Abstract
Measures taken to contain the COVID-19 pandemic are particularly stressful for families. Limited data is available regarding the effects of a mandatory quarantine on the psychological stress of children, adolescents and their parents. Quarantined individuals participating in the online-based CoCo-Fakt study had at least one child <3, 3 to <6, 6 to <10, 10 to <14 and 14 to <16 years old (n = 2153). Parents were asked about how often their children felt nervous, anxious, or tense, down or depressed, lonely or physical reactions occur. A relative sum score characterizing psychosocial stress was determined and related to parents’ socio-demographic factors, psychosocial distress, coping strategies and resilience. Parents reported significantly higher psychological stress if at least one child was quarantined. Parents’ relative psychological stress sum score had the strongest influence on the psychological state of the children across all age groups (β = 0.315–0.457) besides male sex of the reporting parent, no partnership, low to medium socioeconomic status, lower resilience and coping scores, and parents quarantined as close contacts. The variance in the linear regression models was between 17.8% and 31.4%. These findings highlight that the entire family system must be considered during official mandatory quarantines.
1. Introduction
Since the first SARS-CoV-2 infections were identified in Wuhan, China, in December 2019, the virus has spread rapidly across the world and led to significant restrictions in private and public life [1]. Currently, more than 370 million people are affected worldwide, and there have been more than 5.6 million confirmed deaths [2]. In Germany, almost 10 million confirmed cases have been reported so far, 1.6 million of them in children and adolescents (under 15 years). The number of deaths in Germany is more than 117,000 [3]. Depending on the incidence numbers and nation, face masks, contact restrictions, and closures of kindergartens, schools, cultural institutions and sports facilities have become common and continue to dominate the daily lives of children and adolescents. Loneliness and social isolation are associated with poorer mental health among adolescents and young adults even in the absence of a pandemic, exacerbating the burdens of loss of functioning and low self-esteem [4,5]. During the earlier influenza A virus and the H1N1 and SARS-CoV-1 pandemics, it has already been shown that measures such as isolation and quarantine can be particularly traumatizing for children and their parents [6]. Indeed, based on parental statements, 30% of affected children in these earlier pandemics met the criteria for post-traumatic stress syndrome. Panda et al. (2021) studied the effects of the current pandemic, lockdowns and quarantine measures. They included 15 studies in their meta-analysis and showed that, from a total sample of 22,996 children, 34.5% suffered from anxiety, 41.7% from depression, 42.3% from increased irritability and 30.8% from concentration difficulties [7]. Furthermore, studies from China reported symptoms of restlessness, irritability, and concentration difficulties related to the COVID-19 pandemic in children and adolescents [8]. Fransisco et al. (2020) analyzed the immediate psychological and behavioral symptoms associated with COVID-19 quarantine in children and adolescents from Italy, Spain and Portugal [9]. To assess these symptoms, the parents of 1480 children and adolescents (52.8% boys) aged 3–18 years old were interviewed. According to the interviews, for most children, screen time increased from an average of 30–60 min per day to more than 3 h per day, and physical activity decreased to less than 30 min per day. In addition, approximately one-third of all children felt nervous, anxious, restless or fearful during the quarantine period.
In Germany, the Corona and Psyche (COPSY) study showed that, during the first wave of the pandemic in spring 2020, 71% of children and adolescents felt stressed by the shift in school operation toward home-schooling (64.4%), reduced contact with friends (82.2%) and more frequent arguments within the family (27.6%), and 75% of parents felt stressed by changes in their job situation [10]. In addition, the prevalence of children and adolescents with mental health problems almost doubled, from 17.6% (n = 273) to 30.4% (n = 482). In the study, two-thirds of parents felt that they needed support to cope with the schooling demands; their child’s return from lockdown; and their child’s behaviors, feelings and moods. Up to now, there is only limited knowledge about the specific strategies of how parents have dealt with these stresses or what measures they have taken. Knowledge about this is important in order to be able to support and advise parents in a more targeted way. For example, positive coping is associated with a reduction in stress levels, while negative coping is associated with an increase in stress, which in turn leads to an increase in psychological stress [11]. Within the COVID-19 pandemic, Singh et al. (2020) recommended that parents should be advised about appropriate preventive measures and coping mechanisms which the family as a team and children individually are motivated to follow [12].
Most existing studies have examined the consequences of nationally implemented contact-reducing measures, isolation measures and lockdowns [13,14,15]. However, individual, legally mandated quarantines implemented in previous pandemics have been found to cause an extreme psychological burden [16]. Specifically, little is known about how parents in Germany have dealt with the stay-at-home-order and the individual solutions and professional support systems that are required. As part of the Cologne-Corona Counselling and Support for Index and KontAKt Persons during the Quarantine Period (CoCo-Fakt) cohort study, parents were asked about the issues that their children experienced during their or their family’s quarantine. The aim of the present study is to analyse the psychological stress of children and adolescents during family or individual quarantines, the possible influencing factors and coping strategies, as well as to identify any support requirements. Therefore, we hypothesize that an officially ordered quarantine is associated with greater psychological stress in parents and children. In addition, we assume that there are correlations between the psychological stress and parental coping strategies.
2. Materials and Methods
2.1. Study Population
As part of the CoCo-Fakt study, an online survey of individuals who tested positive for COVID-19 infection (IP = infected person) and their close contacts (CP = contact person) was conducted between 12 December 2020 and 6 January 2021, following the COVID-19 Snapshot Monitoring Study conducted by the University of Erfurt, the World Health Organization (WHO), and the ‘Bundeszentrale für gesundheitliche Aufklärung’ (BzgA; Federal Centre for Health Education) [17]. For this purpose, all Ips and CPs registered in the database of ‘Digitales Kontaktmanagement’ (DiKoMa) until 9 December 2020 who were over 16 years old and provided an e-mail address were contacted via email. After participants agreed to the privacy statement and consent form, they received instructions and a brief explanation about the background of the survey, and they were then asked to complete the questionnaire. Individuals under 16 years of age, those without a valid email address and those without informed consent, as well as non-compliant individuals, deceased patients and individuals who were in medical or nursing homes, were excluded from the study. The survey link was sent to 33,699 people by e-mail and opened by 13,057 people. Only IPs or CPs (n = 2153) with at least one child in the age groups of <3 years (n = 586), 3 to <6 years (n = 476), 6 to <10 years (n = 674), 10 to <14 years (n = 718) and 14 to <16 years (n = 417) were included in the analysis, and these individuals provided information regarding whether none or at least one of the children was in quarantine alongside the interviewed parents (see Figure 1). Of the 2153 individuals included in this analysis, 876 (40.7%) were IPs and 1277 (59.3%) were quarantined as CPs. The mean duration of quarantine was 11.8 (±4.4) days. The mean age of the parents was 42.4 (±7.4) years, and 59.8% of the total sample were female (n = 1287). Of the participants, 1939 (91.8%) lived with a partner, 1758 (82.2%) had a high socio-economic status (SES), 365 (17.1%) had a medium SES, and 16 (0.7%) had a low SES; therefore, the medium and low SES groups were combined. Of the participants, 146 (7.0%) had a migrant background, and 133 (6.2%) had neither a garden nor a balcony during their quarantine.
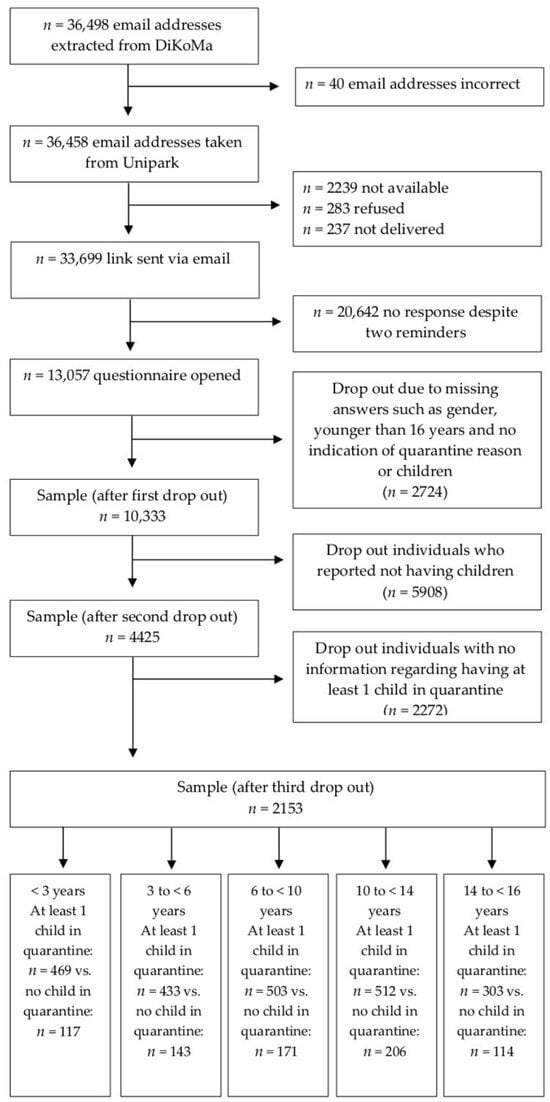
Figure 1.
Study population; all n-values refer to the number of parental statements.
2.2. Study Design
The survey was conducted using the software ‘Unipark’ in German, Turkish and English [18].
In the survey period of this study, CPs were defined according to criteria established by the German Robert Koch Institute (RKI) and the European Centre for Disease Prevention and Control (EDEC), among others, as individuals who had had contact with an IP for more than 10 to 15 min at a distance of less than two meters and without sufficient protection [19,20]. The sample was derived from the digitized data collected from quarantined individuals residing in Cologne. Since February 2020, IPs and CPs have been contacted by trained staff from the Cologne Public Health Department on the telephone and questioned in a standardized manner regarding their symptoms, possible route of infection, chronic diseases, risk factors, and residential and family situation. Additionally, these individuals were quarantined based on the legal regulations for combating infectious diseases according to the Infectious Diseases Protection Act (IfSG; usually 14 days of quarantine after a positive test result or symptom onset). In addition, the CPs of each IP were identified and also quarantined. This quarantine period amounted to between 10 and 14 days at the time of this survey, depending on the time of last contact. Moreover, until October 2020, this period could last for several weeks in families that could not be physically separated. All data were recorded using a specially programmed software, the digital contact management system (DiKoMa) of the Cologne Public Health Department [21].
2.3. Survey
2.3.1. Demographic Data of the Parents
Information regarding age (in years), sex (male or female), quarantine reason (IP or CP), and quarantine duration (in days) were recorded. Socioeconomic status (SES) was calculated based on the number of years of schooling completed (<10 years of schooling corresponded to low SES, 10 years of schooling corresponded to medium SES, and >10 years of schooling corresponded to high SES) [22,23]. Migration background was determined based on the primary language spoken at home (No = German spoken at home; Yes = a language other than German spoken at home). Additionally, information regarding housing situation (house or apartment, with or without garden or balcony) and relationship status (living with a partner or not) was collected.
2.3.2. Psychological Stress in the Different Age Groups
The children’s state of mind was assessed by asking parents the following questions, in line with the COSMO study (Wave 4 questionnaire, 24 March to 25 March 2020), which measured psychological distress during home quarantine [24]:
- -
- ‘The child/children felt nervous, anxious or on edge.’ (Item 1, Generalised Anxiety Disorder Scale-7 [GAD-7]) [25]
- -
- ‘The child/children felt depressed.’ (Item 6, Generalised Depression Scale [ADS]) [26]
- -
- ‘The child/children felt lonely.’ (Item 14, ADS)
- -
- ‘Thoughts about its/their experiences during the Coronavirus pandemic caused it/them to have physical reactions, such as sweating, trouble breathing, nausea or a pounding heart.’ (Item 19, Impact of Event Scale-Revised [IES-R]) [27]
Item responses were given on a six-point Likert scale rated from ‘not at all/less than 1 day’ to ‘always/daily’. To increase the informative value of the responses, they were grouped into ‘not at all’, ‘1–2 days’, ‘3–4 days’ and ‘5–7 days’ per week. A relative sum score was calculated related to the number of questions, with higher scores representing higher levels of psychological stress. The present study measured Cronbach’s alpha coefficients for the psychological distress score and sub-scale reliabilities for the different age groups of children: <3 years: α = 0.803 (0.670–0.842); 3 to <6 years: α = 0.777 (0.615–0.830); 6 to <10 years: α = 0.802 (0.645–0.861); 10 to <14 years: α = 0.811 (0.682–0.842); 14 to <16 years: α = 0.791 (0.660–0.820).
2.3.3. Parental Psychological Stress
Parental psychological distress was assessed using the same questions, supplemented by a question about hope from the COSMO study:
- -
- ‘I felt nervous, anxious or on edge.’ (Item 1, GAD-7)
- -
- ‘I felt down/depressed.’ (Item 6, ADS)
- -
- ‘I felt lonely.’ (Item 14, ADS)
- -
- ‘I thought of the future with hope.’ (Item 8, ADS)
- -
- ‘Thoughts about its/their experiences during the Coronavirus pandemic caused it/them to have physical reactions, such as sweating, trouble breathing, nausea or a pounding heart.’ (Item 19, IES-R)
Responses to these items were also given on the 6-point Likert scale from ‘not at all/less than 1 day’ to ‘always/daily’ and grouped in the same way as for the children’s stress scale. The item ‘I thought of the future with hope’ was reverse coded so that all items could be combined into a relative sum score related to the number of questions. The Cronbach’s alpha coefficient was 0.701 for the psychological distress score, and the subscale reliabilities ranged from 0.540 to 0.784.
2.3.4. Parental Coping Strategies
Parents’ utilisation of coping strategies and support systems was investigated with six items from the COSMO study:
- -
- ‘I have received offers of support from family, friends or neighbours.’ (Item 2, BZgA-coping)
- -
- ‘I had a plan for my daily life in terms of sleep, work or physical activities.’ (Item 4, BZgA-coping)
- -
- ‘I discovered activities for myself that made staying at home easier.’ (Item 6, BZgA-coping)
- -
- ‘I have used digital media to communicate with family, friends and acquaintances.’ (Item 1, BZgA-coping, modified)
- -
- ‘I was bored.’ (Item 7, BZgA-coping)
- -
- ‘I couldn’t do anything myself to influence the situation positively.’ (Item 2, BZgA-solidarity)
As with the previous variables, responses were given on a six-point Likert scale, and a relative sum score was calculated. A high relative score corresponded to greater use of coping strategies. The Cronbach’s alpha coefficient was 0.653 for the coping score, and the subscale reliabilities ranged from 0.564 to 0.650. A Cronbach’s alpha value higher than 0.70 would be ideal, but values higher than 0.6 for five items are statistically acceptable for a screening questionnaire [28].
In addition, with the option of free-text answers, parents were asked how they coped with the lack of care services, social contacts and leisure activities for their children during the stay-at-home quarantine period, regardless of whether the children themselves were under quarantine. These responses were summarized and divided into groups, including positive, neutral and negative evaluated strategies (see Table 1).

Table 1.
Free-text answers regarding coping strategies; divided into groups.
2.3.5. Parental Brief Resilience Scale
A subjective assessment of resilience was conducted with six items from the brief resilience scale (BRS; e.g., ‘I do not need much time to recover from a stressful event’), with responses ranging from 1 (‘I strongly disagree’) to 6 (‘I strongly agree’) [29,30]. In addition, items that focused on the current quarantine situation were used (e.g., ‘I know I will not be discouraged’) [31]. A relative sum score was formed in line with the methodology of the COSMO study, with higher scores representing higher levels of resilience. The present study found a Cronbach’s alpha coefficient of 0.815 for the BRS (0.770–0.803).
2.4. Data Analysis
Descriptive and inductive data analyses were conducted using the programme SPSS 28.0. Internal consistency of psychological stress, BRS and coping strategies was measured using Cronbach’s alpha coefficient. According to Nunnally and Bernstein (1994), a minimum value of Cronbach’s alpha = 0.7 is required [32]. Since the absolute level of the Cronbach’s alpha coefficient depends on the number of items (in our case only five or six items per scale) and a reduced reliability can be accepted for the present objective, reliability indices >0.6 are still assessed as appropriate. Chi-square tests and t-tests were conducted to assess the differences between both groups with children in quarantine and not in quarantine, including in terms of quarantine reason, gender, coping scores, psychological stress scores and BRS scores.
Backwards multiple linear regression was used to examine the factors potentially influencing the children’s psychological distress scores. The selection of those factors was based on a theory-based literature research, such as quarantine as an IP (1) or CP (2), sex of parent (female = 1, male = 2), the parent being in a partnership (yes = 1, no = 2), age (in years), living situation with balcony or garden (yes = 0, no = 1), parental education level (high = 1, middle and low = 2), parental psychological distress score, parental BRS score, parental coping score and migration background (no = 1, yes = 2). Non-significant factors were excluded during stepwise regression. The significance level was set at α = 0.05.
3. Results
3.1. Study Population and Demographic Data
Across all age groups, 1657 parents stated that they had at least one child in quarantine in addition to themselves (77.0%) and 496 had none (23.0%). It was significantly more common for at least one child to also be in quarantine if one parent was quarantined as an IP (p < 0.001), had a migrant background (p < 0.050), had low or middle SES (p < 0.050) or had neither a garden nor a balcony (p < 0.050). There were no identified differences based on parental gender or whether the parents lived with a partner (p > 0.050 for both cases). Parents who reported having at least one child in quarantine in at least one of the age groups were significantly younger (42.2 ± 7.6 versus 43.1 ± 7.0 years; p < 0.050), were themselves in quarantine for longer (12.1 ± 4.4 versus 10.8 ± 4.0 days; p < 0.001) and had a higher psychological burden (1.0 ± 0.7 versus 0.8 ± 0.6 relative sum scores; p < 0.001). Aside from these, there were no other significant differences (see Table 2).

Table 2.
Study population and demographic data.
3.2. Psychological Items and Relative Sum Scores of Psychological Stress in Children
3.2.1. Items
Overall, the children in each age group did not feel nervous, anxious or tense at all or only felt like this rarely during the family quarantine phase (between 72.9% and 81.3% ‘never’ or on ‘1–2 days per week’; between 4.1% and 9.4% on ‘5–7 days per week’). Significant differences were only found in the 6 to <10 age group as there were significantly higher reported levels of nervousness, tension or anxiety when at least one child was in quarantine (p < 0.050). There were no significant differences observed in the other age groups (see Supplementary Materials Table S2; Figure 2a).
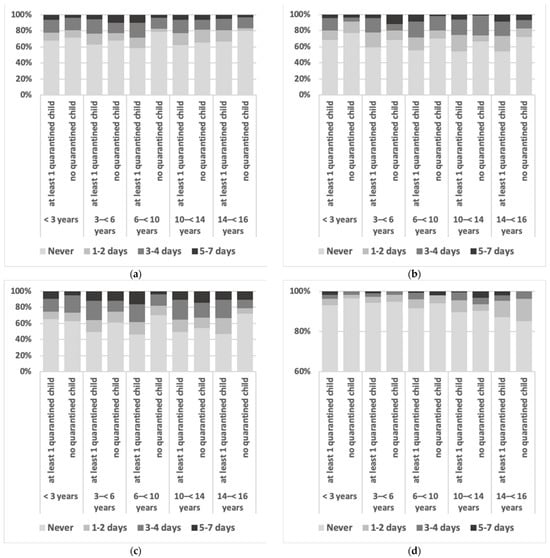
Figure 2.
Frequency of symptoms reported by parents with at least one child in quarantine versus no child in quarantine; (a) frequency of children feeling nervous, anxious, or tense during the quarantine period; (b) frequency of children feeling down or depressed during the quarantine period; (c) frequency of children feeling lonely during the quarantine period; (d) physical reactions in children triggered by the quarantine period, such as sweating, shortness of breath or palpitations; never (light grey), 1–2 days (middle grey), 3–4 days (dark grey), 5–7 days (black); see text for p-values.
Parents of all age groups rarely reported that children felt down or depressed (between 72.5% and 91.5% ‘never’ or on ‘1–2 days per week’; between 4.2% and 8.8% on ‘5–7 days per week’). Children feeling down or depressed occurred significantly more often in the context of child quarantine in the age groups 3 to <6 years and 10 to <14 years (p < 0.050; see Supplementary Materials Table S2; Figure 2b).
Loneliness was the most frequently reported issue in children (between 8.7% and 14.9% on 5–7 days). Additionally, significant differences were identified in children in the 6 to <10 age group (see Supplementary Materials Table S2; Figure 2c). As with children feeling down or depressed, loneliness was reported significantly more often when at least one child was in quarantine (p < 0.010).
Physical reactions in children were reported least often (between 95.2% and 97.5% ‘never’ or on ‘1–2 days per week’; between 0.8% and 1.9% on ‘5–7 days per week’). There were no significant correlations between loneliness and children’s quarantine; descriptively, loneliness was highest in the group with at least one quarantined child under three years of age, at 7.2% (see Supplementary Materials Table S2; Figure 2d).
3.2.2. Parental Strategies
Concerning the parents’ management and evaluation of the lack of childcare, social contacts and leisure activities for their children, results were heterogeneous (Supplementary Materials Table S3a–d). Negative parental evaluations were most common, except for the group of parents with 14 to <16-year-olds. For the 6 to <10-year age group, significant differences were identified between the groups with at least one child versus no child in quarantine in terms of parental assessments of lack of care services (p < 0.001). Indeed, lack of childcare was considered more problematic by parents of quarantined children. Many parents were able to adapt, especially during the lockdown period, in terms of care provision, such as through emergency care and the flexible adjustment of working hours. Additionally, they could adapt to the lack of social contacts and leisure activities through online services and online offers.
3.2.3. Children’s and Adolescents‘ Relative Sum Scores
There were no significant differences in the relative sum scores for psychological distress among the different age groups. Descriptively, psychological distress scores were lowest in children younger than three years old, with a score of 0.5 (±0.7), and these scores were highest in the group of children aged 6 to <10 years old, with a score of 0.7 (±0.8).
In families with no children in quarantine, the relative sum scores varied between 0.4 (±0.6 to ±0.8) for the age groups < 3, 6 to <10 and 14 to <16 years old, and 0.6 (±0.8) for children aged 10 to <14 years old.
In families with at least one child in quarantine, the relative sum scores ranged from 0.5 (±0.7) for the age group <3 years old to 0.7 (±0.8) for age group 6 to <10 years old. Significant higher relative sum scores were observed in families with a child in quarantine in the age group of children of 6 to <10 years old (0.7 [±0.8] versus 0.4 [±0.7]; p < 0.01; see Table 3).

Table 3.
Psychological distress score children in each age group; total scores and scores for at least one quarantined child versus none.
3.2.4. Multiple Linear Regressions
The multiple linear regression (stepwise backwards) revealed that parents’ relative psychological distress sum score was found to have the strongest influence on the psychological state of the children across all age groups (β = 0.315–0.457). In addition, male sex of the reporting parent, parents not living in a partnership, low to medium SES, lower BRS scores, lower coping scores and parents quarantined as CPs were associated with higher levels of psychological distress in children across all age groups. The variance in the models was between 17.8% and 31.4%. The correlations between the factors and psychological distress were strongest in the group of children aged 6 to <10 years old. In this group, male gender of the parent, higher psychological sum scores of the parent, and lower coping scores explained 31.4% of the variance in the child’s psychological distress. The factors of migration background, child quarantine and housing situation did not play significant roles in the model for any age group (see Table 4). The baseline models are presented in the Supplementary Materials (see Table S4).

Table 4.
Final models in multiple linear regressions in terms of children’s relative sum score.
4. Discussion
To the best of our knowledge, this is the first study in Germany examining the psychological status of children and adolescents in the context of officially mandated COVID-19 quarantines across different age groups. The highest levels of stress were found in children aged 6 to <10 years old, especially when at least one child was quarantined. Parents most frequently stated that children felt lonely in the context of family quarantine, with percentage rates between 8.7% and 14.9% for 5–7 days per week. In nearly all age groups, the school and kindergarten closures, lack of social contacts and leisure activities associated with the pandemic were predominantly assessed negatively by parents, except in the group of 14- to under 16-year-old children, possibly because adolescents have a lower need for care and have already developed independent coping strategies like connecting with others through online platforms, including playing video games together, and social media, religious coping styles, etc. [33,34]. As there is evidence that parental practices and coping measures affect children’s mental health, our study also shows that parental psychological stress had the strongest influence on child stress in every age group [12]. In most age groups, the factors of lower parental coping scores and parents being quarantined as CPs rather than IPs were associated with higher child psychological burden. The other analyzed factors, such as parental sex, parental partnerships, SES, resilience scores, migration background, housing situation and whether at least one child was quarantined had either an inconsistent effect or no effect on child psychological stress.
Palgi et al. (2020) stated that loneliness due to social-distancing policy was the main risk-factor for depression, anxiety and their comorbidity [35]. Similar results have been found in a rapid review of 63 studies and 51,576 participants, which showed a clear association between loneliness and mental health problems in children and adolescents [36]. In this review, no specific age group at higher risk could be identified, but the authors highlighted the stressful influence of school closures in the context of the COVID-19 pandemic. The German COSMO study showed that parents with school-age children experienced a significantly higher psychological burden from general contact-reducing measures, such as lockdowns, compared to the general study population, especially during the first pandemic wave from March 2020 to May 2020 [24].
Additionally, Browne et al. (2021) postulated that the pandemic may have led to disruptions in family relationships, which in turn may have affected children’s mental health [37]. They interviewed 549 families with 1098 children (two per family) aged 5–18 years old, and showed that stress related to COVID-19 corresponded to greater differences in the mental health of the siblings; specifically, the sibling with poorer mental health received lower-quality parenting over the study period, such as in terms of less attention. Dawes et al. (2021) also reported particular stress factors experienced by parents of children aged 0–12 years during the COVID-19 pandemic in the UK [38]. Their results highlighted the difficulty of coping with various household tasks and adapting the previous structures and routines of home life to the new situation. In addition, the usual support networks and personal relationships were significantly disrupted by pandemic-related measures, and mothers and single parents were found to be a particularly high-risk group. As a result, the authors called on policymakers and employers to promote appropriate adaptive coping strategies to support parents and, thus, their children during the pandemic. Nevertheless, positive experiences, including strengthened family relationships, have also been reported in the literature.
This call for support systems that involve the whole family is also underlined by our findings, especially for children of primary school age.
Strengths and Limitations
A strength of this study is the large and systematic sample of quarantined patients collected by the Cologne Health Department. In addition, the psychological burden of children and adolescents who were only indirectly affected by the quarantine was also recorded, e.g., if only one parent was in quarantine but not the child. This made it possible to form a comparison group of children and adolescents who were not quarantined. Noteworthy, the survey was conducted when the quarantine period had already lasted several weeks in some cases, which may have influenced the assessment of mental state during quarantine. However, the questionnaire was answered predominantly by people with high (82.2%) or medium (17.1%) SES, while people with a migration background (7.0%) or without a partnership (8.2%) were underrepresented. The group that had neither a garden nor a balcony was very small, too, so this may also have skewed the results. Furthermore, the results might have been different if the children had filled out the questionnaires themselves or if individual data per child had been collected. However, due to this approach, we cannot definitively exclude the possibility that the children’s data may be partially duplicated if both parents were quarantined and were asked to answer questions about their children. In addition, this survey did not record whether the quarantined children were also infected or clinically ill or investigate the effects of this on their psychological burden.
Of note, we chose this approach with the COSMO study in which the children were recorded in age groups in order to compare the two cohorts in terms of the effects of general quarantine or lockdown measures. For this reason, the questions on psychological stress or resilience and coping strategies were also taken from the COSMO study. All Cronbach’s alpha indicated an acceptable and good level of reliability. So far, only results on the psychological burden of adults are available from the COSMO study, but these appear comparable to COSMO in a range between 0.7 and 0.8 [39].
5. Conclusions
Considering the limitations mentioned above, it can be concluded that the psychological stress of children and adolescents in different age groups during an officially mandated quarantine is most strongly influenced by the psychological condition of the parents and the parental quarantine situation. Parents most clearly reported the issue of loneliness in their children, and the highest levels of psychological stress were found among quarantined children of primary school age. The correlation between higher psychological stress of children and adolescents and higher stress or poorer coping strategies of parents highlights the fact that the entire family should be supported during officially mandated quarantine periods. For example, support could be provided through offers of counselling in cases of psychological stress, strategies for dealing with loneliness and help with childcare. In addition, parents should be supported in practicing healthy communication, mental health hygiene, adaptive coping styles being positive role models, and practicing adaptive coping.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/adolescents2010011/s1, Table S1a–e: Study population and demographic (divided per age group); Table S2: Psychological items (1–4) children; Table S3a–d: Free-text answers; coping with the lack of care services, social contacts and leisure activities for their children; Table S4: Baseline Models in multiple linear regressions in terms of children’s relative sum score.
Author Contributions
Conceptualization, W.N., C.J., S.F. and B.G.; methodology, W.N., C.J., L.K. and A.F.; software, N.E. and N.S.; formal analysis, C.J. and W.N.; data curation, N.E.; writing—original draft preparation, W.N.; writing—review and editing, A.K., J.N. and G.A.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee) of the Rheinisch-Westfälische Technische Hochschule Aachen Human Ethics Research Committee (351/20).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used and analyzed during the current study involve sensitive patient information and indirect identifiers.
Acknowledgments
We want to thank all members of the contact tracing team at the Cologne Public Health Department, Bita Barezipour and all members of the CoCo-Fakt-group (Christine Joisten, Annelene Kossow, Julian Book, Lukas Broichhaus, Monika Daum, Nina Eisenburger, Alisa Fabrice, Sven Feddern, Andreas Gehlhar, Anna Carlotta Graf, Barbara Grüne, Markus Lorbacher, Johannes Nießen, Wanja Nöthig, Nikola Schmidt, Marc Tappiser, Gerhard A Wiesmüller). We would also like to thank all persons who participated in this questionnaire.
Conflicts of Interest
The authors declare no conflict of interest.
Correction Statement
This article has been republished with a minor correction to Author Contributions. This change does not affect the scientific content of the article.
References
- World Health Organization (WHO). Coronavirus Disease 2019 (COVID-19) Situation Report—94. 23 April 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200423-sitrep-94-covid-19.pdf (accessed on 5 October 2021).
- World Health Organization (WHO). Dashboard: Data Table: Global. Available online: https://covid19.who.int/table (accessed on 27 January 2022).
- Robert Koch Institut (RKI). COVID-19: Fallzahlen in Deutschland und Weltweit. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Fallzahlen.html (accessed on 27 January 2022).
- Christiansen, J.; Qualter, P.; Friis, K.; Pedersen, S.S.; Lund, R.; Andersen, C.M.; Bekker-Jeppesen, M.; Lasgaard, M. Associations of loneliness and social isolation with physical and mental health among adolescents and young adults. Perspect. Public Health 2021, 141, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Pitman, A.; Mann, F.; Johnson, S. Advancing our understanding of loneliness and mental health problems in young people. Lancet Psychiatry 2018, 5, 955–956. [Google Scholar] [CrossRef]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Francisco, R.; Pedro, M.; Delvecchio, E.; Espada, J.P.; Morales, A.; Mazzeschi, C.; Orgilés, M. Psychological Symptoms and Behavioral Changes in Children and Adolescents During the Early Phase of COVID-19 Quarantine in Three European Countries. Front. Psychiatry 2020, 11, 570164. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Otto, C.; Adedeji, A.; Napp, A.K.; Becker, M.; Blanck-Stellmacher, U.; Löffler, C.; Schlack, R.; Hölling, H.; et al. Mental health and psychological burden of children and adolescents during the first wave of the COVID-19 pandemic-results of the COPSY study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 1, 1–10. (In German) [Google Scholar] [CrossRef]
- Holz, N.E.; Boecker, R.; Jennen-Steinmetz, C.; Buchmann, A.F.; Blomeyer, D.; Baumeister, S.; Plichta, M.M.; Esser, G.; Schmidt, M.; Meyer-Lindenberg, A.; et al. Positive coping styles and perigenual ACC volume: Two related mechanisms for conferring resilience? Soc. Cogn. Affect. Neurosci. 2016, 11, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child. Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef]
- Imran, N.; Zeshan, M.; Pervaiz, Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak. J. Med. Sci. 2020, 36, S67–S72. [Google Scholar] [CrossRef] [PubMed]
- Viola, T.W.; Nunes, M.L. Social and environmental effects of the COVID-19 pandemic on children. J. Pediatr. (Rio J.) 2021, 20, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Mak, I.W.; Chu, C.M.; Pan, P.C.; Yiu, M.G.; Chan, V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 2009, 31, 318–326. [Google Scholar] [CrossRef]
- Betsch, C.; Wieler, L.H.; Bošnjak, M.; Ramharter, M.; Stollorz, V.; Omer, S.B.; Korn, L.; Sprengholz, P.; Felgendreff, L.; Eitze, S.; et al. Germany COVID-19 Snapshot MOnitoring (COSMO Germany): Monitoring knowledge, risk perceptions, preventive behaviours, and public trust in the current coronavirus outbreak in Germany. PsychArchives 2020. [Google Scholar] [CrossRef]
- Joisten, C.; Kossow, A.; Book, J.; Broichhaus, L.; Daum, M.; Eisenburger, N.; Fabrice, A.; Feddern, S.; Gehlhar, A.; Graf, A.C.; et al. How to manage quarantine-adherence, psychosocial consequences, coping strategies and lifestyle of patients with COVID-19 and their confirmed contacts: Study protocol of the CoCo-Fakt surveillance study, Cologne, Germany. BMJ Open 2021, 11, e048001. [Google Scholar] [CrossRef]
- Robert Koch Institut. Kontaktpersonen-Nachverfolgung (KP-N) bei SARS-CoV-2-Infektion. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Kontaktperson/Management.html;jsessionid=6698FA696287D9A6178D68FE43A49F15.internet112?nn=13490888#doc13516162 (accessed on 22 December 2021).
- European Centre for Disease Prevention and Control. Ermittlung von Kontaktpersonen: Umgang des Gesundheitswesens mit Personen (einschließlich Beschäftigten in Gesundheitsberufen), die mit COVID-19-Infizierten in der EU in Kontakt Standen—zweite Aktualisierung. 8 April 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/Public%20health%20management%20people%20in%20contact%20with%20COVID19%20cases_DE.pdf (accessed on 19 December 2021).
- Neuhann, F.; Buess, M.; Wolff, A.; Pusch, L.; Kossow, A.; Winkler, M.; Demir, J.; Beyé, M.; Wiesmüller, G.A.; Nießen, J.; et al. Softwareentwicklung zur Unterstützung der Prozesse im Gesundheitsamt der Stadt Köln in der SARS-CoV-2-Pandemie Digitales Kontaktmanagement (DiKoMa). Epidemiol. Bull. 2020, 23, 3–11. [Google Scholar] [CrossRef]
- Lampert, T.; Kroll, L.E.; Müters, S.; Stolzenberg, H. Measurement of the socioeconomic status within the German Health Update 2009 (GEDA). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2012, 56, 131–143. [Google Scholar] [CrossRef]
- Lange, C.; Jentsch, F.; Allen, J.; Hoebel, J.; Kratz, A.L.; von der Lippe, E.; Müters, S.; Schmich, P.; Thelen, J.; Wetzstein, M.; et al. Data Resource Profile: German Health Update (GEDA)—The health interview survey for adults in Germany. Int. J. Epidemiol. 2015, 44, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Rabe, J.E.; Schillok, H.; Merkel, C.; Voss, S.; Coenen, M.; De Bock, F.; von Rüden, U.; Bramesfeld, A.; Jung-Sievers, C.; COSMO-Gruppe. Burden in parents of school-aged children during different phases of the COVID-19 pandemic in Germany: An analysis within the COVID-19 snapshot monitoring (COSMO) study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 64, 1500–1511. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Hautzinger, M.; Bailer, M.; Hofmeister, D.; Keller, F. ADS—Allgemeine Depressionsskala; Manual. 2., überarbeitete und neu normierte Auflage; Hogrefe: Göttingen, Germany, 2012. [Google Scholar]
- Maercker, A.; Schützwohl, M. Assessment of post-traumatic stress reactions: The Impact of Event Scale-Revised (IES-R). Diagnostica 1998, 44, 130–141. [Google Scholar] [CrossRef]
- Muris, P.; Meesters, C.; Eijkelenboom, A.; Vincken, M. The self report version of the Strengths and Difficulties Questionnaire: Its psychometric properties in 8–13 year old non- clinical children. Br. J. Clin. Psychol. 2004, 43, 437–448. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Kunzler, A.M.; Chmitorz, A.; Bagusat, C.; Kaluza, A.J.; Hoffmann, I.; Schäfer, M.; Quiring, O.; Rigotti, T.; Kalisch, R.; Tüscher, O.; et al. Construct Validity and Population-Based Norms of the German Brief Resilience Scale (BRS). Eur. J. Health Psychol. 2018, 25, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of Uncertainty and Mental Wellbeing: Serial Mediation by Rumination and Fear of COVID-19. Int. J. Ment. Health Addict. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Ferguson, K.N.; Coen, S.E.; Tobin, D.; Martin, G.; Seabrook, J.A.; Gilliland, J.A. The mental well-being and coping strategies of Canadian adolescents during the COVID-19 pandemic: A qualitative, cross-sectional study. CMAJ Open. 2021, 16, E1013–E1020. [Google Scholar] [CrossRef] [PubMed]
- Kadiroğlu, T.; Güdücü Tüfekci, F.; Kara, A. Determining the Religious Coping Styles of Adolescents in Turkey during COVID-19. J. Relig. Health 2021, 60, 3406–3417. [Google Scholar] [CrossRef] [PubMed]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef]
- Browne, D.T.; Wade, M.; May, S.S.; Jenkins, J.M.; Prime, H. COVID-19 disruption gets inside the family: A two-month multilevel study of family stress during the pandemic. Dev. Psychol. 2021, 57, 1681–1692. [Google Scholar] [CrossRef] [PubMed]
- Dawes, J.; May, T.; McKinlay, A.; Fancourt, D.; Burton, A. Impact of the COVID-19 pandemic on the mental health and wellbeing of parents with young children: A qualitative interview study. BMC Psychol. 2021, 9, 194. [Google Scholar] [CrossRef] [PubMed]
- Gilan, D.; Röthke, N.; Blessin, M.; Kunzler, A.; Stoffers-Winterling, J.; Müssig, M.; Yuen, K.; Tüscher, O.; Thrul, J.; Kreuter, F.; et al. Psychomorbidity, Resilience, and Exacerbating and Protective Factors During the SARS-CoV-2 Pandemic. Dtsch. Arztebl. Int. 2020, 117, 625–630. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).