Medicinal Plant Enriched Metal Nanoparticles and Nanoemulsion for Inflammation Treatment: A Narrative Review on Current Status and Future Perspective
Abstract
1. Introduction
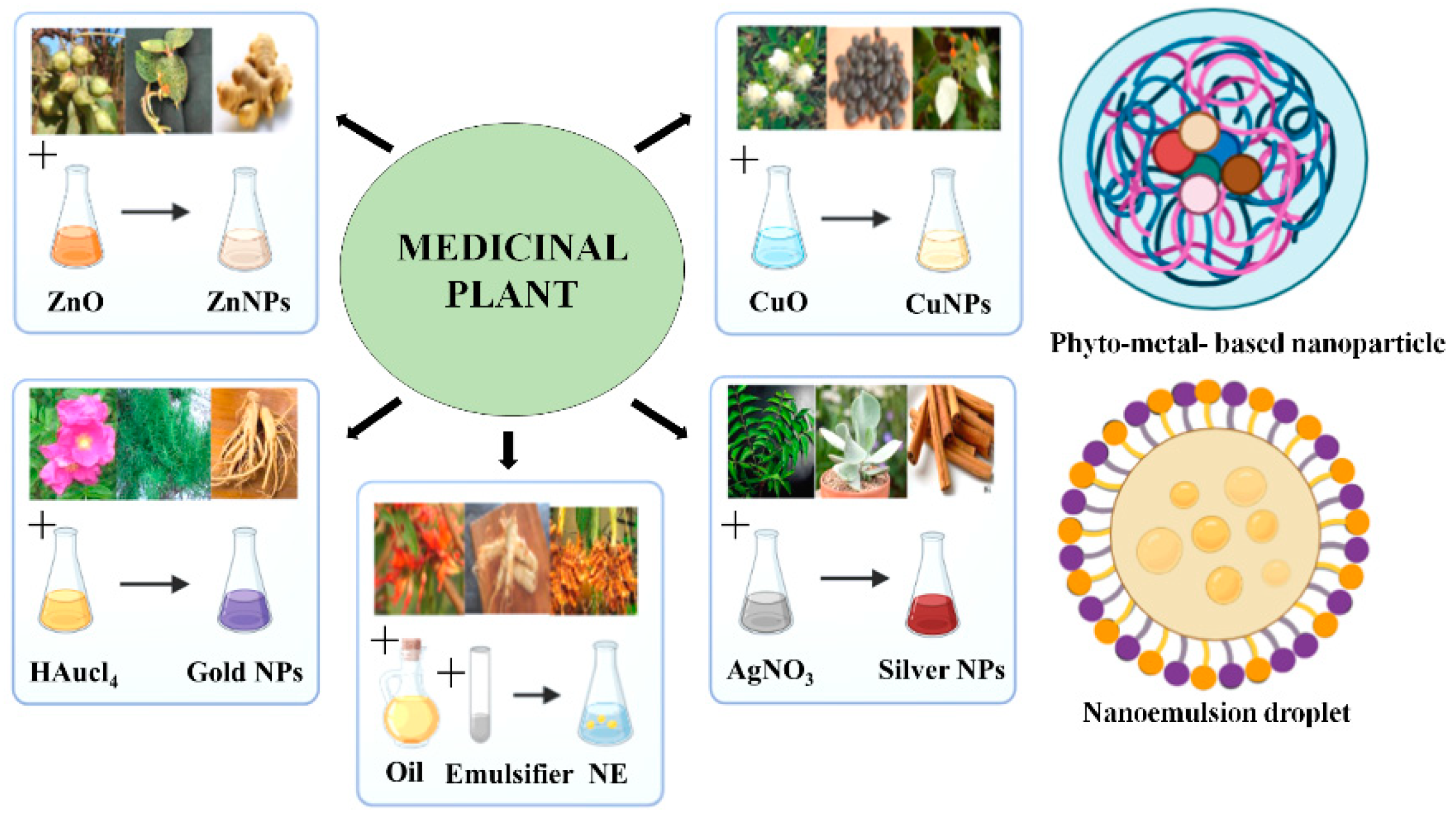
2. Synthesis of Medicinal Plant-Based Metal Nanoparticles and Nanoemulsion
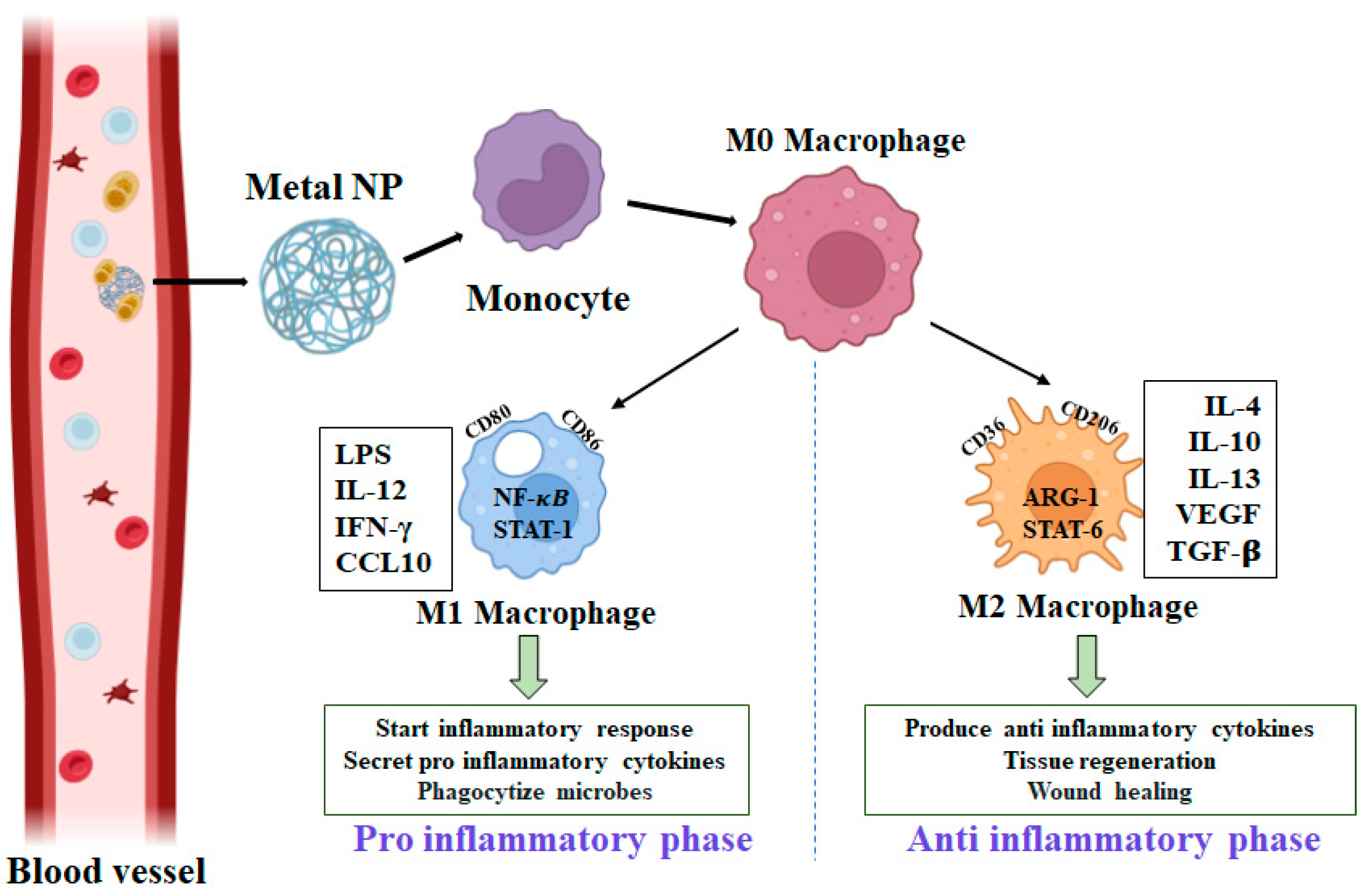
3. Anti-Inflammatory Properties of Metal Nanoparticles and Nanoemulsion
4. Medicinal Plant-Based Metal Nanoparticle
4.1. Therapeutic Gold and Ag Nanoparticles in Inflammation
4.2. Medicinal Plant-Based Zinc and Copper Nanoparticles and Their Impact on Inflammation
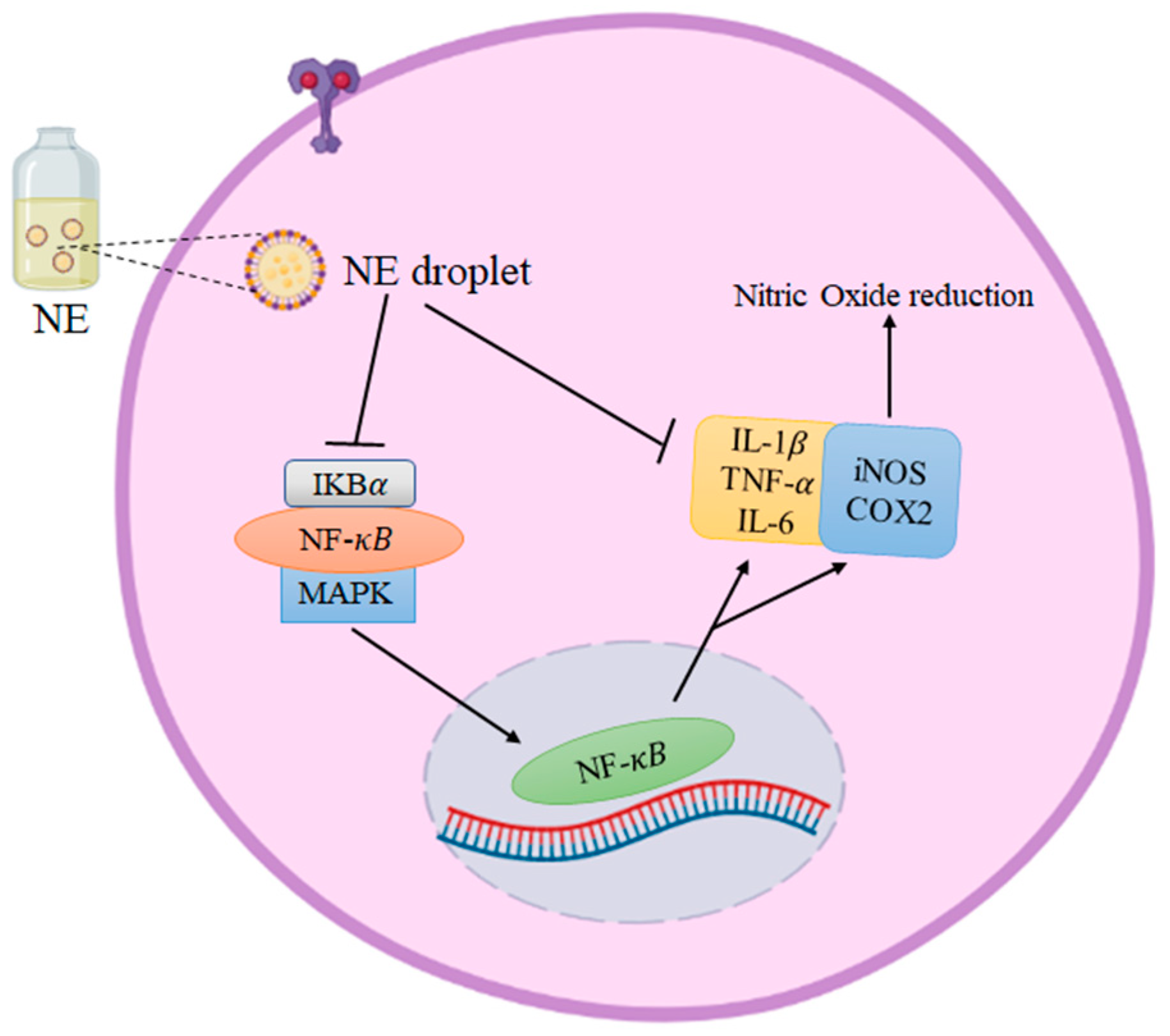
5. Plant-Based Nanoemulsion for Inflammation
6. Current Status, Limitation, and Future Perspective of Metal-Based Nanoparticles and Nanoemulsion for Inflammation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chaloupka, K.; Malam, Y.; Seifalian, A.M. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010, 28, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Li, Q.; Wang, J.; Yu, Y.; Wang, Y.; Zhou, Q.; Li, P. Reactive oxygen species-related nanoparticle toxicity in the biomedical field. Nanoscale Res. Lett. 2020, 15, 1–14. [Google Scholar] [CrossRef]
- Paramanya, A.; Sharma, S.; Bagdat, R.B.; Ali, A. Recent practices of medicinal and aromatic plants in nanotechnology. In Nanomaterials for Agriculture and Forestry Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 435–467. [Google Scholar]
- Ferrero-Miliani, L.; Nielsen, O.H.; Andersen, P.S.; Girardin, S.E. Chronic inflammation: Importance of NOD2 and NALP3 in interleukin-1beta generation. Clin. Exp. Immunol. 2007, 147, 227–235. [Google Scholar] [CrossRef]
- Brusini, R.; Varna, M.; Couvreur, P. Advanced nanomedicines for the treatment of inflammatory diseases. Adv. Drug Deliv. Rev. 2020, 157, 161–178. [Google Scholar] [CrossRef]
- Soltys, L.; Olkhovyy, O.; Tatarchuk, T.; Naushad, M. Green Synthesis of Metal and Metal Oxide Nanoparticles: Principles of Green Chemistry and Raw Materials. Magnetochemistry 2021, 7, 145. [Google Scholar] [CrossRef]
- Shanker, U.; Jassal, V.; Rani, M.; Kaith, B.S. Towards green synthesis of nano-particles: From bio-assisted sources to benign solvents. A review. Int. J. Environ. Anal. Chem. 2016, 96, 801–835. [Google Scholar]
- Singh, J.; Dutta, T.; Kim, K.H.; Rawat, M.; Samddar, P.; Kumar, P. ‘Green’ synthesis of metals and their oxide nanoparticles: Applications for environmental remediation. J. Nanobiotechnol. 2018, 16, 1–24. [Google Scholar] [CrossRef]
- Javadi, S.; Kazemi, N.M.; Halabian, R. Preparation of O/W nano-emulsion containing nettle and fenugreek extract and cumin essential oil for evaluating antidiabetic properties. AAPS Open 2021, 7, 13. [Google Scholar] [CrossRef]
- Elzayat, A.; Adam-Cervera, I.; Álvarez-Bermúdez, O.; Muñoz-Espí, R. Nanoemulsions for synthesis of biomedical nanocarriers. Colloids Surf. B Biointerfaces 2021, 203, 111764. [Google Scholar] [CrossRef] [PubMed]
- Gharibzahedi, S.M.; Jafari, S.M. Fabrication of nanoemulsions by ultrasonication. In Nanoemulsions; Academic Press: Cambridge, MA, USA, 2018; pp. 233–285. [Google Scholar]
- Velusamy, P.; Kumar, G.V.; Jeyanthi, V.; Das, J.; Pachaiappan, R. Bio-inspired green nanoparticles: Synthesis, mechanism, and antibacterial application. Toxicol. Res. 2016, 32, 95–102. [Google Scholar] [CrossRef]
- Fujiwara, N.; Kobayashi, K. Macrophages in Inflammation. Curr. Drug Targets Inflamm. Allergy 2005, 3, 281–286. [Google Scholar] [CrossRef]
- Viscido, A.; Capannolo, A.; Latella, G.; Caprilli, R.; Frieri, G. Nanotechnology in the treatment of inflammatory bowel diseases. J. Crohns Colitis 2014, 8, 903–918. [Google Scholar] [CrossRef]
- Mittal, M.; Siddiqui, M.R.; Tran, K.; Reddy, S.P.; Malik, A.B. Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 2014, 20, 1126–1167. [Google Scholar] [CrossRef]
- Sumbayev, V.V.; Yasinska, I.M.; Garcia, C.P.; Gilliland, D.; Lall, G.S.; Gibbs, B.F.; Bonsall, D.R.; Varani, L.; Rossi, F.; Calzolai, L. Gold nanoparticles downregulate interleukin-1β-induced pro-inflammatory responses. Small 2013, 9, 472–477. [Google Scholar] [CrossRef]
- de Carvalho, T.G.; Garcia, V.B.; de Araújo, A.A.; da Silva Gasparotto, L.H.; Silva, H.; Guerra, G.C.B.; de Castro Miguel, E.; de Carvalho Leitão, R.F.; da Silva Costa, D.V.; Cruz, L.J.; et al. Spherical neutral gold nanoparticles improve anti-inflammatory response, oxidative stress and fibrosis in alcohol-methamphetamine-induced liver injury in rats. Int. J. Pharm. 2018, 548, 1–14. [Google Scholar] [CrossRef]
- Lee, C.G.; Link, H.; Baluk, P.; Homer, R.J.; Chapoval, S.; Bhandari, V.; Kang, M.J.; Cohn, L.; Kim, Y.K.; McDonald, D.M.; et al. Vascular endothelial growth factor (VEGF) induces remodeling and enhances T(H)2-mediated sensitization and inflammation in the lung. Nat. Med. 2004, 10, 1095–1103. [Google Scholar] [CrossRef] [PubMed]
- Franková, J.; Pivodová, V.; Vágnerová, H.; Juráňová, J.; Ulrichová, J. Effects of silver nanoparticles on primary cell cultures of fibroblasts and keratinocytes in a wound healing model. J. Appl. Biomater. Funct. Mater. 2016, 14, 137–142. [Google Scholar] [CrossRef]
- Kim, M.H.; Jeong, H.J. Zinc oxide nanoparticles suppress LPS-Induced NF- κB activation by inducing A20, a negative regulator of NF- κ B, in RAW 264.7 macrophages. J. Nanosci. Nanotechnol. 2015, 9, 6509–6515. [Google Scholar] [CrossRef]
- Britt, R.D., Jr.; Locy, M.L.; Tipple, T.E.; Nelin, L.D.; Rogers, L.K. Lipopolysaccharide-induced Cyclooxygenase-2 expression in mouse transformed clara cells. Cell. Physiol. Biochem. 2012, 29, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, P.; Tripathi, P.; Kashyap, L.; Singh, V. The role of nitric oxide in inflammatory reactions. FEMS Immunol. Med. Microbiol. 2007, 51, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Govindappa, M.; Hemashekhar, B.; Arthikala, M.K.; Rai, V.R.; Ramachandra, Y.L. Characterization, antibacterial, antioxidant, antidiabetic, anti-inflammatory and antityrosinase activity of green synthesized silver nanoparticles using Calophyllum tomentosum leaves extract. Results Phys. 2018, 9, 400–408. [Google Scholar] [CrossRef]
- Yen, C.C.; Chen, Y.C.; Wu, M.T.; Wang, C.C.; Wu, Y.T. Nanoemulsion as a strategy for improving the oral bioavailability and anti-inflammatory activity of andrographolide. Int. J. Nanomed. 2018, 13, 669. [Google Scholar] [CrossRef]
- Shakibaei, M.; John, T.; Schulze-Tanzil, G.; Lehmann, I.; Mobasheri, A. Suppression of NF-kappaB activation by curcumin leads to inhibition of expression of cyclo-oxygenase-2 and matrix metalloproteinase-9 in human articular chondrocytes: Implications for the treatment of osteoarthritis. Biochem. Pharmacol. 2007, 73, 1434–1445. [Google Scholar] [CrossRef] [PubMed]
- Bachstetter, A.D.; Van Eldik, L.J. The p38 MAP kinase family as regulators of proinflammatory cytokine production in degenerative diseases of the CNS. Aging Dis. 2010, 1, 199–211. [Google Scholar]
- Xulu, J.H.; Ndongwe, T.; Ezealisiji, K.M.; Tembu, V.J.; Mncwangi, N.P.; Witika, B.A.; Siwe-Noundou, X. The Use of Medicinal Plant-Derived Metallic Nanoparticles in Theranostics. Pharmaceutics 2022, 14, 2437. [Google Scholar] [CrossRef]
- Shah, M.; Fawcett, D.; Sharma, S.; Tripathy, S.K.; Poinern, G.E.J. Green Synthesis of Metallic Nanoparticles via Biological Entities. Materials 2015, 8, 7278–7308. [Google Scholar] [CrossRef]
- Bharadwaj, K.K.; Rabha, B.; Pati, S.; Sarkar, T.; Choudhury, B.K.; Barman, A.; Bhattacharjya, D.; Srivastava, A.; Baishya, D.; Edinur, H.A.; et al. Green Synthesis of Gold Nanoparticles Using Plant Extracts as Beneficial Prospect for Cancer Theranostics. Molecules 2021, 26, 6389. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.S.; Kim, W.J.; Kim, J.J.; Kim, T.J.; Ye, S.K.; Song, M.D.; Kang, H.; Kim, D.W.; Moon, W.K.; Lee, K.H. Gold nanoparticles attenuate LPS-induced NO production through the inhibition of NF-κB and IFN-β/STAT1 pathways in RAW264.7 cells. Nitric Oxide 2010, 23, 214–219. [Google Scholar] [CrossRef]
- Chandran, S.P.; Chaudhary, M.; Pasricha, R.; Ahmad, A.; Sastry, M. Synthesis of gold nanotriangles and silver nanoparticles using Aloevera plant extract. Biotechnol. Prog. 2006, 22, 577–583. [Google Scholar] [CrossRef]
- Hwang, S.J.; Jun, S.H.; Park, Y.; Cha, S.-H.; Yoon, M.; Cho, S.; Lee, H.-J.; Park, Y. Green synthesis of gold nanoparticles using chlorogenic acid and their enhanced performance for inflammation. Nanomedicine 2015, 11, 1677–1688. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Singh, P.; Castro-Aceituno, V.; Yesmin Simu, S.; Kim, Y.J.; Mathiyalagan, R.; Yang, D.C. Gold nanoparticles synthesized using Panax ginseng leaves suppress inflammatory-mediators production via blockade of NF-κB activation in macrophages. Artif. Cells Nanomed. Biotechnol. 2017, 45, 270–276. [Google Scholar] [CrossRef]
- Cho, J.-Y.; Yang, X.; Park, K.-H.; Park, H.J.; Park, S.-Y.; Moon, J.-H.; Ham, K.-S. Isolation and identification of antioxidative compounds and their activities from Suaeda japonica. Food Sci. Biotechnol. 2013, 22, 1547–1557. [Google Scholar] [CrossRef]
- Kwak, G.Y.; Han, Y.; Baik, S.; Kong, B.M.; Yang, D.C.; Kang, S.C.; Sukweenadhi, J. Green-Synthesized Gold Nanoparticles by the Suaeda japonica Leaf Extract and Screening of Anti-Inflammatory Activities on RAW 267.4 Macrophages. Coatings 2022, 12, 460. [Google Scholar] [CrossRef]
- Nguyen, A.V.; Soulika, A.M. The dynamics of the skin’s immune system. Int. J. Mol. Sci. 2019, 20, 1811. [Google Scholar] [CrossRef] [PubMed]
- Juráňová, J.; Franková, J.; Ulrichová, J. The role of keratinocytes in inflammation. J. Appl. Biomed. 2017, 15, 169–179. [Google Scholar] [CrossRef]
- Wang, R.; Moon, S.K.; Kim, W.J.; Dhandapani, S.; Kim, H.; Kim, Y.J. Biologically Synthesized Rosa rugosa-Based Gold Nanoparticles Suppress Skin Inflammatory Responses via MAPK and NF-κB Signaling Pathway in TNF-α/IFN-γ-Induced HaCaT Keratinocytes. ACS Omega 2022, 7, 35951–35960. [Google Scholar] [CrossRef]
- Zitti, B.; Bryceson, Y.T. Natural killer cells in inflammation and autoimmunity. Cytokine Growth Factor Rev. 2018, 42, 37–46. [Google Scholar] [CrossRef]
- Meirow, Y.; Baniyash, M. Immune biomarkers for chronic inflammation related complications in non-cancerous and cancerous diseases. Cancer Immunol. Immunother. 2017, 66, 1089–1101. [Google Scholar] [CrossRef] [PubMed]
- Elbagory, A.M.; Hussein, A.A.; Meyer, M. The in vitro immunomodulatory effects of gold nanoparticles synthesized from Hypoxis hemerocallidea aqueous extract and hypoxoside on macrophage and natural killer cells. Int. J. Nanomed. 2019, 14, 9007–9018. [Google Scholar] [CrossRef]
- Wynn, T.A.; Chawla, A.; Pollard, J.W. Macrophage biology in development, homeostasis and disease. Nature 2013, 496, 445–455. [Google Scholar] [CrossRef]
- Yu, L.; Chen, Y.; Tooze, S.A. Autophagy pathway: Cellular and molecular mechanisms. Autophagy 2018, 14, 207–215. [Google Scholar] [CrossRef]
- Zhao, T.; Zheng, T.; Yu, H.; Hu, B.H.; Hu, B.; Ma, P.; Yang, Y.; Yang, N.; Hu, J.; Cao, T.; et al. Autophagy impairment as a key feature for acetaminophen-induced ototoxicity. Cell Death Dis. 2021, 12, 3. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wu, Y.; Jin, S.; Tian, Y.; Zhang, X.; Zhao, Y.; Yu, L.; Liang, X.J. Gold nanoparticles induce autophagosome accumulation through size-dependent nanoparticle uptake and lysosome impairment. ACS Nano 2011, 5, 8629–8639. [Google Scholar] [CrossRef]
- Xu, X.Y.; Tran, T.H.M.; Perumalsamy, H.; Sanjeevram, D.; Kim, Y.J. Biosynthetic gold nanoparticles of Hibiscus syriacus L. callus potentiates anti-inflammation efficacy via an autophagy-dependent mechanism. Mater. Sci. Eng. C 2021, 124, 112035. [Google Scholar] [CrossRef] [PubMed]
- Chi, N.T.L.; Narayanan, M.; Chinnathambi, A.; Govindasamy, C.; Subramani, B.; Brindhadevi, K.; Pimpimon, T.; Pikulkaew, S. Fabrication, characterization, anti-inflammatory, and anti-diabetic activity of silver nanoparticles synthesized from Azadirachta indica kernel aqueous extract. Environ. Res. 2022, 208, 112684. [Google Scholar] [CrossRef]
- Tyavambiza, C.; Elbagory, A.M.; Madiehe, A.M.; Meyer, M.; Meyer, S. The antimicrobial and anti-inflammatory effects of silver nanoparticles synthesised from Cotyledon orbiculata aqueous extract. Nanomaterials 2021, 11, 1343. [Google Scholar] [CrossRef] [PubMed]
- Alwan, S.H.; Al-Saeed, M.H. Silver Nanoparticles Biofabricated from Cinnamomum zeylanicum Reduce IL-6, IL-18, and TNF-ɑ in Female Rats with Polycystic Ovarian Syndrome. Int. J. Fertil. Steril. 2023, 17, 80–84. [Google Scholar] [CrossRef]
- Chakravarty, A.; Ahmad, I.; Singh, P.; Sheikh, M.U.D.; Aalam, G.; Sagadevan, S.; Ikram, S. Green synthesis of silver nano-particles using fruits extracts of Syzygium cumini and their bioactivity. Chem. Phys. Lett. 2022, 795, 139493. [Google Scholar] [CrossRef]
- Kedi, P.B.E.; Meva, F.E.A.; Kotsedi, L.; Nguemfo, E.L.; Zangueu, C.B.; Ntoumba, A.A.; Mohamed, H.E.A.; Dongmo, A.B.; Maaza, M. Eco-friendly synthesis, characterization, in vitro and in vivo anti-inflammatory activity of silver nanoparticle-mediated Selaginella myosurus aqueous extract. Int. J. Nanomedicine. 2018, 13, 8537. [Google Scholar] [CrossRef]
- Zhang, X.F.; Liu, Z.G.; Shen, W.; Gurunathan, S. Silver nanoparticles: Synthesis, characterization, properties, applications, and therapeutic approaches. Int. J. Mol. Sci. 2016, 17, 1534. [Google Scholar] [CrossRef]
- Anusha, P.; Narayanan, M.; Natarajan, D.; Kandasamy, S.; Chinnathambi, A.; Alharbi, S.A.; Brindhadevi, K. Assessment of hexavalent chromium (VI) biosorption competence of indigenous Aspergillus tubingensis AF3 isolated from bauxite mine tailing. Chemosphere 2021, 282, 131055. [Google Scholar] [CrossRef]
- Hasan, N.; Ahmad, N.; Zohrameena, S.; Khalid, M.; Akhtar, J. Asparagus racemosus: For medicinal uses &pharmacological actions. Int. J. Adv. Res. 2016, 4, 259–267. [Google Scholar]
- Amina, M.; Al Musayeib, N.M.; Alarfaj, N.A.; El-Tohamy, M.F.; Al-Hamoud, G.A. Antibacterial and immunomodulatory potentials of biosynthesized Ag, Au, Ag-Au bimetallic alloy nanoparticles using the Asparagus racemosus root extract. Nanomaterials 2020, 10, 2453. [Google Scholar] [CrossRef] [PubMed]
- Fulghesu, A.M.; Sanna, F.; Uda, S.; Magnini, R.; Portoghese, E.; Batetta, B. IL-6 serum levels and production is related to an altered immune response in polycystic ovary syndrome girls with insulin resistance. Mediat. Inflamm. 2011, 2011, 389397. [Google Scholar] [CrossRef]
- Narayanan, M.; Gopi, A.; Natarajan, D.; Kandasamy, S.; Saravanan, M.; El Askary, A.; Elfasakhany, A.; Pugazhendhi, A. Hepato and nephroprotective activity of methanol extract of Hygrophila spinosa and its antibacterial potential against multidrug resistant Pandoraea sputorum. Environ. Res. 2021, 201, 111594. [Google Scholar] [CrossRef] [PubMed]
- Aziz, T.; Ullah, A.; Fan, H.; Ullah, R.; Haq, F.; Khan, F.U.; Iqbal, M.; Wei, J. Cellulose nanocrystals applications in health, medicine and catalysis. J. Polym. Environ. 2021, 29, 2062–2071. [Google Scholar] [CrossRef]
- Andarge, E.; Shonga, A.; Agize, M.; Tora, A. Utilization and conservation of medicinal plants and their associated indigenous knowledge (IK) in Dawuro Zone: An ethnobotanical approach. Int. J. Med. Plant Res. 2015, 4, 330–337. [Google Scholar]
- Fadiji, A.E.; Babalola, O.O. Metagenomics methods for the study of plant-associated microbial communities: A review. J. Microbiol. Methods 2020, 170, 105860. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Haw, C.Y.; Zheng, Z.; Kang, J.; Zheng, J.-C.; Wang, H.-Q. Biosynthesis of Zinc Oxide Nanomaterials from Plant Extracts and Future Green Prospects: A Topical Review. Adv. Sustain. Syst. 2021, 5, 200026. [Google Scholar] [CrossRef]
- Sharma, J.; Al-Omran, A.; Parvathy, S. Role of nitric oxide in inflammatory diseases. Inflammopharmacology 2007, 15, 252–259. [Google Scholar] [CrossRef]
- Ramadhania, Z.M.; Nahar, J.; Ahn, J.C.; Yang, D.U.; Kim, J.H.; Lee, D.W.; Kong, B.M.; Mathiyalagan, R.; Rupa, E.J.; Akter, R.; et al. Terminalia ferdinandiana (Kakadu Plum)-Mediated Bio-Synthesized ZnO Nanoparticles for Enhancement of Anti-Lung Cancer and Anti-Inflammatory Activities. Appl. Sci. 2022, 12, 3081. [Google Scholar] [CrossRef]
- Vijayakumar, N.; Bhuvaneshwari, V.K.; Ayyadurai, G.K.; Jayaprakash, R.; Gopinath, K.; Nicoletti, M.; Alarifi, S.; Govindarajan, M. Green synthesis of zinc oxide nanoparticles using Anoectochilus elatus, and their biomedical applications. Saudi J. Biol. Sci. 2022, 29, 2270–2279. [Google Scholar] [CrossRef] [PubMed]
- Scarano, D.; Bertarione, S.; Spoto, G.; Zecchina, A.; Areán, C.O. FTIR spectroscopy of hydrogen, carbon monoxide, and methane absorbed and co-adsorbed on zinc oxide. Thin Solid Film. 2001, 400, 50–55. [Google Scholar] [CrossRef]
- Al-Radadi, N.S.; Faisal, S.; Alotaibi, A.; Ullah, R.; Hussain, T.; Rizwan, M.; Zaman, N.; Iqbal, M.; Iqbal, A.; Ali, Z. Zingiber officinale driven bioproduction of ZnO nanoparticles and their anti-inflammatory, anti-diabetic, anti-Alzheimer, anti-oxidant, and anti-microbial applications. Inorg. Chem. Commun. 2022, 140, 109274. [Google Scholar] [CrossRef]
- Dhivyadharshini, J. Evaluation of anti-inflammatory and antioxidant activity of Adhatoda vasica zinc nanoparticles. Nveo-Nat. Vola. Essen. Oils. 2021, 8, 5950–5964. [Google Scholar]
- Nagajyothi, P.C.; Cha, S.J.; Yang, I.J.; Sreekanth, T.V.M.; Kim, K.J.; Shin, H.M. Antioxidant and anti-inflammatory activities of zinc oxide nanoparticles synthesized using Polygala tenuifolia root extract. J. Photochem. Photobiol. B 2015, 146, 10–17. [Google Scholar] [CrossRef]
- Agarwal, H.; Shanmugam, V.K. Synthesis and optimization of zinc oxide nanoparticles using Kalanchoe pinnata towards the evaluation of its anti-inflammatory activity. J. Drug Deliv. Sci. Technol. 2019, 54, 101291. [Google Scholar] [CrossRef]
- Al-Jubouri, A.K.; Al-Saadi, N.H.; Kadhim, M.A. Anti-Inflammatory and Anti-Bacterial Activity of Copper Nanoparticles Synthesized from Myrtus Communis Leaves Extract. Iraqi J. Agric. Sci. 2022, 53, 698–711. [Google Scholar] [CrossRef]
- Anushya, P.; V Geetha, R.; Rajesh Kumar, S. Evaluation of Anti Inflammatory and Cytotoxic Effect of Copper Nanoparticles Synthesized Using Seed Extract of Mucuna pruriens. J. Pharm. Res. Int. 2021, 33, 816–824. [Google Scholar] [CrossRef]
- Liu, H.; Zheng, S.; Xiong, H.; Alwahibi, M.S.; Niu, X. Biosynthesis of copperoxide nanoparticles using Abies spectabilis plant extract and analyzing its antinociceptive and anti-inflammatory potency in various mice models. Arab. J. Chem. 2020, 13, 6995–7006. [Google Scholar] [CrossRef]
- Manasa, D.J.; Chandrashekar, K.R.; Kumar, D.M.; Niranjana, M.; Navada, K.M. Mussaenda frondosa L. mediated facile green synthesis of Copper oxide nanoparticles–Characterization, photocatalytic and their biological investigations. Arab. J. Chem. 2021, 14, 103184. [Google Scholar] [CrossRef]
- Yu, H.P.; Liu, F.C.; Lin, C.Y.; Umoro, A.; Trousil, J.; Hwang, T.L.; Fang, J.Y. Suppression of neutrophilic inflammation can be modulated by the droplet size of anti-inflammatory nanoemulsions. Nanomedicine 2020, 15, 773–791. [Google Scholar] [CrossRef] [PubMed]
- Rajeshkumar, S.; Menon, S.; Ponnanikajamideen, M.; Ali, D.; Arunachalam, K. Anti-inflammatory and antimicrobial potential of Cissus quadrangularis-assisted copper oxide nanoparticles. Jour. Nanomater. 2021, 2021, 1–11. [Google Scholar] [CrossRef]
- Madene, A.; Jacquot, M.; Scher, J.; Desobry, S. Flavour encapsulation and controlled release—A review. Int. J. Food Sci. Technol. 2006, 41, 1–21. [Google Scholar] [CrossRef]
- Kumar, M.; Bishnoi, R.S.; Shukla, A.K.; Jain, C.P. Techniques for Formulation of Nanoemulsion Drug Delivery System: A Review. Prev. Nutr. Food Sci. 2019, 24, 225–234. [Google Scholar] [CrossRef]
- Thakkar, H.P.; Khunt, A.; Dhande, R.D.; Patel, A.A. Formulation and evaluation of Itraconazole nanoemulsion for enhanced oral bioavailability. J. Microencapsul. 2015, 32, 559–569. [Google Scholar] [CrossRef]
- Mathiyalagan, R.; Wang, C.; Kim, Y.J.; Castro-Aceituno, V.; Ahn, S.; Subramaniyam, S.; Simu, S.Y.; Jiménez-Pérez, Z.E.; Yang, D.C.; Jung, S.-K. Preparation of polyethylene glycol-ginsenoside Rh1 and Rh2 conjugates and their efficacy against lung cancer and inflammation. Molecules 2019, 24, 4367. [Google Scholar] [CrossRef]
- Zhang, R.; Rupa, E.J.; Zheng, S.; Nahar, J.; Yang, D.C.; Kang, S.C.; Wang, Y. Panos-Fermented Extract-Mediated Nanoemulsion: Preparation, Characterization, and In Vitro Anti-Inflammatory Effects on RAW 264.7 Cells. Molecules 2022, 27, 218. [Google Scholar] [CrossRef]
- Wang, X.; Jiang, Y.; Wang, Y.W.; Huang, M.T.; Ho, C.T.; Huang, Q. Enhancing anti-inflammation activity of curcumin through O/W nanoemulsions. Food Chem. 2008, 108, 419–424. [Google Scholar] [CrossRef]
- Borges, R.S.; Keita, H.; Ortiz, B.L.S.; dos Santos Sampaio, T.I.; Ferreira, I.M.; Lima, E.S.; de Jesus Amazonas da Silva, M.; Fernandes, C.P.; de Faria Mota Oliveira, A.E.M.; da Conceição, E.C.; et al. Anti-inflammatory activity of nanoemulsions of essential oil from Rosmarinus officinalis L.: In vitro and in zebrafish studies. Inflammopharmacology 2018, 26, 1057–1080. [Google Scholar] [CrossRef]
- Tran, T.H.M.; Puja, A.M.; Kim, H.; Kim, Y.J. Nanoemulsions prepared from mountain ginseng-mediated gold nanoparticles and silydianin increase the anti-inflammatory effects by regulating NF-κB and MAPK signaling pathways. Biomater. Adv. 2022, 137, 212814. [Google Scholar] [CrossRef] [PubMed]
- Najda, A.; Bains, A.; Klepacka, J.; Chawla, P. Woodfordia fruticosa extract nanoemulsion: Influence of processing treatment on droplet size and its assessment for in vitro antimicrobial and anti-inflammatory activity. Front. Nutr. 2022, 9, 944856. [Google Scholar] [CrossRef]
- El-Naggar, M.E.; Hussein, J.; El-sayed, S.M.; Youssef, A.M.; El Bana, M.; Latif, Y.A.; Medhat, D. Protective effect of the functional yogurt based on Malva parviflora leaves extract nanoemulsion on acetic acid-induced ulcerative colitis in rats. J. Mater. Res. Technol. 2020, 9, 14500–14508. [Google Scholar] [CrossRef]
- Hoseny, S.S.; Soliman, A.M.; Fahmy, S.R.; Sadek, S.A. Development of a Novel Pomegranate Polysaccharide Nanoemulsion Formulation with Anti-Inflammatory, Antioxidant, and Antitumor Properties. Curr. Drug Deliv. 2022, 20, 575–586. [Google Scholar] [CrossRef]
- Rahimi Kalateh Shah Mohammad, G.; Homayouni Tabrizi, M.; Ardalan, T.; Yadamani, S.; Safavi, E. Green synthesis of zinc oxide nanoparticles and evaluation of anti-angiogenesis, anti-inflammatory and cytotoxicity properties. J. Biosci. 2019, 44, 30. [Google Scholar] [CrossRef]
- Kim, C.S.; Nguyen, H.D.; Ignacio, R.M.; Kim, J.H.; Cho, H.C.; Maeng, E.H.; Kim, Y.R.; Kim, M.K.; Park, B.K.; Kim, S.K. Immunotoxicity of zinc oxide nanoparticles with different size and electrostatic charge. Int. J. Nanomed. 2014, 9, 195–205. [Google Scholar] [CrossRef]
- Hooper, H.L.; Jurkschat, K.; Morgan, A.J.; Bailey, J.; Lawlor, A.J.; Spurgeon, D.J.; Svendsen, C. Comparative chronic toxicity of nanoparticulate and ionic zinc to the earthworm Eisenia veneta in a soil matrix. Environ. Int. 2011, 37, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.; Lim, D.H.; Choi, I.H. The impact of nanomaterials in immune system. Immune Netw. 2010, 10, 85–91. [Google Scholar] [CrossRef]
- Pasupuleti, S.; Alapati, S.; Ganapathy, S.; Anumolu, G.; Pully, N.R.; Prakhya, B.M. Toxicity of zinc oxide nanoparticles through oral route. Toxicol. Ind. Health 2012, 28, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Naz, S.; Gul, A.; Zia, M. Toxicity of copper oxide nanoparticles: A review study. IET Nanobiotechnol. 2020, 14, 1–13. [Google Scholar] [CrossRef] [PubMed]
- McClements, D.J.; Rao, J. Food-grade nanoemulsions: Formulation, fabrication, properties, performance, biological fate, and potential toxicity. Crit. Rev. Food Sci. Nutr. 2011, 51, 285–330. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.V.; Fryer, P.J.; Frith, W.J.; Norton, I.T. Emulsification mechanism and storage instabilities of hydrocarbon-in-water sub-micron emulsions stabilised with Tweens (20 and 80), Brij 96v and sucrose monoesters. J. Colloid Interface Sci. 2009, 338, 201–206. [Google Scholar] [CrossRef] [PubMed]
| Nanoparticle | Medicinal Plants | Observation | Characteristics Size/Shape | Anti-Inflammatory Action | Ref |
|---|---|---|---|---|---|
| Gold | Panax gin-seng Meyer leaf | In vitro | 10–20 nm | Reduction of the expression of the inflammatory mediators in the NF-κB signaling pathway | [33] |
| Gold | Suaeda japonica Leaf | In vitro | 8.75 nm Crystalline | Suppress the generation of nitric oxide (NO) and repress the expression of the pro-inflammatory gene | [35] |
| Gold | Rosa ru-gosa(beach rosea) | In vitro | 38.2 ± 3.7 nm Polygonal | Treat skin inflammation by reducing oxidative stress via the MAPK and NF-κB sig-naling pathways | [38] |
| Gold | Hypoxis hemerocallidea | In vitro | 26 ± 2 nm Spherical | Reduce the amounts of pro-inflammatory cytokines in macrophage cells | [41] |
| Gold | Hibiscus syriacus L | In vitro | 3–20 nm Spherical | Suppress pro-inflammatory cytokines and decrease the expressions of PINK1 and Parkin in autophagy-dependent mechanism | [46] |
| Silver | Azadirachta indica kernel | In vitro | 19.27–22.15 nm Spherical | Control protein degradation to fight inflammation | [47] |
| Silver | Cotyledon orbiculata | In vitro | 20 to 40 nm | Suppress the secretion of the pro-inflammatory marker in LPS-treated macrophage | [48] |
| Silver | Cin-namomum zeylanicum bark | In vitro | 60–80 nm Spherical | Decrease TNF-α, IL-6, and IL-18 inflammatory markers of PCOS | [49] |
| Silver | Syzygium cumini fruit | In vitro | ~47 nm Spherical | Protein denaturation in higher concentration | [50] |
| Silver | Selaginella myosurus | In vitro | 33.7, 44.2 | Inhibition of thermally induced denaturation of albumin | [51] |
| Nanoparticle | Medicinal Plants | Observation | Characteristics Size/Shape | Anti-Inflammatory Action | Ref |
|---|---|---|---|---|---|
| Zn | Terminalia ferdinandiana (Kakadu plum) | In vitro | 21.89 nm Crystalline | Inhibition of pro-inflammatory nitric oxide production | [63] |
| Zn | Zingiber officinale | In vitro | 30 nm Spherical | Inhibition of COX1 and COX2 | [66] |
| Zn | Polygala tenuifolia root) | In vitro | 9.22 nm Spherical | Downregulation of both mRNA and protein ex-pressions of inflammatory mediators | [68] |
| Zn | Kalanchoe pinnata | In vitro | 24 nm | Suppress pro-inflammatory mediators such as interleukin 6 (IL-6), interleukin 1 (IL-1), tumor necrosis factor (TNF-α), and cyclooxy-genase-2 (COX-2) | [69] |
| Copper | Myrtus Communis leaves | In vitro | 53.55 nm Crystalline | Inhibition of protein oxidation | [70] |
| Copper | Mucuna pruriens seed | In vitro | NA | Suppress the inflammatory mediators | [71] |
| Copper | Abies spectabilis | In vitro | NA | Suppress the inflammatory cytokines IL-1β, IL-6, and TNF-α | [72] |
| Medicinal Plants | Phases | Types | Observation | Mechanism/Pathway/Action | Ref |
|---|---|---|---|---|---|
| Panax ginseng leaf extract | Leaf extract + Water + Sea buckthorn oil | O/W | In vitro | Suppression of pro-inflammatory mediators for (Cox 2, IL-6, IL-1β, and TNF-α, NF-κB, Ikkα, and iNOS) gene expression | [80] |
| Curcumin | Curcumin + Water + MCT | O/W | In vitro | Inhibition of TPA-induced edema of mouse ear | [81] |
| Rosmarinus officinalis L | Leaf extract + Essential oil | O/W | In vitro | Inhibiting the production of the pro-inflammatory mediator nitric oxide | [82] |
| Mountain gin-seng | Ginseng ex-tract + Gin-seng seed oil | O/W | In vitro | Inhibition of pro-inflammatory genes and proteins, including IL-1β, IL-6, and TNF-α via NF-κB and MAPK signaling pathways | [83] |
| Woodfordia fruticosa flower extract | Flower extract + Sunflower seed oil | O/W | Bacterial cell membrane | Inhibit the release of inflammatory mediators and stabilize cell membrane | [84] |
| Malva parviflora leaf extract | Leaf extract + Yoghurt b | O/W | In vitro | Diminish the production of superoxide by inhibiting NADPH oxidase | [85] |
| Punica granatum peel | Fruit Peel extract + Cremophor RH40 | O/W | In vitro | Stabilize the lysosomal membrane as anti-inflammatory efficacy. | [86] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puja, A.M.; Rupa, E.J.; Kim, Y.J.; Yang, D.-C. Medicinal Plant Enriched Metal Nanoparticles and Nanoemulsion for Inflammation Treatment: A Narrative Review on Current Status and Future Perspective. Immuno 2023, 3, 182-194. https://doi.org/10.3390/immuno3020012
Puja AM, Rupa EJ, Kim YJ, Yang D-C. Medicinal Plant Enriched Metal Nanoparticles and Nanoemulsion for Inflammation Treatment: A Narrative Review on Current Status and Future Perspective. Immuno. 2023; 3(2):182-194. https://doi.org/10.3390/immuno3020012
Chicago/Turabian StylePuja, Aditi Mitra, Eshrat Jahan Rupa, Yeon Ju Kim, and Deok-Chun Yang. 2023. "Medicinal Plant Enriched Metal Nanoparticles and Nanoemulsion for Inflammation Treatment: A Narrative Review on Current Status and Future Perspective" Immuno 3, no. 2: 182-194. https://doi.org/10.3390/immuno3020012
APA StylePuja, A. M., Rupa, E. J., Kim, Y. J., & Yang, D.-C. (2023). Medicinal Plant Enriched Metal Nanoparticles and Nanoemulsion for Inflammation Treatment: A Narrative Review on Current Status and Future Perspective. Immuno, 3(2), 182-194. https://doi.org/10.3390/immuno3020012










