Post-COVID-19 Era Forensics: Hospital Autopsies, New Methodologies, and Medicolegal Perspectives
Abstract
1. Introduction
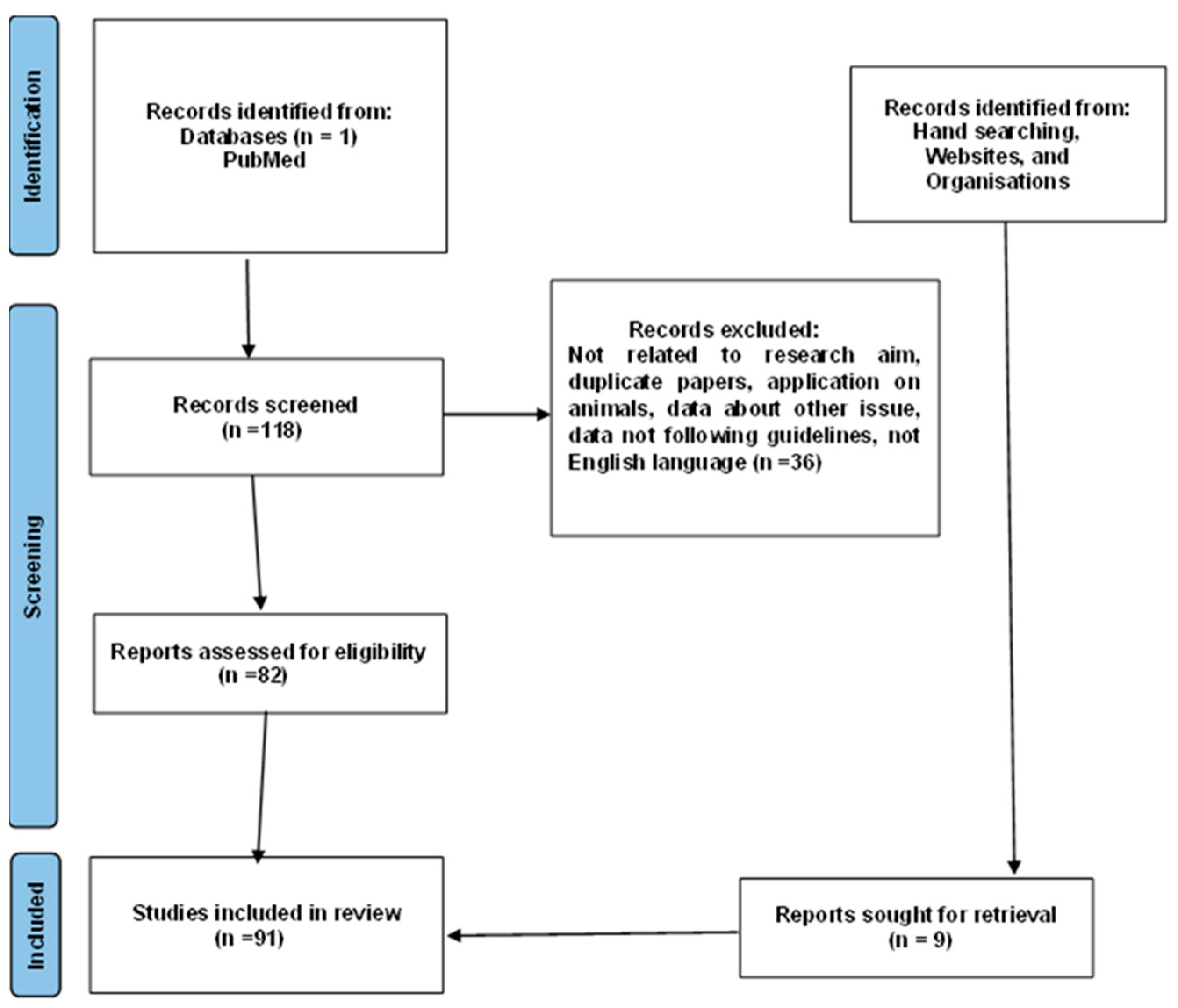
2. Materials and Methods
3. Results
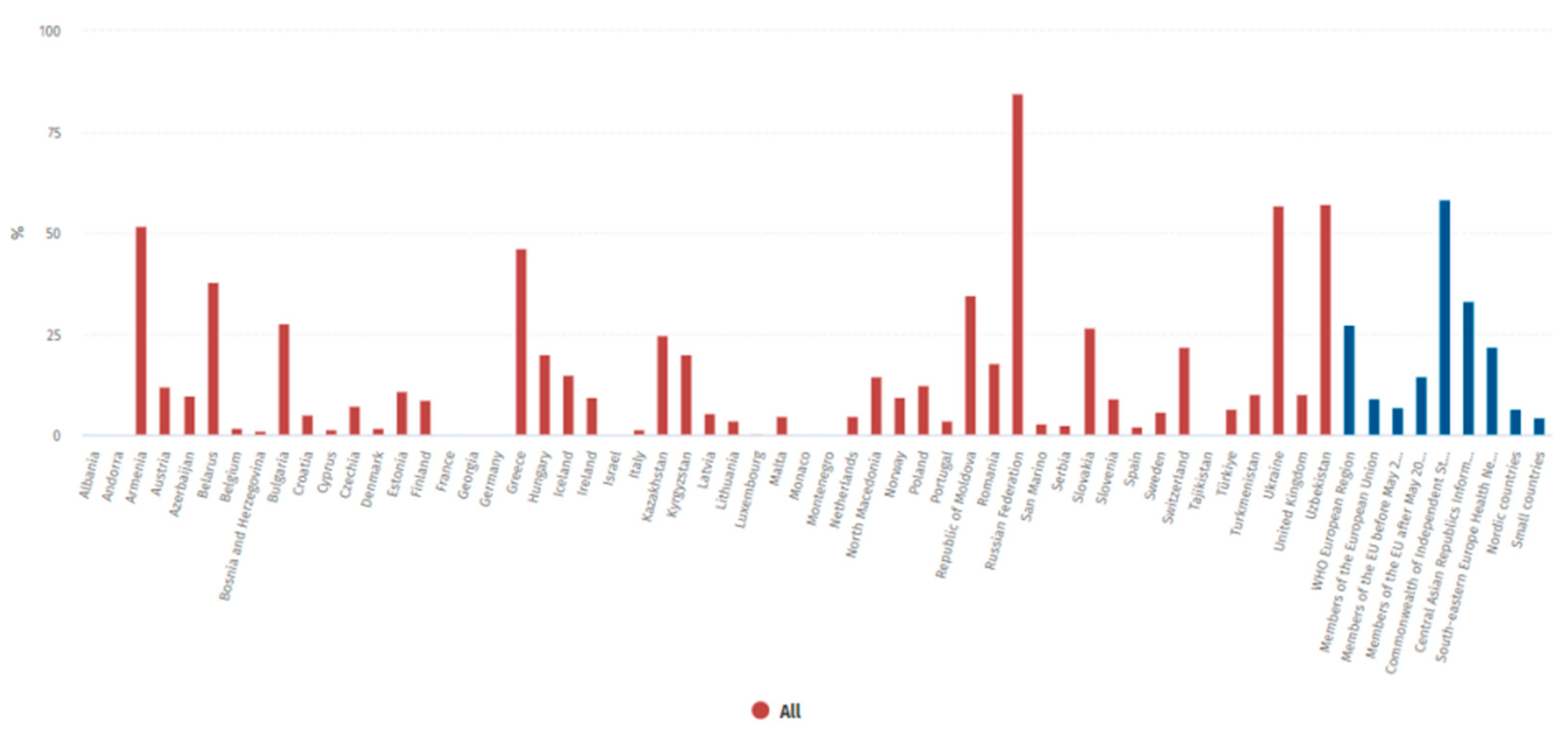
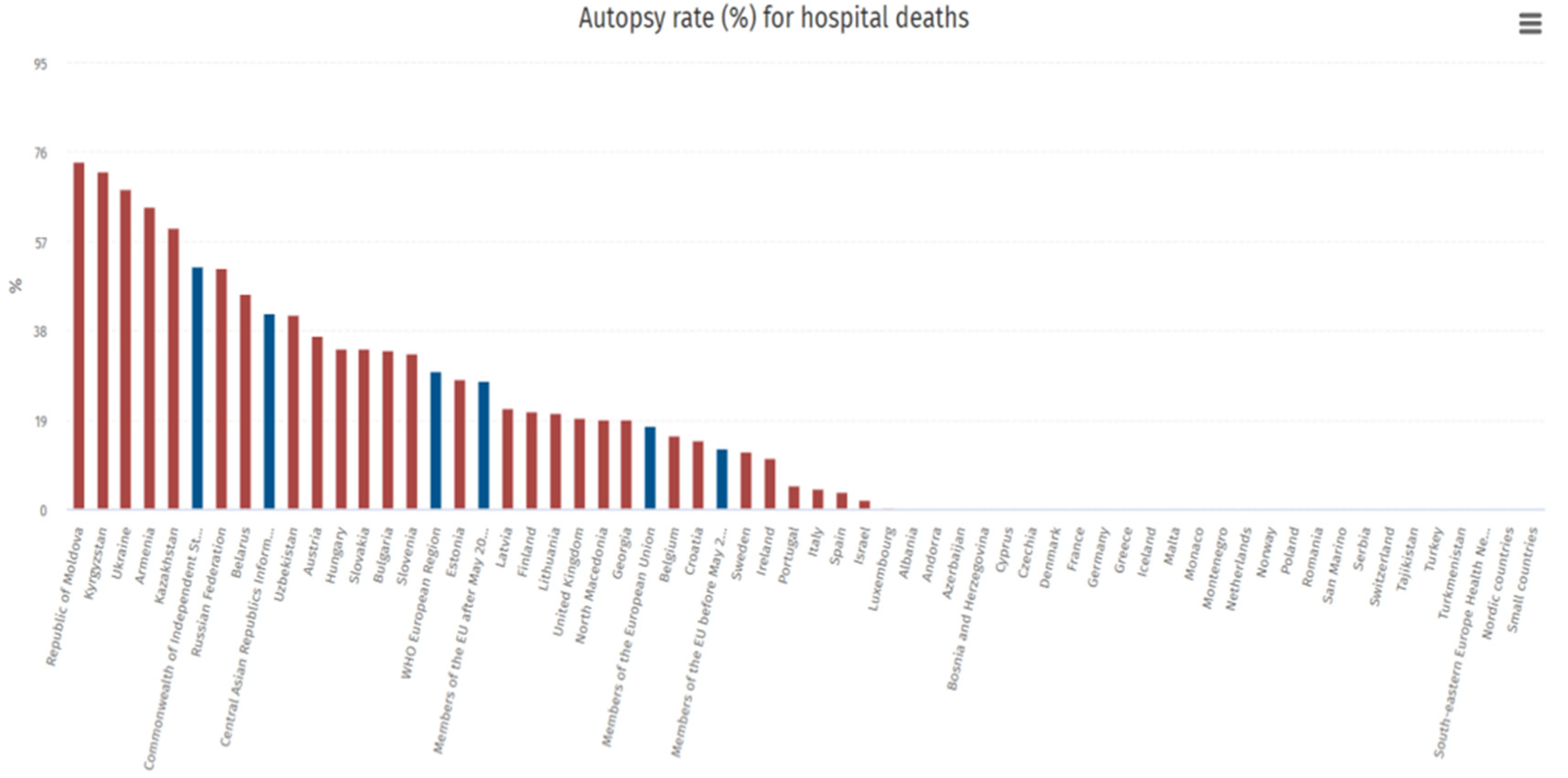
3.1. Autopsy Rates Are Constantly Declining in Western Countries
3.2. The Issue of Family Consent: Differences Between Countries
3.3. COVID-19 and Autopsies in Italy
- Judicial (local jurisdiction);
- Hospitals (organization by company);
- Checks on deceased subjects with no healthcare coverage (local health authority).
3.4. Forensic Doctors and Hospital Autopsies: Europe vs. USA
| Country | Pathology | Forensic Pathology |
|---|---|---|
| Accreditation Council for Graduate Medical Education (United States) [70] | A minimum of 50 autopsy cases including exposure to forensic, pediatric, perinatal, and stillborn autopsies. | A minimum of 200 and no more than 300 autopsy cases |
| Royal College of Physicians and Surgeons of Canada [71] | No minimum number of autopsy cases. Accredited programs must have a volume and diversity of work available for teaching that must be adequate to meet the educational objectives of the program, with an adequate number of adult, pediatric, and forensic autopsies. | A minimum of 100 completed medicolegal post-mortem examinations including infant, children, and adult, with a wide range of natural and unnatural deaths, and 30% of the cases must be of a complex nature (homicides and criminally suspicious deaths) |
| The Royal College of Pathologists (United Kingdom) [72] | Stages A and B (2 years of basic histopathology training) requires 20 adult autopsy cases each year, with a total of two perinatal/pediatric autopsies. | Stage C (minimum of 30 months) requires 80 autopsy cases each year; Stage D (minimum of 6 months) requires 50 autopsy cases; also required to complete 3 months of pediatric pathology and 3 months of neuropathology |
| European Society of Pathology (E.S.P.) [1] | The autopsy should be coordinated by a specialist with proven experience and findings should only be performed by specialists in pathological anatomy or forensic pathology/forensics or possibly by specialists in training under direct supervision. Finally, to ensure adequate expertise, there is a minimum number of annual autopsies per individual team member, equal to at least 50 diagnostic findings and annual judicial autopsies. | The autopsy should be coordinated by a specialist with proven experience and findings should only be performed by specialists in pathological anatomy or forensic pathology/forensics or possibly by specialists in training under direct supervision. Finally, to ensure adequate expertise, there is a minimum number of annual autopsies per individual team member, equal to at least 50 diagnostic findings and annual judicial autopsies |
3.5. What Can Get in the Way of Hospital Autopsies? Does Family Consent Have Any Bearing?
- Infants who died suddenly within one year of life without apparent cause.
- Fetuses who died after the twenty-fifth week of gestation, also without apparent cause.
3.6. If Not Legal, What Reasons for Declining Autopsies? And What of the New Technologies?
3.7. COVID-19 and the Reasserted Value of Hospital Autopsies
4. Discussion
What Can Be Envisioned?
5. Conclusions
6. Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Alfsen, G.C.; Gulczyński, J.; Kholová, I.; Latten, B.; Martinez, J.; Metzger, M.; Michaud, K.; Pontinha, C.M.; Rakislova, N.; Rotman, S.; et al. Code of Practice for Medical Autopsies: A Minimum Standard Position Paper for Pathology Departments Performing Medical (Hospital) Autopsies in Adults. Virchows Arch. 2022, 480, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Autopsy in the 21st Century: Best Practices and Future Directions [PDF] [7totf7fq9r40]. Available online: https://vdoc.pub/documents/autopsy-in-the-21st-century-best-practices-and-future-directions-7totf7fq9r40 (accessed on 13 December 2023).
- Zinserling, V. Infectious Pathology of the Respiratory Tract; Springer International Publishing: Cham, Switzerland, 2021; ISBN 978-3-030-66324-7. [Google Scholar]
- Napoletano, G.; Putrino, A.; Marinelli, E.; Zaami, S.; De Paola, L. Dental Identification System in Public Health: Innovations and Ethical Challenges: A Narrative Review. Healthcare 2024, 12, 1828. [Google Scholar] [CrossRef] [PubMed]
- Volonnino, G.; Paola, L.D.; Spadazzi, F.; Serri, F.; Ottaviani, M.; Zamponi, M.V.; Arcangeli, M.; Russa, R.L. Artificial intelligence and Forensic Medicine: The state of the art and future perspectives. Clin. Ter. 2024, 175, 193–202. [Google Scholar] [CrossRef] [PubMed]
- King, L.S.; Meehan, M.C. A History of the Autopsy. A Review. Am. J. Pathol. 1973, 73, 514–544. [Google Scholar]
- Cecchetto, G.; Bajanowski, T.; Cecchi, R.; Favretto, D.; Grabherr, S.; Ishikawa, T.; Kondo, T.; Montisci, M.; Pfeiffer, H.; Bonati, M.R.; et al. Back to the Future—Part 1. The Medico-Legal Autopsy from Ancient Civilization to the Post-Genomic Era. Int. J. Leg. Med. 2017, 131, 1069–1083. [Google Scholar] [CrossRef]
- Sakellariou, S.; Patsouris, E. Pathology in Greece. Pathologe 2015, 36 (Suppl. 2), 158–161. [Google Scholar] [CrossRef]
- Zampieri, F.; Zanatta, A.; Thiene, G. An Etymological “Autopsy” of Morgagni’s Title: De Sedibus et Causis Morborum per Anatomen Indagatis (1761). Hum. Pathol. 2014, 45, 12–16. [Google Scholar] [CrossRef]
- Participation, E. Anatomy Act. 1984. Available online: https://www.legislation.gov.uk/ukpga/1984/14/contents (accessed on 25 September 2024).
- Riggs, C. An Autopsic Art: Drawings of ‘Dr Granville’s Mummy’ in the Royal Society Archives. Notes Rec. R. Soc. J. Hist. Sci. 2016, 70, 107–133. [Google Scholar] [CrossRef]
- A Trusted Partner in Patient Care|The Joint Commission. Available online: https://www.jointcommission.org/ (accessed on 12 December 2023).
- Gitto, L.; Serinelli, S.; Busardò, F.P.; Panebianco, V.; Bolino, G.; Maiese, A. Can Post-Mortem Computed Tomography Be Considered an Alternative for Autopsy in Deaths Due to Hemopericardium? J. Geriatr. Cardiol. 2014, 11, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Hamza, A. Declining Rate of Autopsies: Implications for Anatomic Pathology Residents. Autops. Case Rep. 2017, 7, 1–2. [Google Scholar] [CrossRef]
- Rosendahl, A.; Mjörnheim, B.; Eriksson, L.C. Autopsies and Quality of Cause of Death Diagnoses. SAGE Open Med. 2021, 9, 20503121211037169. [Google Scholar] [CrossRef]
- Loughrey, M.B.; McCluggage, W.G.; Toner, P.G. The Declining Autopsy Rate and Clinicians’ Attitudes. Ulst. Med. J. 2000, 69, 83–89. [Google Scholar]
- WHO European Health Information at Your Fingertips. Available online: https://gateway.euro.who.int/en/indicators/hfa_544-6400-autopsy-rate-for-hospital-deaths/ (accessed on 13 December 2023).
- Chatelain, D.; Brevet, M.; Guernou, M.; Manaouil, C.; Leclercq, F.; Bruniau, A.; Cordonnier, C.; Sevestre, H. Adult autopsies in a French university hospital (CHU Amiens) for the period 1975–2005. Ann. Pathol. 2007, 27, 269–283. [Google Scholar] [CrossRef]
- Dell’Aquila, M.; Vetrugno, G.; Grassi, S.; Stigliano, E.; Oliva, A.; Rindi, G.; Arena, V. Postmodernism and the Decline of the Clinical Autopsy. Virchows Arch. 2021, 479, 861–863. [Google Scholar] [CrossRef] [PubMed]
- LOI No 94-653 Du 29 Juillet 1994 Relative Au Respect Du Corps Humain (1); 1994. Available online: https://affairesjuridiques.aphp.fr/textes/loi-n-94-653-du-29-juillet-1994-relative-au-respect-du-corps-humain/ (accessed on 25 October 2024).
- Krankenhausstrukturgesetz (KHSG). Available online: https://www.bundesgesundheitsministerium.de/service/gesetze-und-verordnungen/detail/krankenhausstrukturgesetz-khsg.html (accessed on 1 February 2025).
- Participation, E. Human Tissue Act. 2004. Available online: https://www.legislation.gov.uk/ukpga/2004/30/contents (accessed on 1 February 2025).
- BOE-A-1980-13662 Ley 29/1980, de 21 de Junio, de Autopsias Clínicas. Available online: https://www.boe.es/buscar/act.php?id=BOE-A-1980-13662 (accessed on 1 February 2025).
- Connolly, A.J.; Finkbeiner, W.E.; Ursell, P.C.; Davis, R.L. Legal, Social, and Ethical Issues. In Autopsy Pathology: A Manual and Atlas; Elsevier: Amsterdam, The Netherlands, 2016; pp. 15–23. [Google Scholar] [CrossRef]
- Tamsen, F.; Alafuzoff, I. When Is a Postmortem Examination Carried out? A Retrospective Analysis of All Swedish Deaths 1999–2018. Virchows Arch. 2023, 482, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.U.; Khan, M.S.; Navar, A.M.; Warraich, H.J.; Singh, J.; Cainzos-Achirica, M.; Michos, E.D. The Changing Profile of Autopsies in Cardiovascular Deaths in the United States, 2003–2018. Am. J. Cardiol. 2021, 140, 150–151. [Google Scholar] [CrossRef]
- Moretti, M.; Malhotra, A.; Visonà, S.D.; Finley, S.J.; Osculati, A.M.M.; Javan, G.T. The Roles of Medical Examiners in the COVID-19 Era: A Comparison between the United States and Italy. Forensic Sci. Med. Pathol. 2021, 17, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Basso, C.; Stone, J.R. Autopsy in the Era of Advanced Cardiovascular Imaging. Eur. Heart J. 2022, 43, 2461–2468. [Google Scholar] [CrossRef]
- Kircher, T.; Nelson, J.; Burdo, H. The Autopsy as a Measure of Accuracy of the Death Certificate. N. Engl. J. Med. 1985, 313, 1263–1269. [Google Scholar] [CrossRef]
- Landefeld, C.S.; Chren, M.M.; Myers, A.; Geller, R.; Robbins, S.; Goldman, L. Diagnostic Yield of the Autopsy in a University Hospital and a Community Hospital. N. Engl. J. Med. 1988, 318, 1249–1254. [Google Scholar] [CrossRef]
- Scarl, R.; Parkinson, B.; Arole, V.; Hardy, T.; Allenby, P. The Hospital Autopsy: The Importance in Keeping Autopsy an Option. Autops. Case Rep. 2022, 12, e2021333. [Google Scholar] [CrossRef]
- Goldman, L. Autopsy 2018: Still Necessary, Even If Occasionally Not Sufficient. Circulation 2018, 137, 2686–2688. [Google Scholar] [CrossRef] [PubMed]
- Sapino, A.; Facchetti, F.; Bonoldi, E.; Gianatti, A.; Barbareschi, M. Società Italiana di Anatomia Patologica e Citologia—SIAPEC The Autopsy Debate during the COVID-19 Emergency: The Italian Experience. Virchows Arch. 2020, 476, 821–823. [Google Scholar] [CrossRef] [PubMed]
- Download di: Circolare del Ministero della Salute n. 11392 del 1°. Aprile 2020. Available online: https://sso.agc.gov.sg/SL/HSA2020-S835-2023?DocDate=20231214 (accessed on 13 December 2023).
- Marozzi, F. Esami autoptici COVID-19: La posizione ufficiale di SIMLA e del GIPF. Società Italiana di Medicina Legale e delle Assicurazioni. 2020. Available online: https://www.simlaweb.it/esami-autoptici-covid19-la-posizione-ufficiale-di-simla-e-del-gipf/ (accessed on 13 December 2023).
- Emergency Circular n. 15280. Italian Ministry of Health 2nd May 2020. Available online: https://portale.fnomceo.it/wp-content/uploads/2020/05/Copia_DocPrincipale_Aggiornamento_Circolare_serv_funebri_28_5_2020.pdf (accessed on 26 September 2024).
- Circolare Ministero della Salute n. 18457 Del 28/05/2020. Available online: https://www.funerali.org/wp-content/uploads/File/Circolari/cs02005280.htm (accessed on 26 September 2024).
- Circolare (Ministero della Salute) 11-01-2021, n. 818|Indicenormativa.It. Available online: https://www.indicenormativa.it/norma/urn%3Anir%3Aministero.salute%3Acircolare%3A2021-01-11%3B818 (accessed on 13 December 2023).
- Riefolo, M.; Ambrosi, F.; De Palma, A.; Gallo, C.; Damiani, S. Management of Post-Mortem Examination in SARS-CoV-19 Infections. Pathologica 2023, 115, 257–262. [Google Scholar] [CrossRef]
- Hanley, B.; Lucas, S.B.; Youd, E.; Swift, B.; Osborn, M. Autopsy in Suspected COVID-19 Cases. J. Clin. Pathol. 2020, 73, 239–242. [Google Scholar] [CrossRef]
- Volonnino, G.; Spadazzi, F.; De Paola, L.; Arcangeli, M.; Pascale, N.; Frati, P.; La Russa, R. Healthcare Workers: Heroes or Victims? Context of the Western World and Proposals to Prevent Violence. Healthcare 2024, 12, 708. [Google Scholar] [CrossRef]
- Marinelli, S.; Basile, G.; Paola, L.D.E.; Napoletano, G.; Zaami, S. Consequences of COVID-19 Restrictions on Adolescent Mental Health and Drug Abuse Dynamics. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 836–851. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.-P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schröder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef]
- Maiese, A.; Manetti, A.C.; La Russa, R.; Di Paolo, M.; Turillazzi, E.; Frati, P.; Fineschi, V. Autopsy Findings in COVID-19-Related Deaths: A Literature Review. Forensic Sci. Med. Pathol. 2021, 17, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Macor, P.; Durigutto, P.; Mangogna, A.; Bussani, R.; De Maso, L.; D’Errico, S.; Zanon, M.; Pozzi, N.; Meroni, P.L.; Tedesco, F. Multiple-Organ Complement Deposition on Vascular Endothelium in COVID-19 Patients. Biomedicines 2021, 9, 1003. [Google Scholar] [CrossRef]
- Frisoni, P.; Neri, M.; D’Errico, S.; Alfieri, L.; Bonuccelli, D.; Cingolani, M.; Di Paolo, M.; Gaudio, R.M.; Lestani, M.; Marti, M.; et al. Cytokine Storm and Histopathological Findings in 60 Cases of COVID-19-Related Death: From Viral Load Research to Immunohistochemical Quantification of Major Players IL-1β, IL-6, IL-15 and TNF-α. Forensic Sci. Med. Pathol. 2022, 18, 4–19. [Google Scholar] [CrossRef]
- CDC Healthcare Workers. Available online: https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html (accessed on 20 November 2024).
- Infection Prevention and Control for the Safe Management of a Dead Body in the Context of COVID-19: Interim Guidance. Available online: https://www.who.int/publications-detail-redirect/infection-prevention-and-control-for-the-safe-management-of-a-dead-body-in-the-context-of-covid-19-interim-guidance (accessed on 13 December 2023).
- Hoyert, D.L. The Changing Profile of Autopsied Deaths in the United States, 1972–2007; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Washington, DC, USA, 2011; pp. 1–8. [Google Scholar]
- McGuire, A.R.; DeJoseph, M.E.; Gill, J.R. An Approach to Iatrogenic Deaths. Forensic Sci. Med. Pathol. 2016, 12, 68–80. [Google Scholar] [CrossRef]
- Zanon, M.; Valentinuz, E.; Montanaro, M.; Radaelli, D.; Manfredi, A.; Bonuccelli, D.; Martelloni, M.; D’Errico, S. Is Hospital Autopsy Auditing Suitable for Clinical Risk Manage Ment? Actualities and Perspectives of Auditing in the Autopsy Room Following Italian Law 24/2017 on Patient Safety. Curr. Pharm. Biotechnol. 2021, 22, 1964–1970. [Google Scholar] [CrossRef] [PubMed]
- Rueckert, J. Elimination of the Autopsy Requirement by CMS. N. Engl. J. Med. 2020, 382, 683–684. [Google Scholar] [CrossRef]
- Lee, L.A.; Stephens, L.S.; Fligner, C.L.; Posner, K.L.; Cheney, F.W.; Caplan, R.A.; Domino, K.B. Autopsy Utilization in Medicolegal Defense of Anesthesiologists. Anesthesiology 2011, 115, 713–717. [Google Scholar] [CrossRef]
- Gartland, R.M.; Myers, L.C.; Iorgulescu, J.B.; Nguyen, A.T.; Yu-Moe, C.W.; Falcone, B.; Mitchell, R.; Kachalia, A.; Mort, E. Body of Evidence: Do Autopsy Findings Impact Medical Malpractice Claim Outcomes? J. Patient Saf. 2021, 17, 576–582. [Google Scholar] [CrossRef]
- Ondruschka, B.; Baier, C.; Dreßler, J.; Höch, A.; Bernhard, M.; Kleber, C.; Buschmann, C. Additional emergency medical measures in trauma-associated cardiac arrest. Anaesthesist 2017, 66, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Beardmore, S.; Adeley, J.; Brookes, A.; Robinson, C.; Davendralingam, N.; Joseph, J.; McManoman, B.; Morgan, B. Impact of Changing from Autopsy to Post-Mortem CT in an Entire HM Coroner Region Due to a Shortage of Available Pathologists. Clin. Radiol. 2023, 78, 797–803. [Google Scholar] [CrossRef]
- Frati, P.; La Russa, R.; Duse, M. Editorial: Pediatric Specificities of Medical Liability: Improvement Measures in Pediatric Settings. Front. Pediatr. 2021, 9, 667020. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, M.C.; Reed, R.C. Pathologist Effort in the Performance of Fetal, Perinatal, and Pediatric Autopsies: A Survey of Practice. Arch. Pathol. Lab. Med. 2017, 141, 209–214. [Google Scholar] [CrossRef]
- Désilets, V.; Oligny, L.L.; Genetics Committee of the Society of Obstetricians and Gynaecology Canada; Family Physicians Advisory Committee. Medico–Legal Committee of the SOGC Fetal and Perinatal Autopsy in Prenatally Diagnosed Fetal Abnormalities with Normal Karyotype. J. Obstet. Gynaecol. Can. 2011, 33, 1047–1057. [Google Scholar] [CrossRef]
- Chowaniec, C.; Chowaniec, M.; Nowak, A.; Kobek, M. Sudden cardiac death—difficulties in passing a medico-legal opinion for a civil or insurance claim. Arch. Med. Sadowej Kryminol. 2007, 57, 72–77. [Google Scholar] [PubMed]
- Michaud, K.; Mangin, P.; Elger, B.S. Genetic Analysis of Sudden Cardiac Death Victims: A Survey of Current Forensic Autopsy Practices. Int. J. Leg. Med. 2011, 125, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Elger, B.; Michaud, K.; Mangin, P. When Information Can Save Lives: The Duty to Warn Relatives about Sudden Cardiac Death and Environmental Risks. Hastings Cent. Rep. 2010, 40, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Baiardi, S.; Rossi, M.; Capellari, S.; Parchi, P. Recent Advances in the Histo-Molecular Pathology of Human Prion Disease. Brain Pathol. 2019, 29, 278–300. [Google Scholar] [CrossRef] [PubMed]
- Rapkiewicz, A.V.; Mai, X.; Carsons, S.E.; Pittaluga, S.; Kleiner, D.E.; Berger, J.S.; Thomas, S.; Adler, N.M.; Charytan, D.M.; Gasmi, B.; et al. Megakaryocytes and Platelet-Fibrin Thrombi Characterize Multi-Organ Thrombosis at Autopsy in COVID-19: A Case Series. eClinicalMedicine 2020, 24, 100434. [Google Scholar] [CrossRef]
- Farshad, S.; Kanaan, C.; Savedchuk, S.; Karmo, D.S.; Halalau, A.; Swami, A. Systemic Lupus Erythematosus (SLE) with Acute Nephritis, Antineutrophil Cytoplasmic Antibody- (ANCA-) Associated Vasculitis, and Thrombotic Thrombocytopenic Purpura (TTP): A Rare Case Report with Literature Review. Case Rep. Rheumatol. 2019, 2019, 8750306. [Google Scholar] [CrossRef]
- Hammer, U.; Blaas, V.; Büttner, A.; Philipp, M. Autopsies for anatomical teaching and training in clinical forensic medicine. Chirurg 2015, 86, 1128–1131. [Google Scholar] [CrossRef]
- Hamilton, L.E. Teaching the Forensic Autopsy. Acad. Forensic Pathol. 2015, 5, 201–210. [Google Scholar] [CrossRef]
- Khalaf, Z.; Hamidpour, S. Adaptations of Pathology Residencies During COVID-19. Mo. Med. 2023, 120, 192–195. [Google Scholar]
- Accreditation Council for Graduate Medical Education. Available online: https://www.acgme.org (accessed on 26 September 2024).
- Royal College of Physicians and Surgeons of Canada. Forensic Pathology Training Experiences. Issued in May 2019. Available online: https://lmp.utoronto.ca/royal-college-physicians-and-surgeons-canada-academic-certification-program (accessed on 26 September 2024).
- Pathologists, T.R.C. of Autopsy Guidelines Series. Available online: https://www.rcpath.org/profession/guidelines/autopsy-guidelines-series.html (accessed on 26 September 2024).
- Schwanda-Burger, S.; Moch, H.; Muntwyler, J.; Salomon, F. Diagnostic Errors in the New Millennium: A Follow-up Autopsy Study. Mod. Pathol. 2012, 25, 777–783. [Google Scholar] [CrossRef]
- Roberts, I.S.D.; Benbow, E.W.; Bisset, R.; Jenkins, J.P.R.; Lee, S.H.; Reid, H.; Jackson, A. Accuracy of Magnetic Resonance Imaging in Determining Cause of Sudden Death in Adults: Comparison with Conventional Autopsy. Histopathology 2003, 42, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Buja, L.M.; Barth, R.F.; Krueger, G.R.; Brodsky, S.V.; Hunter, R.L. The Importance of the Autopsy in Medicine: Perspectives of Pathology Colleagues. Acad. Pathol. 2019, 6, 2374289519834041. [Google Scholar] [CrossRef]
- Maiese, A.; Gitto, L.; De Matteis, A.; Panebianco, V.; Bolino, G. Post Mortem Computed Tomography: Useful or Unnecessary in Gunshot Wounds Deaths? Two Case Reports. Leg. Med. 2014, 16, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Robb, T.J.; Tse, R.; Blenkiron, C. Reviving the Autopsy for Modern Cancer Evolution Research. Cancers 2021, 13, 409. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, A.; Osborn, M.; Nicholas, N. Hospital Autopsy: Endangered or Extinct? J. Clin. Pathol. 2015, 68, 601–604. [Google Scholar] [CrossRef]
- Weber, M.-A. Minimally invasive autopsy: An alternative to conventional autopsy? Radiologe 2009, 49, 397–398. [Google Scholar] [CrossRef] [PubMed]
- Fröhlich, S.; Ryan, O.; Murphy, N.; McCauley, N.; Crotty, T.; Ryan, D. Are Autopsy Findings Still Relevant to the Management of Critically Ill Patients in the Modern Era? Crit. Care Med. 2014, 42, 336–343. [Google Scholar] [CrossRef]
- Blokker, B.M.; Wagensveld, I.M.; Weustink, A.C.; Oosterhuis, J.W.; Hunink, M.G.M. Non-Invasive or Minimally Invasive Autopsy Compared to Conventional Autopsy of Suspected Natural Deaths in Adults: A Systematic Review. Eur. Radiol. 2016, 26, 1159–1179. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Chowdhury, R. Searching Cause of Death through Different Autopsy Methods: A New Initiative. J. Family Med. Prim. Care 2017, 6, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Di Paolo, M.; Maiese, A.; dell’Aquila, M.; Filomena, C.; Turco, S.; Giaconi, C.; Turillazzi, E. Role of Post Mortem CT (PMCT) in High Energy Traumatic Deaths. Clin. Ter. 2020, 171, e490–e500. [Google Scholar] [CrossRef]
- Bailo, P.; Gibelli, F.; Ricci, G.; Sirignano, A. Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 11749. [Google Scholar] [CrossRef] [PubMed]
- Fiksel, J.; Gilbert, B.; Wilson, E.; Kalter, H.; Kante, A.; Akum, A.; Blau, D.; Bassat, Q.; Macicame, I.; Samo Gudo, E.; et al. Correcting for Verbal Autopsy Misclassification Bias in Cause-Specific Mortality Estimates. Am. J. Trop. Med. Hyg. 2023, 108, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Rosen, T.; Safford, M.M.; Sterling, M.R.; Goyal, P.; Patterson, M.; Al Malouf, C.; Ballin, M.; Del Carmen, T.; LoFaso, V.M.; Raik, B.L.; et al. Development of the Verbal Autopsy Instrument for COVID-19 (VAIC). J. Gen. Intern. Med. 2021, 36, 3522–3529. [Google Scholar] [CrossRef]
- Kniep, I.; Lutter, M.; Ron, A.; Edler, C.; Püschel, K.; Ittrich, H.; Heller, M.; Heinemann, A. Postmortem imaging of the lung in cases of COVID-19 deaths. Radiologe 2020, 60, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Kanchan, T.; Saraf, A.; Krishan, K.; Misra, S. The Advantages of Virtopsy during the Covid-19 Pandemic. Med. Leg. J. 2020, 88, 55–56. [Google Scholar] [CrossRef] [PubMed]
- Filograna, L.; Manenti, G.; Ampanozi, G.; Calcagni, A.; Ryan, C.P.; Floris, R.; Thali, M.J. Potentials of Post-Mortem CT Investigations during SARS-COV-2 Pandemic: A Narrative Review. Radiol. Med. 2022, 127, 383–390. [Google Scholar] [CrossRef]
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial Intelligence in the Diagnosis of COVID-19: Challenges and Perspectives. Int. J. Biol. Sci. 2021, 17, 1581–1587. [Google Scholar] [CrossRef] [PubMed]
- Zaeri, N. Artificial Intelligence and Machine Learning Responses to COVID-19 Related Inquiries. J. Med. Eng. Technol. 2023, 47, 301–320. [Google Scholar] [CrossRef]
- Frati, P.; Frati, A.; Salvati, M.; Marinozzi, S.; Frati, R.; Angeletti, L.R.; Piccirilli, M.; Gaudio, E.; Delfini, R. Neuroanatomy and Cadaver Dissection in Italy: History, Medicolegal Issues, and Neurosurgical Perspectives. J. Neurosurg. 2006, 105, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Karch, S.B.; Busardò, F.P.; Vaiano, F.; Portelli, F.; Zaami, S.; Bertol, E. Levamisole Adulterated Cocaine and Pulmonary Vasculitis: Presentation of Two Lethal Cases and Brief Literature Review. Forensic Sci. Int. 2016, 265, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Piersanti, V.; Napoletano, G.; David, M.C.; Umani Ronchi, F.; Marinelli, E.; De Paola, L.; Zaami, S. Sudden Death Due to Butane Abuse—An Overview. J. Forensic Leg. Med. 2024, 103, 102662. [Google Scholar] [CrossRef]
- Baggio, U.; Tortorella, V.; De Paola, L.; Berloco, T.; D’Antonio, G.; Mangiulli, T. A Rare Case of Suicide by Bleach Fatal Ingestion: A Case Report and a Literature Overview. Clin. Ter. 2024, 175, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Sperhake, J.-P. Autopsies of COVID-19 Deceased? Absolutely! Leg. Med. 2020, 47, 101769. [Google Scholar] [CrossRef] [PubMed]
- Scendoni, R.; Cingolani, M. What Do We Know about Pathological Mechanism and Pattern of Lung Injury Related to SARS-CoV-2 Omicron Variant? Diagn. Pathol. 2023, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Hirata, Y.; Iida, S.; Arashiro, T.; Nagasawa, S.; Saitoh, H.; Abe, H.; Ikemura, M.; Makino, Y.; Sawa, R.; Iwase, H.; et al. Impact of the COVID-19 Pandemic on Pathological Autopsy Practices in Japan. Pathol. Int. 2023, 73, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Neto, A.N.; Monteiro, R.A.A.; da Silva, L.F.F.; Malheiros, D.M.A.C.; de Oliveira, E.P.; Theodoro-Filho, J.; Pinho, J.R.R.; Gomes-Gouvêa, M.S.; Salles, A.P.M.; de Oliveira, I.R.S.; et al. Pulmonary and Systemic Involvement in COVID-19 Patients Assessed with Ultrasound-Guided Minimally Invasive Autopsy. Histopathology 2020, 77, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Benson, P.V.; Litovsky, S.H.; Steyn, A.J.C.; Margaroli, C.; Iriabho, E.; Anderson, P.G. Use of Telepathology to Facilitate COVID-19 Research and Education through an Online COVID-19 Autopsy Biorepository. J. Pathol. Inform. 2021, 12, 48. [Google Scholar] [CrossRef] [PubMed]
- Gareev, I.; Gallyametdinov, A.; Beylerli, O.; Valitov, E.; Alyshov, A.; Pavlov, V.; Izmailov, A.; Zhao, S. The opportunities and challenges of telemedicine during COVID-19 pandemic. Front. Biosci. (Elite Ed.) 2021, 13, 291–298. [Google Scholar] [CrossRef]
- Vidua, R.K.; Duskova, I.; Bhargava, D.C.; Chouksey, V.K.; Pramanik, P. Dead Body Management amidst Global Pandemic of Covid-19. Med. Leg. J. 2020, 88, 80–83. [Google Scholar] [CrossRef]
- De-Giorgio, F.; Grassi, V.M.; Bergamin, E.; Cina, A.; Del Nonno, F.; Colombo, D.; Nardacci, R.; Falasca, L.; Conte, C.; d’Aloja, E.; et al. Dying “from” or “with” COVID-19 during the Pandemic: Medico-Legal Issues According to a Population Perspective. Int. J. Environ. Res. Public Health 2021, 18, 8851. [Google Scholar] [CrossRef] [PubMed]
- Aquila, I.; Ricci, P.; Bonetta, C.F.; Sacco, M.A.; Longhini, F.; Torti, C.; Mazzitelli, M.; Garofalo, E.; Bruni, A.; Trecarichi, E.M.; et al. Analysis of the Persistence Time of the SARS-CoV-2 Virus in the Cadaver and the Risk of Passing Infection to Autopsy Staff. Med. Leg. J. 2021, 89, 40–53. [Google Scholar] [CrossRef]
- Parekh, U.; Chariot, P.; Dang, C.; Stray-Pedersen, A.; Druid, H.; Sajantila, A. A Roadmap to the Safe Practice of Forensic Medicine in the COVID-19 Pandemic. J. Forensic Leg. Med. 2020, 76, 102036. [Google Scholar] [CrossRef] [PubMed]
- Edler, C.; Schröder, A.S.; Aepfelbacher, M.; Fitzek, A.; Heinemann, A.; Heinrich, F.; Klein, A.; Langenwalder, F.; Lütgehetmann, M.; Meißner, K.; et al. Dying with SARS-CoV-2 Infection-an Autopsy Study of the First Consecutive 80 Cases in Hamburg, Germany. Int. J. Leg. Med. 2020, 134, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Geller, R.L.; Aungst, J.L.; Newton-Levinson, A.; Smith, G.P.; Mosunjac, M.B.; Mosunjac, M.I.; Cunningham, C.S.; Gowitt, G.T. Is It COVID-19? The Value of Medicolegal Autopsies during the First Year of the COVID-19 Pandemic. Forensic Sci. Int. 2022, 330, 111106. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.S.; Dmetrichuk, J.M.; Kim, P.; Pollanen, M.S. Postmortem Radiologic and Pathologic Findings in COVID-19: The Toronto Experience with Pre-Hospitalization Deaths in the Community. Forensic Sci. Int. 2021, 322, 110755. [Google Scholar] [CrossRef]
- Waidhauser, J.; Martin, B.; Trepel, M.; Märkl, B. Can Low Autopsy Rates Be Increased? Yes, We Can! Should Postmortem Examinations in Oncology Be Performed? Yes, We Should! A Postmortem Analysis of Oncological Cases. Virchows Arch. 2021, 478, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Schädler, J.; Azeke, A.T.; Ondruschka, B.; Steurer, S.; Lütgehetmann, M.; Fitzek, A.; Möbius, D. Concordance between MITS and Conventional Autopsies for Pathological and Virological Diagnoses. Int. J. Leg. Med. 2024, 138, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Meinhardt, J.; Streit, S.; Dittmayer, C.; Manitius, R.V.; Radbruch, H.; Heppner, F.L. The Neurobiology of SARS-CoV-2 Infection. Nat. Rev. Neurosci. 2024, 25, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Cao, W. Autopsy Education and Rate: Effect of the COVID-19 Pandemic. Rhode Isl. Med. J. 2021, 104, 21–25. [Google Scholar]
- Latten, B.G.H.; Kubat, B.; van den Brandt, P.A.; Zur Hausen, A.; Schouten, L.J. Cause of Death and the Autopsy Rate in an Elderly Population. Virchows Arch. 2023, 483, 865–872. [Google Scholar] [CrossRef]
- Heinrich, F.; Mertz, K.D.; Glatzel, M.; Beer, M.; Krasemann, S. Using Autopsies to Dissect COVID-19 Pathogenesis. Nat. Microbiol. 2023, 8, 1986–1994. [Google Scholar] [CrossRef]
- Burton, J.L.; Underwood, J. Clinical, Educational, and Epidemiological Value of Autopsy. Lancet 2007, 369, 1471–1480. [Google Scholar] [CrossRef] [PubMed]
- Del Duca, F.; Manetti, A.C.; Maiese, A.; Napoletano, G.; Ghamlouch, A.; Pascale, N.; Giorgio, B.; Paola, F.; Russa, R.L. Death Due to Anaphylactic Reaction: The Role of the Forensic Pathologist in an Accurate Postmortem Diagnosis. Medicina 2023, 59, 2184. [Google Scholar] [CrossRef] [PubMed]
- Crouch, E.E.; Damas, C.; Bartrug, W.C.; Shamiyeh, A.; Scelfo, M.; Dreyfus, M.; Gano, D.; Segal, S.; Franck, L.S. Parents’ Views on Autopsy, Organ Donation, and Research Donation After Neonatal Death. JAMA Netw. Open 2023, 6, e2341533. [Google Scholar] [CrossRef]
| Regulation | Issuing Institution | Release Date | Most Relevant Indications |
|---|---|---|---|
| Circular no. 11392 [34] | Ministry of Health | 1 April 2020 | During the emergency phase, autopsies and diagnostic tests should not be conducted on confirmed COVID-19 cases, regardless of whether death occurred in the hospital or at home. |
| SIMLA letter to the Minister of Health [35] | Italian Society of Forensic Medicine | 4 April 2020 (signed by President Prof. Zoja and the Secretary-General Prof. Di Mauro). | A request is made to restructure and adapt autopsy rooms nationwide to meet BSL-3 standards or, at a minimum, to upgrade at least one autopsy room in each provincial capital municipality to comply with the essential technical requirements. |
| Emergency Circular no. 15280 [36] | Italian Ministry of Health | 2 May 2020 | Throughout the emergency phase, autopsies and diagnostic tests must not be performed on confirmed COVID-19 cases, irrespective of whether death occurred in a hospital ward or at home. |
| Circular no. 18457 [37] | Ministry of Health | 28 May 2020. | Previously issued Ministerial Circulars did not aim to prohibit autopsies but only recommended limiting them to safeguard the health of healthcare workers and auxiliary personnel. |
| SIMLA/Italian Society of Forensic Pathologists (GIPF) Communique [35] | Italian Society of Forensic Medicine, signed by Prof. C. Campobasso and G Di Vella | 4 June 2020 | The lack of anatomical biocontainment rooms required to ensure the proper execution of autopsy activities across the country, as well as the safety of healthcare professionals and mortuary staff, represents a critical issue that must be addressed. |
| Circular no. 818 [38] | Ministry of Health | 11 January 2021 | The document no longer includes language “advising against” the execution of autopsies on COVID-19 subjects, effectively lifting the previous restrictions on conducting clinical-forensic autopsy examinations. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaami, S.; Napoletano, G.; Marinelli, E.; Sablone, S.; De Paola, L.; Introna, F. Post-COVID-19 Era Forensics: Hospital Autopsies, New Methodologies, and Medicolegal Perspectives. Forensic Sci. 2025, 5, 8. https://doi.org/10.3390/forensicsci5010008
Zaami S, Napoletano G, Marinelli E, Sablone S, De Paola L, Introna F. Post-COVID-19 Era Forensics: Hospital Autopsies, New Methodologies, and Medicolegal Perspectives. Forensic Sciences. 2025; 5(1):8. https://doi.org/10.3390/forensicsci5010008
Chicago/Turabian StyleZaami, Simona, Gabriele Napoletano, Enrico Marinelli, Sara Sablone, Lina De Paola, and Francesco Introna. 2025. "Post-COVID-19 Era Forensics: Hospital Autopsies, New Methodologies, and Medicolegal Perspectives" Forensic Sciences 5, no. 1: 8. https://doi.org/10.3390/forensicsci5010008
APA StyleZaami, S., Napoletano, G., Marinelli, E., Sablone, S., De Paola, L., & Introna, F. (2025). Post-COVID-19 Era Forensics: Hospital Autopsies, New Methodologies, and Medicolegal Perspectives. Forensic Sciences, 5(1), 8. https://doi.org/10.3390/forensicsci5010008









