Abstract
Background and Objective: Intravenous therapy is widely used in clinics to deliver medications and fluids to patients, and overuse may cause intravenous-infusion-associated circulatory overload (IACO) and death. However, forensic data on deaths from the overuse of intravenous therapy are limited. We performed a retrospective study to identify whether causes of death in forensic practice were associated with IACO. Methods: A total of 572 medical-related cases with a history of intravenous infusion who suffered from injuries or illnesses and died after treatment in hospitals were recruited from two centers of forensic medicine between 2002 and 2018. Results: The results demonstrated that 6.47% of cases (37/572) were exposed to an infusion overdose that resulted in deaths related to IACO, and 43.24% of cases (16/37) had a net fluid retention ranging from 3.0 L/d to 13.8 L/d. The highest case was administered 1.4 L blood products and 13.6 L fluids within 25 h. We observed significant decreases in red blood cells, hematocrit, hemoglobin, and platelets from the time of “on admission” to “before death”, except for white blood cells. Autopsy findings of 16 cases revealed some organ or tissue pathological alterations related to IACO, including pale-yellow liquid overflow under the abdominal epidermis, much transudate in body cavities, and lung edema with a high tissue density and no obvious slurry deposition in the alveolar lumen. Another 21 cases died after a rapid infusion rate ranging from 111 to 293 drops/min, which resulted from viral myocarditis on autopsy. Conclusions: Our data on excessive or irrational use of intravenous therapy indicate a severe circulatory overload, which may eventually result in lethal outcomes. Therefore, the use of improper intravenous therapy should be reduced to ameliorate adverse health consequences during clinical treatment.
1. Introduction
Intravenous (IV) therapy, an effective routine medical treatment in clinical practice, is typically used to correct electrolyte imbalances and deliver medications, blood transfusion, or fluid replacement in patients with dehydration and traumatic hemorrhagic shock [1,2,3]. However, infusion overuse may occur if medical staff or patients do not have adequate knowledge of intravenous therapy. An estimated 16 billion injections are administered annually in underdeveloped countries, and 6.6 billion injections are administered using reused equipment in the absence of sterilization, according to a WHO report [4]. Injection has completely overtaken the real need for this type of administration in certain regions of the world to reach proportions that are no longer based on rational medical treatment. Up to 96% of patients who presented to a primary healthcare provider received an injection in some situations, and over 70% of these injections were unnecessary or could be administered as an oral formulation [4]. Profit-driven overuse of injections and infusions in market-based healthcare systems has become more and more critical as well [5,6]. Statistical publications report that 10.4 billion bottles of medicine were used intravenously in China in 2009, which means that an average of 8 bottles of IV drips per person was used. This average exceeds the world average of 2.5 to 3.3 bottles per person [7]. The irrational use of medications, including the over-prescription of antibiotics, hormones, vitamins, and glucose intravenous infusions, is the biggest problem in China [8].
IV therapy may cause discomfort under permissive infusion volumes or dripping velocities [9]. We previously found numerous cases who died from an excessive infusion through forensic practice [10]. We deemed that administrating a rapid infusion or an extremely large fluid volume may result in circulatory overload. The US Food and Drug Association (FDA) declared that circulatory overload is one of the most frequent complications associated with transfusion-related fatalities [11]. The volume and rate of infusion are the specific risk factors for circulatory overload [12]. However, evidence of deaths in forensic practice is rare. The current study performed a descriptive retrospective study of cases exposed to rapid or extremely large intravenous infusions relating to circulatory overload to gain an understanding of the causation of the overuse of intravenous therapy in forensic practice and stress the importance of regular intravenous infusions in clinics.
2. Materials and Methods
2.1. Study Design
A descriptive retrospective study was implemented after the medical identification of death caused by the Forensic Identification Center of Shantou University (Guangdong, China) and the Institute of Forensic Science, Jiaxing University (Zhejiang, China). A total of 572 medical-related cases were enrolled in the study, and these cases suffered from injuries or illnesses with a history of intravenous infusion and died after treatment in hospitals between 2002 and 2017, excluding the cases that were just sent to the hospital for rescue in a short time or immediately died of trauma or other causes at the crime scene.
All cases were autopsied within 48 h after death. The following individual clinical information was obtained: medical history, reasons for admission and departments, grade of hospitals including third-tier hospitals (with over 500 beds), second-tier hospitals (with 250–500 beds) first-tier hospitals (community hospitals), and clinics according to the classification of Chinese hospitals [13], physical examination, blood biochemical examination, administered fluid therapy (types and amounts of fluid), autopsy and histopathological observation. Experienced pathologists and medico-legists carefully reviewed and checked all data. After reviewing all the data, we analyzed the cause of death [14] of those cases in combination with the medical process and then focused on two types of cases, including those with rapid infusion and heart disease, or at least 4.0 L of net fluid retention per day during admission [15].
2.2. Statistical Analysis
The infusion rate index was calculated using the following equation: the infusion rate index (drops/min) = the volume of fluid intake (mL)/time (min) ×20 drops/mL. We used Wilcoxon signed-rank tests, including paired and two independent samples, to compare the geometric means of routine blood and biochemical indexes from the time of “on admission” to “before death”, and lung weight and density. A statistical p-value lower than 0.05 or 0.01 was considered significant. All data were recorded and analyzed using Microsoft Excel, GraphPad Prism 5, and SPSS software version 16.0.
3. Results
3.1. General Characteristics of the Study Cases
Males accounted for 62.84% of 572 medical-related cases, and 37.16% were female. The age range was 5 to 68 years old (median: 47 y). All cases were distributed amongst infectious diseases (34.4%), orthopedics (25.0%), obstetrics and gynecology (22.6%), pediatrics (12.9%), neurosurgery (3.5%), and others (1.6%) at the beginning of hospitalization (Figure 1a). There were 132 cases from third-tier hospitals, 154 from second-tier hospitals, 97 from first-tier hospitals (community hospitals), and 189 from clinics (Figure 1b).
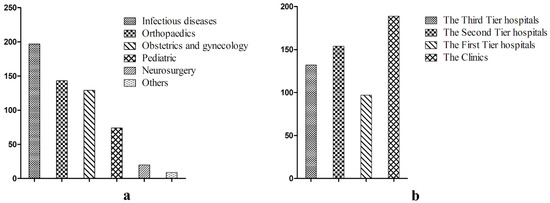
Figure 1.
The general characteristics of the 572 cases. Notes: (a) the disease distribution of the cases; (b) the medical institution distribution of the cases.
3.2. IV-Infusion-Associated Circulatory Overload (IACO)
IACO is a liquid transfusion condition that occurs after the rapid transfusion of a large volume of liquid. A total of 37 cases were exposed to an infusion overdose that resulted in death. Sixteen of these cases had a net fluid retention, and the remaining cases received a relatively rapid infusion accompanied by primary viral myocarditis (Table 1 and Table 2). Clinical reports revealed that the 16 cases with a massive fluid infusion were aged 12 to 53 years (median: 34.5 y) and included 9 males and 7 females who suffered shock because of trauma, infection, or delivery, and accepted high-volume transfusions. Another 21 cases with diagnoses of common cold, upper respiratory tract infection, pneumonia, or acute gastroenteritis died during the infusion treatment process in the hospital or clinic.

Table 1.
The demographic characteristics of the 16 cases of massive fluid infusion.

Table 2.
The demographic characteristics of the 21 cases of rapid infusion.
3.3. IV Fluids and Clinical Laboratory Diagnostics
The amount of IV fluid administered in 16 cases ranged from 3.0 L/d to 13.8 L/d, and the highest administration reached 1.4 L of blood products and 13.6 L of fluids within 25 h. Table 3 shows the total and daily net fluid retention. Cases No. 1 to 7 had a high proportion of colloid fluid administration, such as fresh frozen plasma or whole blood because of active bleeding in the intraperitoneal cavity, and the remaining cases were primarily prescribed crystal fluid (Table 3). The most common type of crystal fluid prescribed was Ringer’s lactate liquid, followed by 5% glucose, normal saline, and others, and some cases were pre-charged with 10% potassium chloride. We also observed a hemodilution and significant decrease in red blood cells, hematocrit, hemoglobin, platelets, potassium ions, sodium ions, and chloride ions from the time of “on admission” to “before death” (p < 0.05). However, there was no significant change in white blood cells because of a severe infection before death in most cases (Table 4).

Table 3.
IV fluid volumes in the 16 cases of massive fluid infusion.

Table 4.
Biochemical outcomes from “on admission” and “before death”.
The average amount of IV fluid administration (1305 ± 605 mL) in 21 cases of rapid infusion was much lower than the 16 cases of massive fluid infusion, and the infusion rate reached approximately 111–293 drops/min, which is 2 times higher than the value recommended by the Chinese Medical Association (Table 5).

Table 5.
IV fluid volumes and rates in the 21 cases of rapid infusion.
3.4. Autopsy Findings
All of the bodies suffered from severe anasarca, except for the primary injury or disease (Figure 2a). Some cases, such as Nos. 3, 5, and 12, had pale-yellow liquids overflowing from subcutaneous soft tissues when making an incision in the epidermis and were diffused with frothy-like edema in subcutaneous soft tissues (Figure 2b,c). A large volume of transudate was found in the body cavities in some cases, especially cases No. 1 to 16, with a varying degree of peritoneal bloody fluid (Table 6). Lungs displayed swollen surfaces, obvious liquid and blood, and a higher tissue density in sections that reached twice the expected normal values [16]. Pulmonary interstitial and alveolar tissues were edematous with the formation of a hyaline membrane and small vessel thrombosis, scattered bleeding, and inflammatory cell infiltration.
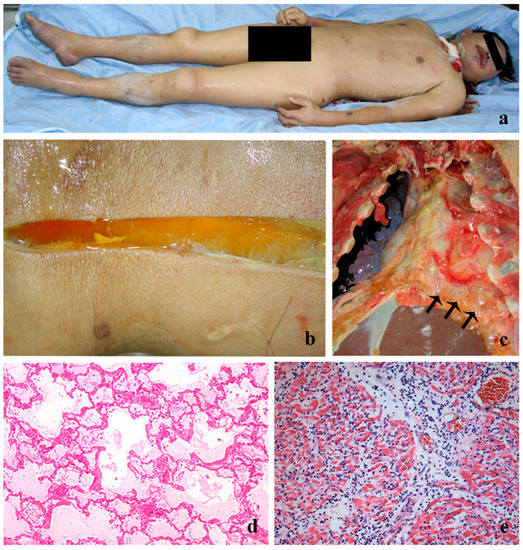
Figure 2.
The pathologic changes of macroscopic and microscopic examination in the 16 cases of massive fluid infusion (a–d) and the 21 cases of rapid infusion (e). Notes: (a) a widespread swelling of the systemic skin; (b) a pale-yellow liquid overflowed from the subcutaneous when making an incision in the epidermis; (c) a diffused frothy-like edema of diaphragm tissues; (d) hypotonic pulmonary edema: formation of hyaline membrane and a blank and lightly staining of alveolar spaces in HE, ×200; (e) diffused infiltration of monocytes and lymphocytes in the myocardial interstitial in HE, ×400.

Table 6.
Lung weight and density and transudate in the cavities.
A slurry deposition was not obvious in alveolar tissues in the 16 cases of the massive fluid infusion, which contradicted the lung edema and higher weight and density of the lungs. The concentration of plasma protein was obviously reduced because the blood was severely diluted after treatment with a large volume of crystalloid solution. The edema fluid was primarily water, and dehydration was observed in hematoxylin-eosin (HE) staining, which showed blank and lightly stained alveolar spaces that are the pathological alterations of hemodilution and severe hypotonic pulmonary edema (Figure 2d). The heart presented significant spherical swelling, highly hydropic degeneration, and an irregular fracture in the myocardium. Diffused edema of the viscera was observed in the brain, liver, kidney, and spleen with cerebellar tentorium hernia, tonsillar hernia formation, and ballooning changes in neurons. Congestion and hemodilution with few blood cells were observed in most vessels of the internal organs.
Effusions were detected in the pleural and pericardial cavities in the 21 cases with rapid infusion, with a smaller volume of transudates in the pleural, peritoneal, and pelvic cavities (p < 0.05) and a similar volume in the pericardial cavity (p > 0.05) compared to the cases of massive fluid infusion. Pulmonary edema was smaller in the rapid infusion cases compared to the massive fluid infusion cases (Table 6). The heart was soft, and the apex was round and obtuse. The histopathological features were quite typical with the following changes (Figure 2e): (1) swollen myocardial interstitium, (2) diffuse infiltration of monocytes and lymphocytes, and (3) splitting of myocardial fibers into cord-like fibers with some irregular fracture of the myocardium. These pathological alterations in 21 cases were finally diagnosed as viral myocarditis.
4. Discussion
Intravenous infusion is the most direct and effective treatment delivery in modern clinics. An overuse of intravenous injections and infusions might occur in the absence of rational management for healthcare nurses. A previous study examining 230,800 prescriptions in 784 community health institutions from 28 cities in China between 2007 and 2009 demonstrated substantial overprescribing, including twice as many prescriptions for antibiotics as recommended by the WHO and rates of injection that was three times higher than rates in similar countries [17]. The number of adverse drug reaction reports to anti-infective agents ranked first in 2017 and accounted for 42.3% of all chemical drugs according to the Annual Report for National Adverse Drug Reaction Monitoring [18]. For example, intravenous injections account for 61.0% of all drug doses in 2017, which rose by 2.1% compared to 2016 [18,19].
The present study found a comparably high use of intravenous therapy and a high composition ratio of medical issues. These observations may be a consequence of poor investment in the healthcare system and the relatively low salaries for doctors in certain areas [7,20]. The reduced subsidy for healthcare and an inappropriate incentive system makes hospitals and doctors seek greater profit. For example, bonuses for physicians, which make up a large share of their total compensation, are linked to the revenue they generate for the hospital. Fortunately, realigning the incentive system for China’s healthcare is underway, such as a “zero profit” policy excluding some drugs, since 2013 to prevent or reduce physicians and hospitals from receiving greater rebates from increased prescriptions and an appropriate increase in the proportion of performance bonuses in total salary to increase the difference in the distribution of gross income for physicians [21]. On the other hand, some doctors may not receive a good health education and may ignore routine medical practices for diseases. Notably, inadequate knowledge and the suboptimal prescribing of fluids and electrolytes were discovered in 25 British hospitals [22]. However, there are no relevant data in China. Some errors, such as a lack of weight monitoring during admission, uncontrolled hemorrhaging, fluid imbalance, and no fluid restriction with acute renal insufficiency upon admission, resulted in an extremely large amount of fluid administration in our study. However, the elevated use of intravenous injections is demanded by patients who want an injection instead of oral medication, which would provide the same recovery [7]. Therefore, the mode of treatment delivery often seems more important than the outcome. Some patients take the initiative to go to outpatient or individual clinics for an infusion to achieve faster recovery because of personal reasons, as reported previously [7] and in the current study.
Intravenous therapies for patients include blood products, antibiotics, crystalloid solutions, hormones, vasodilators, some anesthetics, and parenteral nutrition. IV therapy is accidentally accompanied by circulatory overload, acute lung injury, hemolytic transfusion reactions, microbial infection, or other types of adverse reactions. Advances in blood-donor procurement procedures and infusion techniques have remarkably relieved the incidence of blood transfusion complications, but the impact on intravenous-therapy-associated IACO continues to be underestimated. Accumulating evidence reveals that numerous complications occur during IV therapy, such as tissue infiltration, bloodstream infection, vascular laceration, air embolism, fluid overload, phlebitis, incompatible drug co-infusion, and some medication errors (e.g., incorrect administration of drugs or doses) [23]. Drugs that are administered via direct IV injection likely exhibit 100% bioavailability, especially in cases of circulatory failure. However, only half of the cases can increase cardiac output due to inter-individual variability in the relationship between cardiac output and preload [24]. On the other hand, irrational intravenous therapy and fluid management may cause much higher risks than any other route of administration [25]. Drugs are delivered to the target site rapidly with IV infusion, but the risk of overload is increased if the volume was calculated incorrectly or ignored, and an increased opportunity of side effects occurs if the drug is administered too rapidly [12,26,27,28,29]. Studies have shown that increased fluid balance was independently associated with the mortality of patients in shock, especially during septic shock, and with an increased rate of postoperative complications [30,31].
Fluid overload was detected in cases of massive fluid infusion in the current study. A large volume of colloid liquids, such as plasma and whole blood, and crystal fluids were administered under the condition of uncontrolled active bleeding in cases No. 1 to 7. However, studies in vivo and clinical research on uncontrolled hemorrhaging demonstrated that aggressive fluid resuscitation increases blood pressure, reverses vasoconstriction, dislodges early thrombi, reduces blood loss, causes a dilutional coagulopathy, and reduces oxygen delivery [32,33]. Excessive crystal fluids accumulated daily during admission in all cases. There is no doubt that pulmonary edema will occur due to excessive fluid retention [29] and end with acute respiratory distress syndrome (ARDS) and death [34]. An extreme hemodilution may also have exerted a deleterious effect on patients with trauma to a different degree in the current study. Factors such as electrolyte imbalance and diminution in physiological hormone concentrations [35] and trace elements [36,37,38] may concurrently result in multiple organ failure and death.
Our data further indicated that 21 cases of viral myocarditis with a rapid infusion rate were misdiagnosed with acute upper respiratory tract infection or acute gastroenteritis. A careful history and thorough clinical assessment, including ECG and further diagnostic tests, should be performed despite the absence or limited clinical or imaging findings for myocarditis [39]. This procedure is recommended because viral myocarditis can present as a mild disease without any symptoms but may cause chest pain, heart failure, or sudden death [40]. Some medications, including diuretics, are used to prevent or treat fluid overload because of the high incidence of left ventricle dysfunction [41]. Therefore, a relatively massive and rapid infusion over a short period of time in myocarditis patients without a clearer diagnosis may be fatal because the infusion may result in acute pulmonary edema and circulatory overload, aggravate congestive heart failure, and lead to sudden death. The infusion of antibiotics has no effect against viral infections, which result in acute upper respiratory tract infections, such as the common cold [42]. ECG examinations are necessary before infusion, especially for patients who have heart disease with no obvious symptoms or an unconfirmed diagnosis.
5. Conclusions
In conclusion, some extreme consequences were found in IACO-related death cases, such as pale-yellow liquid overflow under the abdominal epidermis, a large volume of transudate in body cavities, and severe hypotonic pulmonary edema with no obvious slurry deposition in the alveolar lumen. This study highlights the suboptimal infusion practices that may cause an acute hypotonic pulmonary edema that results in severe IACO and ends with death. Therefore, an assessment of IACO risk factors prior to an infusion and fluid management monitoring for patients are needed, and essential healthcare policies to reduce the overuse of intravenous therapy and strengthen the training for doctors are required in the future.
However, there are limitations to this work. Subjects in the massive infusion cases were focused on patients who are diagnosed with certain diseases during admission. They were presented with a variety of diseases but the treatment criteria from different hospitals might not be consistent. Thus, the fluid volumes during transfusion therapy varied with their disease situation. We just retrospectively calculated the amount of fluid intake and output, and it was difficult to identify whether the massive infusion was caused directly by the disease itself or malpractice. Furthermore, the cases in the rapid infusion generally lacked detailed medical history and we could only make an excluded pathological death diagnosis from autopsy findings. Therefore, a further study should be performed in clinical cases to validate these findings in forensic practice.
Author Contributions
Conceptualization, G.X. and X.Y.; methodology, G.X., R.S., J.L., L.X., X.J., D.C. and B.H.; software, R.S.; validation, G.X., R.S. and X.Y.; formal analysis, G.X. and R.S.; investigation, J.L. and R.S.; resources, G.X., R.S. and X.Y.; data curation, R.S.; writing—original draft preparation, G.X. and R.S.; writing—review and editing, X.Y.; supervision, X.Y.; project administration, X.Y.; funding acquisition, G.X. and X.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financially supported by the National Natural Science Foundation of China (grant Nos. 30772458 and 81072508 to Yu X) and the Major Transverse Research Projects of Jiaxing University, China (grant No. 00619006 to Xu G).
Institutional Review Board Statement
All forensic death cases were offered by the Public Security Bureau or Health Commission of Shantou, Chaozhou, Jieyang (all in Guangdong Province, China), and Jiaxing (in Zhejiang Province, China). Medicolegists and pathologists performed all integrated pathological autopsies to inspect organs and tissues from the cranial cavity, chest-abdomen-pelvic cavity, and spinal cord. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of (approval no. SUMC-2018-029).
Informed Consent Statement
Informed consent was obtained from all bereaved family members of subjects involved in the study.
Data Availability Statement
The authors will provide raw data to support the conclusions of this research without reservation.
Acknowledgments
The sponsors of the study were not involved in study design, data collection, data analysis, data interpretation, or writing of the manuscript. We apologize to all those researchers whose work could not be cited due to space limitations.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kuttab, H.I.; Lykins, J.D.; Hughes, M.D.; Wroblewski, K.; Keast, E.P.; Kukoyi, O.; Kopec, J.A.; Hall, S.; Ward, M.A. Evaluation and Predictors of Fluid Resuscitation in Patients with Severe Sepsis and Septic Shock. Crit. Care Med. 2019, 47, 1582–1590. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L. Fluid management in the critically ill. Kidney Int. 2019, 96, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Meyhoff, T.S.; Hjortrup, P.B.; Wetterslev, J.; Sivapalan, P.; Laake, J.H.; Cronhjort, M.; Jakob, S.M.; Cecconi, M.; Nalos, M.; Ostermann, M.; et al. Restriction of Intravenous Fluid in ICU Patients with Septic Shock. New Engl. J. Med. 2022, 386, 2459–2470. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guideline on the Use of Safety-Engineered Syringes for Intramuscular, Intradermal and Subcutaneous Injections in Health-Care Settings; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Dong, L.; Yan, H.; Wang, D. Antibiotic prescribing patterns in village health clinics across 10 provinces of Western China. J. Antimicrob. Chemother. 2008, 62, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Song, F.; Gong, Y.; Tu, X.; Wang, Y.; Cao, S.; Liu, J.; Lu, Z. A systematic review of antibiotic utilization in China. J. Antimicrob. Chemother. 2013, 68, 2445–2452. [Google Scholar] [CrossRef]
- Yuan, S. China should reduce the overuse of intravenous infusion. BMJ 2014, 348, g1262. [Google Scholar] [CrossRef] [PubMed]
- WHO. China-WHO Country Cooperation Strategy (2016-2020); WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Hilton, A.K.; A Pellegrino, V.; Scheinkestel, C.D. Avoiding common problems associated with intravenous fluid therapy. Med. J. Aust. 2008, 189, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Wang, W. Death caused by circulatory overload in the treatment of traumatic hemorrhagic shock: Two cases report. J. Law Med. 2002, 9, 137–138. [Google Scholar]
- FDA. Fatalities Reported to FDA Following Blood Collection and Transfusion: Annual Summary for Fiscal Year 2009; FDA: Silver Spring, MD, USA, 2010.
- Li, G.; Rachmale, S.; Kojicic, M.; Shahjehan, K.; Malinchoc, M.; Kor, D.J.; Gajic, O. Incidence and transfusion risk factors for transfusion-associated circulatory overload among medical intensive care unit patients. Transfusion 2011, 51, 338–343. [Google Scholar] [CrossRef]
- Li, X.; Huang, J.; Zhang, H. An analysis of hospital preparedness capacity for public health emergency in four regions of China: Beijing, Shandong, Guangxi, and Hainan. BMC Public Health 2008, 8, 319. [Google Scholar] [CrossRef]
- Yu, X.; Wang, H.; Feng, L.; Zhu, J. Quantitative Research in Modern Forensic Analysis of Death Cause: New Classification of Death Cause, Degree of Contribution, and Determination of Manner of Death. J. Forensic Res. 2014, 5, 221. [Google Scholar]
- Arieff, A.I. Fatal postoperative pulmonary edemapathogenesis and literature review. Chest J. 1999, 115, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Bai, R.; Yu, X.; Wang, D.; Lv, J.; Xu, G.; Lai, X. The Densities of Visceral Organs and the Extent of Pathologic Changes. Am. J. Forensic Med. Pathol. 2009, 30, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, J.; Wang, F.; Wang, B.; Liu, L.; Hou, W.; Fan, H.; Tong, Y.; Zhang, J.; Lu, Z. Overprescribing in China, Driven by Financial Incentives, Results in Very High Use of Antibiotics, Injections, and Corticosteroids. Health Aff. 2012, 31, 1075–1082. [Google Scholar] [CrossRef]
- FDA. 2017 Annual Report for National Adverse Drug Reaction Monitoring; FDA: Silver Spring, MD, USA, 2018.
- FDA. 2016 Annual Report for National Adverse Drug Reaction Monitoring; FDA: Silver Spring, MD, USA, 2017.
- Blumenthal, D.; Hsiao, W. Privatization and Its Discontents — The Evolving Chinese Health Care System. New Engl. J. Med. 2005, 353, 1165–1170. [Google Scholar] [CrossRef]
- Ma, X.; Wang, H.; Yang, L.; Shi, L.; Liu, X. Realigning the incentive system for China’s primary healthcare providers. BMJ 2019, 365, l2406. [Google Scholar] [CrossRef]
- Lobo, D.; Dube, M.; Neal, K.; Simpson, J.; Rowlands, B.; Allison, S. Problems with solutions: Drowning in the brine of an inadequate knowledge base. Clin. Nutr. 2001, 20, 125–130. [Google Scholar] [CrossRef]
- Kwan, I.; Bunn, F.; Chinnock, P.; Roberts, I. Timing and volume of fluid administration for patients with bleeding. Cochrane Database Syst. Rev. 2014, 2014, CD002245. [Google Scholar] [CrossRef] [PubMed]
- Monnet, X.; Shi, R.; Teboul, J.L. Prediction of fluid responsiveness. What’s new? Ann. Intensive Care 2022, 12, 46. [Google Scholar] [CrossRef]
- John, G.P.; Arthur, K.; John, O.G. The Textbook of Pharmaceutical Medicine; Wiley-Blackwell: Hoboken, NJ, USA, 2013. [Google Scholar]
- Cotter, G.; Metra, M.; Milo-Cotter, O.; Dittrich, H.C.; Gheorghiade, M. Fluid overload in acute heart failure - Re-distribution and other mechanisms beyond fluid accumulation. Eur. J. Hear. Fail. 2008, 10, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, M.; E Villamin, C.; E Murphy, L.; Dasgupta, A.; Bassett, R.L.; Medina, M.C.; Bates, T.S.; Martinez, F.; Couchonal, A.M.K.; Klein, K.; et al. Oncology Patients Who Develop Transfusion-Associated Circulatory Overload: An Observational Study. Lab. Med. 2022, 53, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, L.; Maskens, C.; Cserti-Gazdewich, C.; Hansen, M.; Lin, Y.; Pendergrast, J.; Yi, Q.L.; Callum, J. A Retrospective Review of Patient Factors, Transfusion Practices, and Outcomes in Patients with Transfusion-Associated Circulatory Overload. Transfus. Med. Rev. 2013, 27, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Lowell, J.A.; Schifferdecker, C.; Driscoll, D.F.; Benotti, P.N.; Bistrian, B.R. Postoperative fluid overload: Not a benign problem. Crit. Care Med. 1990, 18, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Messina, A.; Robba, C.; Calabrò, L.; Zambelli, D.; Iannuzzi, F.; Molinari, E.; Cecconi, M. Perioperative liberal versus restrictive fluid strategies and postoperative outcomes: A systematic review and metanalysis on randomised-controlled trials in major abdominal elective surgery. Crit. Care 2021, 25, 205. [Google Scholar] [CrossRef] [PubMed]
- Tigabu, B.M.; Davari, M.; Kebriaeezadeh, A.; Mojtahedzadeh, M. Fluid volume, fluid balance and patient outcome in severe sepsis and septic shock: A systematic review. J. Crit. Care 2018, 48, 153–159. [Google Scholar] [CrossRef]
- Boyd, J.H.; Forbes, J.; Nakada, T.-A.; Walley, K.R.; Russell, J.A. Fluid resuscitation in septic shock: A positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit. Care Med. 2011, 39, 259–265. [Google Scholar] [CrossRef]
- Nolan, J. Fluid resuscitation for the trauma patient. Resuscitation 2001, 48, 57–69. [Google Scholar] [CrossRef]
- Gattinoni, L.; Cressoni, M.; Brazzi, L. Fluids in ARDS: From onset through recovery. Curr. Opin. Crit. Care. 2014, 20, 373–377. [Google Scholar] [CrossRef]
- Desborough, J. The stress response to trauma and surgery. Br. J. Anaesth. 2000, 85, 109–117. [Google Scholar] [CrossRef]
- Hu, B.; Wu, Y.; Tong, F.; Liu, J.; Shen, X.; Shen, R.; Xu, G. Apocynin Alleviates Renal Ischemia/Reperfusion Injury Through Regulating the Level of Zinc and Metallothionen. Biol. Trace Element Res. 2016, 178, 71–78. [Google Scholar] [CrossRef]
- Paynejames, J.; Mcgovern, C.; Jones, R. Simpson’s Forensic Medicine, 13th ed.; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Xu, G.; Su, R.; Li, B.; Lv, J.; Sun, W.; Hu, B.; Yu, X. Trace element concentrations in human tissues of death cases associated with secondary infection and MOF aftersevere trauma. Biol. Trace Elem. Res. 2015, 168, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Cooper, L.T., Jr. Myocarditis. N. Engl. J. Med. 2009, 360, 1526–1538. [Google Scholar] [CrossRef] [PubMed]
- Magnani, J.W.; Dec, G.W. Myocarditis: Current trends in diagnosis and treatment. Circulation 2006, 113, 876–890. [Google Scholar] [CrossRef] [PubMed]
- Kenealy, T.; Arroll, B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst. Rev. 2013, 2013, CD000247. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).