Human-Centred Design (HCD) in Enhancing Dementia Care Through Assistive Technologies: A Scoping Review
Abstract
1. Introduction
2. Objectives
- What types of assistive technologies have been developed using HCD approaches for people with dementia?
- To what extent, and in what ways (how) are people with dementia and other stakeholders involved in the design process?
- What are the reported HCD approaches and frameworks in this context?
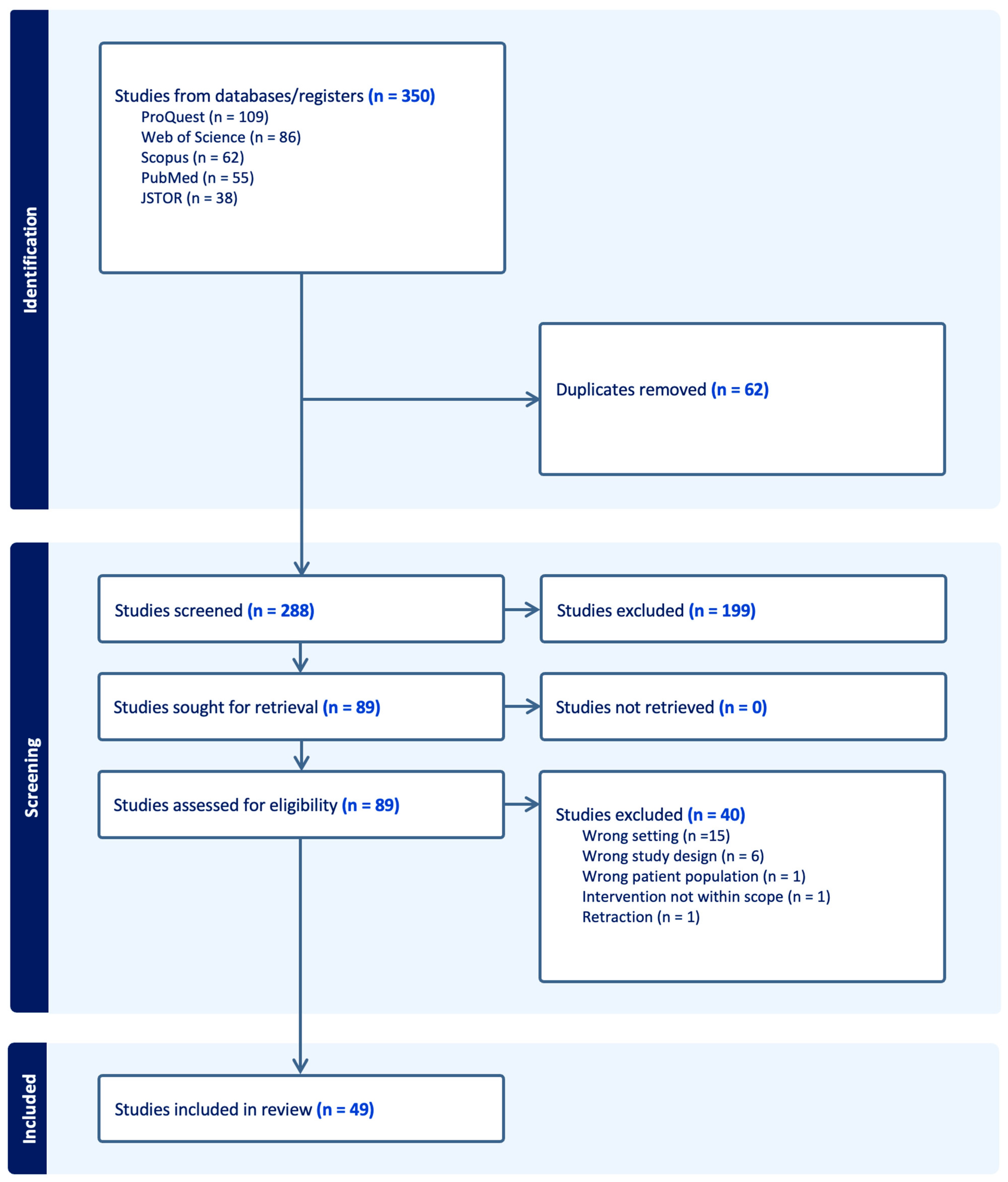
3. Methods
3.1. Scoping Review Framework
3.2. Eligibility Criteria
- Population: People living with dementia, encompassing all stages and types of the condition. In addition to studies that involved people with dementia, this review also included studies if they also incorporated the perspectives and experiences of carers and family members, recognising their central role in the design, use, and implementation of assistive technologies.
- Concept: HCD approaches, including user-centred design, participatory design, co-design, and other methodologies that engage people with dementia and/or their carers in the development or evaluation of assistive technologies.
- Context: Any dementia care setting, including individuals living independently in the community as well as those in institutional environments such as residential aged care facilities. This broad inclusion was intended to capture a comprehensive understanding across diverse care environments and stages of dementia.
| PCC Framework | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | People with dementia, and/or their caregivers | Focus on populations other than people with dementia or their caregivers |
| Concept | Human-centred design approaches, including user-centred design, participatory design, co-design, and other methodologies that engage people with dementia and/or their carers | Focus solely on patient-centred care without any human-centred design components. |
| Context | Any care setting | n/a |
3.3. Literature Search
3.4. Study Selection
3.5. Data Extraction and Synthesis
4. Results
5. Discussion
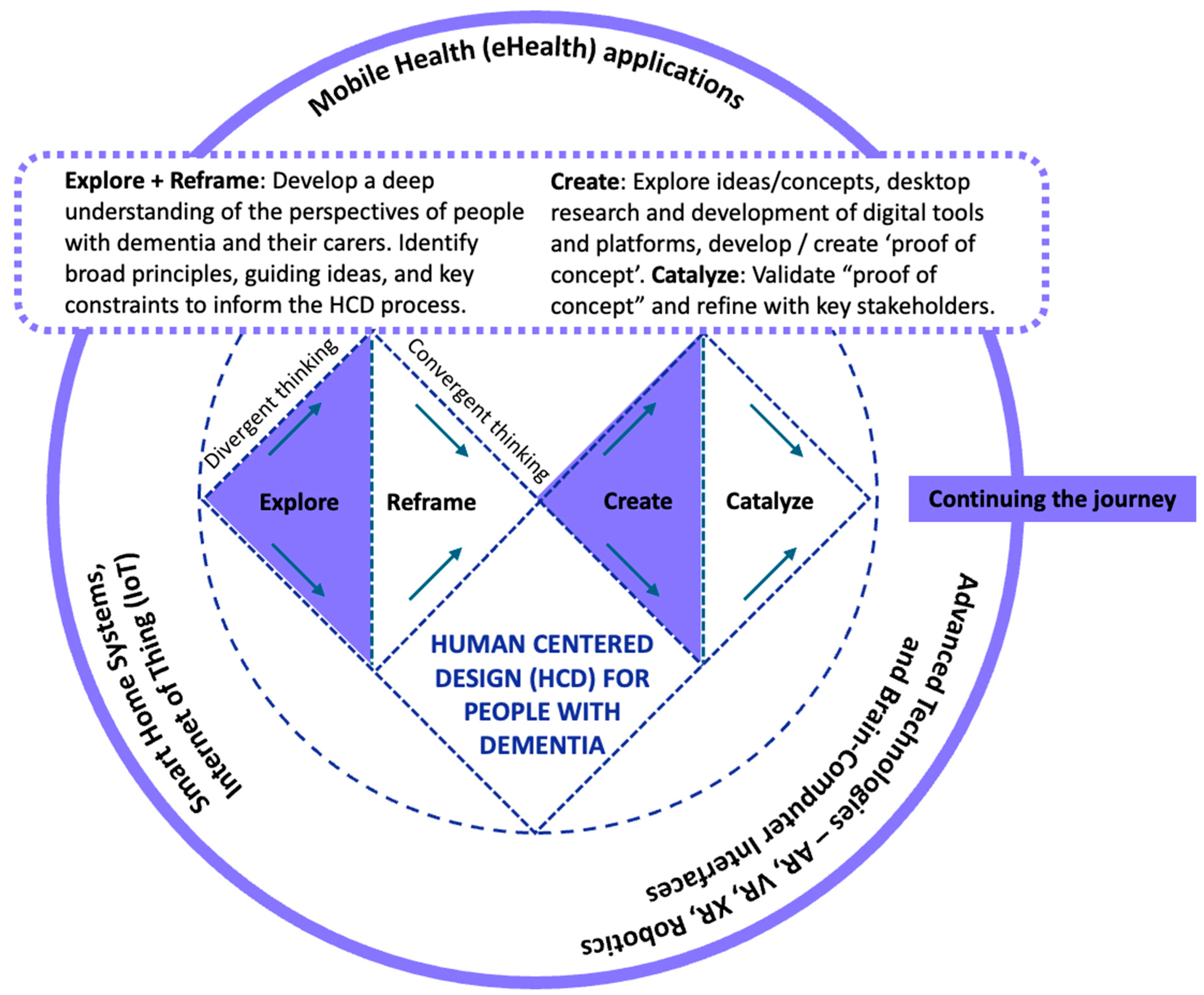
5.1. Diversity of Technologies and Areas of Innovation
- Explore + Reframe: Gain a deep understanding of the perspectives of people with dementia and their carers. Identify broad principles, guiding ideas, and key constraints that inform the HCD process.
- Create + Catalyse: Generate and prototype ideas, leading to the development of products (e.g., digital tools), services, and systems (e.g., platforms). Develop a proof of concept, then validate and refine it in collaboration with key stakeholders, including people with dementia and their carers.
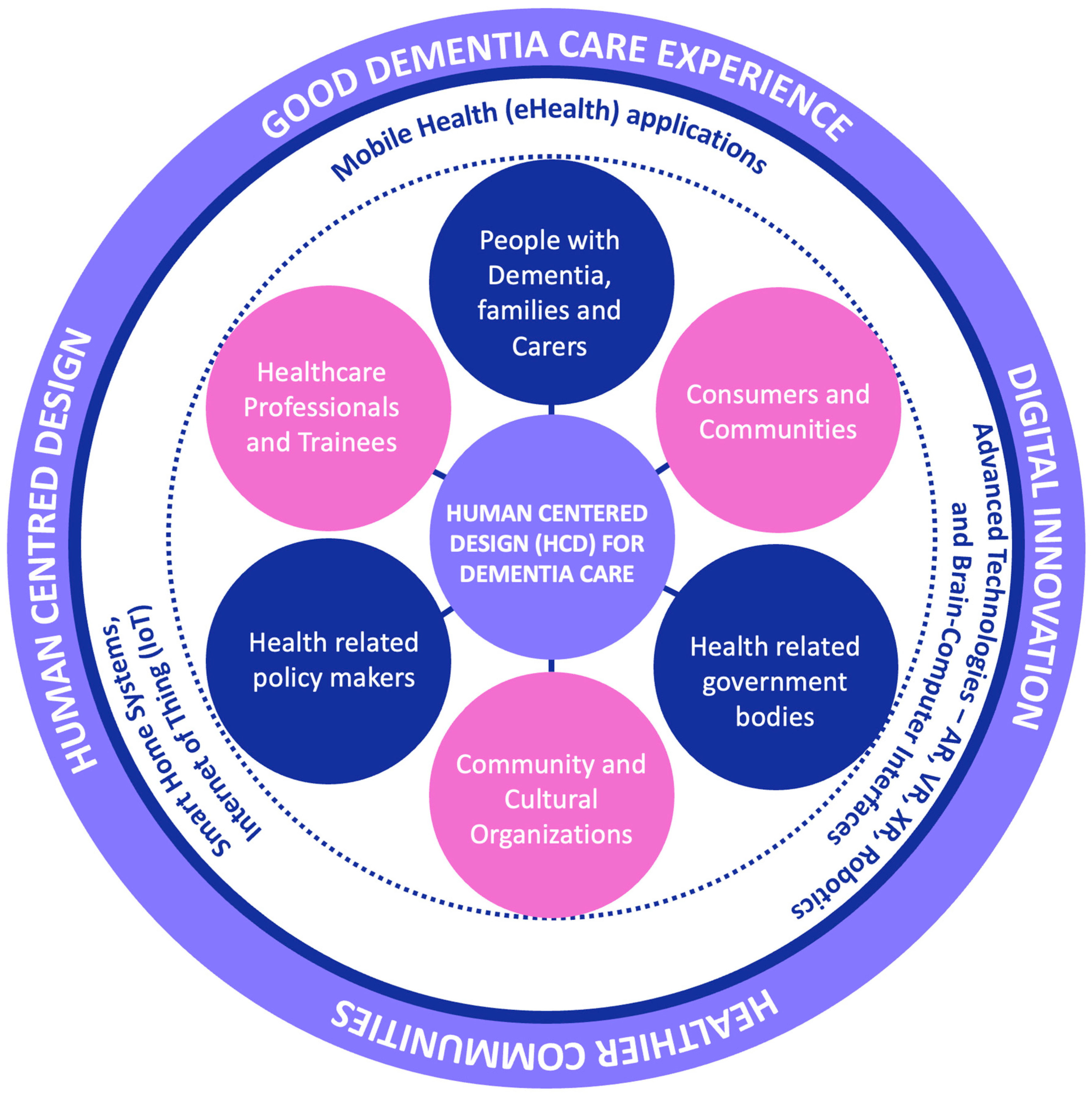
5.2. Patterns in Stakeholder Involvement and Design Frameworks
5.3. Methodological Approaches and Identified Gaps
5.4. Emerging Themes and Trends
6. Limitations in the Literature
7. Implications for Future Research and Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Definitions
Appendix B. Overview of Assistive Technologies, Stakeholder Involvement and HCD Methods and Methodologies
| Study Ref | Methodology | Stakeholders | Technologies |
|---|---|---|---|
| [2] Multiple (Germany, Italy, Portugal, Romania, Spain) Journal Research Article | Qualitative; semi-structured interviews with diverse stakeholders. The study serves as both an evaluative and planning tool for future user-centred design. | Strongly emphasised, with engagement across multiple sectors and roles. | ICT-based healthcare platforms, specifically aimed at supporting care for dementia and Parkinson’s disease. |
| [35] Australia Journal Literature review | Review, with a focus on personal stories and user feedback. | Emphasised, with a focus on adapting technology to meet the needs of individuals with dementia. | Augmented Reality, Microsoft HoloLens, smart mirrors, etc., are used as assistive technologies for dementia care. |
| [30] UK Conference Proceedings (Full Paper) | Co-design, with a focus on the PERCEPT approach to engage vulnerable user groups in the design process. | Emphasised through the co-creation of personas with users, ensuring that the design is grounded in the needs of the end-users. | The focus is on a smart home toolset for individuals with early-stage dementia or Parkinson’s. |
| [10] Norway Journal Systematic Review | A systematic review of qualitative, quantitative, and mixed-method studies, which provides insights into adoption barriers and facilitators. | High emphasis on involving relevant stakeholders, including people with dementia and caregivers. | The study focuses on the implementation and adoption of assistive technology and telecare, including wearables, assistive robots, React app, sensors, remote monitoring technology, etc. |
| [16] UK Journal Scoping Review | Scoping review, with a focus on digital technologies supporting the well-being of people with dementia. | High emphasis on involving people with dementia, family carers, and care professionals in the design and evaluation of technologies. | Focus on measuring engagement and well-being outcomes of assistive technology use. |
| [43] USA Journal Research Article | Quantitative; UX-oriented (heuristic evaluation and card sorting), not participatory or co-creative. | The study reflects an awareness of cultural user needs but lacks direct involvement from users or carers. | Mobile health (mHealth) apps for Alzheimer’s, sourced from public app stores. |
| [59] UK Journal Conceptual Paper | A broad range of qualitative, quantitative, and participatory approaches across the articles is discussed. | Involvement of users, families, clinicians, and lived experience contributors is a consistent theme. | From basic aids to advanced smart systems and digital tools, including Augmentative and Alternative Communication (AAC) devices, smart home tech, textured insoles, and brain-computer interfaces. |
| [50] Spain Journal Evaluation | Qualitative; user-centred, iterative, and evaluative through ecological testing and planned clinical trials. | Strongly emphasised: users, caregivers, professionals, and healthcare systems are considered. | TV-based support system (smart TV), video conferencing, remote monitoring, and cognitive support tools. |
| [23] USA, Mexico Journal Research Article | Mixed methods; framework-based, with application to a case study; follows an iterative and participatory design process informed by HCD/HCAI. | Emphasised as a core element of the framework. Stakeholder needs and perspectives are integrated into design and evaluation. | Socially Assistive Robots (SARs), with application in Cognitive Stimulation Therapy. |
| [28] Spain Journal Research Article | Mixed methods, including usability testing, task-based evaluation, and qualitative analysis. | Occupational therapists were involved as co-designers and evaluators. People with dementia were not directly engaged. | Reminiscence therapy planning app for therapists. |
| [27] Portugal Journal Research Article | Mixed methods; design-based research, user-centred design, and quantitative user experience evaluation. | Therapists, caregivers, and nutritionists were involved in requirements gathering; caregivers participated in usability testing and feedback. | Mobile app for food plan management and nutritional monitoring. |
| [29] USA Journal Research Article | Mixed methods; combining qualitative feedback from caregivers with quantitative usability testing to evaluate the platform’s effectiveness. Use of Design Thinking and iterative testing with caregivers as primary users. Involvement of diverse racial and ethnic groups. | Active and participatory, with dementia caregivers providing continuous feedback throughout the design and evaluation phases, ensuring the platform meets their specific needs. | A platform to provide personalised resources for dementia caregivers, with a focus on financial and legal assistance. It uses a Personalisation Algorithm to tailor information based on user needs. |
| [39] Belgium Journal Research Article | Mixed methods (interviews, surveys, usage data), pre-post-test design with continuous follow-up. | Both people with dementia and family caregivers are involved, particularly in evaluating the tool in real-life conditions. | Web-based advance care planning tool. |
| [33] Austria Journal Conceptual Paper | Framework proposal: user-centred via UX/design thinking, digitally enabled. | User perspective is central; professional stakeholders are engaged through the framework. | Building Information Modelling (BIM) and Internet of Things (IoT), applied to therapeutic environments for dementia care. |
| [36] UK (York) Conference Proceedings (Full Paper) | Mixed methods; multi-phase user-centred methodology including design requirement gathering, system development, and user testing through interviews and surveys. | Dementia caregivers were involved from the discovery and definition stage through to evaluation. | Chatbot for dementia caregiver support (structured vs. generative AI models) |
| [37] Peru Journal Research Article | Mixed methods; multi-phase, including qualitative user input and contextual field observations. | Stakeholders informed the design, tested the chatbot, and shaped context-specific insights and recommendations. | AI-powered chatbot (‘Ana’) for dementia caregiving, tested in both predefined and generative formats; use of WhatsApp as a delivery platform. |
| [26] UK Journal Research Article | Qualitative; Agile, iterative development with formalised co-design structures; user testing and feedback clearly inform final product design. | Strongly emphasised, with meaningful and iterative input from both people living with dementia and their care partners. | Smartphone app (mHealth), designed to track cognitive performance in people with dementia. |
| [41] UK Conference Proceedings (Full Paper) | Qualitative, user-requirement driven. | Clear involvement of patients and informal caregivers through interviews, with distinct needs identified and respected. | Health/home monitoring platforms, with a focus on self-management and care customisation. |
| [40] USA Conference Proceedings (Full Paper) | Qualitative; iterative, user-informed design, with co-created mock-ups indicating a practical application of HCD. | Involves patients, caregivers, and healthcare professionals across multiple clinical sites. | Mobile application (Patient Empowerment Platform) designed for dementia-related multimorbidity care. |
| [32] Germany Journal Research Article | Mixed methods, including structured observation, self-report questionnaires, and qualitative content analysis. | Participants with dementia were directly involved in evaluation and their input was used to assess and prioritise features. | Smartwatch-based assistive technology, used for prompting daily activities and cognitive tasks. |
| [12] Australia Journal Systematic review | Systematic review: summarising design attributes relevant to the field. | Stakeholders are emphasised as necessary in the design process, though actual involvement is discussed at a conceptual level based on secondary evidence. | Socially Assistive Robots (SARs) are used in dementia care. |
| [72] USA Journal Research Article | Qualitative, using semi-structured interviews and affinity diagramming to develop personas, reflecting the user-centred nature of the design process. | Strong stakeholder involvement, with direct input from rural caregivers, community partners, and a study advisory board. | While the study does not focus on a specific technology, the personas created in the study are meant to guide the design of interventions and technologies that address the unique needs of rural caregivers. |
| [31] UK Journal Research Article | Case report, with a focus on implementation strategy using HCD principles. | Inclusion of healthcare managers and informal care partners. | Supportive smart home technology in a hospital alternative level of care setting. |
| [14] USA Journal Scoping review | Scoping review, with thematic analysis, mapping support functions to human needs. | Not directly enacted in this study. | Mobile technologies (various functions, including tracking, memory aids, and social engagement). |
| [52] Italy Journal Research Article | Mixed methods; participatory design case study, combining reflective practice with practical co-creation. | People with dementia participating as expert co-creators. | eHealth and mHealth apps co-designed with people living with dementia. |
| [57] Germany Journal Research Article | Qualitative; interviews with thematic analysis, using fictional vignettes to explore contextualised user perspectives. | Includes direct engagement with people with dementia and caregivers to explore perceptions and ethical concerns. | GPS tracking, dressing aids, and emotion recognition tools. |
| [17] UK Journal Scoping Review | Scoping review: reflects on state of the field and suggests methodological improvements rooted in HCD principles. | Limited in existing studies but strongly advocated for in future work. | Technology for arts-based activities; supporting music, storytelling, and visual arts for older adults with MCI or dementia. |
| [60] The Netherlands Journal Evaluation | Conceptual paper describing the theory and implementation of HCD in healthcare; although not specific to dementia, it offers valuable insights for framing, assessing, and guiding HCD-based research and development in dementia-related technology. | Emphasised as a core HCD element. | Not applicable—this paper is not about a specific device or intervention. |
| [22] Multiple (Austria, Cyprus, Poland) Journal Research Article | Mixed methods; market research to identify user preferences, followed by prototype development and iterative user feedback collection. | The system design is informed by both users with dementia and caregivers, with feedback mechanisms in place. | eSticky reminder system using ePaper displays, base station, and web platform. |
| [34] USA Journal Conceptual Paper | The paper integrates experiences from several studies, both experimental and observational, focusing on the usability and acceptability of passive sensing technology. | End-users (older adults, including those with dementia) and research staff are both considered, with strategies mentioned to address the challenges faced by these groups. | Remote passive sensing technology, used to monitor older adults’ activities and functions for behavioural interventions in home settings |
| [51] Denmark Conference Paper Evaluation | Qualitative: workshops with stakeholders as part of a design process. | The study involves significant stakeholder feedback from multiple sources (caregivers, healthcare professionals, and local government). | Focuses on electronic tagging and tracking technologies. |
| [47] Belgium Journal Research Article | Mixed methods; iterative usability testing (think-aloud, SUS, interviews), guided by formal development frameworks. | People with dementia, caregivers, dyads, and PPI contributors were involved across multiple stages of design and evaluation. | Web-based advance care planning tool. |
| [48] Belgium Journal Research Article | Mixed methods (quantitative usability metrics and qualitative feedback), supporting the depth and rigour of user engagement. The study employs a structured and iterative development process with meaningful involvement from end-users and stakeholders. | Strongly emphasised, with direct involvement from people with dementia, caregivers, and a stakeholder advisory group. | A user-centred, interactive website for advanced care planning in dementia care. |
| [15] Australia Journal Scoping Review | Scoping Review: examining the outcomes of robotics and multimedia technologies in residential care settings. | The study includes evidence on the needs of residents with dementia but does not specifically engage them. | Focuses on robotics and multimedia computer programs for engagement and interaction. |
| [42] Australia Journal Research Article | Qualitative; two-phase co-design approach with expert-informed input, resulting in a prototype application. | Direct and meaningful; includes caregivers and professionals across relevant disciplines. | Android-based mHealth application for caregivers of people with dementia. |
| [45] USA Journal Research Article | Mixed methods; early-stage user-centred design using surveys and a mock-up apartment for pilot testing. | Family caregivers are directly involved. | Mobile interface for cognitive assistive technology (CAT) to support IADLs. |
| [54] USA Journal Conceptual/Protocol Paper | Mixed methods; following recognised NIH intervention development stages, combined with participatory design. | People with dementia, caregivers, care providers, designers, and researchers are involved. | Innovative bio-experiential platform aimed at enhancing emotional health and engagement for dementia dyads. |
| [13] USA Journal Systematic Review | Systematic review, synthesising findings from existing literature to assess the effectiveness and gaps in current remote monitoring technologies. | Strong focus on patients, caregivers, and healthcare professionals, with a call for improved evaluation of these technologies in relation to their usability and privacy concerns. | Remote monitoring technologies, including wearables, environmental sensors, and smart home systems, are designed to support patients with Alzheimer’s and ease caregiver burden. |
| [55] Canada Journal Research Article | Qualitative; participatory, iterative, consistent with HCD and co-design principles. | Direct involvement of people with MCI/EOD and their care partners in shaping design. | Focus on workplace technologies for people with mild cognitive impairment/early onset of dementia. |
| [46] Canada Journal Research Article | Mixed methods; secondary quantitative analysis of real-world interactions, persona development, and design recommendations in conceptual and design-preparatory phases. It uses an evidence-based approach to develop realistic user personas, which are then used to generate context-sensitive design recommendations. | Indirect stakeholder involvement, via video-based behavioural analysis, but robust in capturing real user needs. | The focus is on informing the design of assistive technologies for cognition, not a specific product, but the recommendations are tailored for tech supporting executive function in people with dementia. |
| [11] UK Journal Systematic Review | Systematic review, with an emphasis on carer experience and ethical concerns. | Carers are the focus of the review, but not active participants in the design processes of the technologies covered. | Broad spectrum of assistive devices for home-based dementia care (e.g., medication dispensers, wearables, trackers, robotic aids, smart home management systems, etc.). |
| [56] Canada Journal Research Article | Qualitative, participatory needs assessment with strong cultural sensitivity and community engagement. | Includes people with dementia, carers, healthcare professionals, and community leaders. | Focus is on identifying needs and barriers to technology use in Indigenous dementia care contexts. |
| [9] The Netherlands Journal Systematic Review | Systematic review with interdisciplinary reach (healthcare, HCI, design), assessing phases of involvement and engagement strategies. | Centred on direct participation of people with dementia, including as co-designers in some studies. | Broad range of supportive technologies. |
| [61] 2020 USA Journal Literature review | Narrative mini-review. | Stakeholders’ needs and barriers are acknowledged, but not through participatory methods. | Intelligent Assistive Technologies (IAT), including wearable, handheld devices, mobility aids, voice-activated assistants, robotics, and sensors. |
| [58] Croatia Journal Research Paper | Mixed methods; literature review and qualitative data from focus groups. | Older adults were consulted through focus groups. | Digital platforms and assistive technologies for health and social care. Telehealth, remote monitoring, and assistive devices. |
| [49] Germany Journal Research Article | Qualitative, using focus groups and content analysis to gather and analyse feedback from key stakeholders. An emphasis on iterative feedback and ethical considerations. | Strong involvement of people with dementia, therapists, caregivers, and researchers, ensuring that the technology is developed in alignment with their needs and ethical concerns. | Mobile service robots are applied within a psychosocial group therapy setting, designed to assist therapists and participants with dementia. |
| [44] Canada Journal Research Article | Mixed methods, with qualitative analyses and user experience questionnaires to assess the usability of the technology and guide further modifications. | Strong stakeholder involvement, with users actively participating in both laboratory and real-world settings to inform the design process and address usability issues. | COOK (Cognitive Orthosis for coOKing), an assistive technology designed to support older adults, especially those with cognitive impairments, in cooking tasks. |
| [53] Denmark Conference Proceedings (Full Paper) | Qualitative; participatory workshops using participatory design and design thinking frameworks; iterative. | High involvement of end-users and multi-disciplinary teams throughout the design process. | Focus on natural language processing technology applied in dementia care contexts. |
| [38] Australia Journal Research Article | Mixed methods, including usability testing, interviews, observations, and standardised usability scoring. It reflects core HCD principles such as iteration, user feedback, adaptation to cognitive needs, and the consideration of overlapping but distinct user journeys. | People with dementia and carers were both involved in testing and provided feedback that directly shaped design changes. | Dementia-focused informational website (Forward with Dementia). |
Appendix C. Search Strategy
- (1)
- JSTOR sources
- (2)
- SCOPUS sources
- (3)
- WEB OF SCIENCE sources
- (4)
- ProQuest sources
- #1- TS = (“human centred design” OR “human centred design” OR “user-centred design” OR “user-centred design” OR “design thinking”)
- #2- TS = (“dementia” OR “Alzheimer’s” OR “Alzheimer disease”)
- #3- TS = (“assistive technology” OR “technology” OR “adaptive technology” OR “Assistive Devices” OR “technology, assistive”)
References
- World Health Organization. Dementia. 2023. Available online: https://www.who.int/ (accessed on 15 July 2025).
- Ahmed, M.; Marin, M.; Gangas, P.; Bentlage, E.; Louro, C.; Brach, M. Improving the acceptability and implementation of information and communication technology-based health care platforms for older people with dementia or Parkinson disease: Qualitative study results of key stakeholders. JMIR Form. Res. 2024, 8, e58501. [Google Scholar] [CrossRef] [PubMed]
- Flicker, L. Dementia reconsidered: The person comes first. BMJ (Clin. Res. Ed.) 1999, 318, 880A. [Google Scholar] [CrossRef] [PubMed]
- Nolan, L. Caring for people with dementia in the acute setting: A study of nurses’ views. Br. J. Nurs. (Mark Allen Publ.) 2007, 16, 419–422. [Google Scholar] [CrossRef]
- IDEO Human-Centered Design. 2023. Available online: https://www.ideo.com/ (accessed on 1 June 2025).
- Span, M.; Hettinga, M.; Vernooij-Dassen, M.; Eefsting, J.; Smits, C. Involving people with dementia in the development of supportive IT applications: A systematic review. Ageing Res. Rev. 2013, 12, 535–551. [Google Scholar] [CrossRef]
- ISO 9241-210:2019; Ergonomics of Human-System Interaction, Part 210: Human-Centred Design for Interactive Systems, 2nd ed. International Organization for Standardization: Vernier, Switzerland, 2019. Available online: https://www.iso.org/standard/77520.html (accessed on 1 June 2025).
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Suijkerbuijk, S.; Nap, H.H.; Cornelisse, L.; Ijsselsteijn, W.A.; De Kort, Y.A.W.; Minkman, M.M.N.; Baglio, F. Active involvement of people with Dementia: A systematic review of studies developing supportive technologies. J. Alzheimer’s Dis. 2019, 69, 1041–1065. [Google Scholar] [CrossRef]
- Boyle, L.D.; Husebo, B.S.; Vislapuu, M. Promotors and barriers to the implementation and adoption of assistive technology and telecare for people with dementia and their caregivers: A systematic review of the literature. BMC Health Serv. Res. 2022, 22, 1573. [Google Scholar] [CrossRef]
- Sriram, V.; Jenkinson, C.; Peters, M. Informal carers’ experience of assistive technology use in dementia care at home: A systematic review. BMC Geriatr. 2019, 19, 160. [Google Scholar] [CrossRef]
- Green, M.; Dao, D.; Moyle, W. Design Attributes of Socially Assistive Robots for People with Dementia: A Systematic Review. Int. J. Soc. Robot. 2024, 16, 415–427. [Google Scholar] [CrossRef]
- Shaik, M.A.; Anik, F.I.; Hasan, M.; Chakravarty, S.; Ramos, M.D.; Rahman, M.A.; Ahamed, S.I.; Sakib, N. Advancing Remote Monitoring for Patients With Alzheimer Disease and Related Dementias: Systematic Review. JMIR Aging 2025, 8, e69175. [Google Scholar] [CrossRef]
- Koo, B.M.; Vizer, L.M. Examining Mobile Technologies to Support Older Adults With Dementia Through the Lens of Personhood and Human Needs: Scoping Review. JMIR mHealth uHealth 2019, 7, e15122. [Google Scholar] [CrossRef]
- Neal, I.; du Toit, S.H.J.; Lovarini, M. The use of technology to promote meaningful engagement for adults with dementia in residential aged care: A scoping review. Int. Psychogeriatr. 2020, 32, 913–935. [Google Scholar] [CrossRef]
- Bradley, L.; Shanker, S.; Murphy, J.; Fenge, L.-A.; Heward, M. Effectiveness of digital technologies to engage and support the wellbeing of people with dementia and family carers at home and in care homes: A scoping review. Dementia 2023, 22, 1292–1313. [Google Scholar] [CrossRef]
- MacRitchie, J.; Floridou, G.A.; Christensen, J.; Timmers, R.; de Witte, L. The use of technology for arts-based activities in older adults living with mild cognitive impairment or dementia: A scoping review. Dementia 2023, 22, 252–280. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Pollock, D.; Peters, M.D.; Khalil, H.; McInerney, P.; Alexander, L.; Tricco, A.C.; Evans, C.; de Moraes, É.B.; Godfrey, C.M.; Pieper, D.; et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid. Synth. 2023, 21, 520–532. [Google Scholar] [CrossRef]
- Veritas Health Innovation. Covidence Systematic Review Software. Available online: https://www.covidence.org/ (accessed on 7 May 2025).
- Mettouris, C.; Yeratziotis, A.; Fixl, L.; Parker, S.; Starosta-Sztuczka, J.; Clarke, V.; Rosenauer, G.; Daxberger, W.; Koumou, S.; Panayides, M.; et al. An advanced remote reminder system for people with early dementia. SN Comput. Sci. 2023, 4, 334. [Google Scholar] [CrossRef]
- Cruz-Sandoval, D.; Ten Tori, M.; Favela, J. A framework to design engaging interactions in socially assistive robots to mitigate dementia-related symptoms. ACM Trans. Hum.-Robot. Interact. 2025, 14, 17. [Google Scholar] [CrossRef]
- Peng, F.; Altieri, B.; Hutchinson, T.; Harris, A.J.; McLean, D. Design for Social Innovation: A Systemic Design Approach in Creative Higher Education toward Sustainability. Sustainability 2022, 14, 8075. [Google Scholar] [CrossRef]
- Peng, F. Design thinking: From empathy to evaluation. In Foundations of Robotics: A Multidisciplinary Approach with Python and ROS; Springer Nature: Singapore, 2022; pp. 63–81. [Google Scholar]
- Fox, S.; E Brown, L.J.; Antrobus, S.; Brough, D.; Drake, R.J.; Jury, F.; Leroi, I.; Parry-Jones, A.R.; Machin, M. Co-design of a Smartphone App for People Living With Dementia by Applying Agile, Iterative Co-design Principles: Development and Usability Study. JMIR mHealth uHealth 2022, 10, e24483. [Google Scholar] [CrossRef] [PubMed]
- Duarte, R.P.; Cunha, C.A.S.; Alves, V.N.N. Mobile application for real-time food plan management for Alzheimer patients through design-based research. Future Internet 2023, 15, 168. [Google Scholar] [CrossRef]
- De-Rosende-Celeiro, I.; Francisco-Gilmartin, V.; Bautista-Blasco, S.; Avila-Alvarez, A. Co-creation and evaluation of an app to support reminiscence therapy interventions for older people with dementia. Digit. Health 2024, 10, 20552076241261849. [Google Scholar] [CrossRef] [PubMed]
- DuBose, L.; Fan, Q.; Fisher, L.; Hoang, M.-N.; Salha, D.; Lee, S.; Falohun, T. Development and evaluation of a web-based platform for personalized educational and professional assistance for dementia caregivers: Proposal for a mixed methods study. JMIR Res. Protoc. 2024, 13, e64127. [Google Scholar] [CrossRef]
- Bourazeri, A.; Stumpf, S. Co-designing smart home technology with people with dementia or parkinson’s disease. In Proceedings of the 10th Nordic Conference on Human-Computer Interaction, Oslo, Norway, 29 September–3 October 2018. [Google Scholar] [CrossRef]
- Knoefel, F.; Trudel, C.; Jaana, M.; Wilson, C.; Wallace, R.B.; Ault, L.; Waldie, P.; Attef, M.; Thomas, N.; Goubran, R.; et al. Implementation of smart supportive dementia technology in a hospital transitional care setting using human-centred design. Healthc. Manag. Forum 2022, 35, 318–323. [Google Scholar] [CrossRef]
- Goerss, D.; Koehler, S.; Rong, E.; Temp, A.G.; Kilimann, I.; Bieber, G.; Teipel, S. Smartwatch-based interventions for people with dementia: User-centered design approach. JMIR Aging 2024, 7, e50107. [Google Scholar] [CrossRef]
- Elnimr, H. Assessing Alzheimer’s therapeutic environment digitally through a people with Alzheimer’s disease perspective: A computation-based approach framework. Buildings 2023, 13, 2232. [Google Scholar] [CrossRef]
- Mille, L.M.; Kaye, J.; Lindauer, A.; Mau-Yeung, W.-T.; Rodrigues, N.K.; Czaja, S.J. Remote passive sensing of older adults’ activities and function: User-centered design considerations for behavioral interventions conducted in the home setting. J. Med. Internet Res. 2024, 26, e54709. [Google Scholar] [CrossRef]
- Berrett, J.; de Kruiff, A.; Pedell, S.; Reilly, A. Augmented assistive technology: The importance of tailoring technology solutions for people living with dementia at home. Int. J. Hum.-Comput. Stud. 2022, 165, 102852. [Google Scholar] [CrossRef]
- Espinoza, F.; Cook, D.; Butler, C.R.; Calvo, R.A. Supporting dementia caregivers in Peru through chatbots: Generative AI vs. In structured conversations. In Proceedings of the 36th British Human-Computer Interaction Conference, York, UK, 28–29 August 2023. [Google Scholar]
- Espinoza, F.; Cook, D.; Da Re, M.; Fuentes, M.S.C.; Butler, C.R.; Calvo, R.A. Designing AI-powered chatbots for dementia care in Peru: Stakeholder engagement and field observations. Interact. Comput. 2025, iwae057. [Google Scholar] [CrossRef]
- Zheng, J.; Gresham, M.; Phillipson, L.; Hall, D.; Jeon, Y.-H.; Brodaty, H.; Low, L.-F. Exploring the usability, user experience and usefulness of a supportive website for people with dementia and carers. Disabil. Rehabil.-Assist. Technol. 2024, 19, 1369–1381. [Google Scholar] [CrossRef]
- Dupont, C.; Monnet, F.; Pivodic, L.; De Vleminck, A.; Van Audenhove, C.; Van den Block, L.; Smets, T. Evaluating an advance care planning website for people with dementia and their caregivers: Protocol for a mixed method study. Digit. Health 2023, 9, 117021. [Google Scholar] [CrossRef] [PubMed]
- Gencturk, M.; Laleci Erturkmen, G.B.; Gappa, H.; SchmidtBarzynski, W.; Steinhoff, A.; Abizanda, P.; Robbins, T.; Pournik, O.; Ahmad, B.; Randeva, H.; et al. The design of a mobile platform providing personalized assistance to older multimorbid patients with mild dementia or mild cognitive impairment (MCI). In Proceedings of the 10th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-Exclusion, Lisbon, Portugal, 31 August–2 September 2022; pp. 37–43. [Google Scholar] [CrossRef]
- Gappa, H.; Mohamad, Y.; Breidenbach, M.; Abizanda, P.; Schmidt-Barzynski, W.; Steinhoff, A.; Robbins, T.; Randeva, H.; Kyrou, I.; Cramariuc, O.; et al. Making Person-Centred Health Care Beneficial for People with Mild Cognitive Impairment (MCI) or Mild Dementia—Results of Interviews with Patients and Their Informal Caregivers. In Computers Helping People with Special Needs: Proceedings of the 18th International Conference, ICCHP-AAATE 2022, Lecco, Italy, 11–15 July 2022; Springer Verlag: Berlin/Heidelberg, Germany, 2022; pp. 468–474. [Google Scholar] [CrossRef]
- Rathnayake, S.; Moyle, W.; Jones, C.; Calleja, P. Co-design of an mHealth application for family caregivers of people with dementia to address functional disability care needs. Inform. Health Soc. Care 2021, 46, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Kim, H.N. Usability of Alzheimer’s mHealth Applications. J. Best Pract. Health Prof. Divers. 2018, 11, 31–42. [Google Scholar]
- Yaddaden, A.; Bottari, C.; Lussier, M.; Kenfack-Ngankam, H.; Couture, M.; Giroux, S.; Bier, N. The COOK assistive technology for cognition for older adults with cognitive deficits: A usability study. Disabil. Rehabil. Assist. Technol. 2025, 20, 1838–1852. [Google Scholar] [CrossRef]
- Roberts, E.; Fan, G.; Chen, X. In-Lab Development of a Mobile Interface for Cognitive Assistive Technology to Support Instrumental Activities of Daily Living in Dementia Homecare. J. Aging Environ. 2023, 37, 127–141. [Google Scholar] [CrossRef]
- Spalla, G.; Gouin-Vallerand, C.; Yaddaden, A.; Gagnon-Roy, M.; Bottari, C.; Bier, N. Defining Personas for Assistive Technology Development: Improving the Cognitive Support of Older Adults on the Dementia Continuum. Interact. Comput. 2025, 37, 73–87. [Google Scholar] [CrossRef]
- Monnet, F.; Dupont, C.; Smets, T.; De Vleminck, A.; Van Audenhove, C.; van den Block, L.; Pivodic, L. Advance care planning website for people with dementia and their family caregivers: Protocol for a development and usability study. JMIR Res. Protoc. 2023, 12, e46935. [Google Scholar] [CrossRef]
- Monnet, F.; Dupont, C.; Pivodic, L.; Smets, T.; De Vleminck, A.; Van Audenhove, C.; van den Block, L. A user-centred website to support advance care planning for people with dementia and their family caregivers: Development and usability study. Digit. Health 2025, 11, 20552076241304018. [Google Scholar] [CrossRef]
- Wasic, C.; Erzgraeber, R.; Unger-Buettner, M.; Donath, C.; Boehme, H.-J.; Graessel, E. What helps, what hinders? Focus group findings on barriers and facilitators for mobile service robot use in a psychosocial group therapy for people with dementia. Front. Robot. AI 2024, 11, 1258847. [Google Scholar] [CrossRef]
- Cortellessa, G.; Fracasso, F.; Umbrico, A.; Cesta, A.; Dionisio, P.; Ciucci, L.; Di Guardo, F.; Tamburini, E.; Pérez, M.Á.; Herrero, J.; et al. Co-design of a TV-based home support for early stage of dementia. J. Ambient Intell. Humaniz. Comput. 2021, 12, 4541–4558. [Google Scholar] [CrossRef]
- Møller, A.K. The Design of Electronic Tagging and Tracking Solutions to Improve the Safety and Person-Centered Care for People with Dementia. In Human Aspects of IT for the Aged Population. Healthy and Active Aging; Springer International Publishing: Cham, Switzerland, 2020; pp. 138–148. [Google Scholar] [CrossRef]
- Leorin, C.; Stella, E.; Nugent, C.; Cleland, I.; Paggetti, C. The Value of Including People with Dementia in the Co-Design of Personalized eHealth Technologies. Dement. Geriatr. Cogn. Disord. 2019, 47, 164–175. [Google Scholar] [CrossRef]
- Yu, T.-H.; Chang, W.-L. Incorporating design thinking approach to the mutual learning process: A case study of participatory design with senior daycare workers. In Proceedings of the Human-Computer Interaction Thematic Area Conference (HCI), Part of the 25th International Conference on Human-Computer Interaction (HCII), Copenhagen, Denmark, 23–28 July 2023. [Google Scholar]
- Rochon, E.A.; Sy, M.; Phillips, M.; Anderson, E.; Plys, E.; Ritchie, C.; Vranceanu, A.-M. Bio-Experiential Technology to Support Persons With Dementia and Care Partners at Home (TEND): Protocol for an Intervention Development Study. JMIR Res. Protoc. 2023, 12, e52799. [Google Scholar] [CrossRef]
- Shastri, K.; Boger, J.; Marashi, S.; Astell, A.; Dove, E.; Nedlund, A.-C.; Mäki-Petäjä-Leinonen, A.; Nygård, L. Working towards inclusion: Creating technology for and with people living with mild cognitive impairment or dementia who are employed. Dementia 2022, 21, 556–578. [Google Scholar] [CrossRef] [PubMed]
- Starblanket, D.; O’Connell, M.E.; Gould, B.; Jardine, M.; Ferguson, M.; Bourassa, C. Defining technology user needs of Indigenous older adults requiring dementia care. Gerontechnology 2019, 18, 142–155. [Google Scholar] [CrossRef]
- Loebe, C.; Petersen, N. Between empowerment, patronization, and surveillance. A semi-structured interview study with persons with dementia and family caregivers on the empowering opportunities and perils of intelligent assistive technologies. BMC Med. Ethics 2025, 26, 44. [Google Scholar] [CrossRef] [PubMed]
- Vukšić, V.B.; Stjepić, A.-M.; Vukšić, M. Digital Technologies for Independent Living of Older Adults in Health Care and Social Care: A Study From Croatia. Proceedings of FEB Zagreb International Odyssey Conference on Economics and Business, Istria, Croatia, 10–13 May 2023. [Google Scholar]
- Callaway, L.; Liddle, J. How is assistive technology meeting the needs and goals of people with brain impairment? Building evidence to support practice. Brain Impair. 2023, 24, 133–136. [Google Scholar] [CrossRef]
- Melles, M.; Albayrak, A.; Goossens, R. Innovating health care: Key characteristics of human-centered design. Int. J. Qual. Health Care 2020, 33 (Suppl. S1), 37–44. [Google Scholar] [CrossRef]
- Vollmer Dahlke, D.; Ory, M.G. Emerging Issues of Intelligent Assistive Technology Use Among People With Dementia and Their Caregivers: A U.S. Perspective. Front. Public Health 2020, 8, 191. [Google Scholar] [CrossRef]
- Buchanan, R. Human Dignity and Human Rights: Thoughts on the Principles of Human-Centered Design. Des. Issues 2001, 17, 35–39. Available online: http://www.jstor.org/stable/1511799 (accessed on 1 May 2025). [CrossRef]
- Ward, M.E.; De Brún, A.; Beirne, D.; Conway, C.; Cunningham, U.; English, A.; Fitzsimons, J.; Furlong, E.; Kane, Y.; Kelly, A.; et al. Using Co-Design to Develop a Collective Leadership Intervention for Healthcare Teams to Improve Safety Culture. Int. J. Environ. Res. Public Health 2018, 15, 1182. [Google Scholar] [CrossRef]
- Sanders, E.; Stappers, P. Co-creation and the new landscapes of design. CoDesign 2008, 4, 5–18. [Google Scholar] [CrossRef]
- Sanders, E.; Stappers, P. From designing to co-designing to collective dreaming: Three slices in time. Interactions 2014, 21, 24–33. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Liu, K.Y.; Costafreda, S.G.; Selbæk, G.; Alladi, S.; Ames, D.; Banerjee, S.; Burns, A.; Brayne, C.; et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet 2024, 404, 572–628. [Google Scholar] [CrossRef]
- Alzheimer’s Association. What is Dementia? 2023. Available online: https://www.alz.org/ (accessed on 15 June 2025).
- Zou, Y.; Peng, F. Simultaneously Monitoring System Design for Infants’ Temperature: A Human-Centred Design (HCD) in Fashion Practice. In International Conference on Human-Computer Interaction; Springer International Publishing: Cham, Switzerland, 2022; pp. 467–481. [Google Scholar]
- Zabar, M.; Peng, F.; Davis, A.; Kueh, C.; Gwilt, I. Co-design for sustainable youth mental health in Australia. In Design for Dementia, Mental Health and Wellbeing; Routledge: London, UK, 2024; pp. 37–49. [Google Scholar]
- Brown, T. Change by Design: How to Use Design Thinking to Transform Organizations and Create a Better World; Harper Collins Publishers: New York, NY, USA, 2009. [Google Scholar]
- Kruse, C.S.; Fohn, J.; Umunnakwe, G.; Patel, K.; Patel, S. Evaluating the Facilitators, Barriers, and Medical Outcomes Commensurate with the Use of Assistive Technology to Support People with Dementia: A Systematic Review Literature. Healthcare 2020, 8, 278. [Google Scholar] [CrossRef]
- Jolliff, A.; Hill, J.R.; Zuraw, M.; Elliott, C.; Werner, N.E. Representing the needs of rural caregivers of people living with Alzheimer’s disease and related dementias through user personas. Innov. Aging 2024, 8, igae096. [Google Scholar] [CrossRef]
| Number of Studies (N = 49) | |
|---|---|
| Publication date | |
| After 2020 | 39 |
| 2017–2020 | 10 |
| Before 2017 | 0 |
| Region | |
| Europe | 28 |
| North America | 15 |
| Oceania | 5 |
| South America | 1 |
| Study design | |
| Qualitative | 14 |
| Mixed methods | 18 |
| Quantitative | 1 |
| Other (e.g., review, case report, framework proposal) | 16 |
| Assistive technology type | |
| mHealth/eHealth | 18 |
| Smart Home Systems | 5 |
| Internet of Things (IOT) | 3 |
| Robotics | 3 |
| Chatbot/Natural Language Processing | 3 |
| Mixed | 16 |
| TV-based | 1 |
| Framework | Phases/Cycles | References |
|---|---|---|
| PERCEPT framework | Explore, Design, Evaluate | [30] |
| Human-Centred Design /User-Centred Design approach | Discovery, Development, Evaluation | [35] |
| App identification and categorisation, sampling, expert heuristic evaluation (Nielsen’s Usability Heuristics), guideline development (no iterative or user-involved cycles) | [43] | |
| Exploration; Ideation; Generation; Evaluation (iterative cycles) | [44] | |
| Studying users; Designing for the problem; Testing IADL system components; Evaluating the IADL/CAT system | [45] | |
| Structured observation, self-report questionnaires, qualitative content analysis | [32] | |
| Requirement gathering, prototyping, feedback, iteration, and final design approval | [40] | |
| Persona development/Not applicable | [22,46] | |
| Content specification (user needs assessment, evidence synthesis, translation into preliminary content); Creative design (storyboard, prototype development, iterative usability testing with continuous stakeholder engagement) | [47,48] | |
| Focus group discussion, app improvement suggestions, technical implementation, and deployment | [49] | |
| Phase 1: identify requirements and design prototype; Phase 2: evaluation by occupational therapists | [28,39] | |
| Stakeholder engagement; Intervention design and development; Evaluation (interviews, satisfaction survey) | [36,37] | |
| ISO 9241–210:2019 Discover, Design (Prototyping and Evaluation) | [27] | |
| ISO 9241–210:2019 Understand, Define, Design, Evaluate (ongoing iteration) | [31,41] | |
| Co-Design | User Requirements, Prototype 1, Internal Test, Prototype 2, Feasibility Study, Prototype 3, Clinical Trial, System Improvement. | [50] |
| Research, Ideation, Prototyping, Evaluation | [51] | |
| Needs assessment, Development | [42] | |
| Empathise, Define, Ideate, Prototype, Test | [52] | |
| Planning, Design, Development, Testing (combined with Agile methodology) | [26] | |
| Design Thinking with Participatory Design | Phase I: Platform development and pilot test; Phase II: iterative platform development and evaluation | [29] |
| Empathise, Define, Ideate, Prototype, Test (Stanford d.school model) | [33,53] | |
| Understanding user needs, goals, strengths; Prototype development and refinement; Observing user interactions (aligned with NIH Stage Model) | [54] | |
| Semi-structured interviews, participatory sessions, and data analysis | [55] | |
| Community-Based Participatory Research (CBPR) | Planning, data collection (focus groups/interviews), analysis, theme development, reflection | [56] |
| Qualitative study | Not applicable (using vignettes or interviews) | [2,57,58] |
| Usability and ergonomics focused | Not applicable | [34,38] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, F.; Little, K.; Liu, L. Human-Centred Design (HCD) in Enhancing Dementia Care Through Assistive Technologies: A Scoping Review. Digital 2025, 5, 51. https://doi.org/10.3390/digital5040051
Peng F, Little K, Liu L. Human-Centred Design (HCD) in Enhancing Dementia Care Through Assistive Technologies: A Scoping Review. Digital. 2025; 5(4):51. https://doi.org/10.3390/digital5040051
Chicago/Turabian StylePeng, Fanke, Kate Little, and Lin Liu. 2025. "Human-Centred Design (HCD) in Enhancing Dementia Care Through Assistive Technologies: A Scoping Review" Digital 5, no. 4: 51. https://doi.org/10.3390/digital5040051
APA StylePeng, F., Little, K., & Liu, L. (2025). Human-Centred Design (HCD) in Enhancing Dementia Care Through Assistive Technologies: A Scoping Review. Digital, 5(4), 51. https://doi.org/10.3390/digital5040051






