Privacy Implications of Contacting the At-Risk Relatives of Patients with Medically Actionable Genetic Predisposition, with Patient Consent: A Hypothetical Australian Case Study
Abstract
1. Introduction
2. Materials and Methods
- 1.
- What are the relevant Australian Commonwealth and state/territory privacy regulations?
- 2.
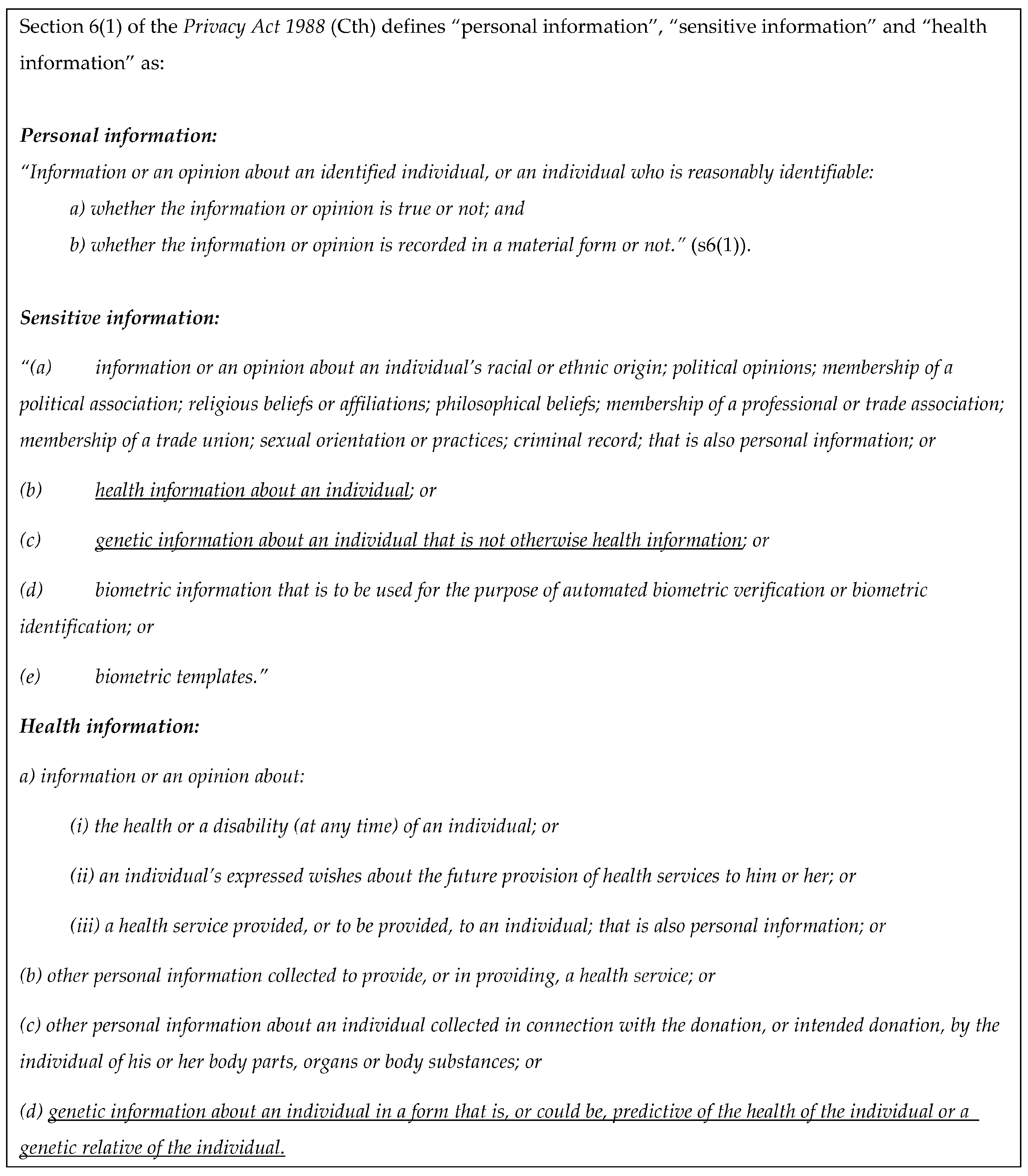
- Are the types of information collected and used in Letters S1/S2 protected under privacy regulations?
- 3.
- Has the genetics service breached its privacy obligations by notifying Darcy directly in the hypothetical case study provided (Figure 1)?
3. Results
3.1. What Are the Relevant Australian Commonwealth and State/Territory Privacy Regulations?
3.2. Are the Types of Information Collected and Used in Letters S1/S2 Protected under Privacy Regulations?
4. Discussion
4.1. How Is the Use of Each Type of Information Identified in the Case Study Regulated by the Relevant Regulations?
4.1.1. Darcy’s Contact Details
4.1.2. The Genetic Information
- Darcy’s contact details are personal information and must be collected and used in accordance with the regulations applicable to personal information.
- The information contained in Letters S1 and S2 is Darcy’s personal information.
- The genetic information contained in Letter S2 (which names the specific gene) is likely to also be Darcy’s sensitive information, and must be used and/or disclosed in accordance with the regulations applicable to sensitive information.
- It is unclear whether the information contained in Letter S1 (which does not name the specific gene and provides general information only) is sensitive information, but to be prudent it should be used and/or disclosed in accordance with the regulations applicable to sensitive information.
- Simon’s genetic information alone is not Darcy’s personal information.
4.2. Are the Proposed Uses a Breach of Privacy?
4.2.1. APP 3: Collection of Solicited Personal Information
4.2.2. APP 5: Notification of Individuals
4.2.3. APP 6: Use or Disclosure of Personal Information
- This analysis supports a conclusion that collection of Darcy’s contact details without her consent is allowed under all Australian privacy regulations, for the purpose of notifying her of her possible genetic risk.
- Reasonable steps should be taken to protect Darcy’s personal information once collected.
- Darcy should be notified as soon as possible after her contact details are collected, about the purpose of the collection and avenues to complain about breach of privacy.
- Darcy’s personal information (her contact details) can only be used for the primary purpose for which it was collected (to notify her about her possible genetic risk), not for any other purpose (without her consent).
- Disclosure of Simon’s genetic information to Darcy is permitted with his consent.
- Disclosure of Darcy’s own genetic information to her is permitted, and the purported “right not to know” does not prevent the disclosure of this information to Darcy, though her autonomy should be respected if she chooses not to pursue this further once notified.
- There is no positive duty on HPs to contact relatives directly to notify them of their risk—the discretion available to HPs to notify patients’ at-risk relatives directly is not an obligation.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marleen van den Heuvel, L.; Stemkens, D.; van Zelst-Stams, W.A.G.; Willeboordse, F.; Christiaans, I. How to inform at-risk relatives? Attitudes of 1379 Dutch patients, relatives, and members of the general population. J. Genet. Couns. 2020, 29, 786–799. [Google Scholar] [CrossRef] [PubMed]
- Healey, E.; Taylor, N.; Greening, S.; Wakefield, C.E.; Warwick, L.; Williams, R.; Tucker, K. Quantifying family dissemination and identifying barriers to communication of risk information in Australian BRCA families. Genet. Med. 2017, 19, 1323–1331. [Google Scholar] [CrossRef]
- Tiller, J.; Bilkey, G.; Macintosh, R.; O’Sullivan, S.; Groube, S.; Palover, M.; Pachter, N.; Rothstein, M.; Lacaze, P.; Otlowski, M. Disclosing genetic information to family members without consent: Five Australian case studies. Eur. J. Med. Genet. 2020, 63, 104035. [Google Scholar] [CrossRef] [PubMed]
- Sermijn, E.; Delesie, L.; Deschepper, E.; Pauwels, I.; Bonduelle, M.; Teugels, E.; De Greve, J. The impact of an interventional counselling procedure in families with a BRCA1/2 gene mutation: Efficacy and safety. Fam. Cancer 2016, 15, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.C.; Dotson, W.D.; DeVore, C.S.; Bednar, E.M.; Bowen, D.J.; Ganiats, T.G.; Green, R.F.; Hurst, G.M.; Philp, A.R.; Ricker, C.N.; et al. Delivery of Cascade Screening for Hereditary Conditions: A Scoping Review of the Literature. Health Affairs 2018, 37, 801–808. [Google Scholar] [CrossRef]
- Henrikson, N.B.; Blasi, P.; Figueroa Gray, M.; Tiffany, B.T.; Scrol, A.; Ralston, J.D.; Fullerton, S.M.; Lim, C.Y.; Ewing, J.; Leppig, K.A. Patient and Family Preferences on Health System-Led Direct Contact for Cascade Screening. J. Pers. Med. 2021, 11, 538. [Google Scholar] [CrossRef]
- Dheensa, S.; Lucassen, A.; Fenwick, A. Limitations and Pitfalls of Using Family Letters to Communicate Genetic Risk: A Qualitative Study with Patients and Healthcare Professionals. J. Genet. Couns. 2018, 27, 689–701. [Google Scholar] [CrossRef]
- Aktan-Collan, K.; Haukkala, A.; Pylvänäinen, K.; Järvinen, H.J.; Aaltonen, L.A.; Peltomäki, P.; Rantanen, E.; Kääriäinen, H.; Mecklin, J.P. Direct contact in inviting high-risk members of hereditary colon cancer families to genetic counselling and DNA testing. J. Med. Genet. 2007, 44, 732–738. [Google Scholar] [CrossRef]
- Van den Heuvel, L.M.; Hoedemaekers, Y.M.; Baas, A.F.; Baars, M.J.; van Tintelen, J.P.; Smets, E.M.; Christiaans, I. A tailored approach to informing relatives at risk of inherited cardiac conditions: Results of a randomised controlled trial. Eur. J. Hum. Genet. 2022, 30, 203–210. [Google Scholar] [CrossRef]
- Newson, A.J. Why Genetics Services Should Contact At-Risk Relatives Directly. 2006. Available online: http://hdl.handle.net/2123/12242 (accessed on 1 November 2022).
- Marks, D.; Thorogood, M.; Neil, S.M. Cascade screening for familial hypercholesterolaemia: Implications of a pilot study for national screening programmes. J. Med. Screen. 2006, 13, 156–159. [Google Scholar] [CrossRef]
- Frey, M.K.; Ahsan, M.D.; Bergeron, H.; Lin, J.; Li, X.; Fowlkes, R.K.; Narayan, P.; Nitecki, R.; Rauh-Hain, J.A.; Moss, H.A.; et al. Cascade Testing for Hereditary Cancer Syndromes: Should We Move Toward Direct Relative Contact? A Systematic Review and Meta-Analysis. J. Clin. Oncol. 2022, 40, 4129–4143. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.; Molster, C.; Poke, S.; O’leary, P. Communicating Familial Hypercholesterolemia Genetic Information within Families. Genet. Test. Mol. Biomark. 2009, 13, 301–306. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Legge, E.; Laundy, C.S.; Egan, S.J.; French, R.; Watts, G.F.; Hagger, M.S. Patients’ Perceptions and Experiences of Familial Hypercholesterolemia, Cascade Genetic Screening and Treatment. Int. J. Behav. Med. 2015, 22, 92–100. [Google Scholar] [CrossRef]
- Suthers, G.K.; Armstrong, J.; McCormack, J.; Trott, D. Letting the family know: Balancing ethics and effectiveness when notifying relatives about genetic testing for a familial disorder. J. Med. Genet. 2006, 43, 665–670. [Google Scholar] [CrossRef]
- Tiller, J.; Stott, A.; Finlay, K.; Boughtwood, T.; Madelli, E.; Horton, A.; Winship, I.; Nowak, K.; Otlowski, M. Direct notification by health professionals of relatives at-risk of genetic conditions (with patient consent): Views of the Australian public. Eur. J. Hum. Genet, 2023; accepted. [Google Scholar]
- Australian Government Office of the Australian Information Commissioner. What Is Personal Information? Australian Government Office of the Australian Information Commissioner: Canberra, Australia, 2017. [Google Scholar]
- Paltiel, M.; Taylor, M.; Newson, A. Protection of genomic data and the Australian Privacy Act: When are genomic data ‘personal information’? Int. Data Priv. Law. 2023, 13, 47–62. [Google Scholar] [CrossRef]
- Australian Law Reform Commission. Essentially Yours: The Protection of Human. Genetic Information in Australia; Australian Law Reform Commission: Sydney, Australia, 2003. Available online: http://www.alrc.gov.au/publications/report-96 (accessed on 1 November 2022).
- Australian Government Attorney General’s Department. Privacy Act Review Report; Australian Government Attorney General’s Department. 2022. Available online: https://www.ag.gov.au/rights-and-protections/publications/privacy-act-review-report (accessed on 1 May 2023).
- Privacy Commissioner v Telstra Corp Ltd. FCAFC 4. 2017. Available online: https://www.ags.gov.au/sites/default/files/el253.pdf (accessed on 1 November 2022).
- Dharmananda, J. Using parliamentary materials in interpretation: Insights from parliamentary process. Univ. N. S. W. Law J. 2018, 41, 4–39. [Google Scholar] [CrossRef]
- Parliament of Australia. Bills Digest No. 9 2006–2007: Privacy Legislation Amendment Bill 2006. 2006. Available online: https://www.aph.gov.au/Parliamentary_Business/Bills_Legislation/bd/bd0607/07bd009 (accessed on 1 November 2022).
- Ademi, Z.; Watts, G.F.; Pang, J.; Sijbrands, E.J.; van Bockxmeer, F.M.; O’Leary, P.; Geelhoed, E.; Liew, D. Cascade screening based on genetic testing is cost-effective: Evidence for the implementation of models of care for familial hypercholesterolemia. J. Clin. Lipidol. 2014, 8, 390–400. [Google Scholar] [CrossRef]
- Bell, D.A.; Pang, J.; Burrows, S.; Bates, T.R.; van Bockxmeer, F.M.; Hooper, A.J.; O’Leary, P.; Burnett, J.R.; Watts, G.F. Effectiveness of genetic cascade screening for familial hypercholesterolaemia using a centrally co-ordinated clinical service: An Australian experience. Atherosclerosis 2015, 239, 93–100. [Google Scholar] [CrossRef]
- Courtney, E.; Chok, A.K.L.; Ting Ang, Z.L.; Shaw, T.; Li, S.T.; Yuen, J.; Ngeow, J. Impact of free cancer predisposition cascade genetic testing on uptake in Singapore. NPJ Genom. Med. 2019, 4, 22. [Google Scholar] [CrossRef]
- Frey, M.K.; Kahn, R.M.; Chapman-Davis, E.; Tubito, F.; Pires, M.; Christos, P.; Anderson, S.; Mukherjee, S.; Jordan, B.; Blank, S.V.; et al. Prospective Feasibility Trial of a Novel Strategy of Facilitated Cascade Genetic Testing Using Telephone Counseling. J. Clin. Oncol. 2020, 38, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.; Leach, E.; Virani, A.; Arbour, L.; Bartels, K.; Wong, E.K. Cascade testing for inherited arrhythmia conditions: Experiences and attitudes of family communication approaches for a Canadian cohort. J. Genet. Counsel. 2022, 31, 815–828. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Won, N.Y.; Dotson, W.D.; Wright, S.T.; Roberts, M.C. Barriers and facilitators for cascade testing in genetic conditions: A systematic review. Eur. J. Hum. Genet. 2020, 28, 1631–1644. [Google Scholar] [CrossRef]
- Tuffaha, H.W.; Mitchell, A.; Ward, R.L.; Connelly, L.; Butler, J.R.; Norris, S.; Scuffham, P.A. Cost-effectiveness analysis of germ-line BRCA testing in women with breast cancer and cascade testing in family members of mutation carriers. Genet. Med. 2018, 20, 985–994. [Google Scholar] [CrossRef]
- Human Genetics Society of Australasia. Submission to the Commonwealth Department of Health MBS Review Advisory Committee: Provision of Services by FHGSA Registered Clinical Genetic Counsellors. 2021. Available online: https://consultations.health.gov.au/medicare-reviews-unit/medicare-benefits-schedule-mbs-review-advisory-com/supporting_documents/HGSA%20Submission%20for%20MRAC%20Review.pdf (accessed on 1 January 2023).
- Forrest, L.E.; Delatycki, M.B.; Curnow, L.; Skene, L.; Aitken, M. Genetic health professionals and the communication of genetic information in families: Practice during and after a genetic consultation. Am. J. Med. Genet. Part A 2010, 152A, 1458–1466. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Kovak, K.; Cox, S.L. Aligning policy to promote cascade genetic screening for prevention and early diagnosis of heritable diseases. J. Genet. Counsel. 2015, 24, 388–399. [Google Scholar] [CrossRef]
- Tiller, J.; Trainer, A.H.; Campbell, I.; Lacaze, P.A. Ethical and practical implications of returning genetic research results: Two Australian case studies. Med. J. Aust. 2021, 214, 259–262.e1. [Google Scholar] [CrossRef]
- Newson, A.J.; Humphries, S.E. Cascade testing in familial hypercholesterolaemia: How should family members be contacted? Eur. J. Hum. Genet. 2005, 13, 401–408. [Google Scholar] [CrossRef]

| Jurisdiction | Act | Privacy Principles |
|---|---|---|
| Commonwealth (CTH) | Privacy Act 1988 (Cth) | Schedule 1—Australian Privacy Principles (APP) |
| Australian Capital Territory (ACT) | Information Privacy Act 2014 (ACT) | Schedule 1—Territory Privacy Principles (TPP) |
| Health Records (Privacy and Access) Act 1997 (ACT) | Schedule 1—Privacy Principles (PP) | |
| New South Wales (NSW) | Privacy and Personal Information Protection Act 1998 (NSW) (PRIPA) | N/A—applicable sections listed |
| Health Records and Information Privacy Act 2002 (NSW) | Schedule 1—Health Privacy Principles (HPP) | |
| Northern Territory (NT) | Information Act 2002 (NT) | Schedule 2—Information Privacy Principles (IPP) |
| Queensland (QLD) | Information Privacy Act 2009 (QLD) | Schedule 3—Information Privacy Principles (IPP) and |
| Schedule 4—National Privacy Principles (IPP) | ||
| South Australia (SA) | Premier and Cabinet Circular PC 012—Information Privacy Principles (IPPs) Instruction (2020) | Part II—Information Privacy Principles (IPP) |
| Tasmania (TAS) | Personal Information Protection Act 2004 (TAS) | Schedule 1—Personal Information Protection Principles (PIPP) |
| Victoria (VIC) | Health Records Act 2001 (VIC) | Schedule 1—Health Privacy Principles (HPP) |
| Privacy and Data Collection Act 2014 (VIC) | Schedule 1—Information Privacy Principles (IPP) | |
| Western Australia (WA) | Health Services Act 2016 (WA) | N/A—applicable sections listed |
| Health Services (Information) Regulations 2017 (WA) | N/A—applicable sections listed |
| CTH Privacy Act | Clause | Application to Contact of At-Risk Relatives with Patient Consent | Principles in State/Territory Regulations Applicable to Collection, Use or Disclosure of Contact Information | Additional State/Territory Principles Applicable to Collection, Use or Disclosure of Health Information | Notes |
|---|---|---|---|---|---|
| APP 3: Collection of solicited personal information | 3.2: Entity must not collect personal information (other than sensitive information) unless the information is reasonably necessary for one or more of the entity’s functions or activities. | Facilitating risk notification and cascade testing of relatives is one of the core functions of a clinical genetics service | ACT: TPP 3.1 NSW: PRIPA s8 NT: IPP 1.1 QLD: IPP1; NPP 1 VIC: IPP1.1 SA: IPP 4(1) TAS: PIPP 1 | ||
| 3.3: Entity must not collect sensitive information about an individual unless the individual consents to the collection of the information and the information is reasonably necessary for one or more of the entity’s functions or activities. | Personal contact details are not sensitive information, thus it is not necessary that relatives’ consent be obtained before the information is collected | VIC: IPP 10 ACT: TPP 3.3; PP 1 NSW: HPP 1 NT: IPP 10 TAS: PIPP 10 | |||
| 3.5: An APP entity must collect personal information only by lawful and fair means. | Collecting contact details of relatives directly from patients, with their consent, for the purpose of providing them with information about their genetic risk, is lawful and fair | VIC: IPP1.2 ACT: TPP 3.5 NSW: PRIPA s8 NT: IPP 1.2 QLD: IPP1 and NPP 1 SA: IPP 4(1) TAS: PIPP 1 | VIC: HPP 1.2 NSW: HPP 1 | ||
| 3.6: An APP entity must collect personal information about an individual only from the individual unless it is unreasonable or impracticable to do so. | Given the purpose is to facilitate risk notification of relatives with whom the service has no contact, it is impracticable to collect contact details directly from those relatives | VIC: IPP 1.4 ACT: TPP 3.6 NSW: PRIPA s9 (and s26) NT: IPP 1.4 QLD: NPP 1 TAS: PIPP 1 | VIC: HPP 1.2 NSW: HPP 1 | NSW: PRIP s9 does not allow for exception to the requirement that personal information must be collected from the individual unless unreasonable or impracticable. However, s26(1) allows for an exemption where compliance would prejudice the interests of the individual to whom the information relates. Clearly, at-risk relatives’ interests will be prejudiced if they cannot be notified of their medically actionable genomic risk. WA: Collection, use or disclosure of personal information is authorised if done with the consent of the person to whom it relates (HSA s220(1)(a)). However, under HSIR s5(1)(a), collection, use or disclosure is authorised if reasonably necessary to lessen or prevent a serious risk to the life, health or safety of an individual. | |
| APP 5: Notification of the collection of personal information | 5.1 and 5.2: As soon as practicable after collecting personal information about an individual, the entity must take reasonable steps to notify the individual of the circumstances of the collection, the entity’s identity and contact details, the purpose of the collection and any consequences of not collecting the information, details of the entity’s privacy policy, mechanisms to correct information and avenues for complaints about breach of privacy, and any other bodies to which the information may be disclosed | These considerations should inform the content of the letter (or other form of communication) sent to relatives, but do not prevent the collection and use of the contact details for this purpose | VIC: IPP 1.3 and 1.5 ACT: TPP 5 NSW: PRIPA s10 NT: IPP 1.3 and 1.5 QLD: NPP 1 SA: IPP 4(2) TAS: PIPP 1 | ACT: PP 2 VIC: HPP 1.4 and 1.5 NSW: HPP 4 | VIC: HPP 1.7 requires that reasonable steps are taken to ensure that health information remains confidential where it is received from a recipient who is not the individual that the health information is about (for general obligations to take reasonable steps to protect personal information, see APP 11.1, VIC IPP 4.1/HPP 4.1; ACT TPP 11/PP 4.1; NSW HPP 5/PRIPA s12; NT IPP 4.1; QLD IPP 4/NPP 4; SA IPP 4(4); TAS PIPP 4). |
| APP 6: Use or disclosure of personal information | 6.1: Personal information about an individual collected for a particular purpose (the primary purpose), must not be used or disclosed for another purpose (the secondary purpose) unless the individual consents or an exception applies | Contact details can only be used to contact relatives to notify them of their possible genetic risk and options for testing, not for any other purpose (without their subsequent consent) | VIC: IPP 2 ACT: TPP 6 NSW: PRIPA s17 NT: IPP 2.1 VIC: IPP10 QLD: NPP 2 SA: IPP 4(8) and IPP 4(10) TAS: PIPP 2 | VIC: HPP 2 ACT: PP 9 and PP 10 NSW: HPP 1 | VIC: IPP 1 applies to the use or disclosure of contact information (personal information that is not health information) VIC: IPP2 and HPP 2 applies to the use or disclosure of the health information. TAS: PIPP 9 has special provisions regarding the disclosure of personal information about an individual to an entity outside of Tasmania. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiller, J.; Nowak, K.; Boughtwood, T.; Otlowski, M. Privacy Implications of Contacting the At-Risk Relatives of Patients with Medically Actionable Genetic Predisposition, with Patient Consent: A Hypothetical Australian Case Study. BioTech 2023, 12, 45. https://doi.org/10.3390/biotech12020045
Tiller J, Nowak K, Boughtwood T, Otlowski M. Privacy Implications of Contacting the At-Risk Relatives of Patients with Medically Actionable Genetic Predisposition, with Patient Consent: A Hypothetical Australian Case Study. BioTech. 2023; 12(2):45. https://doi.org/10.3390/biotech12020045
Chicago/Turabian StyleTiller, Jane, Kristen Nowak, Tiffany Boughtwood, and Margaret Otlowski. 2023. "Privacy Implications of Contacting the At-Risk Relatives of Patients with Medically Actionable Genetic Predisposition, with Patient Consent: A Hypothetical Australian Case Study" BioTech 12, no. 2: 45. https://doi.org/10.3390/biotech12020045
APA StyleTiller, J., Nowak, K., Boughtwood, T., & Otlowski, M. (2023). Privacy Implications of Contacting the At-Risk Relatives of Patients with Medically Actionable Genetic Predisposition, with Patient Consent: A Hypothetical Australian Case Study. BioTech, 12(2), 45. https://doi.org/10.3390/biotech12020045







