Treatment Outcomes of External Beam Radiation Therapy for Unresectable Locally Advanced Thyroid Cancer with or without Metastasis: A Retrospective Single-Center Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Patients
2.3. Evaluation
2.4. Radiation Therapy
3. Results
3.1. Patient Characteristics
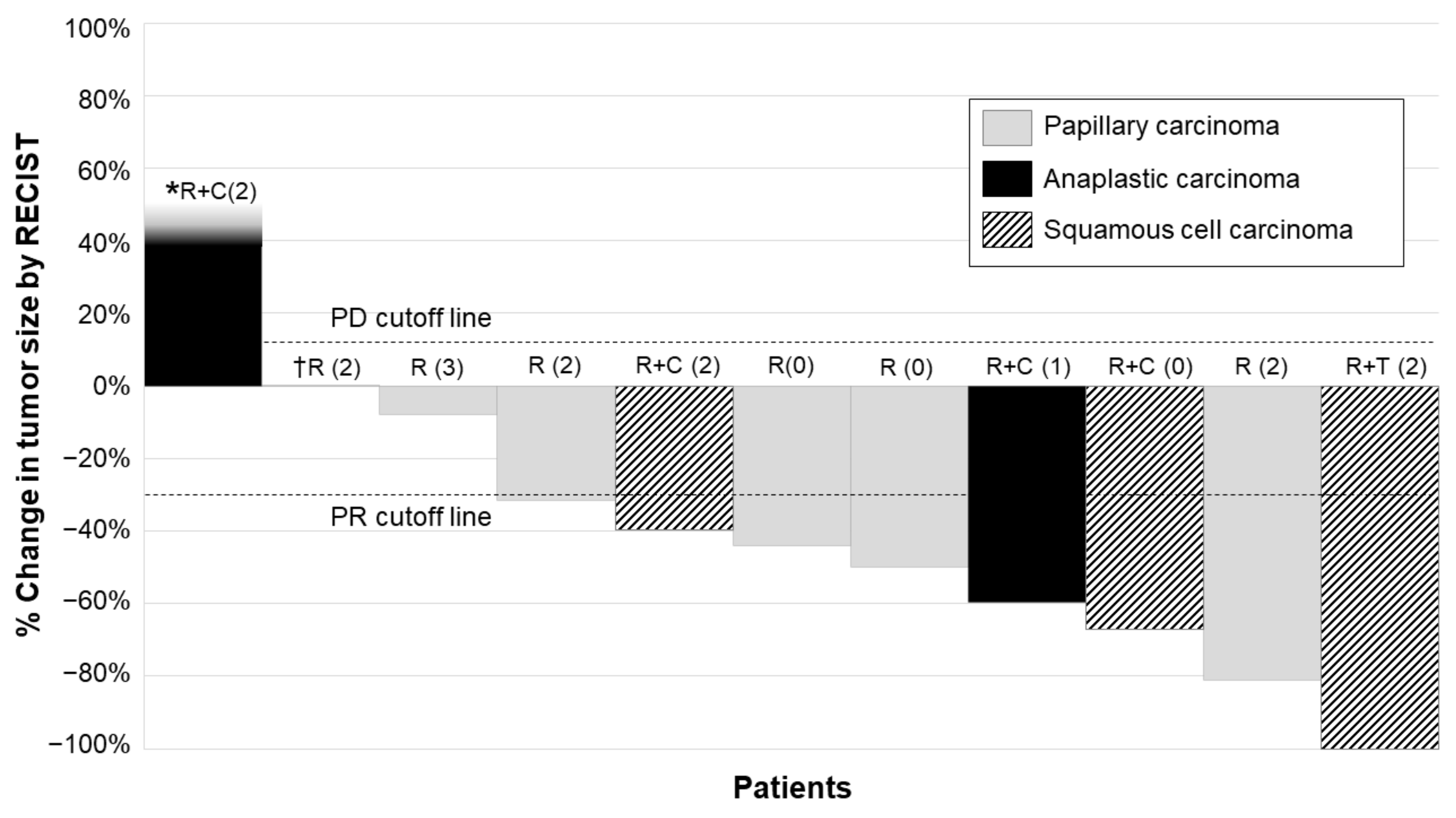
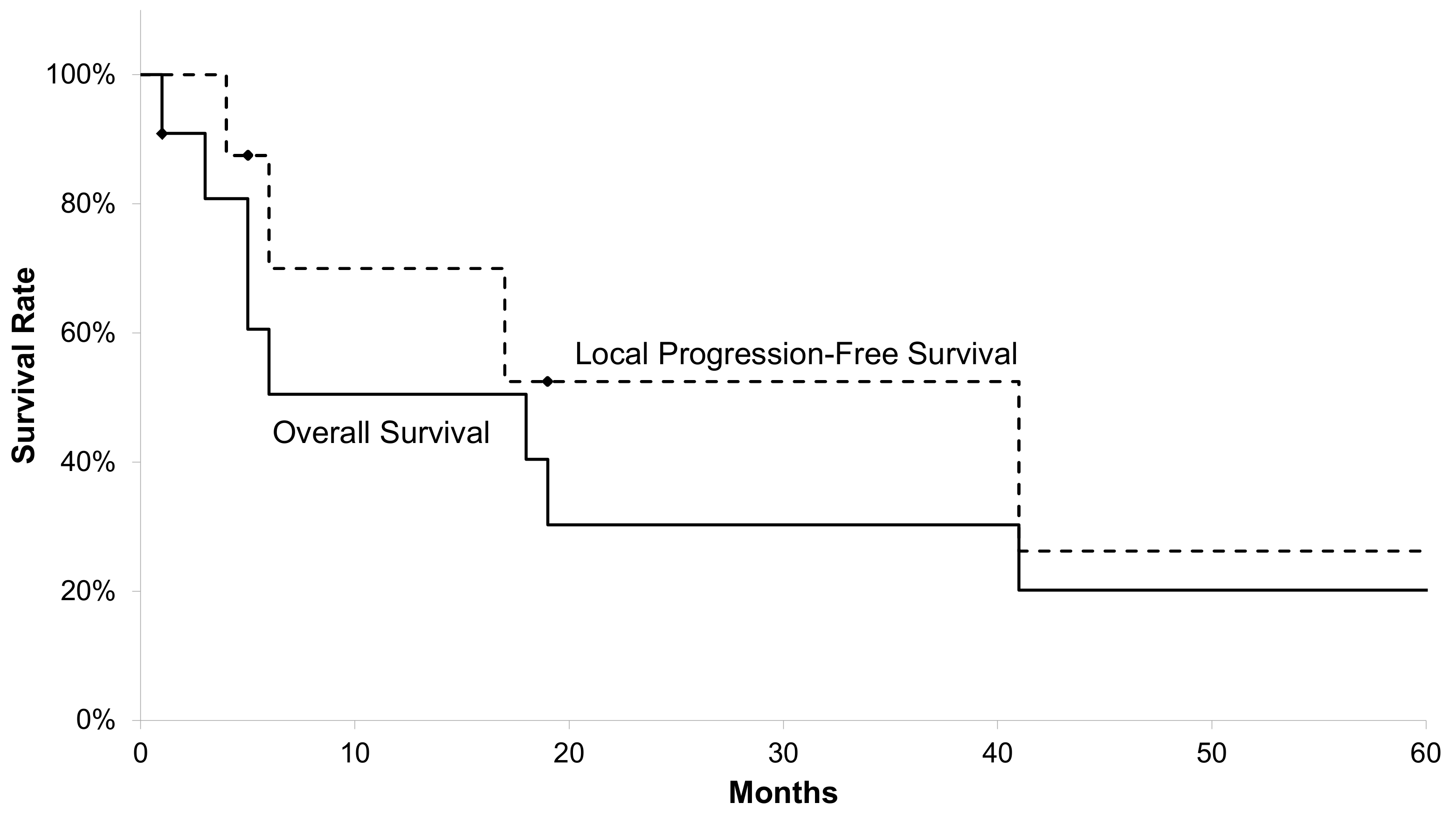
3.2. Treatment Outcomes
3.3. Toxicities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Filetti, S.; Durante, C.; Hartl, D.; Leboulleux, S.; Locati, L.D.; Newbold, K.; Papotti, M.G.; Berruti, A. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1856–1883. [Google Scholar] [CrossRef] [Green Version]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, Y.; Onoda, N.; Okamoto, T. The revised clinical practice guidelines on the management of thyroid tumors by the japan associations of endocrine surgeons: Core questions and recommendations for treatments of thyroid cancer. Endocr. J. 2020, 67, 669–717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlumberger, M.; Tahara, M.; Wirth, L.J.; Robinson, B.; Brose, M.S.; Elisei, R.; Habra, M.A.; Newbold, K.; Shah, M.H.; Hoff, A.O.; et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N. Engl. J. Med. 2015, 372, 621–630. [Google Scholar] [CrossRef] [Green Version]
- Brose, M.S.; Nutting, C.M.; Jarzab, B.; Elisei, R.; Siena, S.; Bastholt, L.; De La Fouchardiere, C.; Pacini, F.; Paschke, R.; Shong, Y.K.; et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic diff erentiated thyroid cancer: A randomised, double-blind, phase 3 trial. Lancet 2014, 384, 319–328. [Google Scholar] [CrossRef] [Green Version]
- Wells, S.A.; Robinson, B.G.; Gagel, R.F.; Dralle, H.; Fagin, J.A.; Santoro, M.; Baudin, E.; Elisei, R.; Jarzab, B.; Vasselli, J.R.; et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: A randomized, double-blind phase III trial. J. Clin. Oncol. 2012, 30, 134–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obata, K.; Sugitani, I.; Ebina, A.; Sugiura, Y.; Toda, K.; Takahashi, S.; Kawabata, K. Common carotid artery rupture during treatment with lenvatinib for anaplastic thyroid cancer. Int. Cancer Conf. J. 2016, 5, 197–201. [Google Scholar] [CrossRef]
- Staub, Y.; Nishiyama, A.; Suga, Y.; Fujita, M.; Matsushita, R.; Yano, S. Clinical characteristics associated with lenvatinib-induced fistula and tumor-related bleeding in patients with thyroid cancer. Anticancer Res. 2019, 39, 3871–3878. [Google Scholar] [CrossRef]
- Meadows, K.M.; Amdur, R.J.; Morris, C.G.; Villaret, D.B.; Mazzaferri, E.L.; Mendenhall, W.M. External beam radiotherapy for differentiated thyroid cancer. Am. J. Otolaryngol. Head Neck Med. Surg. 2006, 27, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.L.; Lobo, M.J.; Ang, K.K.; Morrison, W.H.; Rosenthal, D.I.; Ahamad, A.; Evans, D.B.; Clayman, G.; Sherman, S.I.; Garden, A.S. Postoperative external beam radiotherapy for differentiated thyroid cancer: Outcomes and morbidity with conformal treatment. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 1083–1091. [Google Scholar] [CrossRef] [Green Version]
- Pierie, J.P.E.N.; Muzikansky, A.; Gaz, R.D.; Faquin, W.C.; Ott, M.J. The effect of surgery and radiotherapy on outcome of anaplastic thyroid carcinoma. Ann. Surg. Oncol. 2002, 9, 57–64. [Google Scholar] [CrossRef]
- Rosenbluth, B.D.; Serrano, V.; Happersett, L.; Shaha, A.R.; Tuttle, R.M.; Narayana, A.; Wolden, S.L.; Rosenzweig, K.E.; Chong, L.M.; Lee, N.Y. Intensity-modulated radiation therapy for the treatment of nonanaplastic thyroid cancer. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 1419–1426. [Google Scholar] [CrossRef]
- Terezakis, S.A.; Lee, K.S.; Ghossein, R.A.; Rivera, M.; Tuttle, R.M.; Wolden, S.L.; Zelefsky, M.J.; Wong, R.J.; Patel, S.G.; Pfister, D.G. Role of external beam radiotherapy in patients with advanced or recurrent nonanaplastic thyroid cancer: Memorial Sloan-Kettering Cancer Center experience. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 795–801. [Google Scholar] [CrossRef]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; Blackwell Publishing: Hoboken, NJ, USA, 2017. [Google Scholar]
- Edward, C.H. Liner-Quadratic Equation. In Perez & Brady’s Principles and Practice of Radiation Oncology, 7th ed.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018; pp. 27–30. [Google Scholar]
- Bertok, L.; Nagy, S.U. Effect of irradiation on serum T4 level and response of thyroid gland to exogenous TSH in rats. J. Radiat. Res. 1986, 27, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, Y. Radiation-related thyroid autoimmunity and dysfunction. J. Radiat. Res. 2018, 59, ii98–ii107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, B.; Schlumberger, M.; Wirth, L.J.; Dutcus, C.E.; Song, J.; Taylor, M.H.; Kim, S.B.; Krzyzanowska, M.K.; Capdevila, J.; Sherman, S.I. Characterization of tumor size changes over time from the phase 3 study of lenvatinib in thyroid cancer. J. Clin. Endocrinol. Metab. 2016, 101, 4103–4139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, K.; Iwai, H.; Utsunomiya, K.; Kono, Y.; Kobayashi, Y.; Van Bui, D.; Sawada, S.; Yun, Y.; Mitani, A.; Kondo, N.; et al. Combination therapy with lenvatinib and radiation significantly inhibits thyroid cancer growth by uptake of tyrosine kinase inhibitor. Exp. Cell Res. 2021, 398, 112390. [Google Scholar] [CrossRef]
- Wada, Y. A case of unresectable squamous cell carcinoma of thyroid gland which could be local controlled by lenvatinib combined with radiotherapy. Jpn. J. Clin. Radiol. 2016, 61, 953–958. [Google Scholar]
- Yamazaki, T. Combined use of lenvatinib and external irradiation for undifferentiated thyroid cancer in aged patients with multiple comorbidities: A case study. J. Jpn. Thyroid Assoc. 2018, 9, 69–73. [Google Scholar] [CrossRef]
- Shimo, T.; Yoshidome, K.; Yasuno, K.; Tori, M. Three cases of recurrent thyroid cancer involving the perforation of adjacent structures caused by lenvatinib after external radiation therapy. J. Jpn. Surg. Assoc. 2018, 79, 283–288. [Google Scholar] [CrossRef]
- Hirose, K.; Konno, A.; Hiratsuka, J.; Yoshimoto, S.; Kato, T.; Ono, K.; Otsuki, N.; Hatazawa, J.; Tanaka, H.; Takayama, K.; et al. Boron neutron capture therapy using cyclotron-based epithermal neutron source and borofalan (10B) for recurrent or locally advanced head and neck cancer (JHN002): An open-label phase II trial. Radiother. Oncol. 2021, 155, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Turrisi, A.T., 3rd; Kim, K.; Blum, R.; Sause, W.T.; Livingston, R.B.; Komaki, R.; Wagner, H.; Aisner, S.; Johnson, D.H. Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. N. Engl. J. Med. 1999, 340, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Dandekar, P.; Harmer, C.; Barbachano, Y.; Rhys-Evans, P.; Harrington, K.; Nutting, C.; Newbold, K. Hyperfractionated Accelerated Radiotherapy (HART) for anaplastic thyroid carcinoma: Toxicity and survival analysis. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 518–521. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Value |
|---|---|
| Age (years) | |
| Median | 76 |
| Range | 45–83 |
| Gender | |
| Male | 6 |
| Female | 5 |
| Performance status | |
| 0 | 3 |
| 1 | 1 |
| 2 | 6 |
| 3 | 1 |
| Histology | |
| Papillary carcinoma | 5 |
| Anaplastic carcinoma | 3 |
| Squamous cell carcinoma | 3 |
| Organ invaded by tumor(clinical T stage, UICC 8th) | |
| Common carotid artery (T4b) | 5 |
| Aorta (T4b) | 1 |
| Trachea (T4a) | 4 |
| Larynx (T4a) | 1 |
| Tracheostomy | |
| Yes | 4 |
| No | 7 |
| Irradiation dose | |
| 60 Gy in 30 fractions | 7 |
| 54 Gy in 30 fractions | 1 |
| 50 Gy in 20 fractions | 1 |
| 46 Gy in 23 fractions (canceled halfway) | 1 |
| 30 Gy in 15 fractions (canceled halfway) | 1 |
| Concurrent systemic therapy | |
| Docetaxel | 2 |
| Cisplatin/fluorouracil/docetaxel | 1 |
| Cisplatin/etoposide | 1 |
| Lenvatinib | 1 |
| Toxicities | Number of Patients (%) | ||||
|---|---|---|---|---|---|
| G1 | G2 | G3 | G4 | G5 | |
| Hematological | |||||
| Anemia | 2 (18%) | 2 (18%) | 1 (9%) | 0 (0%) | 0 (0%) |
| Leucopenia | 1 (9%) | 0 (0%) | 1 (9%) | 0 (0%) | 0 (0%) |
| Thrombocytopenia | 0 (0%) | 1 (9%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Non-hematological | |||||
| Dermatitis | 4 (36%) | 3 (27%) | 3 (27%) | 0 (0%) | 0 (0%) |
| Pharyngitis | 0 (0%) | 2 (18%) | 2 (18%) | 0 (0%) | 0 (0%) |
| Nausea | 1 (9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wada, Y.; Anbai, A.; Kumagai, S.; Okuyama, E.; Takagi, N.; Hashimoto, M. Treatment Outcomes of External Beam Radiation Therapy for Unresectable Locally Advanced Thyroid Cancer with or without Metastasis: A Retrospective Single-Center Study. Radiation 2021, 1, 174-182. https://doi.org/10.3390/radiation1030016
Wada Y, Anbai A, Kumagai S, Okuyama E, Takagi N, Hashimoto M. Treatment Outcomes of External Beam Radiation Therapy for Unresectable Locally Advanced Thyroid Cancer with or without Metastasis: A Retrospective Single-Center Study. Radiation. 2021; 1(3):174-182. https://doi.org/10.3390/radiation1030016
Chicago/Turabian StyleWada, Yuki, Akira Anbai, Satoshi Kumagai, Eriko Okuyama, Noriko Takagi, and Manabu Hashimoto. 2021. "Treatment Outcomes of External Beam Radiation Therapy for Unresectable Locally Advanced Thyroid Cancer with or without Metastasis: A Retrospective Single-Center Study" Radiation 1, no. 3: 174-182. https://doi.org/10.3390/radiation1030016
APA StyleWada, Y., Anbai, A., Kumagai, S., Okuyama, E., Takagi, N., & Hashimoto, M. (2021). Treatment Outcomes of External Beam Radiation Therapy for Unresectable Locally Advanced Thyroid Cancer with or without Metastasis: A Retrospective Single-Center Study. Radiation, 1(3), 174-182. https://doi.org/10.3390/radiation1030016






