Abstract
Background/Objectives: Traditional diagnostic criteria for SBS include subdural, subarachnoid, and retinal hemorrhages. While intentional shaking is a known cause, the potential for similar forces acting on the head resulting from accidental trauma has not been fully explored. This study investigated the biomechanical forces on a model infant’s head during improper handling to determine if such forces could contribute to SBS without malicious intent. Methods: A realistic silicone infant model was equipped with an inertial measurement unit (IMU) to quantify head accelerations during two conditions: (1) placement of the infant model on a table with the head unsupported, and (2) manual shaking at maximum effort by 2 participants holding the model by the torso. Peak head accelerations were recorded for both conditions, and the results were analyzed for comparative assessment of the forces involved. Results: The average peak head acceleration when placing the infant model on a table with the head unsupported was +31,000 ± 7000 mg, with a range of +19,000.00 to +43,000 mg across trials. The average peak head accelerations during maximum effort shaking were significantly lower than placing the infant on the table, averaging 11,000 ± 10,000 vs. 31,000 ± 7000 mg, p < 0.0001). There were no significant differences in head accelerations between participants when placing the infant model on the table with the head unsupported (p = 0.89) nor with shaking the baby with maximum effort (p = 0.96). Conclusions: The study highlights that even accidental non-recommended handling of infants can result in high G-forces to the head, potentially leading to injuries similar to those observed in SBS. These findings highlight the necessity of supporting an infant’s head during handling and warrants caution against prematurely attributing physical abuse in SBS cases without considering unintentional causes.
1. Introduction
Annually, approximately 33 per 100,000 infants are diagnosed with abusive head trauma (AHT), also known as Shaken baby syndrome (SBS), in hospitals within the United States [1]. Infant AHT generally refers to conditions resulting with or without direct impact to the skull which leads to injuries within the cranium [2]. The diagnosis of SBS is often based on signs such as subdural, subarachnoid, and retinal hemorrhages [3]. While intentional shaking is widely recognized as a cause of these injuries, the potential for similar forces resulting from improper or accidental handling of infants has not been fully explored.
Contrary to the implications of the phrase “Shaken Baby Syndrome,” evidence shows that the act of shaking alone may not generate sufficient forces to cause the severe intracranial injuries typically associated with SBS. These studies involve infant models to prevent harm to an actual infant, and have reported that head accelerations during shaking generally peak around 8.5 G-force [4]. In a another study, similar results of shaking a baby produced head accelerations of 10–15 G-forces [5] and another producing mean peak head accelerations of 18.6 G-forces in the fore-aft direction [6].
Because there is not a validated threshold of G-force that definitively cause infant head injuries, comparing magnitude of forces during different tasks allows for inference of potential trauma. Car safety experiments demonstrate 29.3 G-forces with simulated 18-mph car accidents and 5.2 G-forces in 5-mph bumper car collisions. These simulated collisions have adult dummies in car seats with the body in a semi-reclined position. This is similar to the position of infants during the head shaking tasks described above. However, other researchers have shown that impacts from babies falling over 1 m falls can result in head accelerations over 200 G-force [7]. This much larger force may be generated both because of the supine position of the body, and the direct impact of the head with a surface, however is highly dependent upon the stiffness of the infant model used, as well as the rigidity of the surface that can alter the impulse.
While research has focused on head accelerations resulting from shaking or falls [8], less attention has been given to other scenarios such as placing infants on hard surfaces without proper head support. The potential for such actions to produce high G-forces and cause trauma comparable to SBS remains poorly understood, especially in cases of accidental abusive head trauma. As such, the purpose of this study was to determine infant head G-forces in two conditions: (1) shaking a baby at maximum force, and (2) placing the infant on a table with the head unsupported. To ensure repeatability, we compared forces between two participants, and to identify whether differences in forces exist between placing on a table and forces identified in other studies during shaking, we compared forces during these tasks. We hypothesized that head accelerations would be significantly higher in placing an infant on a table with the head unsupported compared to shaking an infant at maximum force.
2. Materials and Methods
2.1. Case Review
2.1.1. Incident
A 34-week prematurely born 8-month-old female infant was brought to local hospital in Texas after a call was made to 911 from a distressed father who stated his baby became non-responsive and stopped breathing. The infant was 64.0 cm in length and 8.62 kg in weight. The father brought his baby into the bedroom, placed her on the bed while he used the restroom briefly and then changed his shirt. Upon changing shirts and looking at his baby, the infant’s shirt was wet and covered in her own spit. The father got baby wipes on the other side of the room, walked back to the bed and the baby was making gurgling sounds. The father picked up the infant, turned her into a prone position, supported the infant’s body with one hand leaving the head unsupported and delivered back blows to get out whatever she choked on. The infant jerked and went limp. The father called 911 and ran out to the kitchen holding his infant. The infant was placed on the kitchen table, potentially with the head unsupported, and 911 was held on speaker phone. After some time, the father picked up the infant rapidly, ran to the front door and placed the infant on the grass while waiting for the ambulance to arrive. The infant did not survive.
2.1.2. Medical Records
The autopsy reports reported diagnoses of: blunt force injuries of the head and neck and bilateral panlobar acute pneumonia. Specifically, there were diagnoses of bilateral subdural hemorrhage (2 mL total), bilateral subarachnoid hemorrhage, intraventricular hemorrhage, bilateral optic nerve hemorrhages, COVID-19 positive, and posterior C1–C2 intramuscular hemorrhages without associated fractures. For the infant’s body measurements respective to age, the body length was less than 1st percentile, weight 70th percentile, head circumference of 43.0 cm in the 23rd percentile, chest circumference of 43.0 cm in the 28th percentile and abdominal circumference of 42.0 cm. The conclusion of the medical report is that this was a case of infant homicide. The infant born premature had early respiratory issues and the pneumonia may have been related to the positive COVID-19 diagnosis.
2.1.3. Instrumentation
One silicone life-like infant model was purchased for testing purposes. The height of the infant was 55.88 cm and the weight of the infant was 5.08 kg. This was slightly shorter and quite a bit lighter than the infant in the case,
The data collection was conducted in the SensorLab at the University of Arizona. Three-dimensional motion analysis of the infant’s head was conducted with one wireless Ultium inertial measurement unit (IMU) system collecting at 200 Hz (Noraxon, Scottsdale, AZ, USA). The IMU was securely affixed to the model infant’s head using a Velcro strap with the IMU at the anterior cranial just above the eyes in the midline (Figure 1).

Figure 1.
A photograph of the study design with an inertial measurement unit Velcroed around the silicone baby infant’s head to determine the head acceleration during a non-recommended handling and head impact with a table.
2.1.4. Procedures
Two participants (1M and 1F with no baby handling experience) were instructed to simulate placing an infant on a kitchen table (30 cm height and aluminum material). The participants were directed to hold the infant model by its torso, intentionally leaving the head unsupported, and then place the model supine on the table. Each participant was allowed five practice trials to familiarize themselves with the task and was explicitly instructed to avoid rough handling. Following this, five experimental trials were recorded for each participant.
Additionally, both participants were instructed to pick up the infant model, place their hands around the infant’s thorax, and shake the infant with maximum effort in a back-and-forth motion. This shaking task was performed once for approximately 5 s to simulate vigorous handling.
2.1.5. Data Analysis
The inertial measurement unit was positioned on the infant’s head in an orientation such that X was vertical, Y was mediolateral, and Z was anteroposterior. Peak head acceleration was defined as the value of the first positive peak after the infant’s impact with the table. The peak vertical force was designated as the first spike immediately following head impact onto the table. The peak head acceleration for the Z-axis (anteroposterior) during the maximum effort shaking trials were extracted, rectified, and the highest 5 peak accelerations during the 5 s shake were selected and averaged. The 5 highest accelerations from each condition were selected for analysis as they represent the worst-case scenarios, which are clinically relevant when evaluating potential head trauma in infants. To ensure fairness, accelerations were ranked by magnitude within each trial, and the top 5 were consistently selected. This method allowed for a standardized comparison across trials without excluding outliers. The peak head acceleration values for the Z-axis (anteroposterior) during the placing the infant on the table was calculated and averaged from the 5 trials. Peak head accelerations are reported as “mg” where 1 mg is equal to 0.001 G-force (e.g., 31,000 mg is the equivalent of 31 G-Force), and 1 G-force is equal to −9.81 m/s2.
To assess the magnitude of head acceleration between tasks, an independent t-test was conducted to compare the peak head accelerations during table placement with the peak head accelerations during the shaking with maximum effort of the infant model (SPSS, version 29, IBM Corp., Armonk, NY, USA). To assess inter-participant differences during the table placement task, an independent t-test was performed to compare the peak head accelerations during the table placement between the two participants’ five trials. To assess inter-participant differences during the maximum effort shake task, an independent t-test was performed to compare the peak head accelerations. Cohen’s d was conducted to determine the effect size of peak head accelerations between maximum effort shaking and placing the infant model on the table. Significance was determined at an alpha level of p < 0.05.
3. Results
The summarized results are presented in Table 1 and Table 2. The average peak head acceleration of the infant models’ head when being placed on a table with the head unsupported was +31,000 ± 7000 mg. In contrast, the peak head accelerations of the infant during a maximum exertion shake was significantly lower compared to the table condition (10,000 ± 3800 vs. 31,000 ± 7000 mg, t(18) = 9.34, p < 0.0001, Figure 2. The difference in peak head accelerations between the table-placement condition and maximum-effort shaking was both statistically significant and practically meaningful, with an extremely large effect size (mean difference = 20,000 mg; Cohen’s d = 3.88; 95% CI [14,400 mg, 25,600 mg]). This indicates that the magnitude of head accelerations generated during improper handling significantly exceeds those produced by maximum-effort shaking, highlighting the substantial biomechanical differences between these two scenarios. There were no significant differences in peak head acceleration between the two participants during the table task (31,000 ± 9400 vs. 31,000 ± 2800 mg, p = 0.89, Figure 3). There were no significant differences in peak head acceleration between the two participants during the maximum effort shaking task (16,000 ± 9500 vs. 12,000 ± 10,000 mg, p = 0.96).

Table 1.
The summarized results of the mean peak head accelerations (mg) for each participant observed in placing the infant model on the table with the head unsupported and shaking the infant with maximum effort. There were no significant differences between individuals’ results in the maximum effort shaking and table placement task (n = 5 for each condition).

Table 2.
The summarized results of the average peak head accelerations (mg) of both participants observed in placing the infant model on the table with the head unsupported and shaking the infant with maximum effort (n = 10 per condition).
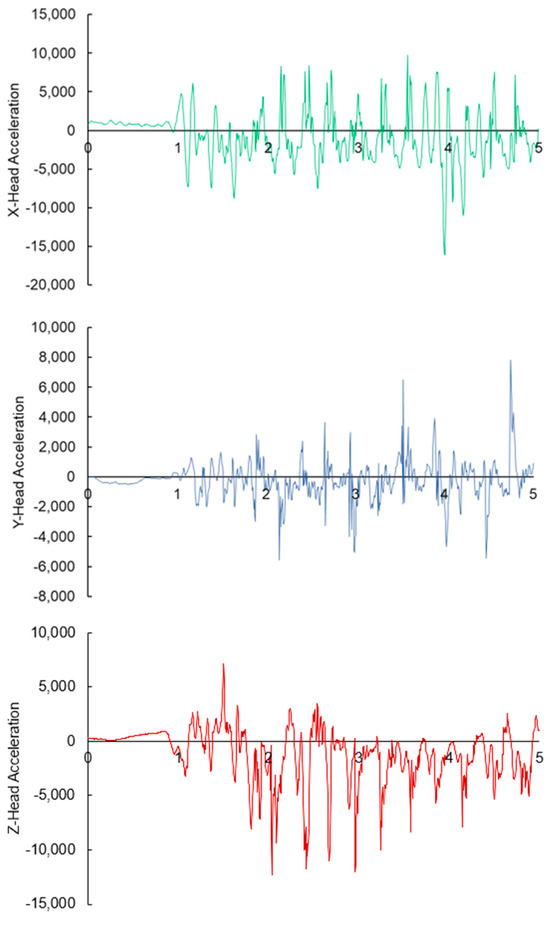
Figure 2.
A graph of the head acceleration (mg) of the infant while being shaken at maximum-force. The x-axis represents the time in seconds.
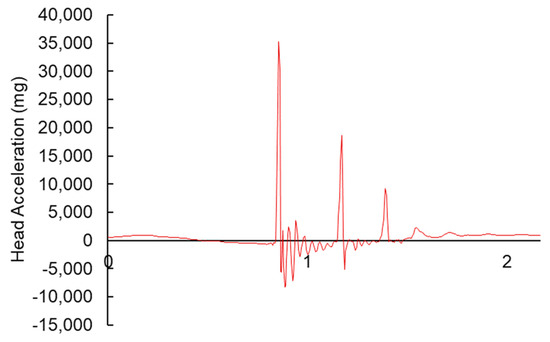
Figure 3.
An example of a graph of the infant’s head acceleration (mg) during the impact with the table. The x-axis represents time in seconds.
4. Discussion
Linear G-forces have been implicated in causing significant head injuries in infants, particularly in the context of abusive head trauma (AHT) [9]. In this study, we hypothesized that improper handling, such as placing an infant on a table without head support, could generate G-forces comparable to or even exceeding those associated with intentional shaking. Our findings confirmed this hypothesis, demonstrating that peak head accelerations during unsupported placement of the infant model on a table were over 300% higher than those recorded during maximum exertion shaking. These results highlight that G-forces produced in everyday scenarios, such as placing an infant on a hard surface without supporting the head, can exceed those generated during violent shaking.
When compared to known magnitudes, the G-forces observed in this study bring a new perspective in understanding the biomechanical forces on SBS. The peak head acceleration from placing an infant model on the table exceeds the 29.3 G-forces experienced in an 18-mph car crash and exceed the 5.2 G-forces head accelerations recorded in a 5-mph bumper car collision [10]. The results from these prior studies, and compared to the results of this current study, highlight the potential for significant head injury in scenarios lacking malicious intent or due to improper handling of infants.
Previous studies have raised concerns about the traditional diagnostic criteria for SBS [11]. From a biomechanical perspective, the G-forces induced on shaking a baby to create intracranial damage would induce significant spinal cord damage rather than head injuries [12,13]. This inherently makes sense as the infant’s head is the heaviest segment of the infant body, and the weak neck muscles would be unable to control forces acting on the vertebrae and spinal cord. This raises concerns about the role of other forms of trauma, including those that may occur unintentionally, in producing similar intracranial damage. While the autopsy report in this case study reported intramuscular cervical hemorrhages, it is important to note that the cervical hemorrhages aren’t as severe as expected from actual shaking of a baby [12]. It is plausible that an unsupported head while delivering back blows or placing the baby on the table with the head unsupported could have caused the intramuscular cervical hemorrhages given the high G-forces. Our findings suggest that it may be more appropriate to consider other forms of trauma, including those from unintentional mishandling, as contributing factors to head injuries in infants. The classic maximum exertion shaking was shown to produce 9–15 G-forces in prior work [5]. The prior study used an infant model that was 3.18 kg. This was not similar to the size of the 5.08 kg infant model used in this study. Even with the mass discrepancy, this study’s results confirmed prior work showing that maximum exerted shaking of an infant produced approximately 11 G-Forces [4,5]. It is important to clarify, however, that similar acceleration values across studies using different infant model masses do not imply that acceleration remains constant across all body sizes during shaking. When the same amount of effort is applied to heavier infants, the resulting accelerations would generally be lower, not equal. Moreover, while this study focused on acceleration values, the force experienced upon impact (e.g., when the head strikes a surface) is directly proportional to mass. For a given deceleration, a more massive head would result in a proportionally greater impact force. Therefore, a real infant, especially one heavier than the model used in this study, may experience substantially greater forces during head impact, even if acceleration magnitudes are similar. This distinction is important when interpreting biomechanical outcomes across different infant sizes and highlights the need for future studies using size-scaled models and force measurements. With that in mind, the size of this model was smaller than the reported case. Since force is directly influenced by the mass of the object, a larger infant could experience even greater forces when placed on a table without head support. Furthermore, it is important to consider the improper handling of an infant as the head accelerations during the transfer of an infant to a table with the unsupported head resulted in 316% higher G-forces than maximum exertion of shaking an infant.
It is important to acknowledge that Shaken Baby Syndrome (SBS) injuries are multifactorial and often involve a combination of biomechanical forces beyond linear accelerations alone. Previous research has emphasized that rotational (angular) accelerations significantly contribute to the characteristic injuries observed in SBS, including subdural hemorrhage, retinal hemorrhage, and cerebral edema. Furthermore, spinal injuries or cervical trauma may occur due to the unique biomechanical interactions of shaking motions. The current study specifically quantified linear accelerations during certain non-recommended handling scenarios, but did not measure rotational accelerations or spinal forces. Therefore, while the high linear G-forces reported in this study demonstrate the potential for injury from isolated impacts, comprehensive diagnosis of SBS should consider all biomechanical components and associated clinical diagnostic criteria. As such, the current findings demonstrate that improper handling can produce head accelerations greater than those observed during maximum shaking, this study does not establish a direct causal relationship between these accelerations and specific injuries such as subdural or retinal hemorrhages. Injury determination requires consideration of tissue-level responses, injury thresholds, and validated models, none of which were within the scope of this preliminary investigation. Therefore, our results should be interpreted as highlighting the potential for elevated head loading, rather than as definitive evidence of traumatic injury from improper handling alone.
Several methodological limitations must be recognized in interpreting these findings. First, this study utilized a single silicone infant surrogate, which inherently does not fully replicate the biomechanical properties of human infants. Silicone models differ significantly in tissue elasticity, skull compliance, cerebrospinal fluid distribution, and internal anatomical complexity compared to a living infant. Such discrepancies may influence the measured head accelerations and limit direct clinical generalizations. The selection of this surrogate was based on ethical considerations prohibiting the use of live infants and practical constraints associated with more sophisticated anthropomorphic test devices (ATDs). Second, the small sample size of only two participants without prior infant-handling experience, further limits the generalizability of our results and introduces potential inter-operator variability. Although participants were trained briefly to standardize handling, individual differences in technique likely persisted. Third, although the Head Injury Criterion (HIC) is a widely accepted metric for estimating head injury risk in adult populations, this study did not compute HIC values due to the sampling frequency limitations of the inertial measurement unit (200 Hz). Accurate HIC calculation requires high-resolution acceleration data—typically ≥1000 Hz—to capture the rapid dynamics of head impacts. Future investigations should employ higher-frequency data acquisition systems to enable valid computation of HIC and support the development of age-specific injury risk curves for infants. Fourth, while this study reports peak linear accelerations as a first-order estimate of head loading, we acknowledge that peak acceleration alone is an imperfect predictor of injury. More advanced biomechanical models, including stress–strain analyses and finite element simulations, offer greater insight into tissue-level deformations and injury mechanisms, particularly for bridging veins and subdural spaces. Future studies should incorporate such models to improve understanding of how mechanical loading translates to specific intracranial injuries. Our current findings highlight relative differences in mechanical input across scenarios but do not represent a comprehensive biomechanical injury prediction framework. Furthermore, future studies should consider using more physiologically accurate ATDs, computational models validated against pediatric biomechanical data, and larger participant pools with varied infant-handling expertise to enhance validity and applicability of results.
While the medical reports concluded that this was a case of infant homicide, it may be important to understand that blunt trauma may also stem from improper handling which can result in accidental trauma and high amounts of head acceleration in infants. Consideration of the entire medical incident is important to help determine whether the blunt trauma was accidental or intention. In this case study, the father’s account of the incident suggests unintentional harm may have occurred. This father found his infant in medical distress and possibly choking. The emotional stress and trauma of this on the parent could have caused him to handle his infant with the dire intention of reviving and seeking medical attention. The mechanical data from this study demonstrated that such scenarios with no malicious intent can still pose a severe risk to an infant. This study highlights the importance of supporting an infant’s head during handling to prevent accidental injury, and further highlights that SBS warrants additional context of the situation before ascribing malintent on a caregiver.
5. Conclusions
This study offers insights into the biomechanical forces acting on an infant’s head during common caregiving scenarios, specifically when the head is not supported. The peak head accelerations observed during table placement without head support were significantly higher than those during maximum effort shaking, indicating that even non-malicious actions from improper handling can result in substantial g-forces. These findings emphasize the need for caregivers to be aware in supporting an infant’s head to prevent accidental injury. Additionally, our results highlight the importance of considering non-abusive causes when diagnosing SBS and suggest that further research is needed to explore the range of forces involved in everyday caregiving scenarios.
Author Contributions
Conceptualization, J.S.L.-C. and K.L.H.; Methodology, J.S.L.-C. and K.L.H.; Software, J.S.L.-C.; Validation, J.S.L.-C., L.T.W. and K.L.H.; Formal Analysis, J.S.L.-C.; Investigation, J.S.L.-C. and L.T.W.; Resources, J.S.L.-C.; Data Curation, J.S.L.-C. and L.T.W.; Writing—Original Draft Preparation, J.S.L.-C.; Writing—Review & Editing, J.S.L.-C., L.T.W. and K.L.H.; Visualization, J.S.L.-C. and K.L.H.; Supervision, J.S.L.-C.; Project Administration, J.S.L.-C. and K.L.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are not publicly available.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Shanahan, M.E.; Zolotor, A.J.; Parrish, J.W.; Barr, R.G.; Runyan, D.K. National, regional, and state abusive head trauma: Application of the CDC algorithm. Pediatrics 2013, 132, e1546–e1553. [Google Scholar] [CrossRef] [PubMed]
- Lopes, N.R.L.; Eisenstein, E.; Williams, L.C.A. Abusive head trauma in children: A literature review. J. Pediatr. (Rio. J.). 2013, 89, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Gabaeff, S.C. Challenging the pathophysiologic connection between subdural hematoma, retinal hemorrhage and shaken baby syndrome. West. J. Emerg. Med. 2011, 12, 144. [Google Scholar] [PubMed]
- Duhaime, A.-C.; Gennarelli, T.A.; Thibault, L.E.; Bruce, D.A.; Margulies, S.S.; Wiser, R. The shaken baby syndrome: A clinical, pathological, and biomechanical study. J. Neurosurg. 1987, 66, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Glowinski, S.; Majdanik, S.; Glowinska, A.; Majdanik, E. Trauma in a shaken infant? A case study. Aggress. Violent Behav. 2021, 56, 101515. [Google Scholar] [CrossRef]
- Stray-Pedersen, A.; Strisland, F.; Rognum, T.O.; Schiks, L.A.H.; Loeve, A.J. Violent infant surrogate shaking: Continuous high-magnitude centripetal force and abrupt shift in tangential acceleration may explain high risk of subdural hemorrhage. Neurotrauma Rep. 2021, 2, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, B. Head injury—Abuse or accident? Arch. Dis. Child. 1997, 76, 393–397. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lloyd, J.; Willey, E.N.; Galaznik, J.G.; Lee, W.; Luttner, S. Biomechanical evaluation of head kinematics during infant shaking versus pediatric activities of daily living. J. Forensic Biomech. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Iqbal O’Meara, A.M.; Sequeira, J.; Miller Ferguson, N. Advances and future directions of diagnosis and management of pediatric abusive head trauma: A review of the literature. Front. Neurol. 2020, 11, 118. [Google Scholar] [CrossRef] [PubMed]
- Pfister, B.J.; Chickola, L.; Smith, D.H. Head motions while riding roller coasters: Implications for brain injury. Am. J. Forensic Med. Pathol. 2009, 30, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Lynøe, N.; Elinder, G.; Hallberg, B.; Rosén, M.; Sundgren, P.; Eriksson, A. Insufficient evidence for ‘shaken baby syndrome’—A systematic review. Acta Paediatr. 2017, 106, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- Bandak, F.A. Shaken baby syndrome: A biomechanics analysis of injury mechanisms. Forensic Sci. Int. 2005, 151, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Davison, M.A.; Button, K.D.; Benzel, E.C.; Weaver, B.T.; Rundell, S.A. A biomechanical assessment of shaken baby syndrome: What about the spine? World Neurosurg. 2022, 163, e223–e229. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).