 2.155) | ** |
| Low financial family situation | n.s. | n.s. |
| Dissatisfied with health | n.s. | n.s. |
| Dissatisfied with himself | n.s. | n.s. |
| High academic performance | n.s. | n.s. |
| I think I spend way too much time gaming = I agree | n.s. | n.s. |
| My parents tell me, I spend way too much time gaming = I agree | 1.800 (1.295; 2.501) | *** |
| Gambler’s profile = at risk | n.s. | n.s. |
| Gambler’s profile = problem | n.s. | n.s. |
| Drinking 10 or more alcoholic drink in a month | 1.683 (1.135; 2.497) | * |
| Smoking 6 or more cigarettes per day | n.s. | n.s. |
| Use of energy drinks during last year | n.s. | n.s. |
| Overweight | ||
| OR (95% CI) | p-value | |
| Being under 18 | n.s. | n.s. |
| Physical activity = hardly ever/rarely | 1.969 (1.538; 2.521) | *** |
| Low financial family situation | 1.649 (1.145; 2.374) | ** |
| Dissatisfied with health | 2.132 (1.512; 3.007) | *** |
| Dissatisfied with himself | n.s. | n.s. |
| High academic performance | n.s. | n.s. |
| I think am spending too much time to play = I agree | n.s. | n.s. |
| My parents tell me, that I am spending too much time to play = I agree | n.s. | n.s. |
| Gambler’s profile = at risk | n.s. | n.s |
| Gambler’s profile = problem | 1.804 (1.280; 2.542) | ** |
| Drinking 10 or more alcoholic drink in a month | 1.597 (1.160; 2.198) | ** |
| Smoking 6 or more cigarettes per day | n.s. | n.s. |
| Use of energy drinks during last year | n.s. | n.s. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denoth, F.; Biagioni, S.; Baldini, F.; Baroni, M.; Franchini, M.; Molinaro, S. Weight Categories among Male Adolescents Linked to Risky Behaviors: High or Low BMI, Which Is Worse? Adolescents 2022, 2, 128-139. https://doi.org/10.3390/adolescents2010012
Denoth F, Biagioni S, Baldini F, Baroni M, Franchini M, Molinaro S. Weight Categories among Male Adolescents Linked to Risky Behaviors: High or Low BMI, Which Is Worse? Adolescents. 2022; 2(1):128-139. https://doi.org/10.3390/adolescents2010012
Chicago/Turabian StyleDenoth, Francesca, Silvia Biagioni, Federica Baldini, Marina Baroni, Michela Franchini, and Sabrina Molinaro. 2022. "Weight Categories among Male Adolescents Linked to Risky Behaviors: High or Low BMI, Which Is Worse?" Adolescents 2, no. 1: 128-139. https://doi.org/10.3390/adolescents2010012
APA StyleDenoth, F., Biagioni, S., Baldini, F., Baroni, M., Franchini, M., & Molinaro, S. (2022). Weight Categories among Male Adolescents Linked to Risky Behaviors: High or Low BMI, Which Is Worse? Adolescents, 2(1), 128-139. https://doi.org/10.3390/adolescents2010012






