1. Introduction
Over the past two decades, the progressive digitization of dentistry has dramatically reshaped clinical practice, improving diagnostic accuracy, treatment planning, and patient communication [
1]. Among the most transformative tools are intraoral scanners and facial photogrammetry systems, which have enabled the generation of precise three-dimensional (3D) models of both hard and soft tissues. Initially developed to support restorative and orthodontic procedures, such as crown fabrication, implant planning, and aligner design, these technologies have evolved to capture increasingly complex anatomical surfaces, extending their utility well beyond the boundaries of traditional dental applications [
2].
Modern intraoral scanners utilize structured light- or laser-based triangulation to record detailed surface geometries [
3]. While their primary target has been the dentition, recent hardware and software advancements now allow the reliable digitization of intraoral mucosa, gingiva, and even perioral cutaneous structures. This has opened the door to their application in areas such as prosthodontics, oral surgery, and maxillofacial rehabilitation, where soft-tissue integration plays a critical role. Concurrently, photogrammetry, a technique based on the processing of multiple photographic images from different angles, has gained ground in dental and medical aesthetics, offering clinicians the ability to analyze facial symmetry, proportions, and volumetric changes with high fidelity and to plan orthodontic and prosthetic treatment plans by previewing the results [
4].
Although these two methods originate from distinct clinical domains, they share a common technical foundation: the non-invasive digital acquisition and rendering of anatomical surfaces with high spatial resolution. This convergence has led to their experimental application in other disciplines like forensic science. In forensic odontology, for example, 3D digitization has enabled more reliable documentation of anatomical features, such as palatal rugae and lip prints, which can be used for human identification [
5]. Moreover, the capacity to generate permanent, shareable, and metrically accurate digital models represents a critical advancement in forensic pathology, particularly in the documentation of time-sensitive or degradable evidence.
Bite marks, whether of human or animal origin, are among the most debated and methodologically complex forms of forensic evidence. The irregular morphology, shaped in part by primary distortion at the moment of the bite, itself influenced by variable posture and soft-tissue tension, together with the susceptibility to decomposition and the risk of deformation during impression taking, poses significant challenges to reproducibility and expert interpretation. In addition to the limitations already discussed, it is important to acknowledge that the transfer of bite force to soft tissues does not always result in a lesion that faithfully represents the dentition of the biter. As a consequence, correlating a bite mark with a specific individual may often be unreliable or even impossible [
6]. Traditional documentation methods, including two-dimensional photography and physical casts [
7], are often inadequate to capture the true spatial characteristics of these injuries, especially when recorded on curved or soft-tissue surfaces.
Furthermore, a major limitation in bite mark analysis lies in the inconsistency of expert evaluations. Interpretations are often discordant between practitioners and may even vary over time when re-evaluated by the same examiner, as highlighted by previous studies [
8]. This lack of inter- and intra-observer reliability undermines the forensic value of bite mark evidence and reinforces the importance of objective and standardized documentation protocols. Also for this reason, alternative investigative approaches are being explored, including the detection of the victim’s DNA in the oral cavity of the dog [
9].
In this context, digital 3D acquisition methods offer several compelling advantages: non-contact scanning reduces the risk of evidence deformation; accurate scaling and texture mapping preserve both morphological and dimensional fidelity; and the resulting models can be archived, reanalyzed, or transmitted for remote consultation without loss of information. However, to date, their application to post-mortem forensic investigation remains underexplored, particularly in cases involving soft-tissue trauma.
The present study aims to address this gap by documenting two real forensic cases of animal-related fatalities. In the first, a clinical intraoral scanner (Dexis IS 3600) was repurposed for use on external skin surfaces, while in the second, a complete photogrammetric protocol was implemented using a DSLR camera (Canon EOS 6D) and the Agisoft Metashape Professional 2.2.1 [
10] software. Both methods were used to reconstruct the lesions three-dimensionally, with the goal of assessing their feasibility, strengths, and limitations within the specific constraints of the forensic workflow. By comparing these techniques across parameters such as model resolution, morphological fidelity, metric accuracy, and operational practicality, this paper proposes a preliminary framework to explore the potential of these techniques as complementary tools in the evolving landscape of medico-legal imaging.
2. Materials and Methods
2.1. Case Overview
This study examined two post-mortem cases involving human cadavers with evident soft-tissue injuries attributable to animal bites. Both autopsies were conducted as part of routine forensic procedures in a controlled dissection room under standardized lighting conditions. The lesions, characterized by lacerations, avulsions, and irregular wound margins, were primarily located on exposed skin surfaces, particularly the limbs and head areas, which are most susceptible to post-mortem scavenging.
Case 1 involved an 85-year-old male subject examined three days after death. A total of six distinct bite lesions were documented, distributed across the scalp, upper limbs, and hands. These were digitized using a handheld intraoral scanner, repurposed for extraoral application.
Case 2 involved a 62-year-old female subject examined five days after death. The subject exhibited three major bite lesions located on the right thigh, left upper arm, and diffuse soft-tissue damage across the entire scalp. A full photogrammetric acquisition protocol was employed for documentation of the lesions and surrounding anatomical context.
2.2. Integration of Guideline-Based Quality Criteria
Although the intraoral scanning and photogrammetry techniques used in this study are not yet codified within formal forensic guidelines, their application was designed to align with key quality criteria outlined by the American Board of Forensic Odontology (ABFO) and the International Organization for Forensic Odonto-Stomatology (IOFOS) [
11,
12]. These include attention to scale referencing, dimensional fidelity, and photographic clarity. Furthermore, the digital nature of both methods ensures the creation of permanent, shareable, and non-destructive records, thus addressing a central requirement of these protocols: the long-term preservation and reusability of forensic evidence. By integrating these principles into a digital workflow, we aimed to meet the highest standards of forensic documentation while exploring novel acquisition modalities.
2.3. Intraoral Scanner Protocol
In the first case, a DEXIS IS 3600 intraoral scanner, originally developed for capturing the intraoral anatomy, was repurposed for cutaneous application. The scanning procedure was carried out directly on the skin without the application of any matting agents or contrast-enhancing substances. The DEXIS IS ScanFlow software was used to acquire and render the scan in real time.
As intraoral scanners are optimized for dental anatomy, the absence of characteristic oral reference points (e.g., teeth or gingival margins) on flat skin surfaces initially compromised tracking reliability. To address this, the operator placed a gloved index finger adjacent to the lesion (
Figure 1). The software recognized the textured glove surface, allowing for initial alignment and stabilization of the scanning process. Once initiated, the scanner was able to register the natural texture of the skin, hair, and lesion margins as reliable features for spatial tracking.
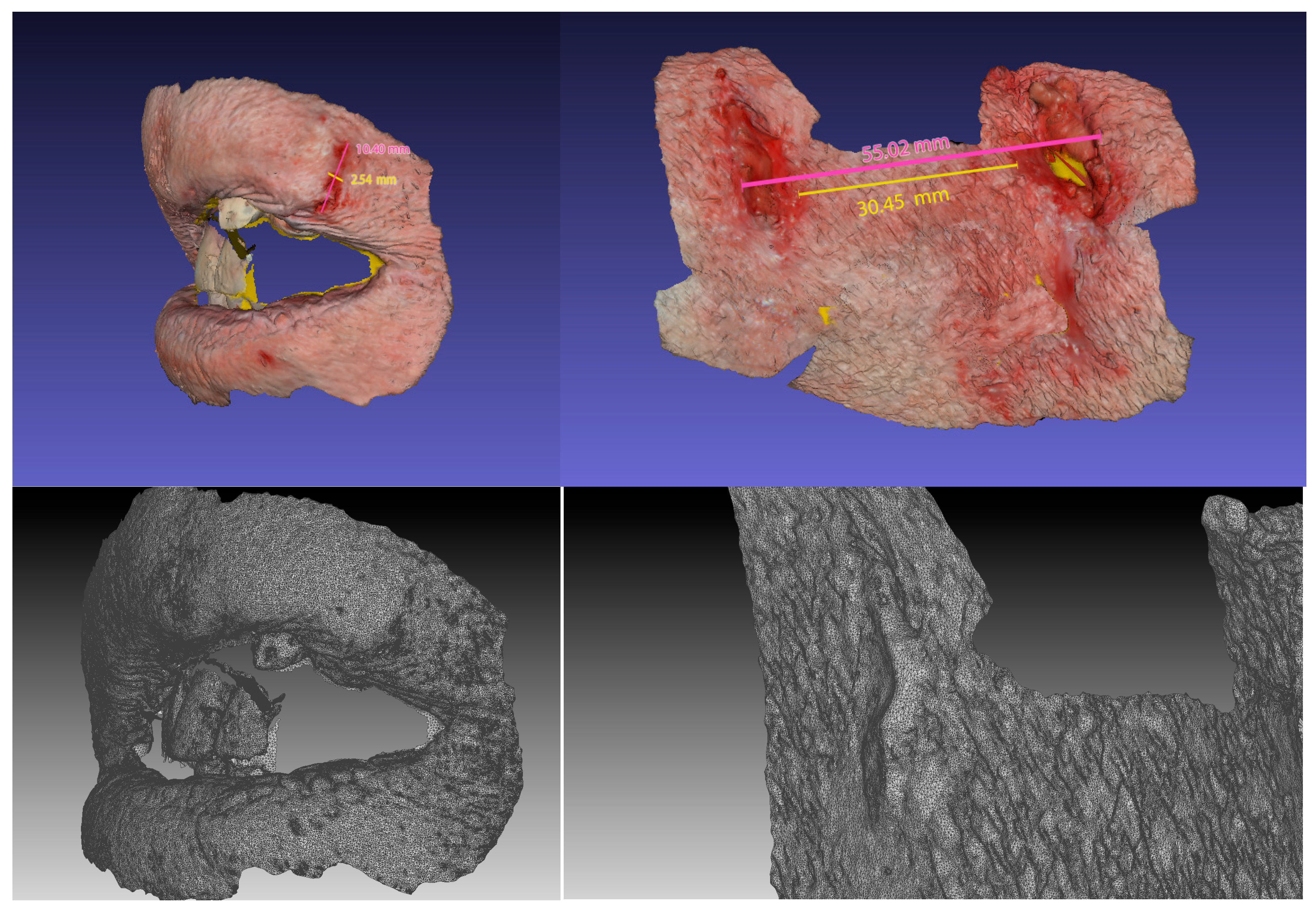
The scanner captured both geometric and color texture data, generating a polygonal 3D mesh. Scans were exported in both STL (geometry-only) and PLY (geometry with texture) formats. The resulting files were examined using 3D visualization software, and the lesion dimensions were cross-validated through manual caliper measurements obtained during the autopsy (
Figure 2).
2.4. Photogrammetry Protocol
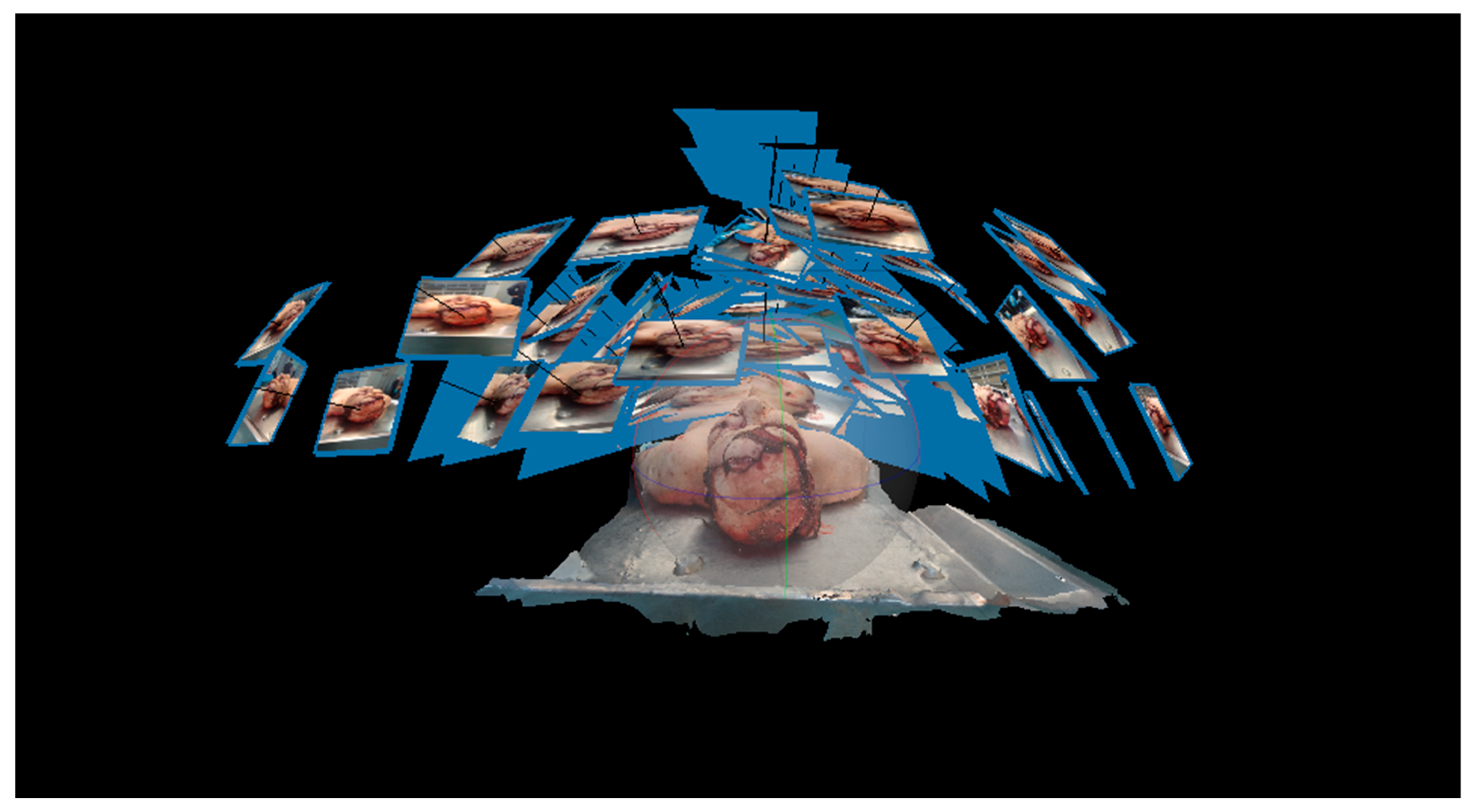
In the second case, a photogrammetric protocol was applied using a Canon EOS 6D DSLR camera with a 50 mm f/1.8 STM fixed-focal-length lens. Over 100 overlapping high-resolution images were captured from various angles around the lesion sites (
Figure 3), ensuring consistent lighting and minimal shadowing. A rigid metric ruler was placed adjacent to each lesion to provide an accurate scaling reference.
Image sets were processed using Agisoft Metashape Professional (version 2.2.1). The workflow included the following:
Photo alignment using high-accuracy settings.
Sparse and dense point cloud generation.
Mesh reconstruction from the dense cloud.
Texture mapping using the original photographs.
The 3D models were scaled to real-world dimensions based on the known reference length of the inserted scale bar. The final models were exported in OBJ format for texture analysis and in STL for purely geometric assessment (
Figure 4).
2.5. Measurement and Analysis
All exported 3D models were imported into Geomagic Control X (Artec 3D) [
13], a metrological software platform for dimensional analysis of digital meshes. Linear measurements of lesion length and width were obtained digitally and compared with the corresponding caliper measurements acquired during the autopsy.
The software also allowed qualitative evaluation of surface texture, spatial continuity of the lesion margins, and the potential for pattern recognition. While this study did not apply a formal bite mark-matching protocol, the fidelity of lesion documentation was assessed based on morphological clarity, dimensional stability, and the potential for long-term digital archiving.
3. Results
3.1. Intraoral Scanner Outcomes
The intraoral scanner (Dexis IS 3600) demonstrated a high degree of dimensional precision in documenting six bite lesions located on the scalp and limbs. Although not originally designed for cutaneous applications, the scanner was able to generate metrically stable polygonal meshes without requiring physical contact or impression material, thus avoiding any mechanical deformation of the lesions. The scanning process benefited from the incidental use of a gloved finger near the lesion to provide an initial tracking reference, an empirical but reproducible workaround to compensate for the absence of dental landmarks.
Once initiated, the scanner maintained continuous acquisition by recognizing anatomical texture features such as skin folds, hair, and wound borders. The resulting models were directly exported in STL and PLY formats, preserving both geometric and colorimetric information. However, the scanner’s field of view and depth acquisition are optimized for intraoral cavities, leading to a partial loss of morphological fidelity in highly curved or irregular regions. Additionally, the surface texture appeared moderately accurate but displayed occasional artifacts in areas with reflective or moist surfaces (
Figure 5). Despite these limitations, the scanner allowed for fast, portable, and reproducible acquisition, generating anatomically coherent 3D data with built-in dimensional consistency.
3.2. Photogrammetric Model Outcomes
In the second case, three bite lesions and an extensive scalp wound were documented via close-range photogrammetry. Over 100 high-resolution images were taken using a DSLR camera (Canon EOS 6D) under standardized lighting conditions (the surgical light of the autopsy room). A rigid metric scale was positioned adjacent to the wounds to enable proper scaling during digital reconstruction.
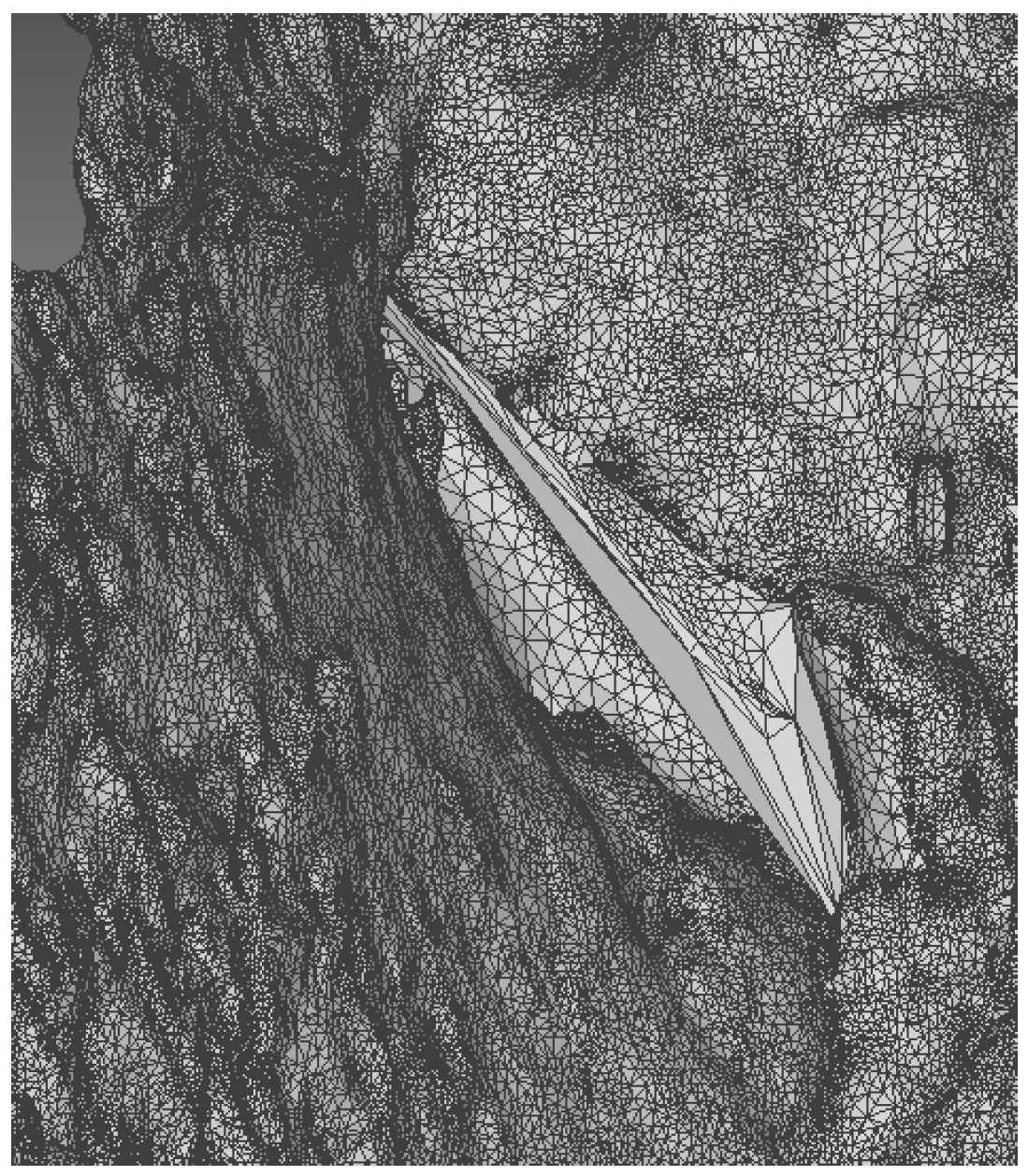
Photogrammetry produced morphologically detailed and visually rich 3D models, encompassing both the lesions and their surrounding anatomical environment. The ability to document broader surfaces and anatomical context provided additional forensic value. The texture quality was superior to that obtained with the intraoral scanner, capturing minute variations in skin and wound appearance. However, the method required longer acquisition and processing times, as well as a higher degree of operator experience. Moreover, challenges such as soft-tissue reflectivity and moist areas occasionally caused localized texture artifacts (
Figure 6), which were partially corrected during post-processing.
The dimensional accuracy in photogrammetry was dependent on the proper placement and recognition of the reference scale. When scaled correctly, the reconstructed lesions were consistent with manual observations and photographic records, although the absence of automated internal calibration introduced a non-negligible potential for deviation.
3.3. Morphology and Measurement Findings
Both intraoral scanning and photogrammetry allowed for successful three-dimensional documentation of the post-mortem bite injuries. The resulting models preserved the anatomical fidelity of the tissues with small, localized artifacts that did not involve the lesions and enabled subsequent digital manipulation and analysis.
Through the reconstructed 3D models, we were able to extract and analyze relevant forensic data, including the overall morphology of the bite marks, the number and arrangement of individual tooth impressions, and the precise dimensions of the injuries [
14,
15,
16]. Intraoral scanning provided high-resolution models suitable for detailed morphometric evaluation, revealing clear arc patterns and tooth-specific features, such as incisal edges, cusp tips, and inter-dental spacing. Photogrammetry, while slightly less precise in metric terms, yielded models with rich surface texture and broader contextual information, facilitating the spatial interpretation of the lesion within the facial soft tissue.
Both technologies enabled the measurement of bite mark dimensions, including inter-canine distances and the surface area of tissue involvement. These parameters are critical in forensic odontology for individualization, comparison with suspect dentition, and injury pattern interpretation.
Despite minor challenges in image acquisition, such as glare from moist surfaces or motion artifacts during scanning, the collected data were consistently analyzable, offering a reproducible and durable digital record of the lesions.
3.4. Comparative Observations
A comparative evaluation of the two acquisition methods revealed complementary strengths and limitations, particularly in the trade-off between dimensional precision and morphological representativeness.
The intraoral scanner, with a native accuracy of approximately 50–100 microns [
17], ensured submillimetric and microscale precision. This level of dimensional fidelity is inherently built into the scanner’s optical triangulation system and is routinely validated for intraoral dental structures. However, this same precision is obtained at the cost of morphological context: due to the limited field of view and software optimization for smooth intraoral surfaces, the broader anatomical features and spatial relationships of complex lesions are only partially reconstructed. In other words, while the scanner precisely maps microscopic geometry, it often lacks the macroscopic anatomical integration critical in forensic interpretation.
Conversely, photogrammetry yielded morphologically rich and anatomically comprehensive models, capturing the lesion in continuity with surrounding tissues, including the scalp, limbs, and adjacent anatomical landmarks. The overall dimensional accuracy of photogrammetric models depends on the photographic resolution, shooting angle redundancy, and proper scaling. When performed under controlled conditions and scaled via a rigid metric reference, typical accuracy ranges between 0.5 and 1.7 mm [
18], sufficient for macroscopic documentation but limited in microstructural detail. Therefore, photogrammetry excels in preserving the spatial and contextual morphology of lesions, at the expense of submillimetric accuracy. These differences are synthesized in
Table 1 below.
This comparison highlights a fundamental methodological dichotomy: the intraoral scanner captures microscale accuracy without full macroscale integration, whereas photogrammetry reconstructs anatomically realistic models but with less intrinsic metric precision. In forensic practice, selecting between the two approaches or combining them strategically depends on the specific analytical goals, whether emphasizing quantitative geometric analysis or qualitative anatomical interpretation.
4. Discussion
This pilot study explored the application of intraoral scanning and photogrammetry for the three-dimensional documentation of post-mortem bite marks, highlighting the unique advantages and limitations of each technique within a forensic context. Although these technologies were originally developed for clinical dental and orthodontic use, their non-contact and high-resolution nature render them promising tools for preserving delicate forensic evidence, such as soft-tissue trauma.
The intraoral scanner demonstrated strong performance in terms of dimensional accuracy, generating metrically stable models that aligned well with manual measurements obtained during autopsy. This finding aligns with the prior literature attesting to the submillimetric precision of structured light scanners used in dentistry. However, this precision was not without trade-offs. The scanner’s narrow field of view and algorithmic optimization for intraoral anatomy limited its ability to capture broader or topographically complex surfaces, particularly on curved or highly reflective skin regions. Furthermore, the lack of natural landmarks on cutaneous surfaces required the use of external reference points, such as a gloved finger, to initiate tracking, underscoring the scanner’s dependency on recognizable texture cues.
In contrast, the photogrammetric workflow yielded more morphologically expressive models, offering detailed reconstructions of the lesion topology and surrounding anatomical context. This contextual richness is particularly valuable in forensic casework, where understanding wound orientation, location, and spatial distribution contributes to reconstructive hypotheses and behavioral inferences. Despite its strengths, photogrammetry proved more time- and labor-intensive, requiring extensive image acquisition, careful lighting control, and post-processing. Moreover, its dimensional reliability was contingent on the correct placement and scaling of physical reference objects, a source of potential variability absent in the internally calibrated scanner system.
Importantly, both techniques share a critical forensic advantage: the avoidance of physical contact. Traditional bite mark documentation methods, including impression taking with dental silicone or alginate, are known to introduce mechanical distortion to soft tissues. This is particularly problematic in post-mortem settings, where tissue elasticity is altered by decomposition processes. In contrast, non-contact digital acquisition methods preserve the native morphology of wounds, facilitating more faithful reconstructions and enabling long-term digital archiving.
It is worth noting that this study was not designed to validate bite mark matching, but rather to evaluate the documentation phase. Nevertheless, the quality of the resulting models, especially in photogrammetry, suggests the feasibility of future integration with artificial intelligence or pattern recognition algorithms for comparative analysis. Additionally, the preservation of both geometric and texture data enables asynchronous expert consultation and remote analysis, offering practical advantages in multidisciplinary or transjurisdictional investigations.
Several limitations must be acknowledged. First, the sample size was inherently limited by the opportunistic nature of forensic casework and the pilot design of this study. Second, the variability in surface conditions (e.g., moist skin and hair interference) influenced the scan quality and may not be fully generalized to all forensic scenarios. Third, neither technique offers internal anatomical visualization, restricting analysis to surface-level injuries.
Despite these constraints, our findings support the feasibility of integrating both intraoral scanning and photogrammetry into post-mortem forensic workflows. Rather than being mutually exclusive, these methods may be viewed as complementary: the scanner offers high-fidelity metric precision for small, well-defined lesions, and photogrammetry provides contextual and morphological depth for broader anatomical reconstructions.
Future research should aim to expand the sample size, test the protocols in varied forensic scenarios (including human bite injuries), and evaluate inter-operator reproducibility. Additionally, the development of semi-automated pipelines for digital acquisition, scaling, and archiving could streamline adoption in routine forensic practice. Finally, the coupling of these technologies with machine learning may open new avenues for objective bite mark analysis, potentially addressing some of the methodological criticisms that have historically challenged the forensic validity of bite mark evidence.
5. Conclusions
This pilot study demonstrates the feasibility and forensic relevance of employing both intraoral scanning and photogrammetry for three-dimensional documentation of post-mortem bite injuries. Despite originating from distinct clinical domains, both technologies proved capable of generating analyzable, metrically valid digital reconstructions without physical contact, thereby preserving delicate and perishable anatomical evidence. The intraoral scanner offered rapid acquisition and high-dimensional precision, making it suitable for detailed metric analysis of localized lesions. Photogrammetry, in contrast, provided superior morphological context and texture fidelity, proving advantageous in cases requiring broad surface reconstruction and anatomical framing. While each method presents specific operational and technical limitations, such as a restricted field of view and surface reflectivity artifacts, these are offset by the benefits of digital permanence, shareability, and the potential for remote expert consultation. The non-destructive nature of both approaches aligns well with the preservation principles of forensic documentation, particularly when dealing with evidence subject to rapid post-mortem degradation.
Given the promising outcomes observed in this study, future work should focus on standardizing acquisition protocols, validating these methods across larger sample sizes, and integrating artificial intelligence to enhance pattern recognition and comparative analysis. Ultimately, the implementation of these digital tools into routine forensic workflows could contribute to more accurate, reproducible, and ethically sound documentation of soft-tissue injuries, marking a significant step forward in the evolution of forensic imaging.
Author Contributions
Conceptualization, S.N. and D.A.F.; methodology S.N., D.A.F., and E.D.V.; software, E.C. and D.A.; validation, P.M., G.A.S., S.Z., and A.A.; formal analysis, D.A.; investigation, M.P.; resources, S.Z., A.A., D.A., and M.P.; data curation, P.M., G.A.S., and E.C.; writing—original draft preparation, S.N. and D.A.F.; writing—review and editing, M.P.; visualization, E.D.V.; supervision, P.M. and G.A.S.; project administration, A.A. and G.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Our investigations were carried out following the rules of the Declaration of Helsinki of 1975, revised in 2013. According to Italian legislation, ethical approval for a single case is not required, as long as the data are kept anonymous and the investigations performed do not imply genetic results (GDPR nr 679/2016; 9/2016 and recent law addition number 424/19, July 2018).
Informed Consent Statement
The current Italian legislation requires neither the family’s consent nor ethical approval, as long as the data are strictly kept anonymous. Because summoning the parents was not possible, as it would badly interfere with the grieving process, the parents’ consent was completely waived, according to the Italian Authority of Privacy and Data Protection (“Garante della Privacy”: GDPR nr 679/2016; 9/2016 and recent law addition number 424/19, July 2018).
Data Availability Statement
The original contributions presented in this study are included in this article. Further inquiries can be directed to the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Haidar, Z.S. Digital dentistry: Past, present, and future. Digit. Med. Healthc. Technol. 2023, 2, 1–16. [Google Scholar] [CrossRef]
- Eggmann, F.; Blatz, M.B. Recent advances in intraoral scanners. J. Dent. Res. 2024, 103, 1349–1357. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Groth, C.; Jones, P.E.; Graham, J.W.; Redmond, W.R. Intraoral digital scanners. J. Clin. Orthod. 2014, 48, 337–347. [Google Scholar] [PubMed]
- Knyaz, V.A.; Zheltov, S.Y. Photogrammetric techniques for dentistry analysis, planning and visualisation. In Proceeding of the ISPRS Congress Beijing, Beijing, China, 3–11 July 2008; pp. 783–788. [Google Scholar]
- Di Vita, E.; Cacioppo, A.; Sciarra, F.M.; Messina, P.; Cumbo, E.M.; Caivano, G.; Zerbo, S.; Argo, A.; Albano, G.D.; Scardina, G.A. Preliminary insights into 3D cheiloscopy for forensic applications: A pilot study. Appl. Sci. 2025, 15, 1726. [Google Scholar] [CrossRef]
- Sauerwein, K.; Butler, J.M.; Reed, C.; Reczek, K.K. A NIST Scientific Foundation Review; NIST: Gaithersburg, MD, USA, 2003. [Google Scholar]
- Giovannini, E.; Bianchini, S.; Roccaro, M.; Pelletti, G.; Grandis, A.; Peli, A.; Lenz, J.; Pelotti, S.; Fais, P. Morphometric analysis of dog bitemarks. An experimental study. Forensic Sci. Int. 2025, 368, 112392. [Google Scholar] [CrossRef] [PubMed]
- Reesu, G.V.; Brown, N.L. Inconsistency in opinions of forensic odontologists when considering bite mark evidence. Forensic Sci. Int. 2016, 266, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Iarussi, F.; Cipolloni, L.; Bertozzi, G.; Sasso, L.; Ferrara, M.; Salerno, M.; Maglietta, F.; Dinisi, A.; Albano, D.; Sessa, F. Dog-bite-related attacks: A new forensic approach. Forensic Sci. Int. 2020, 310, 110254. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.agisoft.com/ (accessed on 1 April 2025).
- American Board of Forensic Odontology, Inc. Diplomates Reference Manual: Section IV Standards Guidelines (February 2021 Edition); American Board of Forensic Odontology, Inc.: Denver, Colorado, USA, 2001. [Google Scholar]
- International Organization for Forensic Odonto-Stomatology (IOFOS). Recommendations for Quality Assurance: Tooth Mark (Bite Mark) Analysis and Comparison; IOFOS: Lisbon, Portugal, 2018. [Google Scholar]
- Available online: https://www.artec3d.com/3d-software/geomagic-control-x (accessed on 1 April 2025).
- Tedeschi-Oliveira, S.V.; Trigueiro, M.; Oliveira, R.N.D.; Melani, R.F.H. Intercanine distance in the analysis of bite marks: A comparison of human and domestic dog dental arches. J. Forensic Odonto-Stomatol. 2011, 29, 39. [Google Scholar]
- Di Nunzio, M.; Della Valle, A.; Serino, A.; Corrado, F.; Di Nunzio, C. How the forensic multidisciplinary approach can solve a fatal dog pack attack. Forensic Sci. Med. Pathol. 2024, 20, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, E.; Roccaro, M.; Peli, A.; Bianchini, S.; Bini, C.; Pelotti, S.; Fais, P. Medico-legal. implications of dog bite injuries: A systematic review. Forensic Sci. Int. 2023, 352, 111849. [Google Scholar] [CrossRef] [PubMed]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and practicality of intraoral scanner in dentistry: A literature review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Urbanová, P.; Hejna, P.; Jurda, M. Testing photogrammetry-based techniques for three-dimensional surface documentation in forensic pathology. Forensic Sci. Int. 2015, 250, 77–86. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).