Abstract
The exact knowledge of the mandibular canal position is fundamental in oral surgery and implantology. Clinicians have to be extremely cautious when operating in close proximity to this structure in order to avoid damaging the neurovascular bundle. Several anatomical variations of the mandibular canal have been described in the literature, such as bifid or trifid structures. The use of cone-beam computed tomography (CBCT) offers a detailed representation of the inferior alveolar nerve path, albeit with some difficulties of identification when dental implants or metal prosthesis are present. The aim of this study is to retrospectively evaluate the prevalence and location of bifid/trifid mandibular canals (BMC/TMC) by CBCT in Italian patients. The screening phase involved 584 patients, only 238 enrolled (97 men; 141 women), with an average age of 51 ± 17.20. A total of 36 patients (15.25%) showed at least one bifid mandibular canal; only 2 patients (0.84%) showed a trifid mandibular canal. Overall, 12 patients (5.04%) presented this variation bilaterally. There was no association with the sex of the enrolled sample. In conclusion, the presence of BMCs and TMCs may be considered as a risk factor for the onset of neurovascular complications. Being aware of changes in the mandibular canal helps clinicians to prevent inferior alveolar nerve impairments that may occur during oral surgery and implantology.
1. Introduction
Knowing the exact position of the mandibular canal (MC) is crucial to the planning of oral and maxillofacial surgery (e.g., extractions, dental implants) and orthognathic surgery (e.g., sagittal split ramus osteotomy) [1]. Generally, MC is described as singular, while several techniques have been reported in literature as being suitable for bifid mandibular canal (BMC) and trifid mandibular canal (TMC) detection, such as panoramic radiography [2,3,4], computed tomography (CT) [5,6,7], and cone-beam computed tomography (CBCT) [8,9,10]. CT and CBCT investigations showed a higher incidence rate than panoramic radiographies. As explained by Naitoh M. et al. [11], this occurred because of the overlapping of the mandibular ramus region—the opposite site of the mandible—soft palate, and pharynx found in orthopantomography. The MC and its variations are better expressed through CT and CBCT than panoramic radiography due to the acquisition of 3D images with a higher resolution [12]. Rashsuren O. et al. [1] reported that the presence of BMC was 0.08–0.95% when using panoramic radiography and 10.2–65% when evaluating CBCT images. The authors also confirmed the same for the TMC, which was identified more effectively using CBCT (5.8%). Several systematic reviews and meta-analyses have showed different figures for the prevalence of BMCs. Regarding the patient-level prevalence of BMCs, Shan S. et al. [10] recently described a rate of 38%, while Valenzuela F. et al. experienced an individual rate of 57% [13]. Additionally, Hass LF et al. [14] noticed this variation in 16.25% of screened patients. Ngeow WC et al. [15] provided data for BMCs that ranged between 0.05% and 69% of the studied population. Due to this variation, the authors agreed that patient-level and hemi-mandible-level prevalence would be the focus of the present study. The assessment of MC variations has a large impact on daily practice, from anesthesia to tooth extractions, dental implants, and orthognathic surgery [16]. For example, Sîrbu VD et al. [17] reported that the second mandibular molar is the most common tooth involved in accidental MC damage and that overlooking its precise position may not only lead to several complications in dentoalveolar surgical procedures but also in endodontic therapy in the posterior region of the mandible. Because of these clinical considerations, the present study aimed to investigate the prevalence, gender distribution, and age group distribution of BMCs and TMCs in an adult Italian population.
2. Materials and Methods
This cross-sectional study involved patients from the Dentistry Clinic of University G. d’Annunzio of Chieti, Italy. Naitoh M. et al.’s [11] classification was used to examine CBCT scans. A class for TMC was added (Table 1). More specifically, the goal of the present examination was to collect the number of BMCs/TMCs, the unilateral/bilateral presence, and the prevalence in gender and age groups.

Table 1.
Naitoh M. et al.’s [11] classification of bifid mandibular canals using CBCT. The trifid mandibular canal was added.
Radiographic examinations were conducted using a Newtom VGi EVO CBCT scanner (Quantitative Radiology s.r.l., Verona, Italy). All images were recorded at 120 kVP and 3–5 mA using a 9-inch field of view, 1 mm axial slice thickness, and isotropic voxels. The X-ray parameters of kV and mA were automatically determined by the scout views from the NewTom 3G. Depending on the size of the patient and the extent of beam attenuation, an exposure variation of up to 40% was possible. NNT software version 15.1 [Installation package: 15.1.0.0] was used to reconstruct and evaluate all projections. The images were exported and saved as single frame DICOM files. All constructions and measurements were performed directly on the monitor screen (color active matrix display and 24-inch Full HD LED 3200 × 1800 pixel flat panel). Axial, sagittal, transverse, and panoramic images were reconstructed for all hemi-mandibles and evaluated by an experienced dentist in cooperation with the radiologist technician. When disagreement occurred, it was discussed with the maxillofacial surgeon. The age at the time of the scan was recorded for each patient. Pearson’s Chi-Square test was employed to assess the association with categorical variables (location and sex). The p-value was considered significant for a value of p ≤ 0.05.
2.1. Inclusion Criteria
Patients older than 18 y.o., able to provide informed consent, and without noticeable signs of maxillofacial trauma and mandibular lesions in the MC path were enrolled. CBCT scans were examined according to a chronological order of collection.
2.2. Exclusion Criteria
Children; patients unable to provide informed consent; and those with fractures of the mandible, mandibular titanium plates, and mandibular neoplastic or cystic lesions that may have affected the identification of the mandibular canal were excluded.
2.3. Statistical Analysis
Pearson’s Chi-Square test was employed to assess the association with categorical variables (location and sex). The p-value was considered significant for a value of p ≤ 0.05.
3. Results
CBCT images of 584 Italian patients who visited the University Dental Clinic of Chieti between January 2022 and September 2022 were screened. As a result of the first screening, 238 Italian subjects (476 hemi-mandibles) were enrolled, and 346 cases were excluded. The sex distribution was as follows: 97 men (40.76%) and 141 women (59.24%), with a mean overall age of 51 y.o. ± 17.20. Detailed results are shown in Table 2.

Table 2.
Main results. Prevalence of bifid mandibular canals (BMCs) and trifid mandibular canals (TMCs) based on type, gender, and location. M—male; F—female.
Examples of images considered positive for BMC and TMC are shown in Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6 and Figure 7. Regarding the distribution among patients, 36 subjects (15.13%) showed at least one BMC, 12 (5.04%) bilaterally, while 2 subjects (0.84%) showed a TMC. Among patients with cases considered positive for BMC, 21 were women, accounting for 8.82% of the total studied population and 14.89% of female patients overall. On the other hand, 15 BMC patients were men, accounting for 6.30% of the whole sample and 15.4% of men in the study. Considering the hemi-mandibles, BMC appeared in 9.87% of images, while TMC only appeared in 0.42%. The Patient group that was positive for BMCs had a mean age of 34 ± 13.30, while the group that was positive for TMCs presented a mean age of 43 ± 19.8. Pearson’s Chi-Square test was not significant; no association was found between gender and the prevalence of mandibular canals.
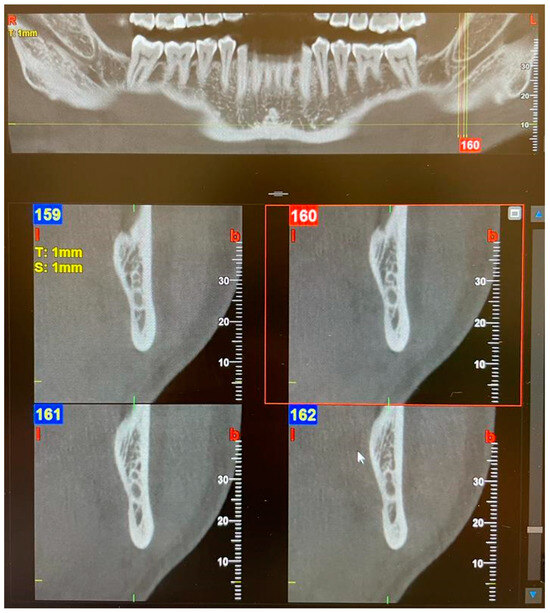
Figure 1.
Panoramic view and transverse section of a bilateral Type 1—Retromolar (bifid mandibular canals) BMC. l, lingual. b, buccal. T, thickness. S, section.
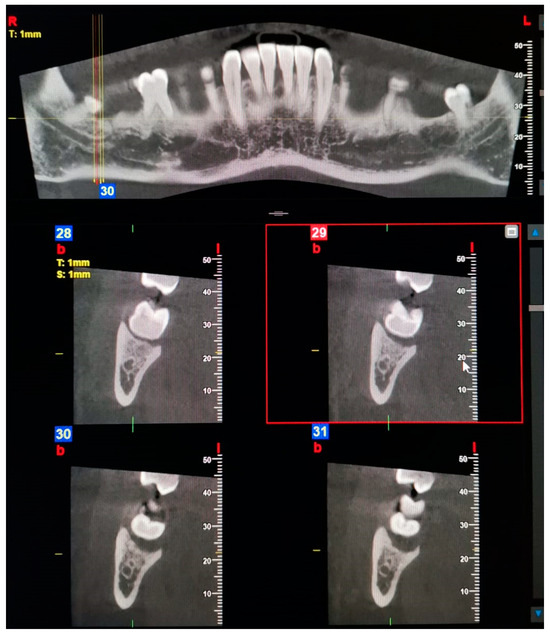
Figure 2.
Panoramic view and transverse section of a right Type 2—Dental BMC. l, lingual. b, buccal. T, thickness. S, section.
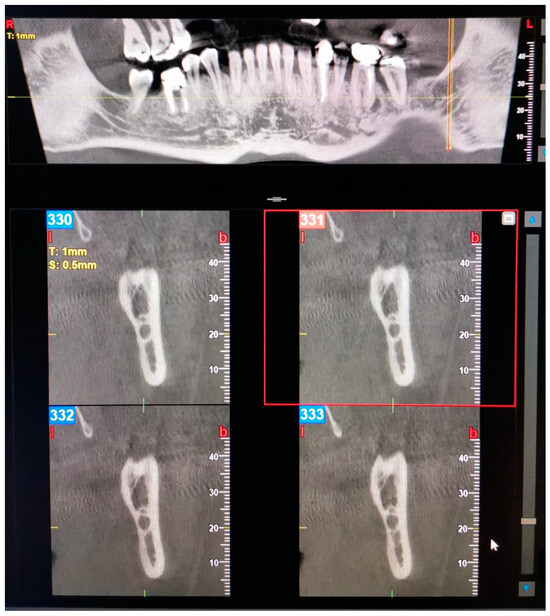
Figure 3.
Panoramic view and transverse section of a left Type 3—Forward BMC with confluence. l, lingual. b, buccal. T, thickness. S, section.
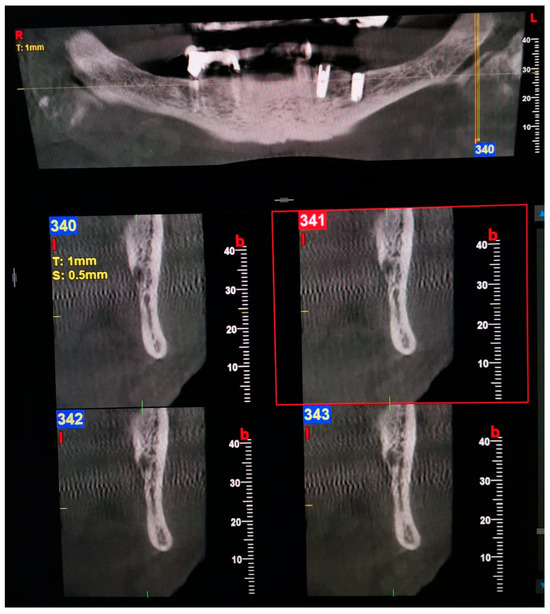
Figure 4.
Panoramic view and transverse section of a left Type 3—Forward BMC without confluence. l, lingual. b, buccal. T, thickness. S, section.
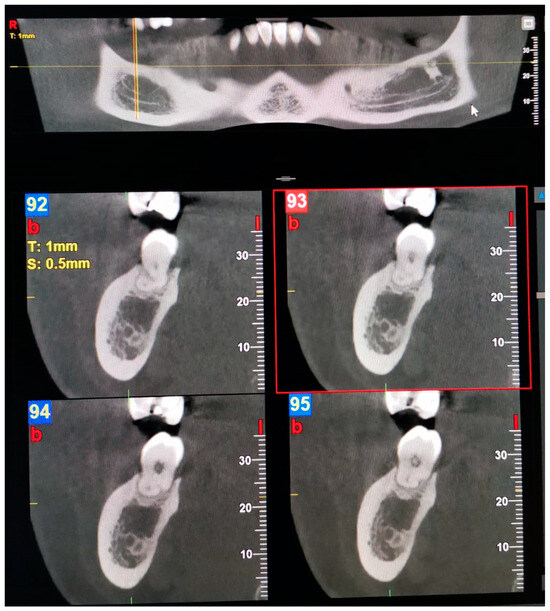
Figure 5.
Panoramic view and transverse section of a right Type 4—Buccolingual BMC. l, lingual. b, buccal. T, thickness. S, section.

Figure 6.
Panoramic view and transverse section of a left TMC. l, lingual. b, buccal. T, thickness. S, section.
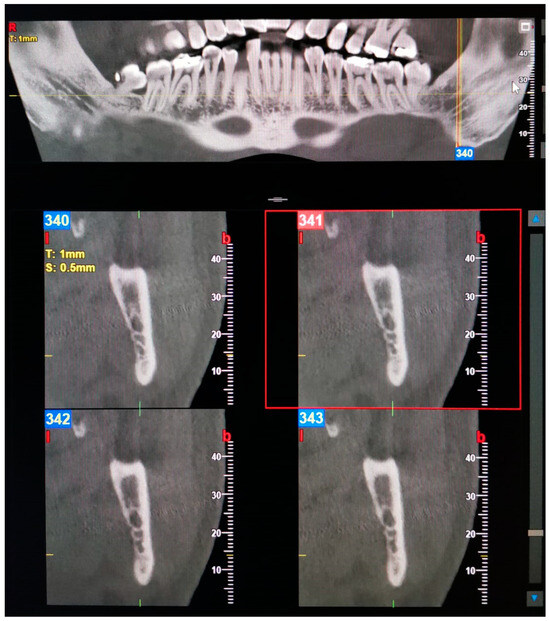
Figure 7.
Panoramic view of TMC (left) and forward BMC without confluence (right). Transverse section of the left TMC. l, lingual. b, buccal. T, thickness. S, section.
4. Discussion
The purpose of this study was to provide support to dental practitioners with regards to the importance of anatomical knowledge and to remind them to be aware of MC variations in order to avoid any iatrogenic damage. The BMC is one of the most common anatomical variations in the mandible, although it can often be overlooked in clinical practice. Knowledge of the morphology and topography of the mandibular canal is essential due to the presence of the neurovascular bundle, which must be preserved. It has been suggested that problems affecting the BMC may occur during local anesthesia [18], implant placement [19], bone harvesting, and mandibular osteotomy procedures [20]. In recent years, corrective preoperative approaches and the identification of anatomical anomalies have made significant progress thanks to improvements in technology and the widespread use of CBCT. The prevalence of BMCs estimated in the present study was 9.87% out of the total hemi-mandibles evaluated, and these data seem to be in line with the very wide range provided in the literature, which detects incidences from 0.08% to 65.0% [1]. However, the presence of such a wide range was due to the strongly discordant results between studies conducted using panoramic radiography and those performed using CBCT. Since Naitoh et al.’s classification [11] was the first using CBCT, all the studies before this one used panoramic radiographies. Considering that the present work used CBCT scans, the data reported in this study should be compared to studies that also used CBCT scans. As stated by Naitoh M et al. [11], the anterior canal is the most common type (27.9%), while the buccolingual canal is the least common (0.8%). Orhan K et al. [21] used the same classification on a Turkish population and found the anterior canal to be the most common type (17.8%), although the dental canal was the least common (4.3%). In the present study, the retromolar canal was the most common type (3.57%), while the trifid canal was the rarest (0.42%), meaning that our results align with studies by Kang JH et al. [22] and Rashsuren O et al. [1] on a Korean population. Finally, it is necessary to point out that Naitoh et al.’s classification does not include classes for the TMC; however, in this study, we included two trifid cases. The BMCs contain neurovascular bundles which, if damaged during a surgical procedure, can lead to complications such as traumatic neuroma and paraesthesia, anesthesia, and intraoperative/postoperative bleeding.
As evidence of this, the retromolar canal may be particularly at risk of injury during the extraction of an impacted third molar due to its location adjacent to the tooth or during autologous bone harvesting, as this area is often used as a donor site. Furthermore, It should be noted that canals that bifurcate lingually or buccally cannot be verified with panoramic radiographs; therefore, increasing general awareness of the limitations of dimensional images in this area is crucial. Another consideration regarding the suspicion of a possible bifurcation can be made in purely clinical settings. It is well known that bifid mandibular canals, regardless of type, may be associated with greater difficulty in achieving inferior alveolar nerve involvement when performing an incision. In particular, this difficulty is expressed in the presence of soft tissue anesthesia around the injection site, the ipsilateral lip, and the chin (but not for the teeth). The most commonly administered injection point for anesthesia is often inferior to the location of bifurcation in the mandibular ramus; thus, the Akinosi technique or the Gow-Gates technique can be used, injecting the anesthetic solution at a higher level before the bifurcation of MC [23].
Nithya J et al. [16] expressed the problem of discomfort or pain in patients with BMCs and mandibular prostheses because of the pression located in the area of the additional neurovascular bundle.
Moreover, Shen EC et al. [24] observed that 32.4% of BMCs were located in the potential position for dental implant placement. Regarding age and sex distribution, Okumuş Ö et al. [25] affirmed that the difference between genders was not significant. In fact, Fu E et al. [26] discovered that gender variations were due to the population studied rather than the type of imaging employed. Regarding age groups, Kang JH et al. [22] stated that there was no significant difference in terms of incidence; however, BMCs were more frequent in patients aged 30 or above. The present study agreed with these data. To the best of the authors’ knowledge, no specific age groups have been expressed for TMCs in the existing literature.
Chavez ME et al. [27] suggested a model whereby the BMC and TMC are formed at birth. According to this model, during embryonic maturation, three canals develop in the body of the mandible and subsequently fuse to form a single canal. The first canal to form is the one directed towards the incisors, followed by the canal towards the deciduous molars, and finally by one or more canals towards the permanent molars. Similarly, the inferior alveolar nerve initially appears as three individual nerve pathways, which then merge to create a single nerve. An incomplete fusion of the nerves around which ossification takes place produces a bifid canal.
Limitations of the Study
The present observational cross-sectional study had some limitations, namely, the sampling technique, the absence of calibration, the number of samples, and the absence of an intra-/inter-rater reliability test. The introduction of a calibration system in the screening phase and the enlargement samples should be considered for future studies.
5. Conclusions
In conclusion, BMCs were more common than TMCs. These variants are more frequently unilateral. The occurrence of BMCs and TMCs should always kept in mind for clinicians operating in the posterior mandible for surgery or endodontic treatments and also for inferior alveolar nerve block anesthesia. Intraoperative and postoperative complications may be avoided by using CBCT and carefully analyzing the resulting scans. The presence of BMCs and TMCs may be considered as a risk factor for the onset of neurovascular complications.
Author Contributions
Conceptualization, S.D. and A.B.; methodology, S.D.; software, A.B.; validation, M.D., E.F. and G.V.; formal analysis, S.D.; investigation, S.D. and A.B.; data curation, A.B.; writing—original draft preparation, S.D.; writing—review and editing, M.D.; visualization, E.F. and G.V.; supervision, S.D. and M.D.; project administration, M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The protocol was submitted to the Ethics Committee of University G. d’Annunzio of Chieti and granted an IRB exemption as the study was retrospective.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Data are unavailable due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Correction Statement
This article has been republished with a minor correction of the information included in the Institutional Review Board Statement. This change does not affect the scientific content of the article.
References
- Rashsuren, O.; Choi, J.W.; Han, W.J.; Kim, E.K. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci. Dent. 2014, 44, 229–236. [Google Scholar] [CrossRef]
- Thakur, N.; Kumar, A.; Singh, P.; Gopalakrishnan, D.; Mishra, B.P.; Jha, M.S. Assessment of Anatomical Variations of Mandibular Canal Depicted in Panoramic Radiography. J. Pharm. Bioallied. Sci. 2021, 13 (Suppl. S2), S1394–S1397. [Google Scholar] [CrossRef] [PubMed]
- Miličević, A.; Salarić, I.; Đanić, P.; Miličević, H.; Macan, K.; Orihovac, Ž.; Zajc, I.; Brajdić, D.; Macan, D. Anatomical Variations of the Bifid Mandibular Canal on Panoramic Radiographs in Citizens from Zagreb, Croatia. Acta Stomatol. Croat. 2021, 55, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.M.; Peñarrocha, M.; Soler, F. Bifid mandibular canal. J. Oral Maxillofac. Surg. 2003, 61, 422–424. [Google Scholar] [CrossRef] [PubMed]
- Claeys, V.; Wackens, G. Bifid mandibular canal: Literature review and case report. Dentomaxillofac. Radiol. 2005, 34, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Naitoh, M.; Hiraiwa, Y.; Aimiya, H.; Gotoh, M.; Ariji, Y.; Izumi, M.; Kurita, K.; Ariji, E. Bifid mandibular canal in Japanese. Implant Dent. 2007, 16, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Rouas, P.; Nancy, J.; Bar, D. Identification of double mandibular canals: Literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac. Radiol. 2007, 36, 34–38. [Google Scholar] [CrossRef]
- Soman, C.; Wahass, T.; Alahmari, H.; Alamri, N.; Albiebi, A.; Alhabashy, M.; Talha, A.; Alqhtani, N. Prevalence and Characterization of bifid mandibular Canal Using Cone Beam Computed Tomography: A Retrospective Cross-Sectional Study in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2022, 14, 297–306. [Google Scholar] [CrossRef] [PubMed]
- De Castro, M.A.A.; Barra, S.G.; Vich, M.O.L.; Abreu, M.H.G.; Mesquita, R.A. Mandibular canal branching assessed with cone beam computed tomography. Radiol. Med. 2018, 123, 601–608. [Google Scholar] [CrossRef]
- Shan, S.; Zhong, S.; Li, J.; Wang, T. Systematic review and meta-analysis of mandibular canal variations on cone beam computed tomography. Oral Radiol. 2022, 38, 445–451. [Google Scholar] [CrossRef]
- Naitoh, M.; Hiraiwa, Y.; Aimiya, H.; Ariji, E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int. J. Oral Maxillofac. Implants 2009, 24, 155–159. [Google Scholar]
- Reia, V.C.B.; de Toledo Telles-Araujo, G.; Peralta-Mamani, M.; Biancardi, M.R.; Rubira, C.M.F.; Rubira-Bullen, I.R.F. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 4721–4733. [Google Scholar] [CrossRef]
- Valenzuela-Fuenzalida, J.J.; Cariseo, C.; Gold, M.; Díaz, D.; Orellana, M.; Iwanaga, J. Anatomical variations of the mandibular canal and their clinical implications in dental practice: A literature review. Surg. Radiol. Anat. 2021, 43, 1259–1272. [Google Scholar] [CrossRef]
- Haas, L.F.; Dutra, K.; Porporatti, A.L.; Mezzomo, L.A.; De Luca Canto, G.; Flores-Mir, C.; Corrêa, M. Anatomical variations of mandibular canal detected by panoramic radiography and CT: A systematic review and meta-analysis. Dentomaxillofac. Radiol. 2016, 45, 20150310. [Google Scholar] [CrossRef] [PubMed]
- Ngeow, W.C.; Chai, W.L. The clinical anatomy of accessory mandibular canal in dentistry. Clin. Anat. 2020, 33, 1214–1227. [Google Scholar] [CrossRef] [PubMed]
- Nithya, J.; Aswath, N. Assessing the Prevalence and Morphological Characteristics of Bifid Mandibular Canal Using Cone-Beam Computed Tomography—A Retrospective Cross-Sectional Study. J. Clin. Imaging Sci. 2020, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Sîrbu, V.D.; Perlea, P.; Nimigean, V.R.; Bădiţă, D.G.; Şerban, A.; Nimigean, V. Morphological assessment of the mandibular canal trajectory in dentate subjects. Rom. J. Morphol. Embryol. 2017, 58, 1401–1408. [Google Scholar]
- Fuentes, R.; Farfán, C.; Astete, N.; Garay, I.; Dias, F.; Arias, A. Bilateral bifid mandibular canal: A case report using cone beam computed tomography. Folia Morphol. 2018, 77, 780–784. [Google Scholar] [CrossRef]
- Kageyama, I.; Maeda, S.; Takezawa, K. Importance of anatomy in dental implant surgery. J. Oral Biosci. 2021, 63, 142–152. [Google Scholar] [CrossRef]
- Zhou, X.; Gao, X.; Zhang, J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg. Radiol. Anat. 2020, 42, 1073–1079. [Google Scholar] [CrossRef]
- Orhan, K.; Aksoy, S.; Bilecenoglu, B.; Sakul, B.U.; Paksoy, C.S. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: A retrospective study. Surg. Radiol. Anat. 2011, 33, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Lee, K.S.; Oh, M.G.; Choi, H.Y.; Lee, S.R.; Oh, S.H.; Choi, Y.J.; Kim, G.T.; Choi, Y.S.; Hwang, E.H. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci. Dent. 2014, 44, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A.; Pai, K.M.; Mupparapu, M. Multiple mandibular nerve canals: Radiographic observations and clinical relevance. Report of 6 cases. Quintessence Int. 2007, 38, 781–787. [Google Scholar]
- Shen, E.C.; Fu, E.; Fu, M.M.; Peng, M. Configuration and corticalization of the mandibular bifid canal in a Taiwanese adult population: A computed tomography study. Int. J. Oral Maxillofac. Implants 2014, 29, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Okumuş, Ö.; Dumlu, A. Prevalence of bifid mandibular canal according to gender, type and side. J. Dent. Sci. 2019, 14, 126–133. [Google Scholar] [CrossRef]
- Fu, E.; Peng, M.; Chiang, C.Y.; Tu, H.P.; Lin, Y.S.; Shen, E.C. Bifid mandibular canals and the factors associated with their presence: A medical computed tomography evaluation in a Taiwanese population. Clin. Oral Implants Res. 2014, 25, e64–e67. [Google Scholar] [CrossRef]
- Chávez-Lomeli, M.E.; Mansilla Lory, J.; Pompa, J.A.; Kjaer, I. The human mandibular canal arises from three separate canals innervating different tooth groups. J. Dent. Res. 1996, 75, 1540–1544. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).