Improving Traditional Post Mortem Healthcare—The Cross-Sectional Use of Blood-Based Biomarkers
Abstract
1. Introduction
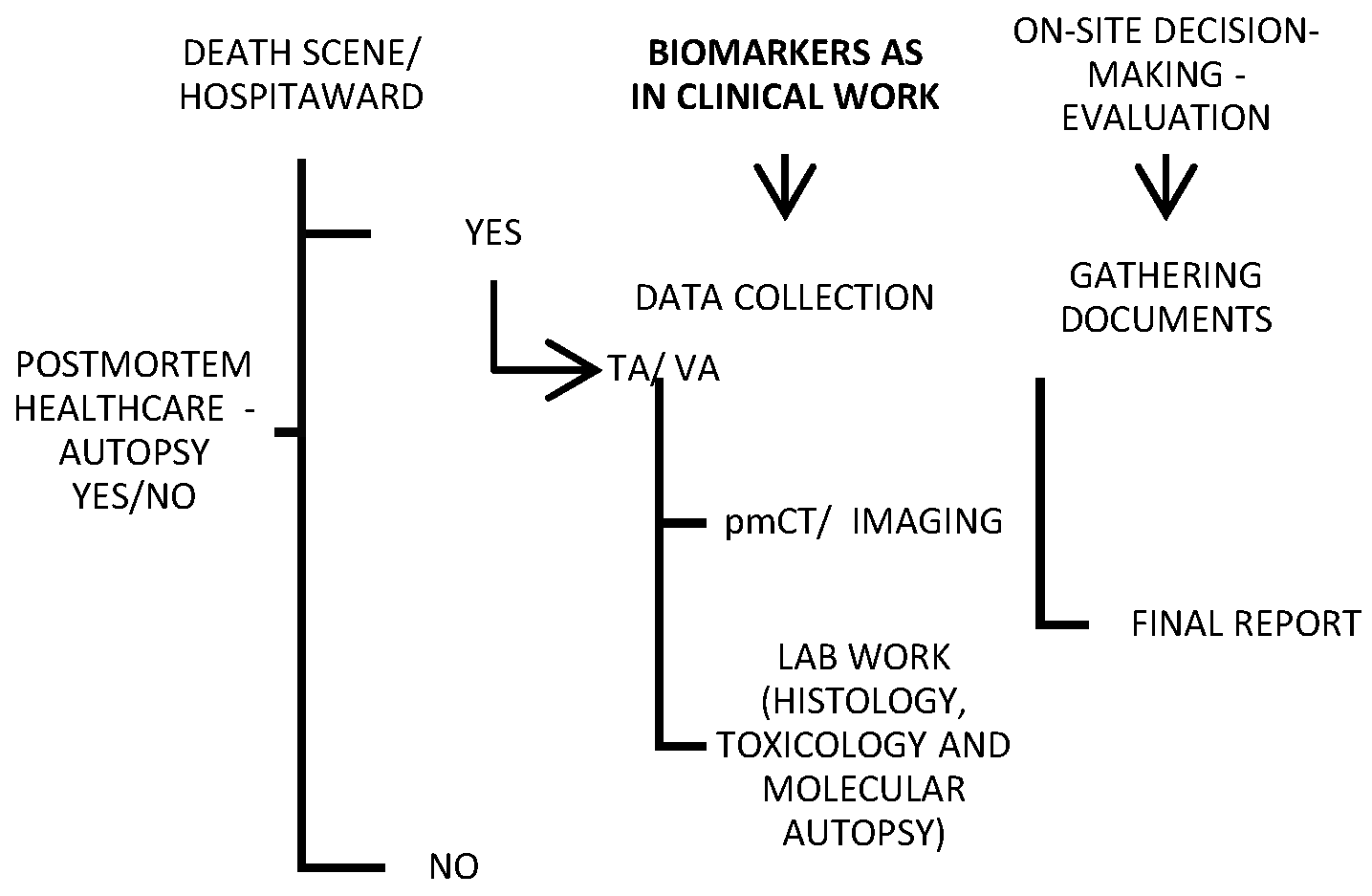
2. Traditional Post Mortem Healthcare
3. Options for Traditional Autopsy
4. Post Mortem Biomarkers
5. Biomarkers of Vascular Quiescence
5.1. Circulating Markers of the Extracellular Matrix: Biomarkers Related to the Vascular Wall
5.2. Proteins Associated with Vascular Lumen: Inflammation and Thrombosis Biomarkers
6. Vascular Cognitive Impairment: Room for Biomarkers at Post Mortem
7. Applying Clinical Biomarkers in a Post Mortem Setting
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordon, I.M.; Hinchliffe, R.J. Biomarkers in Vascular Disease. In Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists [Internet]; University of Adelaide Press: Adelaide, Australia, 2011. [Google Scholar]
- Cui, Z.; Zhao, G.; Liu, X. Blood fibrinogen level as a biomarker of adverse outcomes in patients with coronary artery disease: A systematic review and meta-analysis. Medicine 2022, 101, e30117. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.D.; Aghaeepour, N.; Ahn, A.H.; Angst, M.S.; Borsook, D.; Brenton, A.; Burczynski, M.E.; Crean, C.; Edwards, R.; Gaudilliere, B.; et al. Discovery and validation of biomarkers to aid the development of safe and effective pain therapeutics: Challenges and opportunities. Nat. Rev. Neurol. 2020, 16, 381–400. [Google Scholar] [CrossRef] [PubMed]
- Kutlu, E.; Cil, N.; Avci, E.; Bir, F.; Kilic, I.D.; Dereli, A.K.; Acar, K. Significance of postmortem biomarkers and multimarker strategy in sudden cardiac death. Leg. Med. 2023, 61, 102212. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Zhao, M.; Xu, C.; Zhang, T.; Jia, Y.; Wang, T.; Zhu, B. Evaluation of Agonal Cardiac Function for Sudden Cardiac Death in Forensic Medicine with Postmortem Brain Natriuretic Peptide (BNP) and NT-proBNP: A Meta-analysis. J. Forensic. Sci. 2020, 65, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Puchenkova, O.A.; Soldatov, V.O.; Belykh, A.E.; Bushueva, O.; Piavchenko, G.A.; Venediktov, A.A.; Shakhpazyan, N.K.; Deykin, A.V.; Korokin, M.V.; Pokrovskiy, M.V. Cytokines in Abdominal Aortic Aneurysm: Master Regulators With Clinical Application. Biomark. Insights 2022, 17, 11772719221095676. [Google Scholar] [CrossRef]
- Medeiros, F.A. Biomarkers and Surrogate Endpoints: Lessons Learned From Glaucoma. Investig. Ophthalmol. Vis. Sci. 2017, 58, BIO20–BIO26. [Google Scholar] [CrossRef]
- Vlachopoulos, C.; Xaplanteris, P.; Aboyans, V.; Brodmann, M.; Cifkova, R.; Cosentino, F.; De Carlo, M.; Gallino, A.; Landmesser, U.; Laurent, S.; et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation: Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis 2015, 241, 507–532. [Google Scholar] [CrossRef]
- Basso, C.; Stone, J.R. Autopsy in the era of advanced cardiovascular imaging. Eur. Heart J. 2022, 43, 2461–2468. [Google Scholar] [CrossRef]
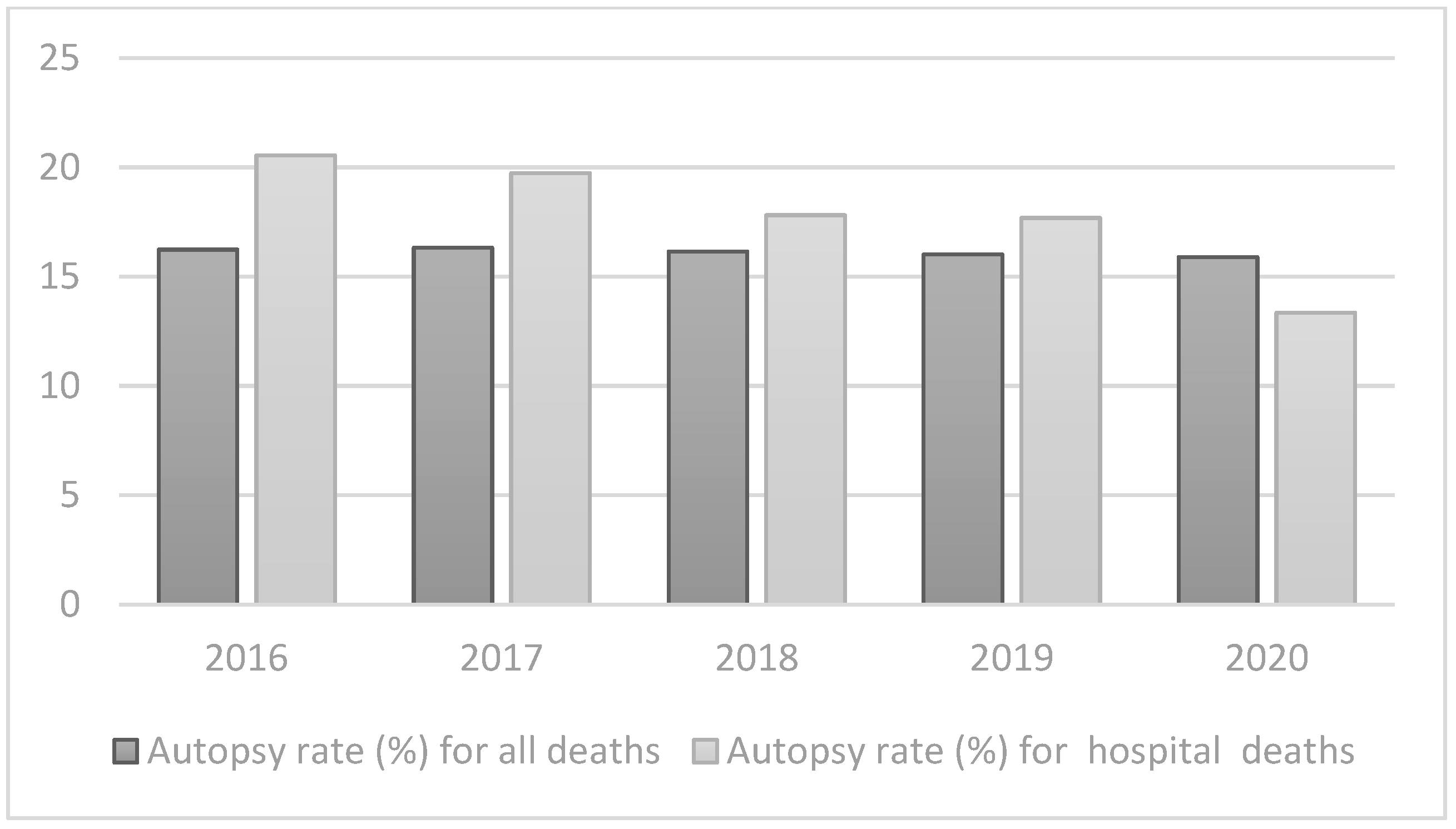
- (WHO), W.H.O. Autopsy Rate (%) for All Deaths. Available online: https://gateway.euro.who.int/en/indicators/hfa_545-6410-autopsy-rate-for-all-deaths/ (accessed on 3 May 2023).
- (WHO), W.H.O. Autopsy Rate (%) for Hospital Deaths. Available online: https://gateway.euro.who.int/en/indicators/hfa_544-6400-autopsy-rate-for-hospital-deaths/ (accessed on 3 May 2023).
- Waidhauser, J.; Martin, B.; Trepel, M.; Markl, B. Can low autopsy rates be increased? Yes, we can! Should postmortem examinations in oncology be performed? Yes, we should! A postmortem analysis of oncological cases. Virchows Arch. 2021, 478, 301–308. [Google Scholar] [CrossRef]
- Bunei, M.; Muturi, P.; Otiato, F.; Njuguna, H.N.; Emukule, G.O.; Otieno, N.A.; Dawa, J.; Chaves, S.S. Factors Influencing Acceptance of Post-Mortem Examination of Children at a Tertiary Care Hospital in Nairobi, Kenya. Ann. Glob. Health 2019, 85, 95. [Google Scholar] [CrossRef]
- Rosendahl, A.; Mjörnheim, B.; Eriksson, L.C. Autopsies and quality of cause of death diagnoses. SAGE Open Med. 2021, 9, 20503121211037169. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, S.; Namusanya, D.; Hamuza, A.; Huwa, C.; Chasweka, D.; Kelley, M.; Molyneux, S.; Voskuijl, W.; Denno, D.M.; Desmond, N. Hypothetical acceptability of hospital-based post-mortem pediatric minimally invasive tissue sampling in Malawi: The role of complex social relationships. PLoS ONE 2021, 16, e0246369. [Google Scholar] [CrossRef] [PubMed]
- Stambouly, J.J.; Kahn, E.; Boxer, R.A. Correlation between clinical diagnoses and autopsy findings in critically ill children. Pediatrics 1993, 92, 248–251. [Google Scholar] [CrossRef]
- Mitrovic, D.; Savic, I.; Jankovic, R. Discrepancies between clinical and autopsy diagnosis of cause of death among psychiatric patients who died due to natural causes. A retrospective autopsy study. Vojnosanit. Pregl. 2019, 76, 278–283. [Google Scholar] [CrossRef]
- Herath, J.C.; Herath, S.O. Is it time for targeted and minimally invasive post-mortem examination using total body computed tomography in a medicolegal autopsy? Forensic Sci. Med. Pathol. 2021, 17, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Mercala, E.; Benbow, E.W. Autopsy by Imaging: The Last 10 Years. Forensic Sci. 2022, 2, 696–714. [Google Scholar] [CrossRef]
- Ferencic, A.; Stemberger, C.; Cuculić, D.; Jakovac, H. Autopsies during COVID-19 pandemic—Caution is never too much: Postmortem detection of SARS-CoV-2 in the severely burned and carbonized bodies. Indian J. Pathol. Microbiol. 2022, 65, 959–960. [Google Scholar] [CrossRef] [PubMed]
- Kurz, S.D.; Sido, V.; Herbst, H.; Ulm, B.; Salkic, E.; Ruschinski, T.M.; Buschmann, C.T.; Tsokos, M. Discrepancies between clinical diagnosis and hospital autopsy: A comparative retrospective analysis of 1112 cases. PLoS ONE 2021, 16, e0255490. [Google Scholar] [CrossRef]
- Buja, L.M.; Barth, R.F.; Krueger, G.R.; Brodsky, S.V.; Hunter, R.L. The Importance of the Autopsy in Medicine: Perspectives of Pathology Colleagues. Acad. Pathol. 2019, 6, 2374289519834041. [Google Scholar] [CrossRef]
- van den Tweel, J.G.; Wittekind, C. The medical autopsy as quality assurance tool in clinical medicine: Dreams and realities. Virchows Arch. 2016, 468, 75–81. [Google Scholar] [CrossRef]
- Rodrigues, F.S.; Oliveira, I.C.; Cat, M.N.L.; Mattos, M.C.L.; Silva, G.A. Agreement between Clinical and Anatomopathological Diagnoses in Pediatric Intensive Care. Rev. Paul. Pediatr. 2021, 39, e2019263. [Google Scholar] [CrossRef] [PubMed]
- Thiene, G.; Saffitz, J.E. Autopsy as a Source of Discovery in Cardiovascular Medicine: Then and Now. Circulation 2018, 137, 2683–2685. [Google Scholar] [CrossRef] [PubMed]
- Bombi, J.A.; Llebaria, C.; Rives, A. Analysis of a series of 500 clinical post mortem studies. II. Basic diagnosis (author’s transl). Med. Clin. 1981, 77, 185–189. [Google Scholar]
- Smith, A.M.; Lingard, L.; Heslop, P.; Gray, J.; Walker, D.J. Vascular disease as a cause of death in patients with severe disability due to osteoarthritis and rheumatoid arthritis. Springerplus 2015, 4, 328. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.; Rayner, M.; Leal, J.; Luengo-Fernandez, R.; Gray, A. European Cardiovascular Disease Statistics; British Heart Foundation: Glasgow, UK, 2000. [Google Scholar]
- EUROSTAT. Causes of Death Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Causes_of_death_statistics (accessed on 3 May 2023).
- Earle, W.; Misra, S.; Herzig, M.; Abdallah, G.; Ross, C.D.; Secemsky, E.A.; Carroll, B. Cause of Death Analysis in Patients with Intermeditate Risk Acute Pulmonary Embolism. J. Am. Coll. Cardiol. 2023, 81, 2088. [Google Scholar] [CrossRef]
- Hamer, H.M.; Stroobants, A.K.; Bavalia, R.; Ponjee, G.A.E.; Klok, F.A.; van der Hulle, T.; Huisman, M.V.; Hendriks, H.A.; Middeldorp, S. Diagnostic accuracy of four different D-dimer assays: A post-hoc analysis of the YEARS study. Thromb. Res. 2021, 201, 18–22. [Google Scholar] [CrossRef]
- Donaldson, A.E.; Lamont, I.L. Biochemistry changes that occur after death: Potential markers for determining post-mortem interval. PLoS ONE 2013, 8, e82011. [Google Scholar] [CrossRef]
- Yao, Y.; Cao, J.; Wang, Q.; Shi, Q.; Liu, K.; Luo, Z.; Chen, X.; Chen, S.; Yu, K.; Huang, Z.; et al. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: A case control study. J. Intensive Care 2020, 8, 49. [Google Scholar] [CrossRef]
- Aronson, J.K. When I use a word.... Too much healthcare—Biomarkers. BMJ 2022, 379, o2533. [Google Scholar] [CrossRef]
- Aronson, J.K.; Ferner, R.E. Biomarkers-A General Review. Curr. Protoc. Pharmacol. 2017, 76, 9–23. [Google Scholar] [CrossRef]
- Solarino, B.; Ferorelli, D.; Dell’Erba, A. Post-mortem routine practice in the era of the COVID-19 pandemic. J. Forensic. Leg. Med. 2020, 74, 102010. [Google Scholar] [CrossRef] [PubMed]
- Roberts, I.S.; Benamore, R.E.; Benbow, E.W.; Lee, S.H.; Harris, J.N.; Jackson, A.; Mallett, S.; Patankar, T.; Peebles, C.; Roobottom, C.; et al. Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: A validation study. Lancet 2012, 379, 136–142. [Google Scholar] [CrossRef]
- Blokker, B.M.; Wagensveld, I.M.; Weustink, A.C.; Oosterhuis, J.W.; Hunink, M.G. Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: A systematic review. Eur. Radiol. 2016, 26, 1159–1179. [Google Scholar] [CrossRef]
- Wichmann, D.; Obbelode, F.; Vogel, H.; Hoepker, W.W.; Nierhaus, A.; Braune, S.; Sauter, G.; Pueschel, K.; Kluge, S. Virtual autopsy as an alternative to traditional medical autopsy in the intensive care unit: A prospective cohort study. Ann. Intern. Med. 2012, 156, 123–130. [Google Scholar] [CrossRef]
- Flaxman, A.D.; Stewart, A.; Joseph, J.C.; Alam, N.; Alam, S.S.; Chowdhury, H.; Mooney, M.D.; Rampatige, R.; Remolador, H.; Sanvictores, D.; et al. Collecting verbal autopsies: Improving and streamlining data collection processes using electronic tablets. Popul. Health Metr. 2018, 16, 3. [Google Scholar] [CrossRef]
- Sinard, J.H. Factors affecting autopsy rates, autopsy request rates, and autopsy findings at a large academic medical center. Exp. Mol. Pathol. 2001, 70, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Paratz, E.D.; Rowe, S.J.; Stub, D.; Pflaumer, A.; La Gerche, A. A systematic review of global autopsy rates in all-cause mortality and young sudden death. Heart Rhythm. 2023, 20, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Michaud, K.; Jacobsen, C.; Basso, C.; Banner, J.; Blokker, B.M.; de Boer, H.H.; Dedouit, F.; O’Donnell, C.; Giordano, C.; Magnin, V. Application of postmortem imaging modalities in cases of sudden death due to cardiovascular diseases–current achievements and limitations from a pathology perspective. Virchows Archiv. 2023, 482, 385–406. [Google Scholar] [CrossRef]
- De Souza, P.M.M.; Gerson, G.; Dias, J.S.; De Melo, D.N.; De Souza, S.G.; Ruiz, E.M.; Fernandes Tavora, F.R.; Cavalcanti, L.P.D.G. Validation of verbal autopsy and nasopharyngeal swab collection for the investigation of deaths at home during the COVID-19 pandemics in Brazil. PLoS Neglected Trop. Dis. 2020, 14, e0008830. [Google Scholar] [CrossRef]
- Rosen, T.; Safford, M.M.; Sterling, M.R.; Goyal, P.; Patterson, M.; Al Malouf, C.; Ballin, M.; Del Carmen, T.; LoFaso, V.M.; Raik, B.L.; et al. Development of the Verbal Autopsy Instrument for COVID-19 (VAIC). J. Gen. Intern. Med. 2021, 36, 3522–3529. [Google Scholar] [CrossRef]
- Nasaruddin, N.H.; Ganapathy, S.S.; Awaluddin, S.M.; Anuar, M.F.M.; Binti Alias, N.; Mang, C.Y.; Wan-Fei, K. Conducting verbal autopsy by telephone interview during the pandemic to support mortality surveillance: A feasibility study in Malaysia. West. Pac. Surveill. Response J. 2022, 13, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Singh, A. Childhood Malnutrition in India. In Perspective of Recent Advances in Acute Diarrhea; IntechOpen: London, UK, 2020. [Google Scholar]
- Caleo, G.; Sy, A.; Balandine, S.; Polonsky, J.; Palma, P.; Grais, R. The 2012 WHO verbal autopsy instrument. Lancet 2018, 12, 1–11. [Google Scholar]
- Thomas, L.M.; D’Ambruoso, L.; Balabanova, D. Verbal autopsy in health policy and systems: A literature review. BMJ Glob. Health 2018, 3, e000639. [Google Scholar] [CrossRef]
- Mahesh, B.P.K.; Hart, J.D.; Acharya, A.; Chowdhury, H.R.; Joshi, R.; Adair, T.; Hazard, R.H. Validation studies of verbal autopsy methods: A systematic review. BMC Public Health 2022, 22, 2215. [Google Scholar] [CrossRef]
- Joshi, R.; Praveen, D.; Jan, S.; Raju, K.; Maulik, P.; Jha, V.; Lopez, A.D. How much does a verbal autopsy based mortality surveillance system cost in rural India? PLoS ONE 2015, 10, e0126410. [Google Scholar] [CrossRef] [PubMed]
- Krehbiel, K.; Pinckard, J.K. The Toolbox Approach to Forensic Pathology. Acad. Forensic Pathol. 2015, 5, 534–547. [Google Scholar] [CrossRef]
- Yi-Li, G.W.; Lai, P.S.; Noor, M.H.M.; Chinna, K.; Ibrahim, M. Reliability of Post-Mortem Computed Tomography in Measuring Foramen Magnum Dimensions: A Pilot Study. Forensic Anthropol. 2023, 1–9. [Google Scholar] [CrossRef]
- Guidi, B.; Aquaro, G.D.; Gesi, M.; Emdin, M.; Di Paolo, M. Postmortem cardiac magnetic resonance in sudden cardiac death. Heart Fail. Rev. 2018, 23, 651–665. [Google Scholar] [CrossRef]
- Cartocci, G.; Santurro, A.; Neri, M.; Zaccagna, F.; Catalano, C.; La Russa, R.; Turillazzi, E.; Panebianco, V.; Frati, P.; Fineschi, V. Post-mortem computed tomography (PMCT) radiological findings and assessment in advanced decomposed bodies. Radiol. Med. 2019, 124, 1018–1027. [Google Scholar] [CrossRef]
- Filograna, L.; Manenti, G.; O’Donnell, C.; Floris, R.; Oliva, A. Potentials of post-mortem CT (PMCT) in paediatric cases related to SARS-CoV-2 infection. Forensic. Sci. Med. Pathol. 2023, 19, 289–290. [Google Scholar] [CrossRef]
- Hyde, G.; Rummery, R.; Whitby, E.H.; Bloor, J.; Raghavan, A.; Cohen, M.C. Benefits and Limitations of the Minimally Invasive Postmortem: A Review of an Innovative Service Development. Pediatr. Dev. Pathol. 2020, 23, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Zech, W.D.; Jackowski, C.; Schwendener, N.; Brencicova, E.; Schuster, F.; Lombardo, P. Postmortem CT versus forensic autopsy: Frequent discrepancies of tracheobronchial content findings. Int. J. Legal. Med. 2016, 130, 191–198. [Google Scholar] [CrossRef]
- Mondello, C.; Baldino, G.; Bottari, A.; Sapienza, D.; Perri, F.; Argo, A.; Asmundo, A.; Ventura Spagnolo, E. The role of PMCT for the assessment of the cause of death in natural disaster (landslide and flood): A Sicilian experience. Int. J. Legal. Med. 2022, 136, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Chatzaraki, V.; Thali, M.J.; Ampanozi, G. Diagnostic accuracy of postmortem computed tomography for bleeding source determination in cases with hemoperitoneum. Int. J. Legal. Med. 2021, 135, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Shelmerdine, S.C.; Sebire, N.J.; Arthurs, O.J. Diagnostic accuracy of postmortem ultrasound vs. postmortem 1.5-T MRI for non-invasive perinatal autopsy. Ultrasound Obstet. Gynecol. 2021, 57, 449–458. [Google Scholar] [CrossRef]
- Thayyil, S.; Chandrasekaran, M.; Chitty, L.S.; Wade, A.; Skordis-Worrall, J.; Bennett-Britton, I.; Cohen, M.; Withby, E.; Sebire, N.J.; Robertson, N.J.; et al. Diagnostic accuracy of post-mortem magnetic resonance imaging in fetuses, children and adults: A systematic review. Eur. J. Radiol. 2010, 75, e142–e148. [Google Scholar] [CrossRef]
- Puntmann, V.O. How-to guide on biomarkers: Biomarker definitions, validation and applications with examples from cardiovascular disease. Postgrad. Med. J. 2009, 85, 538–545. [Google Scholar] [CrossRef]
- Bondareva, O.; Sheikh, B.N. Vascular Homeostasis and Inflammation in Health and Disease-Lessons from Single Cell Technologies. Int. J. Mol. Sci. 2020, 21, 4688. [Google Scholar] [CrossRef]
- Almulhim, A.M.; Menezes, R.G. Evaluation of Postmortem Changes; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- O’Keefe, H.; Shenfine, R.; Brown, M.; Beyer, F.; Rankin, J. Are non-invasive or minimally invasive autopsy techniques for detecting cause of death in prenates, neonates and infants accurate? A systematic review of diagnostic test accuracy. BMJ Open 2023, 13, e064774. [Google Scholar] [CrossRef]
- Ricard, N.; Bailly, S.; Guignabert, C.; Simons, M. The quiescent endothelium: Signalling pathways regulating organ-specific endothelial normalcy. Nat. Rev. Cardiol. 2021, 18, 565–580. [Google Scholar] [CrossRef]
- Schlereth, K.; Weichenhan, D.; Bauer, T.; Heumann, T.; Giannakouri, E.; Lipka, D.; Jaeger, S.; Schlesner, M.; Aloy, P.; Eils, R.; et al. The transcriptomic and epigenetic map of vascular quiescence in the continuous lung endothelium. Elife 2018, 7, e34423. [Google Scholar] [CrossRef] [PubMed]
- Qian, G.; Adeyanju, O.; Olajuyin, A.; Guo, X. Abdominal Aortic Aneurysm Formation with a Focus on Vascular Smooth Muscle Cells. Life 2022, 12, 191. [Google Scholar] [CrossRef]
- Pal, D.; Szilagyi, B.; Berczeli, M.; Szalay, C.I.; Sardy, B.; Olah, Z.; Szekely, T.; Racz, G.; Banga, P.; Czinege, Z.; et al. Ruptured Aortic Aneurysm and Dissection Related Death: An Autopsy Database Analysis. Pathol. Oncol. Res. 2020, 26, 2391–2399. [Google Scholar] [CrossRef] [PubMed]
- Takada, M.; Yamagishi, K.; Tamakoshi, A.; Iso, H. Height and Mortality from Aortic Aneurysm and Dissection. J. Atheroscler. Thromb. 2022, 29, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.; Goyal, A.; Grigorova, Y.; Farci, F.; Le, J.K. Aortic Dissection. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- La Russa, R.; Maiese, A.; Viola, R.V.; De Matteis, A.; Pinchi, E.; Frati, P.; Fineschi, V. Searching for highly sensitive and specific biomarkers for sepsis: State-of-the-art in post-mortem diagnosis of sepsis through immunohistochemical analysis. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419855226. [Google Scholar] [CrossRef] [PubMed]
- Imanaka-Yoshida, K.; Matsumoto, K.I. Multiple Roles of Tenascins in Homeostasis and Pathophysiology of Aorta. Ann. Vasc. Dis. 2018, 11, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Brady, A.R.; Thompson, S.G.; Fowkes, F.G.; Greenhalgh, R.M.; Powell, J.T.; Participants, U.K.S.A.T. Abdominal aortic aneurysm expansion: Risk factors and time intervals for surveillance. Circulation 2004, 110, 16–21. [Google Scholar] [CrossRef]
- Pierrakos, C.; Velissaris, D.; Bisdorff, M.; Marshall, J.C.; Vincent, J.L. Biomarkers of sepsis: Time for a reappraisal. Crit. Care 2020, 24, 287. [Google Scholar] [CrossRef]
- Bown, M.J.; Sutton, A.J.; Bell, P.R.; Sayers, R.D. A meta-analysis of 50 years of ruptured abdominal aortic aneurysm repair. Br. J. Surg. 2002, 89, 714–730. [Google Scholar] [CrossRef]
- Rastogi, V.; Stefens, S.J.M.; Houwaart, J.; Verhagen, H.J.M.; de Bruin, J.L.; van der Pluijm, I.; Essers, J. Molecular Imaging of Aortic Aneurysm and Its Translational Power for Clinical Risk Assessment. Front. Med. 2022, 9, 814123. [Google Scholar] [CrossRef]
- Li, T.; Jiang, B.; Li, X.; Sun, H.Y.; Li, X.T.; Jing, J.J.; Yang, J. Serum matrix metalloproteinase-9 is a valuable biomarker for identification of abdominal and thoracic aortic aneurysm: A case-control study. BMC Cardiovasc. Disord. 2018, 18, 202. [Google Scholar] [CrossRef] [PubMed]
- Bihlet, A.R.; Karsdal, M.A.; Sand, J.M.; Leeming, D.J.; Roberts, M.; White, W.; Bowler, R. Biomarkers of extracellular matrix turnover are associated with emphysema and eosinophilic-bronchitis in COPD. Respir. Res. 2017, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, J.H.; Karsdal, M.A.; Sand, J.M.; Willumsen, N.; Diefenbach, C.; Svensson, B.; Hagglund, P.; Oersnes-Leeming, D.J. Serological assessment of neutrophil elastase activity on elastin during lung ECM remodeling. BMC Pulm. Med. 2015, 15, 53. [Google Scholar] [CrossRef] [PubMed]
- Aragon-Vela, J.; Alcala-Bejarano Carrillo, J.; Moreno-Racero, A.; Plaza-Diaz, J. The Role of Molecular and Hormonal Factors in Obesity and the Effects of Physical Activity in Children. Int. J. Mol. Sci. 2022, 23, 15413. [Google Scholar] [CrossRef]
- Demestre, M.; Parkin-Smith, G.; Petzold, A.; Pullen, A.H. The pro and the active form of matrix metalloproteinase-9 is increased in serum of patients with amyotrophic lateral sclerosis. J. Neuroimmunol. 2005, 159, 146–154. [Google Scholar] [CrossRef]
- Silvello, D.; Narvaes, L.B.; Albuquerque, L.C.; Forgiarini, L.F.; Meurer, L.; Martinelli, N.C.; Andrades, M.E.; Clausell, N.; dos Santos, K.G.; Rohde, L.E. Serum levels and polymorphisms of matrix metalloproteinases (MMPs) in carotid artery atherosclerosis: Higher MMP-9 levels are associated with plaque vulnerability. Biomarkers 2014, 19, 49–55. [Google Scholar] [CrossRef]
- Beck-Joseph, J.; Lehoux, S. Molecular Interactions Between Vascular Smooth Muscle Cells and Macrophages in Atherosclerosis. Front. Cardiovasc. Med. 2021, 8, 737934. [Google Scholar] [CrossRef]
- Makita, S.; Nakamura, M.; Hiramori, K. The association of C-reactive protein levels with carotid intima-media complex thickness and plaque formation in the general population. Stroke 2005, 36, 2138–2142. [Google Scholar] [CrossRef]
- Andrade, C.; Bosco, A.; Sandrim, V.; Silva, F. MMP-9 Levels and IMT of Carotid Arteries are Elevated in Obese Children and Adolescents Compared to Non-Obese. Arq. Bras. Cardiol. 2017, 108, 198–203. [Google Scholar] [CrossRef]
- Antoniou, G.A.; Georgiadis, G.S.; Antoniou, S.A.; Murray, D.; Smyth, J.V.; Serracino-Inglott, F.; Paraskevas, K.I. Plasma matrix metalloproteinase 9 levels may predict endoleaks after endovascular aortic aneurysm repair. Angiology 2013, 64, 49–56. [Google Scholar] [CrossRef]
- Maguire, E.M.; Pearce, S.W.A.; Xiao, R.; Oo, A.Y.; Xiao, Q. Matrix Metalloproteinase in Abdominal Aortic Aneurysm and Aortic Dissection. Pharmaceuticals 2019, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Kumarasamy, G.; Ismail, M.N.; Tuan, S.E.; Sharif, C.D.; Mittal, P.; Hoffmann, P.; Kaur, G. Conference Proceedings–6th International Conference on Molecular Diagnostics and Biomarker Discovery (MDBD 2022): Building Resilience in Biomedical Research. In Proceedings of the BMC Proceedings, Penang, Malaysia, 11–13 October 2022; p. 1. [Google Scholar]
- Palstrom, N.B.; Matthiesen, R.; Rasmussen, L.M.; Beck, H.C. Recent Developments in Clinical Plasma Proteomics-Applied to Cardiovascular Research. Biomedicines 2022, 10, 162. [Google Scholar] [CrossRef] [PubMed]
- Hong, L.Z.; Xue, Q.; Shao, H. Inflammatory Markers Related to Innate and Adaptive Immunity in Atherosclerosis: Implications for Disease Prediction and Prospective Therapeutics. J. Inflamm. Res. 2021, 14, 379–392. [Google Scholar] [CrossRef]
- Soleimani, Z.; Amighi, F.; Vakili, Z.; Momen-Heravi, M.; Moravveji, S.A. Diagnostic value of procalcitonin, erythrocyte sedimentation rate (ESR), quantitative C-reactive protein (CRP) and clinical findings associated with osteomyelitis in patients with diabetic foot. Hum. Antibodies 2021, 29, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Albu, E.; Filip, C.; Zamosteanu, N.; Jaba, I.M.; Linic, I.S.; Sosa, I. Hyperhomocysteinemia is an indicator of oxidant stress. Med. Hypotheses 2012, 78, 554–555. [Google Scholar] [CrossRef] [PubMed]
- Atre, A.S.; CR, W.D.S.; Suresh, V.; Nagaraja, M.; Madhuvan, H. Evaluation of Plasma Total Antioxidant Capacity Levels and Osteocalcin in Prediabetes and Healthy Subjects. RGUHS J. Med. Sci. 2020, 10, 20–26. [Google Scholar] [CrossRef]
- Hirano, T. IL-6 in inflammation, autoimmunity and cancer. Int. Immunol. 2021, 33, 127–148. [Google Scholar] [CrossRef]
- Ridker, P.M.; MacFadyen, J.G.; Glynn, R.J.; Bradwin, G.; Hasan, A.A.; Rifai, N. Comparison of interleukin-6, C-reactive protein, and low-density lipoprotein cholesterol as biomarkers of residual risk in contemporary practice: Secondary analyses from the Cardiovascular Inflammation Reduction Trial. Eur. Heart J. 2020, 41, 2952–2961. [Google Scholar] [CrossRef]
- Holcomb, D.; Alexaki, A.; Hernandez, N.; Hunt, R.; Laurie, K.; Kames, J.; Hamasaki-Katagiri, N.; Komar, A.A.; DiCuccio, M.; Kimchi-Sarfaty, C. Gene variants of coagulation related proteins that interact with SARS-CoV-2. PLoS Comput. Biol. 2021, 17, e1008805. [Google Scholar] [CrossRef]
- Petel, D.; Winters, N.; Gore, G.C.; Papenburg, J.; Beltempo, M.; Lacroix, J.; Fontela, P.S. Use of C-reactive protein to tailor antibiotic use: A systematic review and meta-analysis. BMJ Open 2018, 8, e022133. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Cockerill, G.W.; Choke, E.; Belli, A.M.; Loftus, I.; Thompson, M.M. Aortic aneurysms secrete interleukin-6 into the circulation. J. Vasc. Surg. 2007, 45, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Artemiou, P.; Charokopos, N.; Rouska, E.; Sabol, F.; Chrysogonidis, I.; Tsavdaridou, V.; Paschalidis, G. C-reactive protein/interleukin-6 ratio as marker of the size of the uncomplicated thoracic aortic aneurysms. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Cui, N.; Zhang, H.; Chen, Z.; Yu, Z. Prognostic significance of PCT and CRP evaluation for adult ICU patients with sepsis and septic shock: Retrospective analysis of 59 cases. J. Int. Med. Res. 2019, 47, 1573–1579. [Google Scholar] [CrossRef]
- Tan, M.; Lu, Y.; Jiang, H.; Zhang, L. The diagnostic accuracy of procalcitonin and C-reactive protein for sepsis: A systematic review and meta-analysis. J. Cell. Biochem. 2019, 120, 5852–5859. [Google Scholar] [CrossRef]
- Hung, S.K.; Lan, H.M.; Han, S.T.; Wu, C.C.; Chen, K.F. Current Evidence and Limitation of Biomarkers for Detecting Sepsis and Systemic Infection. Biomedicines 2020, 8, 494. [Google Scholar] [CrossRef]
- Al-Barjas, H.S.; Ariens, R.; Grant, P.; Scott, J.A. Raised plasma fibrinogen concentration in patients with abdominal aortic aneurysm. Angiology 2006, 57, 607–614. [Google Scholar] [CrossRef]
- Menekşe, E.; Düz, M.E. Changes in D-dimer, Ferritin, and Fibrinogen in Healthy Smokers and Nonsmokers during the COVID-19 Outbreak. J. Surg. Res. 2023, 6, 94–99. [Google Scholar] [CrossRef]
- Ezaki, M.; Wada, H.; Ichikawa, Y.; Ikeda, N.; Shiraki, K.; Yamamoto, A.; Moritani, I.; Shimaoka, M.; Shimpo, H. Plasma Soluble Fibrin Is Useful for the Diagnosis of Thrombotic Diseases. J. Clin. Med. 2023, 12, 2597. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; de Curtis, A.; Costanzo, S.; Persichillo, M.; Olivieri, M.; Zito, F.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Investigators, M.-S.P. Association of D-dimer levels with all-cause mortality in a healthy adult population: Findings from the MOLI-SANI study. Haematologica 2013, 98, 1476–1480. [Google Scholar] [CrossRef]
- Takagi, H.; Manabe, H.; Kawai, N.; Goto, S.; Umemoto, T. Plasma fibrinogen and D-dimer concentrations are associated with the presence of abdominal aortic aneurysm: A systematic review and meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2009, 38, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Couturaud, F.; Kearon, C.; Bates, S.M.; Ginsberg, J.S. Decrease in sensitivity of D-dimer for acute venous thromboembolism after starting anticoagulant therapy. Blood Coagul. Fibrinolysis 2002, 13, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Sadanaga, T.; Sadanaga, M.; Ogawa, S. Evidence that D-dimer levels predict subsequent thromboembolic and cardiovascular events in patients with atrial fibrillation during oral anticoagulant therapy. J. Am. Coll. Cardiol. 2010, 55, 2225–2231. [Google Scholar] [CrossRef] [PubMed]
- Crawford, F.; Andras, A.; Welch, K.; Sheares, K.; Keeling, D.; Chappell, F.M. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst. Rev. 2016, 2016, CD010864. [Google Scholar] [CrossRef]
- Wang, H. Evaluation of D-Dimer in Postmortem Blood Using the SERATEC PMB Test; Boston University: Boston, MA, USA, 2019. [Google Scholar]
- Gevsemezoglu, O.F.; Karadayi, B.; Koca, Y.; Cetin, G. Investigation of the use of seratec pmb test on postmortem peripheral blood samples for forensic purposes. Medicine 2022, 11, 159–165. [Google Scholar] [CrossRef]
- Goncalves, F.A.R.; Besen, B.; Lima, C.A.; Cora, A.P.; Pereira, A.J.R.; Perazzio, S.F.; Gouvea, C.P.; Fonseca, L.A.M.; Trindade, E.M.; Sumita, N.M.; et al. Use and misuse of biomarkers and the role of D-dimer and C-reactive protein in the management of COVID-19: A post-hoc analysis of a prospective cohort study. Clinics 2021, 76, e3547. [Google Scholar] [CrossRef]
- Gorelick, P.B.; Scuteri, A.; Black, S.E.; Decarli, C.; Greenberg, S.M.; Iadecola, C.; Launer, L.J.; Laurent, S.; Lopez, O.L.; Nyenhuis, D.; et al. Vascular contributions to cognitive impairment and dementia: A statement for healthcare professionals from the american heart association/american stroke association. Stroke 2011, 42, 2672–2713. [Google Scholar] [CrossRef]
- Han, X.; Wang, W.; He, J.; Jiang, L.; Li, X. Osteopontin as a biomarker for osteosarcoma therapy and prognosis. Oncol. Lett. 2019, 17, 2592–2598. [Google Scholar] [CrossRef]
- Chai, Y.L.; Chong, J.R.; Raquib, A.R.; Xu, X.; Hilal, S.; Venketasubramanian, N.; Tan, B.Y.; Kumar, A.P.; Sethi, G.; Chen, C.P.; et al. Plasma osteopontin as a biomarker of Alzheimer’s disease and vascular cognitive impairment. Sci. Rep. 2021, 11, 4010. [Google Scholar] [CrossRef]
- Wei, R.; Wong, J.P.C.; Kwok, H.F. Osteopontin—A promising biomarker for cancer therapy. J. Cancer 2017, 8, 2173–2183. [Google Scholar] [CrossRef]
- Bruha, R.; Vitek, L.; Smid, V. Osteopontin—A potential biomarker of advanced liver disease. Ann. Hepatol. 2020, 19, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Farrokhi, V.; Chabot, J.R.; Neubert, H.; Yang, Z. Assessing the Feasibility of Neutralizing Osteopontin with Various Therapeutic Antibody Modalities. Sci. Rep. 2018, 8, 7781. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, M.; MovaseghiGargari, M.; Chand, M.T. The importance of autopsies despite the declining number amidst the COVID-19 pandemic. Autops. Case Rep. 2022, 12, e2021371. [Google Scholar] [CrossRef]
- Elmsjo, A.; Vikingsson, S.; Soderberg, C.; Kugelberg, F.C.; Green, H. Post-Mortem Metabolomics: A Novel Approach in Clinical Biomarker Discovery and a Potential Tool in Death Investigations. Chem. Res. Toxicol. 2021, 34, 1496–1502. [Google Scholar] [CrossRef]
- Hudak, L.; Nagy, A.C.; Molnar, S.; Mehes, G.; Nagy, K.E.; Olah, L.; Csiba, L. Discrepancies between clinical and autopsy findings in patients who had an acute stroke. Stroke Vasc. Neurol. 2022, 7, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Lilla, H.; (Penang, Malaysia). Personal communication, 2023.
- Goldman, L. Autopsy 2018: Still necessary, even if occasionally not sufficient. Circulation 2018, 137, 2686–2688. [Google Scholar] [CrossRef]
- Lunetta, P.; Lounamaa, A.; Sihvonen, S. Surveillance of injury-related deaths: Medicolegal autopsy rates and trends in Finland. Inj. Prev. 2007, 13, 282–284. [Google Scholar] [CrossRef]
- Perkins, G.D.; McAuley, D.F.; Davies, S.; Gao, F. Discrepancies between clinical and postmortem diagnoses in critically ill patients: An observational study. Crit. Care 2003, 7, R129–R132. [Google Scholar] [CrossRef]
- Nehring, S.; Goyal, A.; Patel, B. C Reactive Protein. 2021 Dec 28. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Nourkami-Tutdibi, N.; Graf, N.; Beier, R.; Zemlin, M.; Tutdibi, E. Plasma levels of osteopontin from birth to adulthood. Pediatr. Blood Cancer 2020, 67, e28272. [Google Scholar] [CrossRef]
- Sikora-Skrabaka, M.; Skrabaka, D.; Ruggeri, P.; Caramori, G.; Skoczynski, S.; Barczyk, A. D-dimer value in the diagnosis of pulmonary embolism-may it exclude only? J. Thorac. Dis. 2019, 11, 664–672. [Google Scholar] [CrossRef]
- Alvarez, B.; Ruiz, C.; Chacon, P.; Alvarez-Sabin, J.; Matas, M. Serum values of metalloproteinase-2 and metalloproteinase-9 as related to unstable plaque and inflammatory cells in patients with greater than 70% carotid artery stenosis. J. Vasc. Surg. 2004, 40, 469–475. [Google Scholar] [CrossRef] [PubMed]
| Related Process | Biomarker | Medium | Reference Values | Half-Life |
|---|---|---|---|---|
| Inflammation | CRP | S | <0.3 mg/dL: normal 0.3 to 1.0 mg/dL: normal to minor elevation (can be seen in obesity, pregnancy, diabetes, common cold, gingivitis, periodontitis, sedentary lifestyle, cigarette smoking, and genetic polymorphisms) [130]. | ~19 h [99] |
| OPT | S | 122.3 ± 39.2 ng/mL | 5 to 15 h [122] | |
| P | 463.7 ng/mL–587.0 ng/mL [131]. | |||
| Related to thrombus | D-dimer | S | <2152 ng/mL [132]. | 4 to 6 h [111] |
| Matrix-degrading enzymes | MMP-9 | S | 436 ng/mL (range, 169–705 ng/mL) [133]. | Short [83] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šoša, I. Improving Traditional Post Mortem Healthcare—The Cross-Sectional Use of Blood-Based Biomarkers. Forensic Sci. 2023, 3, 368-380. https://doi.org/10.3390/forensicsci3030028
Šoša I. Improving Traditional Post Mortem Healthcare—The Cross-Sectional Use of Blood-Based Biomarkers. Forensic Sciences. 2023; 3(3):368-380. https://doi.org/10.3390/forensicsci3030028
Chicago/Turabian StyleŠoša, Ivan. 2023. "Improving Traditional Post Mortem Healthcare—The Cross-Sectional Use of Blood-Based Biomarkers" Forensic Sciences 3, no. 3: 368-380. https://doi.org/10.3390/forensicsci3030028
APA StyleŠoša, I. (2023). Improving Traditional Post Mortem Healthcare—The Cross-Sectional Use of Blood-Based Biomarkers. Forensic Sciences, 3(3), 368-380. https://doi.org/10.3390/forensicsci3030028






