A Case of Atypical Klippel-Trenaunay Syndrome
Abstract
:1. Introduction
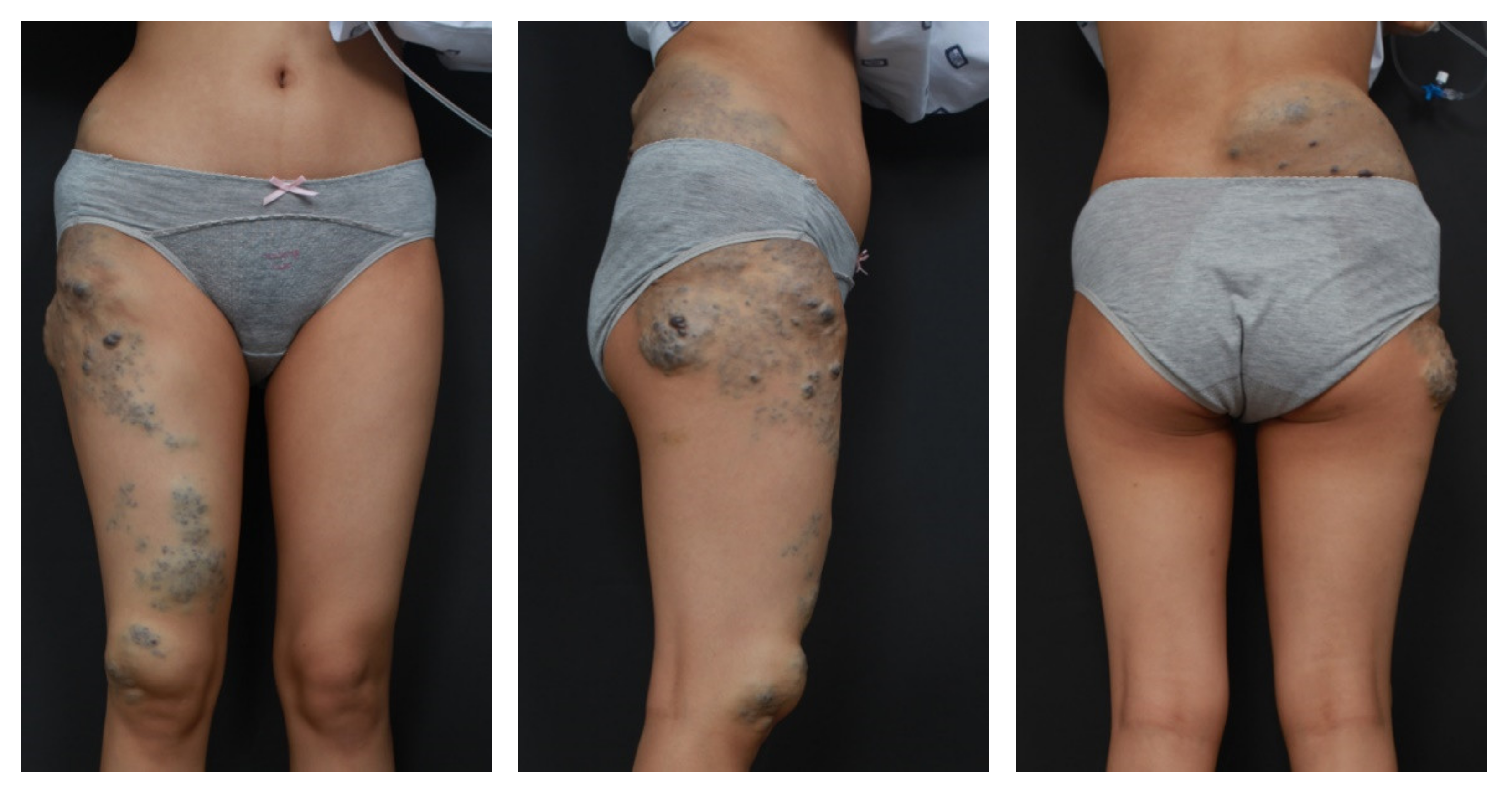
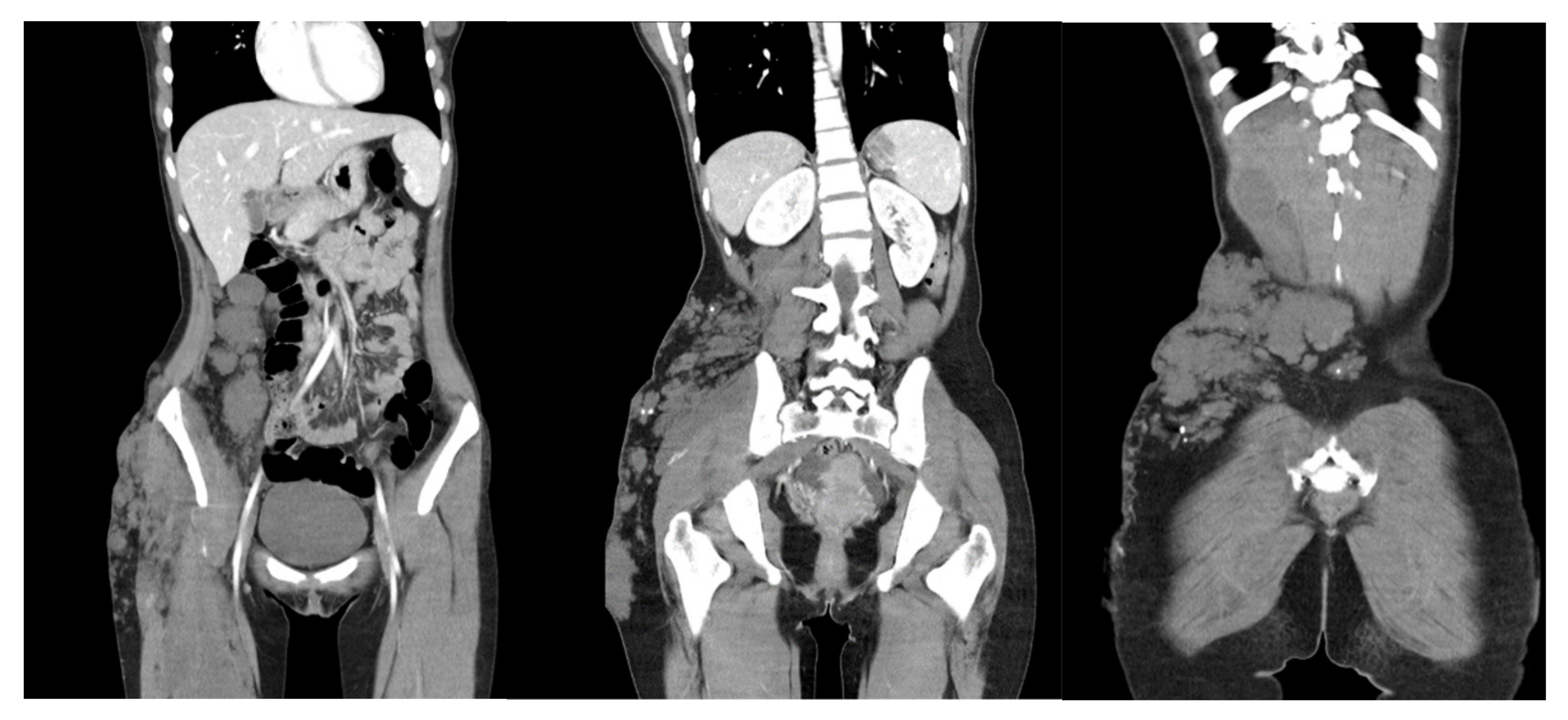
2. Case
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Redondo, P.; Aguado, L.; Martínez-Cuesta, A. Diagnosis and management of extensive vascular malformations of the lower limb: Part I. Clinical diagnosis. J. Am. Acad. Dermatol. 2011, 65, 893–908. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.G.; Driscoll, D.J.; Shaughnessy, W.J.; Stanson, A.W.; Clay, R.P.; Gloviczki, P. Klippel-Trénaunay syndrome: Spectrum and management. Mayo Clin. Proc. 1998, 73, 28–36. [Google Scholar] [CrossRef]
- Klippel, M.; Trenaunay, P. Du noevus variqueux osteohypertrophiques. Arch. Gen. Med. 1900, 3, 641–672. [Google Scholar]
- Craven, N.; Wright, A.L. Familial Klippel-Trenaunay syndrome: A case report. Clin. Exp. Dermatol. 1995, 20, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Asghar, F.; Aqeel, R.; Farooque, U.; Haq, A.; Taimur, M. Presentation and Management of Klippel-Trenaunay Syndrome: A Review of Available Data. Cureus 2020, 12, e8023. [Google Scholar] [CrossRef] [PubMed]
- Schoch, J.J.; Nguyen, H.; Schoch, B.S.; Anderson, K.R.; Stans, A.A.; Driscoll, D.; Tollefson, M. Orthopaedic diagnoses in patients with Klippel-Trenaunay syndrome. J. Child. Orthop. 2019, 13, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Hammer, J.; Seront, E.; Duez, S.; Dupont, S.; Van Damme, A.; Schmitz, S.; Hoyoux, C.; Chopinet, C.; Clapuyt, P.; Hammer, F.; et al. Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: A monocentric prospective phase II study. Orphanet J. Rare Dis. 2018, 13, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, P.R. Klippel-Trenaunay Syndrome. Tech. Vasc. Interv. Radiol. 2019, 22, 100634. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, Y.; Lee, S.-H.; Cho, M.; Cho, S.-H.; Lee, J.-D.; Woo, Y.-R.; Kim, H.-S. A Case of Atypical Klippel-Trenaunay Syndrome. Dermato 2021, 1, 43-46. https://doi.org/10.3390/dermato1020007
Han Y, Lee S-H, Cho M, Cho S-H, Lee J-D, Woo Y-R, Kim H-S. A Case of Atypical Klippel-Trenaunay Syndrome. Dermato. 2021; 1(2):43-46. https://doi.org/10.3390/dermato1020007
Chicago/Turabian StyleHan, Yujin, Se-Hoon Lee, Minah Cho, Sang-Hyun Cho, Jeong-Deuk Lee, Yu-Ri Woo, and Hei-Sung Kim. 2021. "A Case of Atypical Klippel-Trenaunay Syndrome" Dermato 1, no. 2: 43-46. https://doi.org/10.3390/dermato1020007
APA StyleHan, Y., Lee, S.-H., Cho, M., Cho, S.-H., Lee, J.-D., Woo, Y.-R., & Kim, H.-S. (2021). A Case of Atypical Klippel-Trenaunay Syndrome. Dermato, 1(2), 43-46. https://doi.org/10.3390/dermato1020007






