1. Introduction
Currently, in Germany, vaccination records are traditionally recorded in a physical yellow booklet that is manually filled out by doctors. This booklet is often transferred between different hospitals and practices, as individuals receive vaccinations from various healthcare providers throughout their lives. During the COVID-19 pandemic, the drawbacks of this analog system became visible: In many countries, including Germany, exit restrictions and various restrictions on social life were imposed, which were gradually eased. Initially, however, these relaxations only applied to those who had been vaccinated.
This created opportunities for fraud, with unvaccinated people faking the analog vaccination booklet and therefore potentially putting themselves and others into danger [
1] and leading to false statistics regarding breakthrough infections [
2]. With the release of COVID-19 vaccination certificate solutions [
3,
4] in Germany, manageable with the smartphone app CovPass, medical doctors and vaccination centers additionally handed out these certificates in the form of a QR code printed on paper, which would increase the validity of the vaccination status. However, alternatively, pharmacists were also enabled and made responsible for issuing these QR codes, using the booklet to check vaccination status and identity. As a result, fakes were still possible, and the entire process led to increased effort for pharmacists and, thus, to additional costs. Even fake pharmacies were discovered, handing out valid fake certificates, and unfortunately, due to the lack of a mutual application all over Europe, this issue was not directly solved for a wider range, but solely on the German app [
5]. A European digital vaccination record managed only by the vaccinating doctors and centers would have remedied this, saved resources, and led to even greater validity. In addition to the correctness and the locally independent access option via the internet, the possibility of a reminder function for the necessity of re-vaccinations including trustworthy information could be a beneficial feature. Besides the technical benefits, this might help against vaccine hesitancy, as it would target towards optimized communication and foster the awareness of campaigns [
6], potentially improving vaccination rates.
Medicine develops gradually, and established knowledge can always become outdated as a result. One example of this is the yellow fever vaccination. In 2013, the WHO determined that a single dose of the yellow fever vaccine provides lifelong protection for most individuals. In 2015, the Permanent Vaccination Commission (STIKO) aligned with the WHO’s recommendation, suggesting booster shots only for specific groups like pregnant individuals or those with immunodeficiency, such as HIV. However, a 2020/2021 systematic review with meta-analysis revealed that lifelong immunity cannot be assured with just one vaccine dose, and the rate of waning immunity depends on age and initial immunization status [
7]. If a vaccination app forwarded such information to the patient, they would potentially make an appointment with the doctor for a booster, instead of relying on outdated knowledge.
In 2022, it became possible to store vaccination status digitally in Germany. This was realized with the e-vaccination certificate (“E-Impfpass”), which is part of the electronic patient file [
8], currently denoting only a national solution. However, the last years of the pandemic displayed the need for connecting local solutions in a border-crossing way [
9].
Generally, making patient data accessible across devices and systems has many benefits, as has been thoroughly researched in science [
10,
11,
12,
13,
14]. However, the sharing of medical data between hospitals, or even departments of a single hospital, in Germany is often challenging and often requires decentralized solutions [
15,
16]. Here, one of the greatest challenges is building systems that can provide data in an interoperable manner. Health Level 7 (HL7) attempts to solve this problem with its Fast Healthcare Interoperability Resources (FHIRs) standard, applied to manifold areas in medical informatics [
17,
18,
19] and even proven to create an application using authorization and authentication [
20]. In the context of vaccination systems, leaders from IBM, the World Economic Forum, and the International Air Transport Association (IATA) have advocated for an interoperable standard [
21]. The WHO relate, in their guidelines related to Digital Documentation of COVID-19, to the FHIR standard [
22]. FHIR builds on the previous standards HL7 v2.x and HL7 v3. As HL7 v3 has been perceived as too complex and too expensive to use in practice by the community, FHIR strives to build a more consistent and accessible standard for interoperable exchange of medical data [
23]. Although the first release of the FHIR standard dates back to 2014, the normative version of FHIR was released on October 30, 2019. Since then, it has only been partly adopted in industry, as many of the existing systems still rely on HL7 v2 or have not introduced digital data exchange standards at all. Although, there is the “E-Impfpass” and Austria’s vaccination registry [
24], to this date, no digital vaccination pass using FHIR has been developed, nor any system showcasing a prototypical implementation has been released. Also, no FHIR profiling exists for such a use case.
Thus, in this study, we investigate the feasibility of using FHIR for implementing a digital vaccination pass. We propose a digital vaccination status management and monitoring system that has the potential to improve the efficiency and effectiveness of the vaccination process for both patients and medical doctors (MDs). For patients, the system provides a secure and convenient way to examine their immunization records, allowing them to easily check their vaccination status. The system also offers personalized recommendations for missing vaccinations based on individual factors such as age, medical history, and current immunization status. For MDs, the system offers a more efficient and secure way to manage vaccination records, reducing the need for manual record-keeping and minimizing the risk of errors. It also enables doctors to easily access a patient’s complete vaccination history, allowing them to make more informed decisions while streamlining the vaccination process through increased efficiency in administration and follow-up. The use of FHIR as the underlying standard in the proposed system enables interoperability with a wide variety of other healthcare systems, facilitating the exchange of vaccination information and supporting the broader goal of digitizing the healthcare system. The proposed system has been prototyped using modern standard technologies, such as React [
25], Quarkus [
26], and Keycloak [
27]. While focusing on the FHIR, aspects of privacy and security, although crucial, especially in the healthcare sector, will not be evaluated deeply, hence posing potential aspects in future work. The same applies to ethical issues of healthcare digitalization and the systems built, of which we are aware. For both, we refer to related work [
3,
4,
6,
28].
1.1. Fast Healthcare Interoperability Resources
Interoperability refers to the ability of systems, processes, and organizations within an enterprise to effectively communicate, exchange data, and collaborate with each other. It encompasses the seamless integration of diverse components, technologies, and standards to enable smooth interactions and shared functionality. Interoperability involves addressing conceptual, technological, and organizational barriers to achieve harmonious operation and compatibility across different levels and domains within the enterprise. It facilitates the efficient flow of information, services, and processes, leading to enhanced coordination, flexibility, and responsiveness in achieving business objectives [
29,
30,
31].
Fast Healthcare Interoperability Resources (FHIRs) is a data exchange standard for the healthcare industry, developed by HL7. It is designed to foster interoperability by supporting the exchange of the EHR (Electronic Health Record) between different systems and organizations and has been employed in various use cases, as revealed by a systematic literature review, emphasizing its pivotal role in the digitization of healthcare and its potential for further research and implementation [
32]. For this, it utilizes modern web standards, including Hypertext Transfer Protocol (HTTP), JavaScript Object Notation (JSON), and Extensible Markup Language (XML), to provide a common language for health data, allowing for seamless communication and data sharing. A key web paradigm used in FHIR is Representational State Transfer (REST), which provides a set of architectural principles for web-based systems. REST allows for the creation of a standardized, modular Application Programming Interface (API) that can be easily accessed by different systems. This enables the creation of scalable, flexible systems that can be easily integrated with other applications.
FHIR is composed of a set of modular components, known as “resources,” that can be combined to create a wide range of clinical and administrative data models. This modular design allows for a high degree of flexibility and customization, making FHIR well-suited for a wide range of use cases.
By using FHIR, medical information systems (MISs) can more easily share and access data, which can help improve the quality and accuracy of the information that is available to healthcare providers. This, in turn, can help improve patient care and make the administrative aspects of running a medical practice or healthcare facility more efficient. Additionally, because FHIR is a standardized format, it can help to ensure that the data being exchanged are structured and consistent, which can make them easier to use and analyze. This is particularly useful for medical documentation and billing, as it helps to ensure that the information being recorded is accurate and complete.
1.2. FHIR Implementation Guides
FHIR Implementation Guides are sets of instructions and rules for implementing the FHIR standard in a specific healthcare context [
33]. These guides are designed to help healthcare organizations to adopt the FHIR standard and to improve the interoperability of their systems.
FHIR Implementation Guides typically include information on the specific data elements and resources that need to be exchanged, as well as any rules that need to be followed. At the core of this are resource profiles that both restrict and extend base resources defined by the core FHIR standard. Constraints placed on resources can, for instance, include the cardinality of their attributes, making some of them required or specifying a precise number of occurrences. Extensions are used to add custom attributes of arbitrary complexity to resources. An Implementation Guide may also include custom and standard terminologies, such as the International Statistical Classification of Diseases and Related Health Problems—Version 10 (ICD-10) [
34], as well as rules for how they are used in resources.
The SUSHI software tool [
35] enables the creation of FHIR Implementation Guides using FHIR Shorthand [
36] text files to define resource profiles. It provides a means of efficiently and accurately constructing FHIR Implementation Guides, enabling the standardized representation of healthcare data and information exchange between systems.
1.3. FHIR RESTful API
The FHIR RESTful API is a web-based interface that allows applications to access and exchange healthcare data using FHIR Resources and the REST interface architecture style [
33]. It supports search and discovery operations, allowing clients to search for specific resources using a query language specified by the FHIR specification. The search parameters include elements such as the resource type, the resource identifier, and search criteria based on the data elements in the resource. For example, a client may use a search operation to find all patient records with a specific diagnosis code or to retrieve a specific lab result by its identifier. The server responds with a collection of resources that match the search criteria, along with relevant metadata such as the total number of matching resources and links for pagination. More elaborate search queries can be formulated using FHIR Path.
1.4. FHIR Path
FHIR Path is a language for querying and manipulating data in the FHIR data model [
37]. It is similar to other query languages, such as XPath [
38] and SQL [
39], but is specifically designed to work with the hierarchical structure of FHIR resources. FHIR Path allows users to extract and manipulate specific pieces of information from these resources in a standardized and interoperable manner. It uses a combination of elements and operators to perform operations on FHIR data. Elements are used to identify specific data items within a FHIR resource, and operators are used to perform operations such as filtering, sorting, and aggregation on the data. For example, a FHIR Path query might use the “patient” element to identify a specific patient record and the “where” operator to filter the records based on specific criteria, such as the patient’s age.
2. Materials and Methods
The development of the vaccination pass showcase application involved a multi-faceted approach, including the creation of a domain model to represent the problem space, the representation of this domain model using FHIR resources, and the selection and implementation of both existing open-source software and new software components to meet the requirements of the application. In the following sections, we detail the specific methods and approaches employed in each of these areas.
2.1. General Non-Functional Requirements
Firstly, ensuring the availability of the digital vaccination pass was paramount. Users needed seamless access to their vaccination records at any time, regardless of location or device. Thus, it was implemented as a web application.
Secondly, usability was a fundamental aspect of the digital vaccination pass. Recognizing the diverse needs of users, the interface was designed to be intuitive and easy to navigate.
Next, interoperability played a crucial role in the development of the digital vaccination pass. To prepare the system for future seamless data exchange within the healthcare industry, the system was designed to be based on the FHIR standard.
Lastly, since our work presents a prototypical implementation, we limited the non-functional requirement security to authentication, authorization, and access restrictions, which limit user access to specific data within the system. This ensures privacy as the data are only accessible to specific authorized users, i.e., the user himself and the assigned doctor.
2.2. Domain Model
To develop a domain model that accurately reflects the real-world requirements of vaccination management, we utilized both the vaccination recommendations for Diphtheria, Tetanus, Polio, and SARS-CoV-2 from the Robert Koch Institute (RKI) [
40] and the product information for the corresponding recommended vaccines as examples to be represented in the model [
41]. To maintain conformance to the FHIR standard, we adapted already existing FHIR base resources to our domain whenever a conceptually matching resource existed. Otherwise, we used the “Basic” FHIR resource and extended it accordingly. Subsequently, a FHIR Implementation Guide was created.
2.3. System Architecture
The stated goals were realized through a systematic process. First, we identified system components at an abstract level. Next, we aligned the requirements for each component with an appropriate existing software solution or developed a custom implementation specifically for the vaccination pass use case. The following system components were identified, and their relationships are displayed in
Figure 1:
FHIR Resource Repository to store, modify, access, and search both user data (i.e., personal immunizations) and domain knowledge (i.e., vaccination recommendations by RKI) as FHIR resources.
Event Processor that automatically generates personalized vaccination recommendations when user data or domain knowledge changes.
Patient User Interface to visualize an individual’s immunization record, present recommendations to them, and display the modeled domain knowledge on vaccines and targeted diseases.
Medical Doctor User Interface to allow a practitioner to view the immunization record for each patient in the system, record new immunizations, generate and adjust recommendations, and view and update domain knowledge on vaccines and targeted diseases.
Identity Provider that allows the patient and MD accounts to be managed and serves as a centralized authority on user roles and permissions for the other components.
The requirements for the system components are described in further detail in the following subsections.
2.3.1. FHIR Resource Repository
The FHIR resource repository serves as a centralized store for all FHIR resources consumed and created in the system. It is the only component where FHIR resources can persist. Components that create resources transmit them to the FHIR resource repository to save them. Components that require existing FHIR resources query it to retrieve them. To fulfill this role, the software component should implement the FHIR RESTful API to allow other software components to query and create FHIR resources. Additionally, all incoming FHIR resources should be validated to ensure the correctness of saved resources including conformance to custom profiles. Supporting the event processor component requires the repository to implement a method for subscribing to changes in the FHIR resources. In addition, integration with the identity provider component requires the FHIR resource repository to implement the authentication of clients that is based on an external system as an authority on user accounts and roles.
2.3.2. Event Processor
Generating and updating immunization recommendations based on a patient’s immunization record and risk profile is handled by the event processor component. Software that fulfills the requirements of this component needs to re-evaluate immunization recommendations of all affected patients if one of the following situations occur:
a patient is created;
an immunization is added to the patient immunization record;
recommendations for which patients should receive vaccines targeting a disease are changed;
a patient plans a vacation for which additional immunities are recommended.
This component must be able to subscribe to the feed of FHIR resource changes offered by the FHIR resource repository. It should use the FHIR RESTful API to retrieve additional information required for the re-evaluation triggered by a FHIR resource change and to store updated immunization recommendations in the repository.
2.3.3. Identity Provider
The identity provider is the central store for the patient and MD user accounts that provides information on user authentication and roles to all other components. To fulfill the requirements of this component, the software should offer a UI that allows both patients and MDs to log in to their accounts. On a successful user authentication in the log-in interface, the identity provider should issue a token that can be used to prove the identity of the user in communication with other components. This way, the log-in interface of the identity provider can be integrated with the patient and MD UIs. These requirements can be fulfilled by implementing the industry standard OpenID Connect (OIDC) [
42], together with the security-related advantages that OIDC comes with.
2.4. User Interface
2.4.1. Patient Facing
The Patient User Interface provides patients with information regarding their current immunization status, as well as their immunization history. By employing an iterative prototyping approach, beginning with the creation of low-fidelity User Interface (UI) mock-ups, it was identified that a mobile UI would be most appropriate for the Patient UI. The creation of high-fidelity mock-ups in Figma [
43] and their discussion with users led to the conclusion that a minimal UI design with color-based micro-interactions would lead to a better user experience (UX), which is confirmed by Strecker et al. [
44]. To further enhance the usability of the Patient UI, qualitative interviews with experts (doctors) and users were conducted according to ISO 9241-210 [
45], to understand the needs and preferences of the users. These interviews helped to identify a minimal set of features that the interface should include, based on the doctors’ knowledge of the current use of paper vaccination cards.
2.4.2. Medical-Doctor-Facing
The Medical Doctor User Interface aids MDs in providing immunization recommendations to patients. It should be coherent with the Patient UI and leverage common design elements and functionalities and therefore was developed using the same principles. The UI should enable MDs to get insights into a patient’s vaccination history and provide an overview of the patient’s current immunization status. Furthermore, it should enable the MD to make informed decisions about the next steps in a patient’s immunization based on the recommendations generated. The MD should be able to configure the patient-facing application via the UI and configure the recommendation engine through custom settings for each disease. All design decisions, represented in high-fidelity UI models designed in Figma, were based on interviews with MDs. To ensure the usability and effectiveness of the MD UI in practice settings, it should be optimized for desktop use. This design choice was made with the specific needs and usage patterns of MDs in mind and represents a departure from the design considerations for the Patient UI.
2.4.3. Implementation
Initially, the MD UI was a standalone application. However, to optimize reuse in this prototypical implementation, the MD UI and the Patient UI were integrated into a single client-facing application, resulting in a reduction in boilerplate code for API calls, among other things. Both are realized as a web application based on the JavaScript UI framework React. The UIs utilize ChakraUI, a component library that provides a wide range of pre-designed UI elements [
46], in combination with custom CSS generated using Sassy Cascading Style Sheets (SCSS).
Both UIs utilize subscriptions to receive create- and update-notifications from the FHIR server. Upon initial loading, the UIs initialize themselves through the utilization of the FHIR REST API. Upon receipt of update-notifications from the FHIR server, the UIs evaluate if the update may impact the data utilized within the view, and if so, fetch the relevant data again.
3. Results
The following section outlines a comprehensive explanation of the developed prototype, including a thorough demonstration of how the requirements previously specified were satisfied through the integration of various open-source and custom-developed software components.
3.1. Domain Model
To evaluate an individual patient’s immunization status, the vaccination pass application requires personal data from patients as well as general domain knowledge about vaccination recommendations, diseases, vaccines, and the vaccination process.
Figure 2 shows the resulting domain model using the Unified Modeling Language (UML).
All patient-specific data are represented by the resources “Patient”, “Immunization”, “Immunization-Recommendation”, and “VacationPlan”. “Patient” represents all general information such as name, birth date, and address. The address is of particular importance as additional immunizations based on location may be recommended. An instance of an “Immunization” models that the patient received a single dose of vaccine. It corresponds to a single row in a physical vaccination booklet. An “ImmunizationRecommendation” is a single vaccination dose that should be administered in the future. The “VacationPlan” allows the patient to add vacation destinations so that applicable travel vaccinations can be recommended. Specifying the departure date ensures that immunization is achieved before departure if multiple shots are required.
All domain knowledge is represented by “TargetDisease”, “PopulationRecommendation”, “Medication”, “VaccinationScheme”, and “VaccinationDose”. A “TargetDisease” contains general information about a disease (i.e., Tetanus) such as its name and ICD-10 code. A “PopulationRecommendation” predicates that all persons of the specified age living in the specified location should have immunization against a certain target disease. An instance of “Medication” provides information on a single vaccine such as the diseases it protects against. Note that one vaccine can protect against multiple diseases, as is the case with Boostrix, which offers protection from Diphtheria, Tetanus, and Pertussis. A “VaccinationScheme” represents a specific vaccination scheme of the referenced vaccine, for example, a fast or booster scheme. It consists of one or more instances of “VaccinationDose”, representing either a single shot (“VaccinationDoseSingle”) or infinitely repeated shots (“VaccinationDoseRepeating”). For example, a scheme of the Boostrix vaccine could consist of five “VaccinationDoseSingle” instances at the ages of 2 months, 4 months, 11 months, 5–6 years, and 9–16 years, as well as one “VaccinationDoseRepeating” instance which is administered every 10 years after the last single dose.
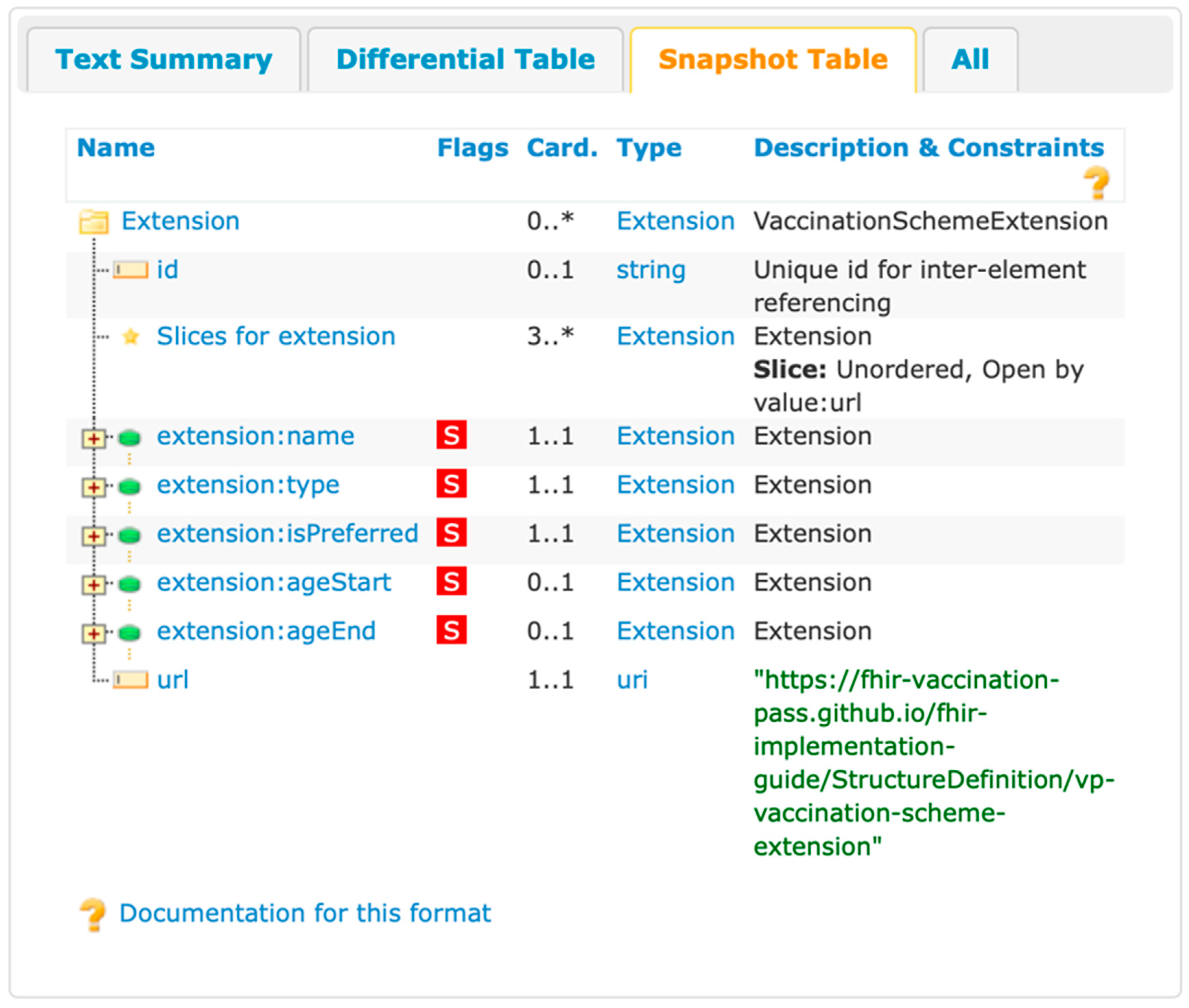
3.2. FHIR Implementation Guide
A FHIR Implementation Guide was created to adapt the FHIR standard to our needs according to the domain model specified in
Figure 2. For this purpose, the domain-specific language FHIR Shorthand (FSH) [
36], as well as its compiler SUSHI [
35], was used.
For each class in the domain model, a FHIR base resource was identified and customized using profiles. This included describing constraints on the use of elements of the base resource as well as defining extensions that contain additional attributes not included in the base resource. For example, in our version of the resource “Immunization”, one vaccine code must be a Pharmazentralnummer (PZN), a German national drug code. In addition, an extension was defined that references a “VaccinationDose”.
Furthermore, search parameters for extensions were defined. This allows filtering resources based on attributes of extensions. For base attributes, the most common search parameters were already defined as part of the base resource definition.
To specify the vaccination scheme type, a code system was created. It determines which types exist and how they are understood.
Using the HL7 Implementation Guide Publisher [
47], a full HTML-based documentation of the Implementation Guide has been created [
48].
Figure 3 depicts an example rendering of the constraints contained in the implementation guide.
3.3. FHIR Resource Repository
The LinuxForHealth FHIR Server (formerly IBM FHIR Server) [
49] was used as the implementation of the FHIR resource repository in our prototype. This FHIR server was chosen because of the following features:
FHIR RESTful interface version R4;
delegation of authentication and authorization to OIDC-compliant identity provider;
event subscriptions for changes to FHIR resources;
FHIR resource validation with custom implementation guide.
The FHIR server’s REST request authentication was configured to authenticate requests made to its API by checking for the presence of a JSON Web Token (JWT) in the request headers and validating the JWT token using the public key published in the OpenID Connect (OIDC) endpoint of the prototype’s Keycloak instance. This way, the server verifies that requests made to it originate from users that have successfully obtained JWT tokens issued by Keycloak.
To support event subscriptions, the server’s notification service was enabled and configured to provide FHIR resource change events as messages on a Web-Socket endpoint.
To provide validation of FHIR resources according to the prototype’s Implementation Guide, a Java JAR file containing an implementation of the FHIRRegistryResourceProvider interface must be created and placed in the FHIR server’s userlib directory. This was achieved by making use of the PackageRegistryResourceProvider class provided by LinuxForHealth and packaging the prototype’s Implementation Guide as a FHIR package. This process was automated as part of the tooling for the creation of the prototype’s Implementation Guide.
3.4. Event Processor
The event processor component was implemented as a stateless Java microservice based on the Quarkus framework. The event processor connects to the FHIR server’s websocket endpoint to receive events for each modification of a FHIR resource. Events are routed internally to the corresponding function that handles them by resource type and operation type, for instance, Patient/create. Resources modeled with the “Basic” resource type due to them representing a concept missing in the FHIR standard present an additional challenge in this process: they are additionally routed by utilizing the FHIR profile URL given in the metadata of the resource. This way, a resource of type “Basic” that represents information about a target disease can be routed to one handling function, while a “Basic” resource that represents information about a vacation plan can be routed to another handling function. Resources that do not conform to the prototype’s implementation guide are simply ignored by the event processor, regardless of the resource type.
Once routing is completed, the called event handling function will create or update immunization recommendations for one or multiple patients. Since the specific function handling the Patient/create event is the most complex (and since all other functions can be trivially replaced by deleting all immunization recommendations and generating them from scratch for every patient), we describe it in the following:
Identify all diseases the patient should have immunization coverage for, considering the patient’s age, places of residence, and vacation plans.
Derive the actual coverage from existing immunizations, and match them to the diseases identified in step 1.
Generate immunization recommendations for diseases without existing immunizations:
Select vaccines that exactly cover all diseases without existing immunizations. Prefer combination vaccines to reduce the number of doses.
Choose vaccination schemes for all selected vaccines. Ensure that immunization is completed before traveling. Prefer schemes with type “standard” and priority “preferred”.
Generate immunization recommendations for diseases with existing immunizations: Recommend the next dose for every administered vaccine in the current scheme. Change the scheme to type “booster” if all doses of type “standard” or “fast” have been administered.
3.5. Identity Provider
Due to the industry standard nature of OIDC, multiple commercial and non-commercial software products exist that implement it. In the vaccination pass prototype, Keycloak was selected as the identity provider component, as it is open-source software, and the project provides Docker [
50] containers of the application that make it easy to self-host for prototyping purposes. Note that this component is rather interchangeable, and a production deployment institution should make use of existing identity infrastructure if it implements OIDC. If desired, it is also possible to utilize existing identity infrastructure to log in to a user account store in Keycloak, if replacing Keycloak is not desirable.
In the prototype, the web application that provides the patient and MD user interfaces, the event processor and the LinuxForHealth FHIR server were added as clients in the Keycloak configuration to allow them to initiate login flows, validate authentication tokens, and retrieve information about user accounts.
3.6. User Interfaces
In the following, we present the two user interfaces: the administrative UI for the MD and the consumer interface for the patient. A demonstration video of the application can be found in
Supplementary Materials Video S1.
3.6.1. Patient-Facing
To realize the proposed design of the patient-facing UI, a web application was developed. The color-coded micro-interactions previously mentioned were included in the design to highlight important elements of the UI and draw attention to alerts, notifications, and other important information. It intends to quickly convey the status or importance of the information being presented to the user. The micro-interactions are divided into four states, which are distinguished by their color coding:
The Default State is displayed when there is no available information about an individual’s immunization status for a particular disease, or when immunization against the disease is optional. This state is represented by the default color used in the UI.
The Immunized State indicates that an individual has completed all necessary immunizations, and no further action is required at this time. This state is represented by the color green to convey the absence of any outstanding issues.
The Due State indicates that an individual’s immunization for a particular disease is imminent or will be necessary for the near future, and that action should be taken to receive it. This state is represented by the color orange to signify its urgency.
The Overdue State refers to a situation in which an individual’s immunity to a particular disease has waned or never existed, and it is recommended that they receive immunization against the disease. This state is depicted using the color red to indicate its importance.
The Patient UI consists of three components that allow patients to view their immunization information from different perspectives, depending on their current needs:
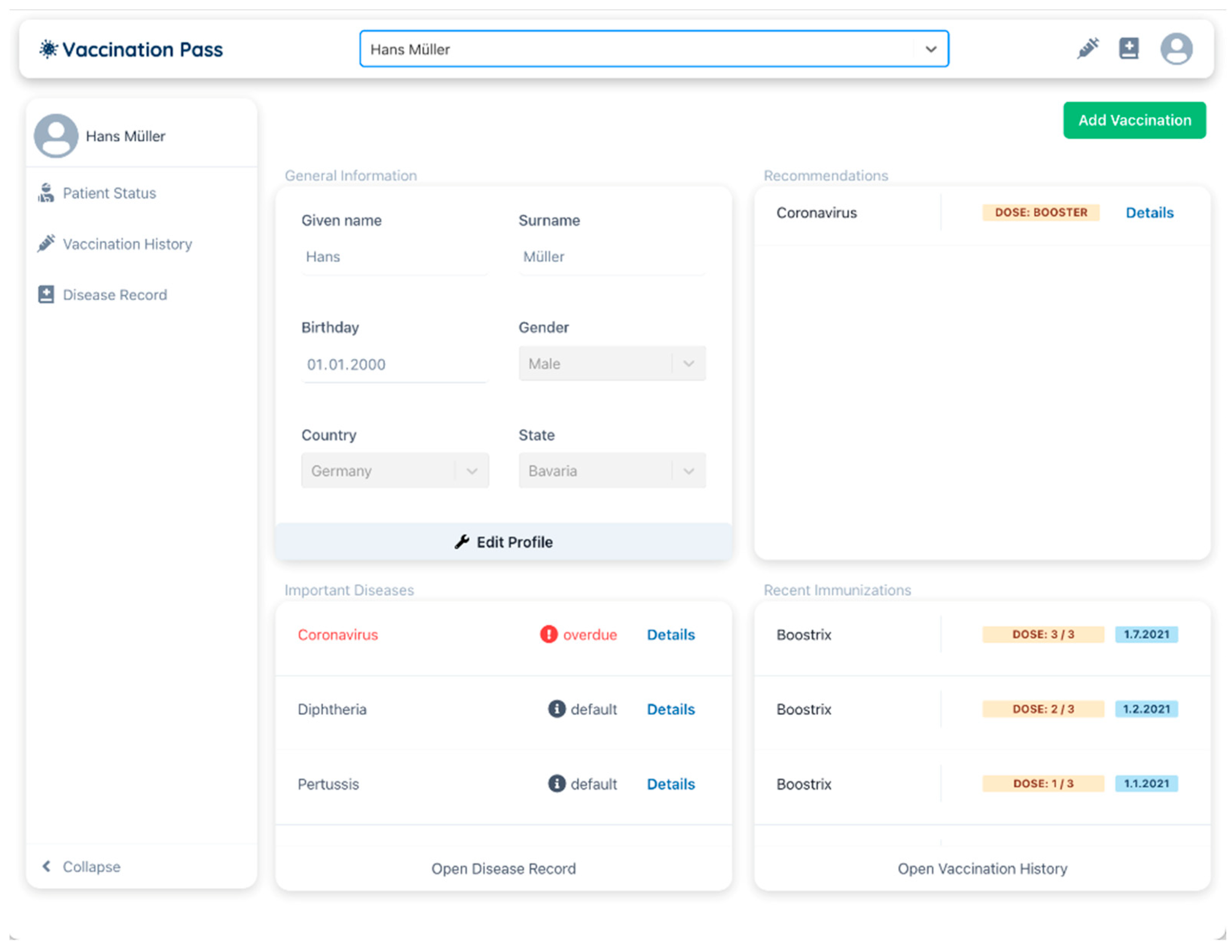
Recommendation Dashboard: The Patient UI includes a recommendation dashboard, which is displayed in
Figure 4, that provides a comprehensive overview of a patient’s vaccination status for various diseases and displays vaccinations that are pending, due, or overdue. This feature aims to facilitate the patient’s ability to access clear, concise information about recommended vaccination measures. The recommendation dashboard calculates an aggregated vaccination status, which is a summary of the patient’s vaccination status across multiple diseases. This is achieved by considering the vaccination information for all relevant diseases. The aggregated vaccination status allows the patient to easily ascertain their overall vaccination status, rather than having to review the vaccination status for each disease individually.
Vaccination History: The vaccination history shown in
Figure 5a is a comprehensive record of all immunizations administered to an individual, organized by the specific disease and the corresponding date of vaccination. This representation allows the patient to retrospectively examine their vaccination status for various diseases and the temporal relationships between them.
Patient Disease Record: The patient disease record, displayed in
Figure 5b, serves as the central repository for information related to immunizations within the system. This record lists all diseases for which immunization is recommended or required and includes a summary of the patient’s vaccination status for each disease. When a specific disease is selected, a detailed overview of relevant information is provided, including general information about the disease (e.g., population recommendations, available vaccines, countries where the disease is prevalent), as well as personalized information regarding the patient’s vaccination status for that disease. The header of the detailed overview includes micro-interactions that provide a summary of the patient’s overall vaccination status and can be expanded to display information about upcoming immunizations and previous vaccination procedures, complete with details about each individual vaccination. The detail overview is depicted in
Figure 5c.
3.6.2. Medical-Doctor-Facing
The MD UI has been implemented based on the high-fidelity mockups created with Figma. This implementation grants the MD the ability to configure the system and manage patients effectively. The interface is structured into various components to facilitate the smooth navigation and utilization of various features and functions. The MD UI consists of the following components:
Base Configuration: Via the Base Configuration interface, the MD can configure various aspects of the system. This interface enables MDs to specify the content that is displayed in the patient UI, as well as the relationships between different entities such as diseases and vaccines. To manage diseases, MDs can use Create, Read, Update, and Delete (CRUD) operations. For example, they can create a target disease with a name, ICD-10 code, and a description. They can also create population recommendations for a particular disease, specifying the affected ages and locations using ISO-3166 location codes [
51]. Similarly, MDs can use CRUD operations to manage vaccines as shown in
Figure 6. They can create a vaccine with a name, PZN code, manufacturer, and target disease. They can also create vaccination schemes for a particular vaccine, specifying the name, age range, and type of the scheme. In addition, they can create doses for a vaccination scheme, specifying the dose number and quantity. MDs can also create booster vaccination schemes that repeat indefinitely.
MD Patient Dashboard: MDs can manage individual patients using the patient dashboard displayed in
Figure 7. This dashboard allows MDs to select patients from a list or search for a particular patient. The dashboard provides a quick overview of a patient’s immunization status using different widgets. These widgets summarize important information about the patient, such as their name and date of birth, as well as all recommendations for immunizations. The widgets also display the most recent vaccinations and a list of the most important diseases that a person should be immunized against.
MD Patient Vaccination History: The MD patient vaccination history provides an overview of a patient’s past immunizations and is based on the patient’s vaccination history in the patient UI. The MD patient vaccination history serves to provide MDs with knowledge on when to administer vaccines to patients based on their previous immunization history. This can help to ensure that patients receive the appropriate vaccines at the appropriate intervals, ultimately improving vaccination rates and public health outcomes.
MD Patient Disease Record: The MD patient disease record is a feature that provides an overview of all diseases that are recorded in the system and whether a patient is immune to them. When a disease is clicked, detailed information about the patient’s vaccination against that disease is displayed, including recommendations and past immunizations. This helps MDs to understand a patient’s immunity status for various diseases and make informed decisions about vaccinations.