Strategy for the Construction of SARS-CoV-2 S and N Recombinant Proteins and Their Immunogenicity Evaluation
Abstract
1. Introduction
2. Materials and Methods
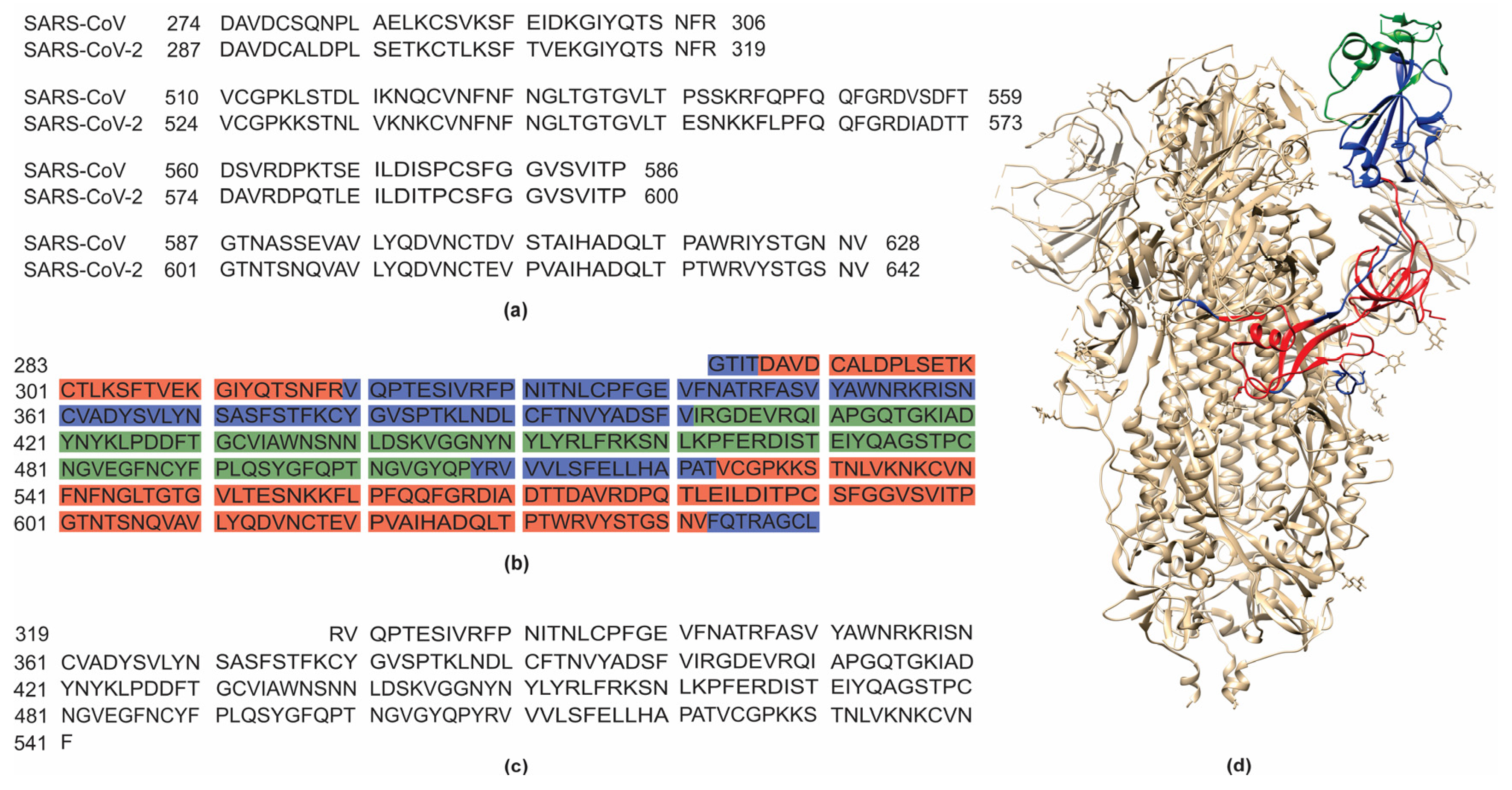
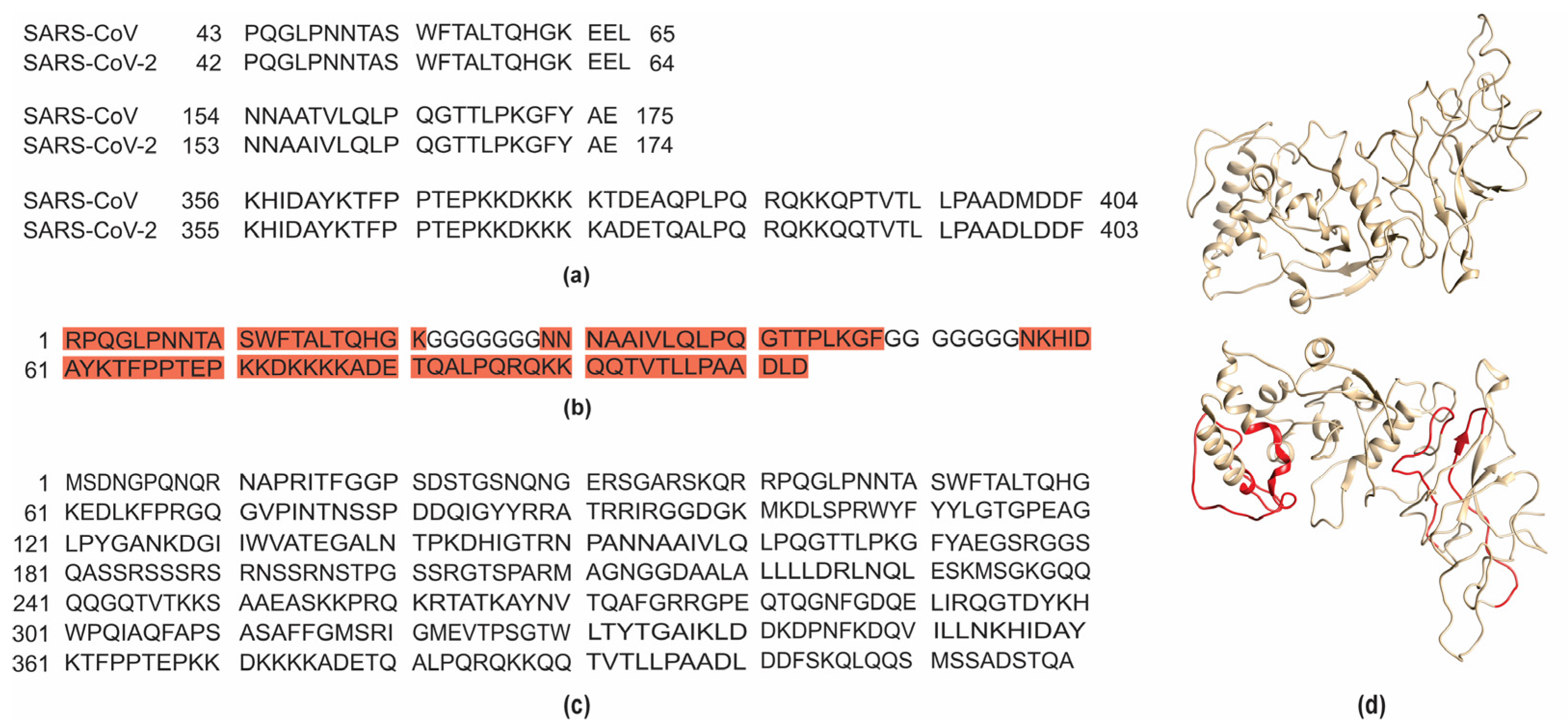
2.1. Analysis of B-Cell Epitopes, Protein Design, and Construction of Expression Vectors for S and N Recombinant Proteins
2.2. Expression of pET28aS_epit, pET28aN_epit, and Controls in E. coli and Recombinant Proteins Purification
2.3. Mice Immunization
2.4. Blood Samples
2.5. ELISA
2.6. Statistical Analysis
3. Results and Discussion
3.1. pET28aS_epit and pET28aN_epit Constructs, and In Silico Analysis of the S_ epit and N_epit Recombinant Proteins
3.2. SARS-CoV-2 S and N Recombinant Proteins Are Expressed in Escherichia coli BL21 (DE3) Star
3.3. S_epit and N_epit Induce Humoral Immune Response in Mice and Are Recognized by Sera from COVID-19-Positive and/or Vaccinated Humans
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. A Pneumonia Outbreak Associated with a New Coronavirus of Probable Bat Origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Lauxmann, M.A.; Santucci, N.E.; Autrán-Gómez, A.M. The SARS-CoV-2 Coronavirus and the COVID-19 Outbreak. Int. Braz. J. Urol 2020, 46, 6–18. [Google Scholar] [CrossRef]
- Mingaleeva, R.N.; Nigmatulina, N.A.; Sharafetdinova, L.M.; Romozanova, A.M.; Gabdoulkhakova, A.G.; Filina, Y.V.; Shavaliyev, R.F.; Rizvanov, A.A.; Miftakhova, R.R. Biology of the SARS-CoV-2 Coronavirus. Biochemistry 2022, 87, 1662–1678. [Google Scholar] [CrossRef]
- El-Maradny, Y.A.; Badawy, M.A.; Mohamed, K.I.; Ragab, R.F.; Moharm, H.M.; Abdallah, N.A.; Elgammal, E.M.; Rubio-Casillas, A.; Uversky, V.N.; Redwan, E.M. Unraveling the Role of the Nucleocapsid Protein in SARS-CoV-2 Pathogenesis: From Viral Life Cycle to Vaccine Development. Int. J. Biol. Macromol. 2024, 279, 135201. [Google Scholar] [CrossRef] [PubMed]
- Alhamlan, F.S.; Al-Qahtani, A.A. SARS-CoV-2 Variants: Genetic Insights, Epidemiological Tracking, and Implications for Vaccine Strategies. Int. J. Mol. Sci. 2025, 26, 1263. [Google Scholar] [CrossRef]
- Wang, M.Y.; Zhao, R.; Gao, L.J.; Gao, X.F.; Wang, D.P.; Cao, J.M. SARS-CoV-2: Structure, Biology, and Structure-Based Therapeutics Development. Front. Cell. Infect. Microbiol. 2020, 10, 587269. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, J.B.; García, A.H.; Moreno, D.; Hajduch, M. Coronavirus Infection: An Immunologists’ Perspective. Scand J. Immunol. 2021, 93, e13043. [Google Scholar] [CrossRef]
- Le Bert, N.; Tan, A.T.; Kunasegaran, K.; Tham, C.Y.L.; Hafezi, M.; Chia, A.; Chng, M.H.Y.; Lin, M.; Tan, N.; Linster, M.; et al. SARS-CoV-2-Specific T Cell Immunity in Cases of COVID-19 and SARS, and Uninfected Controls. Nature 2020, 584, 457–462. [Google Scholar] [CrossRef]
- Weiskopf, D.; Immunol, S.; Weiskopf, D.; Schmitz, K.S.; Raadsen, M.P.; Grifoni, A.; Okba, N.M.A.; Van Den Akker, J.P.C.; Molenkamp, R.; Koopmans, M.P.G.; et al. Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci. Immunol. 2020, 2071, 1–15. [Google Scholar]
- Li, G.; Fan, Y.; Lai, Y.; Han, T.; Li, Z.; Zhou, P.; Pan, P.; Wang, W.; Hu, D.; Liu, X.; et al. Coronavirus Infections and Immune Responses. J. Med. Virol. 2020, 92, 424–432. [Google Scholar] [CrossRef]
- Yadav, R.; Chaudhary, J.K.; Jain, N.; Chaudhary, P.K.; Khanra, S.; Dhamija, P.; Sharma, A.; Kumar, A.; Handu, S. Role of Structural and Non-Structural Proteins and Therapeutic Targets of SARS-CoV-2 for COVID-19. Cells 2021, 10, 821. [Google Scholar] [CrossRef]
- Grifoni, A.; Sidney, J.; Zhang, Y.; Scheuermann, R.H.; Peters, B.; Sette, A. A Sequence Homology and Bioinformatic Approach Can Predict Candidate Targets for Immune Responses to SARS-CoV-2. Cell Host Microbe 2020, 27, 671–680.e2. [Google Scholar] [CrossRef] [PubMed]
- Vidal, L.E.L.; Figueira-Mansur, J.; Jurgilas, P.B.; Argondizzo, A.P.C.; Pestana, C.P.; Martins, F.O.; da Silva Junior, H.C.; Miguez, M.; Loureiro, B.O.; Marques, C.d.F.S.; et al. Process Development and Characterization of Recombinant Nucleocapsid Protein for Its Application on COVID-19 Diagnosis. Protein Expr. Purif. 2023, 207, 106263. [Google Scholar] [CrossRef] [PubMed]
- Simões, R.S.d.Q.; Rodríguez-Lázaro, D. Classical and Next-Generation Vaccine Platforms to SARS-CoV-2: Biotechnological Strategies and Genomic Variants. Int. J. Environ. Res. Public Health 2022, 19, 2392. [Google Scholar] [CrossRef]
- Kovalenko, A.; Ryabchevskaya, E.; Evtushenko, E.; Nikitin, N.; Karpova, O. Recombinant Protein Vaccines against Human Betacoronaviruses: Strategies, Approaches and Progress. Int. J. Mol. Sci. 2023, 24, 1701. [Google Scholar] [CrossRef] [PubMed]
- Tarke, A.; Grifoni, A.; Sette, A. Bioinformatic and Experimental Analysis of T Cell Immune Reactivity to SARS-CoV-2 and Its Variants. Front. Bioinform. 2022, 2, 876380. [Google Scholar] [CrossRef] [PubMed]
- Deepthi, V.; Sasikumar, A.; Mohanakumar, K.P.; Rajamma, U. Computationally Designed Multi-Epitope Vaccine Construct Targeting the SARS-CoV-2 Spike Protein Elicits Robust Immune Responses in Silico. Sci. Rep. 2025, 15, 9562. [Google Scholar] [CrossRef]
- Eswar, N.; John, B.; Mirkovic, N.; Fiser, A.; Ilyin, V.A.; Pieper, U.; Stuart, A.C.; Marti-Renom, M.A.; Madhusudhan, M.S.; Yerkovich, B.; et al. Tools for Comparative Protein Structure Modeling and Analysis. Nucleic Acids Res. 2003, 31, 3375–3380. [Google Scholar] [CrossRef]
- Šali, A.; Blundell, T.L. Comparative Protein Modelling by Satisfaction of Spatial Restraints. J. Mol. Biol. 1993, 234, 779–815. [Google Scholar] [CrossRef]
- Yuan, M.; Liu, H.; Wu, N.C.; Wilson, I.A. Recognition of the SARS-CoV-2 Receptor Binding Domain by Neutralizing Antibodies. Biochem. Biophys. Res. Commun. 2021, 538, 192–203. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A Visualization System for Exploratory Research and Analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
- Gasteiger, E.; Hoogland, C.; Gattiker, A.; Duvaud, S.; Wilkins, M.R.; Appel, R.D.; Bairoch, A. Protein Identification and Analysis Tools on the ExPASy Server. In The Proteomics Protocols Handbook; Springer: Berlin/Heidelberg, Germany, 2005; pp. 571–607. [Google Scholar] [CrossRef]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A Server for Prediction of Protective Antigens, Tumour Antigens and Subunit Vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Krogh, A.; Larsson, B.; Von Heijne, G.; Sonnhammer, E.L.L. Predicting Transmembrane Protein Topology with a Hidden Markov Model: Application to Complete Genomes. J. Mol. Biol. 2001, 305, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Hall, T. BioEdit: A User-Friendly Biological Sequence Alignment Editor and Analysis Program for Windows 95/98/NT. Nucleic Acids Symp. Ser. 1999, 41, 95–98. [Google Scholar]
- Green, M.R.; Sambrook, J. Cloning and Transformation with Plasmid Vectors. Cold Spring Harb. Protoc. 2021, 2021, 420–436. [Google Scholar] [CrossRef]
- Laemmli, U.K. Cleavage of Structural Proteins during the Assembly of the Head of Bacteriophage T4. Nature 1970, 227, 680–685. [Google Scholar] [CrossRef]
- Ghaemi, A.; Roshani Asl, P.; Zargaran, H.; Ahmadi, D.; Hashimi, A.A.; Abdolalipour, E.; Bathaeian, S.; Miri, S.M. Recombinant COVID-19 Vaccine Based on Recombinant RBD/Nucleoprotein and Saponin Adjuvant Induces Long-Lasting Neutralizing Antibodies and Cellular Immunity. Front. Immunol. 2022, 13, 974364. [Google Scholar] [CrossRef]
- Nazarian, S.; Olad, G.; Abdolhamidi, R.; Motamedi, M.J.; Kazemi, R.; Kordbacheh, E.; Felagari, A.; Olad, H.; Ahmadi, A.; Bahiraee, A.; et al. Preclinical Study of Formulated Recombinant Nucleocapsid Protein, the Receptor Binding Domain of the Spike Protein, and Truncated Spike (S1) Protein as Vaccine Candidates against COVID-19 in Animal Models. Mol. Immunol. 2022, 149, 107–118. [Google Scholar] [CrossRef]
- Chen, W.H.; Pollet, J.; Strych, U.; Lee, J.; Liu, Z.; Kundu, R.T.; Versteeg, L.; Villar, M.J.; Adhikari, R.; Wei, J.; et al. Yeast-Expressed Recombinant SARS-CoV-2 Receptor Binding Domain RBD203-N1 as a COVID-19 Protein Vaccine Candidate. Protein Expr. Purif. 2022, 190, 106003. [Google Scholar] [CrossRef]
- Rabdano, S.O.; Ruzanova, E.A.; Pletyukhina, I.V.; Saveliev, N.S.; Kryshen, K.L.; Katelnikova, A.E.; Beltyukov, P.P.; Fakhretdinova, L.N.; Safi, A.S.; Rudakov, G.O.; et al. Immunogenicity and In Vivo Protective Effects of Recombinant Nucleocapsid-Based SARS-CoV-2 Vaccine Convacell®. Vaccines 2023, 11, 874. [Google Scholar] [CrossRef]
- Primard, C.; Monchâtre-Leroy, E.; Del Campo, J.; Valsesia, S.; Nikly, E.; Chevandier, M.; Boué, F.; Servat, A.; Wasniewski, M.; Picard-Meyer, E.; et al. OVX033, a Nucleocapsid-Based Vaccine Candidate, Provides Broad-Spectrum Protection against SARS-CoV-2 Variants in a Hamster Challenge Model. Front. Immunol. 2023, 14, 1188605. [Google Scholar] [CrossRef]
- Silva, E.K.V.B.; Bomfim, C.G.; Barbosa, A.P.; Noda, P.; Noronha, I.L.; Fernandes, B.H.V.; Machado, R.R.G.; Durigon, E.L.; Catanozi, S.; Rodrigues, L.G.; et al. Immunization with SARS-CoV-2 Nucleocapsid Protein Triggers a Pulmonary Immune Response in Rats. PLoS ONE 2022, 17, e0268434. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Peng, Y.; Huang, B.; Ding, X.; Wang, X.; Niu, P.; Meng, J.; Zhu, Z.; Zhang, Z.; Wang, J.; et al. Genome Composition and Divergence of the Novel Coronavirus (2019-NCoV) Originating in China. Cell Host Microbe 2020, 27, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Nithya Shree, J.; Premika, T.; Sharlin, S.; Annie Aglin, A. Diverse Approaches to Express Recombinant Spike Protein: A Comprehensive Review. Protein Expr. Purif. 2024, 223, 106556. [Google Scholar] [CrossRef]
- Ghaderi, H.; Shoari, A.; Salehi, S.; Eskafi, A.H.; Habibi-Anbouhi, M.; Cohan, R.A.; Moazzami, R.; Behdani, M. Expression and Purification of SARS-CoV-2 Receptor Binding Domain in Escherichia Coli for Diagnostic and Therapeutic Purposes. Res. Pharm. Sci. 2024, 19, 500. [Google Scholar] [CrossRef]
- Djukic, T.; Mladenovic, M.; Stanic-Vucinic, D.; Radosavljevic, J.; Smiljanic, K.; Sabljic, L.; Devic, M.; Cujic, D.; Vasovic, T.; Simovic, A.; et al. Expression, Purification and Immunological Characterization of Recombinant Nucleocapsid Protein Fragment from SARS-CoV-2. Virology 2021, 557, 15–22. [Google Scholar] [CrossRef]
- Bhatwa, A.; Wang, W.; Hassan, Y.I.; Abraham, N.; Li, X.Z.; Zhou, T. Challenges Associated with the Formation of Recombinant Protein Inclusion Bodies in Escherichia Coli and Strategies to Address Them for Industrial Applications. Front. Bioeng. Biotechnol. 2021, 9, 630551. [Google Scholar] [CrossRef]
- Chan, P.; Curtis, R.A.; Warwicker, J. Soluble Expression of Proteins Correlates with a Lack of Positively-Charged Surface. Sci. Rep. 2013, 3, 3333. [Google Scholar] [CrossRef]
- Kamtekar, S.; Schiffer, J.M.; Xiong, H.; Babik, J.M.; Hecht, M.H. Protein Design by Binary Patterning of Polar and Nonpolar Amino Acids. Science 1993, 262, 1680–1685. [Google Scholar] [CrossRef] [PubMed]
- Falak, S.; Sajed, M.; Rashid, N. Strategies to Enhance Soluble Production of Heterologous Proteins in Escherichia Coli. Biologia 2022, 77, 893–905. [Google Scholar] [CrossRef]
- Qing, R.; Hao, S.; Smorodina, E.; Jin, D.; Zalevsky, A.; Zhang, S. Protein Design: From the Aspect of Water Solubility and Stability. Chem. Rev. 2022, 122, 14085–14179. [Google Scholar] [CrossRef]
- Wang, C.; Zou, Q. Prediction of Protein Solubility Based on Sequence Physicochemical Patterns and Distributed Representation Information with DeepSoluE. BMC Biol. 2023, 21, 12. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.X.; Nong, F.T.; Wang, Y.Z.; Yan, C.X.; Gu, Y.; Song, P.; Sun, X.M. Strategies for Efficient Production of Recombinant Proteins in Escherichia Coli: Alleviating the Host Burden and Enhancing Protein Activity. Microb. Cell Fact. 2022, 21, 191. [Google Scholar] [CrossRef] [PubMed]
- Ramos, F.F.; Pereira, I.A.G.; Cardoso, M.M.; Bandeira, R.S.; Lage, D.P.; Scussel, R.; Anastacio, R.S.; Freire, V.G.; Melo, M.F.N.; Oliveira-da-Silva, J.A.; et al. B-Cell Epitopes-Based Chimeric Protein from SARS-CoV-2 N and S Proteins Is Recognized by Specific Antibodies in Serum and Urine Samples from Patients. Viruses 2023, 15, 1877. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.d.O.; Castro-Amarante, M.F.; Venceslau-Carvalho, A.A.; Almeida, B.d.S.; Daher, I.P.; Souza-Silva, G.A.d.; Yamamoto, M.M.; Koike, G.; de Souza, E.E.; Wrenger, C.; et al. Enhanced Immunogenicity and Protective Effects against SARS-CoV-2 Following Immunization with a Recombinant RBD-IgG Chimeric Protein. Vaccines 2024, 12, 356. [Google Scholar] [CrossRef] [PubMed]
- D’Atri, V.; Imiołek, M.; Quinn, C.; Finny, A.; Lauber, M.; Fekete, S.; Guillarme, D. Size Exclusion Chromatography of Biopharmaceutical Products: From Current Practices for Proteins to Emerging Trends for Viral Vectors, Nucleic Acids and Lipid Nanoparticles. J. Chromatogr. A 2024, 1722, 464862. [Google Scholar] [CrossRef]
- Feng, W.; Xiang, Y.; Wu, L.; Chen, Z.; Li, Q.; Chen, J.; Guo, Y.; Xia, D.; Chen, N.; Zhang, L.; et al. Nucleocapsid Protein of SARS-CoV-2 Is a Potential Target for Developing New Generation of Vaccine. J. Clin. Lab. Anal. 2022, 36, e24479. [Google Scholar] [CrossRef]
- Rak, A.; Isakova-Sivak, I.; Rudenko, L. Overview of Nucleocapsid-Targeting Vaccines against COVID-19. Vaccines 2023, 11, 1810. [Google Scholar] [CrossRef]
- Dobaño, C.; Santano, R.; Jiménez, A.; Vidal, M.; Chi, J.; Rodrigo Melero, N.; Popovic, M.; López-Aladid, R.; Fernández-Barat, L.; Tortajada, M.; et al. Immunogenicity and Crossreactivity of Antibodies to the Nucleocapsid Protein of SARS-CoV-2: Utility and Limitations in Seroprevalence and Immunity Studies. Transl. Res. 2021, 232, 60–74. [Google Scholar] [CrossRef]
- De Marco Verissimo, C.; O’Brien, C.; López Corrales, J.; Dorey, A.; Cwiklinski, K.; Lalor, R.; Doyle, J.M.; Field, S.; Masterson, C.; Martinez, E.R.; et al. Improved Diagnosis of SARS-CoV-2 by Using Nucleoprotein and Spike Protein Fragment 2 in Quantitative Dual ELISA Tests. Epidemiol. Infect. 2021, 149, e140. [Google Scholar] [CrossRef]
- Zhang, L.; Zheng, B.; Gao, X.; Zhang, L.; Pan, H.; Qiao, Y.; Suo, G.; Zhu, F. Development of Patient-Derived Human Monoclonal Antibodies Against Nucleocapsid Protein of Severe Acute Respiratory Syndrome Coronavirus 2 for Coronavirus Disease 2019 Diagnosis. Front. Immunol. 2020, 11, 595970. [Google Scholar] [CrossRef]
- Schunk, M.K.; Macallum, G.E. Applications and Optimization of Immunization Procedures. ILAR J 2005, 46, 241–257. [Google Scholar] [CrossRef] [PubMed]
- Mamat, U.; Wilke, K.; Bramhill, D.; Schromm, A.B.; Lindner, B.; Kohl, T.A.; Corchero, J.L.; Villaverde, A.; Schaffer, L.; Head, S.R.; et al. Detoxifying Escherichia Coli for Endotoxin-Free Production of Recombinant Proteins. Microb. Cell Fact. 2015, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Shahar, E.; Emquies, K.; Bloch, I.; Eliahu, D.; Ben Adiva, R.; Pitcovski, J.; Yadid, I. Endotoxin-Free Gram-Negative Bacterium as a System for Production and Secretion of Recombinant Proteins. Appl. Microbiol. Biotechnol. 2023, 107, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Alcantara, L.C.J.; Nogueira, E.; Shuab, G.; Tosta, S.; Fristch, H.; Pimentel, V.; Souza-Neto, J.A.; Coutinho, L.L.; Fukumasu, H.; Sampaio, S.C.; et al. SARS-CoV-2 Epidemic in Brazil: How the Displacement of Variants Has Driven Distinct Epidemic Waves. Virus Res. 2022, 315, 198785. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borges, P.H.G.; Gregio, B.; Suzukawa, H.T.; Silva-Rodrigues, G.; Andreassa, E.d.C.; Castro, I.M.d.; Bartolomeu-Gonçalves, G.; Venancio, E.J.; Pinge-Filho, P.; Góes, V.M.; et al. Strategy for the Construction of SARS-CoV-2 S and N Recombinant Proteins and Their Immunogenicity Evaluation. BioTech 2025, 14, 38. https://doi.org/10.3390/biotech14020038
Borges PHG, Gregio B, Suzukawa HT, Silva-Rodrigues G, Andreassa EdC, Castro IMd, Bartolomeu-Gonçalves G, Venancio EJ, Pinge-Filho P, Góes VM, et al. Strategy for the Construction of SARS-CoV-2 S and N Recombinant Proteins and Their Immunogenicity Evaluation. BioTech. 2025; 14(2):38. https://doi.org/10.3390/biotech14020038
Chicago/Turabian StyleBorges, Paulo Henrique Guilherme, Barbara Gregio, Helena Tiemi Suzukawa, Gislaine Silva-Rodrigues, Emanuella de Castro Andreassa, Isabela Madeira de Castro, Guilherme Bartolomeu-Gonçalves, Emerson José Venancio, Phileno Pinge-Filho, Viviane Monteiro Góes, and et al. 2025. "Strategy for the Construction of SARS-CoV-2 S and N Recombinant Proteins and Their Immunogenicity Evaluation" BioTech 14, no. 2: 38. https://doi.org/10.3390/biotech14020038
APA StyleBorges, P. H. G., Gregio, B., Suzukawa, H. T., Silva-Rodrigues, G., Andreassa, E. d. C., Castro, I. M. d., Bartolomeu-Gonçalves, G., Venancio, E. J., Pinge-Filho, P., Góes, V. M., Nakamura, C. V., Tavares, E. R., Souza, T. d. A. C. B. d., Yamada-Ogatta, S. F., & Yamauchi, L. M. (2025). Strategy for the Construction of SARS-CoV-2 S and N Recombinant Proteins and Their Immunogenicity Evaluation. BioTech, 14(2), 38. https://doi.org/10.3390/biotech14020038







