Quality-of-Life Comparison of Three Different Breath-Hold Techniques for Left-Sided Breast Radiation †
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Breath-Hold Techniques
2.3. QOL Tools
2.4. Statistical Analysis
3. Results
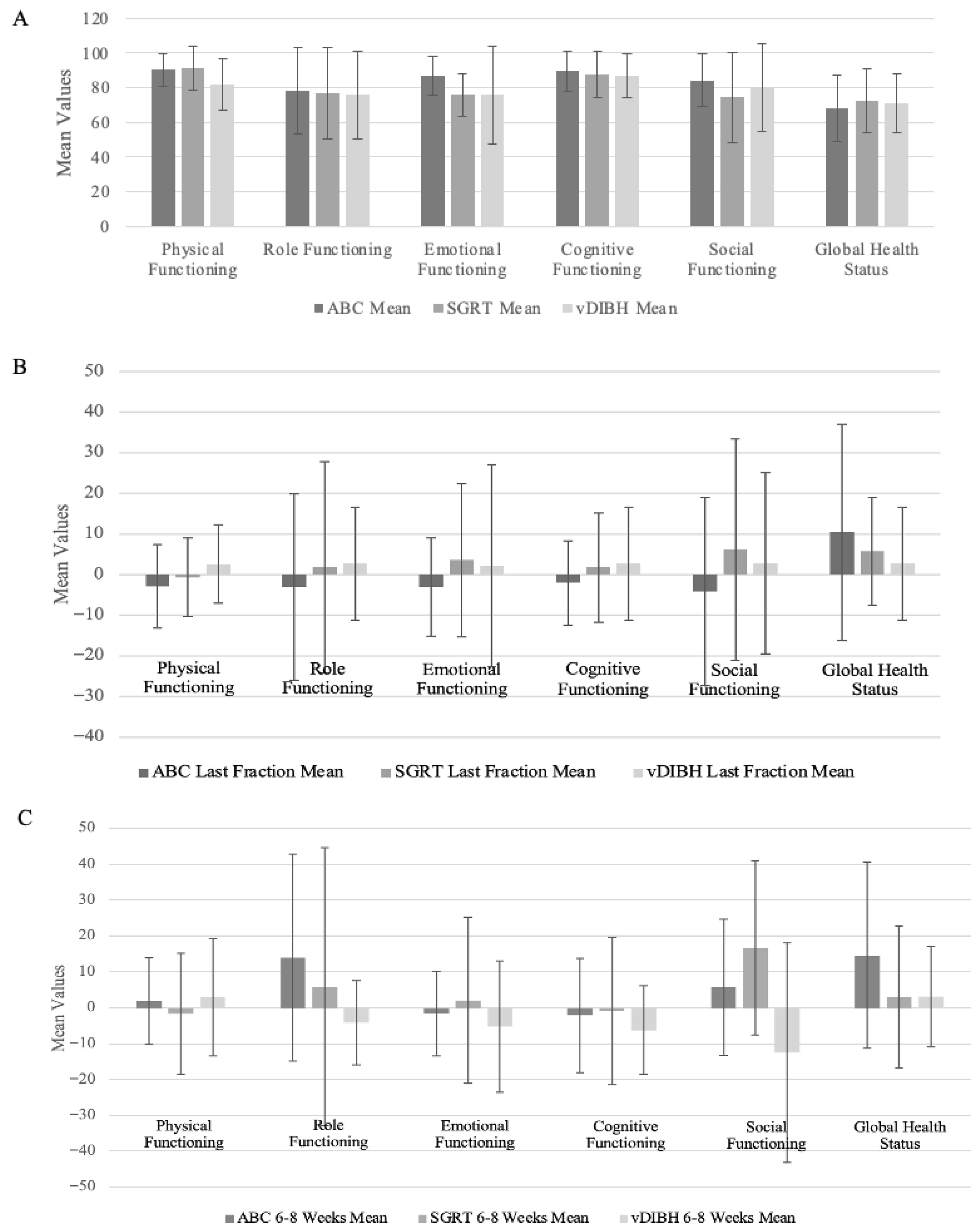
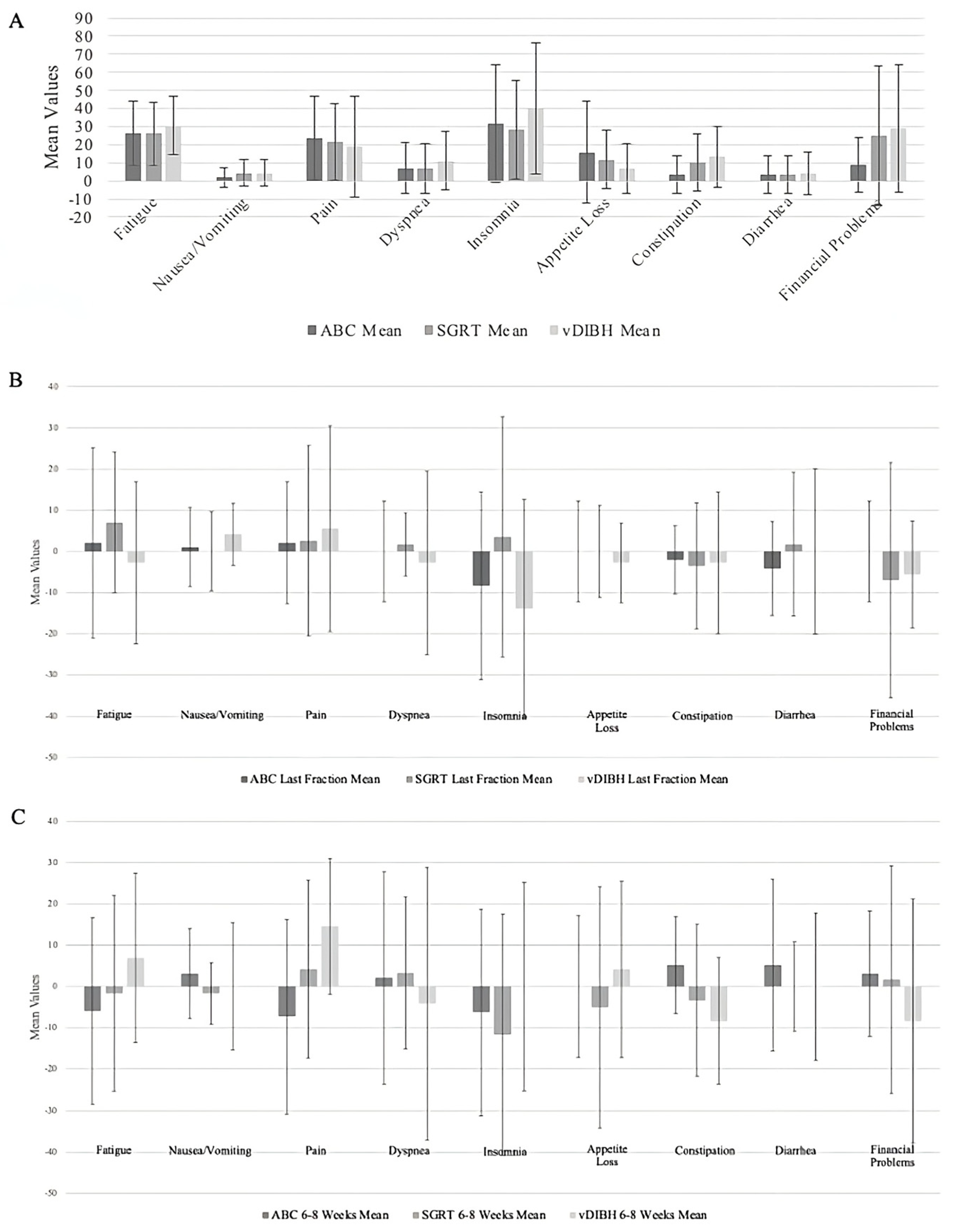
3.1. Descriptive Analysis of EORTC QLQ-C30 Scales
3.2. Comparison of the Breath-Hold Techniques at Last Fraction Compared to Baseline
3.3. Comparison of the Breath-Hold Techniques at 6–8 Weeks Follow-Up Compared to Baseline
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- EBCTCG (Early Breast Cancer Trialists’ Collaborative Group); McGale, P.; Taylor, C.; Correa, C.; Cutter, D.; Duane, F.; Ewertz, M.; Gray, R.; Mannu, G.; Peto, R.; et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: Meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 2014, 383, 2127–2135. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005, 366, 2087–2106. [Google Scholar] [CrossRef]
- Darby, S.C.; McGale, P.; Taylor, C.W.; Peto, R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005, 6, 557–565. [Google Scholar] [CrossRef]
- Smyth, L.M.; Knight, K.A.; Aarons, Y.K.; Wasiak, J. The cardiac dose-sparing benefits of deep inspiration breath-hold in left breast irradiation: A systematic review. J. Med. Radiat. Sci. 2015, 62, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Aznar, M.C.; Carrasco de Fez, P.; Corradini, S.; Mast, M.; McNair, H.; Meattini, I.; Persson, G.; van Haaren, P. ESTRO-ACROP guideline: Recommendations on implementation of breath-hold techniques in radiotherapy. Radiother. Oncol. 2023, 185, 109734. [Google Scholar] [CrossRef]
- Remouchamps, V.M.; Vicini, F.A.; Sharpe, M.B.; Kestin, L.L.; Martinez, A.A.; Wong, J.W. Significant reductions in heart and lung doses using deep inspiration breath hold with active breathing control and intensity-modulated radiation therapy for patients treated with locoregional breast irradiation. Int. J. Radiat. Oncol. 2003, 55, 392–406. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, F.R.; Donovan, E.M.; McNair, H.A.; Corsini, L.A.; Colgan, R.M.; Evans, P.M.; Maynard, L.; Griffin, C.; Haviland, J.S.; Yarnold, J.R.; et al. The UK HeartSpare Study (Stage II): Multicentre Evaluation of a Voluntary Breath-Hold Technique in Patients Receiving Breast Radiotherapy. Clin. Oncol. 2017, 29, e51–e56. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, F.R.; Colgan, R.M.; Carr, K.; Donovan, E.M.; McNair, H.A.; Locke, I.; Evans, P.M.; Haviland, J.S.; Yarnold, J.R.; Kirby, A.M. The UK HeartSpare Study: Randomised evaluation of voluntary deep-inspiratory breath-hold in women undergoing breast radiotherapy. Radiother. Oncol. 2013, 108, 242–247. [Google Scholar] [CrossRef]
- Naidoo, W.; Leech, M. Feasibility of surface guided radiotherapy for patient positioning in breast radiotherapy versus conventional tattoo-based setups- a systematic review. Tech. Innov. Patient Support Radiat. Oncol. 2022, 22, 39–49. [Google Scholar] [CrossRef]
- Zagar, T.M.; Kaidar-Person, O.; Tang, X.; Jones, E.E.; Matney, J.; Das, S.K.; Green, R.L.; Sheikh, A.; Khandani, A.H.; McCartney, W.H.; et al. Utility of Deep Inspiration Breath Hold for Left-Sided Breast Radiation Therapy in Preventing Early Cardiac Perfusion Defects: A Prospective Study. Int. J. Radiat. Oncol. 2017, 97, 903–909. [Google Scholar] [CrossRef]
- Cashell, A.; Qadeer, J.; Rosewall, T. Exploring the Experiences of Left-Sided Breast Cancer Patients Receiving Radiation Therapy Using the Active Breathing Coordinator. J. Med. Imaging Radiat. Sci. 2016, 47, 323–328. [Google Scholar] [CrossRef]
- Beaton, N.; Watson, S.; Browne, P.; Sharma, H.; Mai, G.T.; Harvey, J.; Bernard, A.; Brown, E.; Hargrave, C.; Lehman, M. Deep inspiration breath hold in breast cancer: Development and analysis of a patient experience questionnaire. J. Med. Imaging Radiat. Oncol. 2018, 62, 854–860. [Google Scholar] [CrossRef]
- Dower, K.; Halkett, G.K.B.; Dhillon, H.; Naehrig, D.; O’Connor, M. Eliciting the views of left breast cancer patients’ receiving deep inspiration breath hold radiation therapy to inform the design of multimedia education and improve patient-centred care for prospective patients. J. Med. Radiat. Sci. 2024, 71, 384–395. [Google Scholar] [CrossRef]
- Chan, A.W.; Hoang, A.; Chen, H.; McGuffin, M.; Sheikh, A.; Vesprini, D.; Zhang, L.; Wronski, M.; Karam, I. Comparing Interfractional Stability of Heart Dose Among Three Breath-Hold Radiotherapy Techniques in Breast Cancer. Clin. Oncol. 2025, 38, 103699. [Google Scholar] [CrossRef]
- Chan, A.W.; Hoang, A.; Chen, H.; McGuffin, M.; Vesprini, D.; Zhang, L.; Wronski, M.; Karam, I. Prospective Trial on the Impact of Weekly Cone Beam Computed Tomography-Guided Correction on Mean Heart Dose in Breast Cancer Breath-Hold Radiation Therapy. Adv. Radiat. Oncol. 2024, 9, 101651. [Google Scholar] [CrossRef]
- Karam, D.I. Assessment of Left-Sided Cardiac Sparing Through the Use of 3-Dimensional Surface Matching-Based Deep Inspiration Breath Hold and Active Breathing Control. Clinicaltrials.Gov. 2022. Available online: https://clinicaltrials.gov/study/NCT03459898 (accessed on 3 December 2024).
- Osoba, D.; Aaronson, N.; Zee, B.; Sprangers, M.; Te Velde, A. Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. The Study Group on Quality of Life of the EORTC and the Symptom Control and Quality of Life Committees of the NCI of Canada Clinical Trials Group. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 1997, 6, 103–108. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Freislederer, P.; Kügele, M.; Öllers, M.; Swinnen, A.; Sauer, T.-O.; Bert, C.; Giantsoudi, D.; Corradini, S.; Batista, V. Recent Advances in Surface Guided Radiation Therapy. Radiat. Oncol. 2020, 15, 187. [Google Scholar] [CrossRef] [PubMed]
- Andersen, K.G.; Kehlet, H. Persistent Pain After Breast Cancer Treatment: A Critical Review of Risk Factors and Strategies for Prevention. J. Pain. 2011, 12, 725–746. [Google Scholar] [CrossRef]
- Mosconi, P.; Apolone, G.; Barni, S.; Secondino, S.; Sbanotto, A.; Filiberti, A. Quality of Life in Breast and Colon Cancer Long-term Survivors: An Assessment with the Eortc Qlq-c30 and Sf-36 Questionnaires. Tumori J. 2002, 88, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Nolte, S.; Liegl, G.; Petersen, M.A.; Aaronson, N.K.; Costantini, A.; Fayers, P.M.; Groenvold, M.; Holzner, B.; Johnson, C.D.; Kemmler, G.; et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur. J. Cancer. 2019, 107, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Bjelic-Radisic, V.; Cardoso, F.; Weis, J.; Pogoda, K.; Arraras, J.I.; Greimel, E.; Bottomley, A.; Cameron, D.; Brain, E.; Hartup, S.; et al. An international phase IV field study—Psychometric properties of the updated module on assessing quality of life of patients with breast cancer EORTC QLQ-BR42. Breast 2025, 80, 103890. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Category | ABC (n = 19), % | SGRT (n = 20), % | vDIBH (n = 16), % |
|---|---|---|---|---|
| Age, y | Mean (IQR) | 56.6 (47.5–62.5) | 53.7 (44.3–64.2) | 54.6 (47–65) |
| Surgery | Breast-conserving surgery | 78.9 | 60 | 93.7 |
| Mastectomy | 21.1 | 40 | 6.2 | |
| Dose fractionation | 50 Gy/25 fr | 15.8 | 15 | 6.3 |
| 42.56 Gy/16 fr | 84.2 | 85 | 75 | |
| 40.05 Gy/15 fr | 0 | 0 | 18.8 | |
| Field arrangement | 2 field | 47.3 | 35 | 68.8 |
| 3 or 4 field | 52.6 | 65 | 31.2 |
| Last Fraction | 6–8 Weeks Follow-Up | |||||
|---|---|---|---|---|---|---|
| EORTC QLQ C30 Changed Scales from Baseline | ABC vs. vDIBH (p-Value) | SGRT vs. vDIBH (p-Value) | SGRT vs. ABC (p-Value) | ABC vs. vDIBH (p-Value) | SGRT vs. vDIBH (p-Value) | SGRT vs. ABC (p-Value) |
| Physical Functioning | 0.1443 | 0.3633 | 0.5121 | 0.8646 | 0.4528 | 0.4917 |
| Role Functioning | 0.4949 | 0.9022 | 0.5253 | 0.1953 | 0.4590 | 0.4473 |
| Emotional Functioning | 0.4707 | 0.8376 | 0.3027 | 0.6577 | 0.3609 | 0.5676 |
| Cognitive Functioning | 0.3184 | 0.8269 | 0.3748 | 0.5910 | 0.4702 | 0.8349 |
| Social Functioning | 0.4665 | 0.7144 | 0.2264 | 0.0830 | 0.0053 * | 0.1762 |
| Global Health Status | 0.2993 | 0.6791 | 0.4694 | 0.2242 | 0.9816 | 0.1124 |
| Fatigue | 0.5257 | 0.1887 | 0.4688 | 0.1998 | 0.3712 | 0.5821 |
| Nausea/Vomiting | 0.3747 | 0.2221 | 0.7381 | 0.4953 | 0.7060 | 0.1806 |
| Pain | 0.6696 | 0.7097 | 0.9395 | 0.0240 * | 0.2546 | 0.1206 |
| Dyspnea | 0.6083 | 0.3878 | 0.7154 | 0.5542 | 0.4630 | 0.8784 |
| Insomnia | 0.5851 | 0.0814 | 0.1938 | 0.5964 | 0.3085 | 0.5537 |
| Appetite Loss | 0.5173 | 0.5025 | 1.0000 | 0.6917 | 0.3685 | 0.5396 |
| Constipation | 0.8965 | 0.8872 | 0.7638 | 0.0539 | 0.4524 | 0.1137 |
| Diarrhea | 0.5103 | 0.7736 | 0.2942 | 0.4660 | 0.9999 | 0.3477 |
| Financial Problems | 0.4840 | 0.8483 | 0.3212 | 0.2800 | 0.3285 | 0.8581 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hircock, C.; Chan, A.W.; Hoang, A.; Chen, H.; McGuffin, M.; Vesprini, D.; Zhang, L.; Wronski, M.; Karam, I. Quality-of-Life Comparison of Three Different Breath-Hold Techniques for Left-Sided Breast Radiation. Radiation 2025, 5, 38. https://doi.org/10.3390/radiation5040038
Hircock C, Chan AW, Hoang A, Chen H, McGuffin M, Vesprini D, Zhang L, Wronski M, Karam I. Quality-of-Life Comparison of Three Different Breath-Hold Techniques for Left-Sided Breast Radiation. Radiation. 2025; 5(4):38. https://doi.org/10.3390/radiation5040038
Chicago/Turabian StyleHircock, Caroline, Adrian Wai Chan, Anh Hoang, Hanbo Chen, Merrylee McGuffin, Danny Vesprini, Liying Zhang, Matt Wronski, and Irene Karam. 2025. "Quality-of-Life Comparison of Three Different Breath-Hold Techniques for Left-Sided Breast Radiation" Radiation 5, no. 4: 38. https://doi.org/10.3390/radiation5040038
APA StyleHircock, C., Chan, A. W., Hoang, A., Chen, H., McGuffin, M., Vesprini, D., Zhang, L., Wronski, M., & Karam, I. (2025). Quality-of-Life Comparison of Three Different Breath-Hold Techniques for Left-Sided Breast Radiation. Radiation, 5(4), 38. https://doi.org/10.3390/radiation5040038






