Plasma Cytokine Levels and Cytokine Genetic Polymorphisms in Patients with Metastatic Breast Cancer Receiving High-Dose Chemotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Cytokine Quantitation in Plasma Samples
2.3. Analysis of SNPs
2.4. Statistical Methods
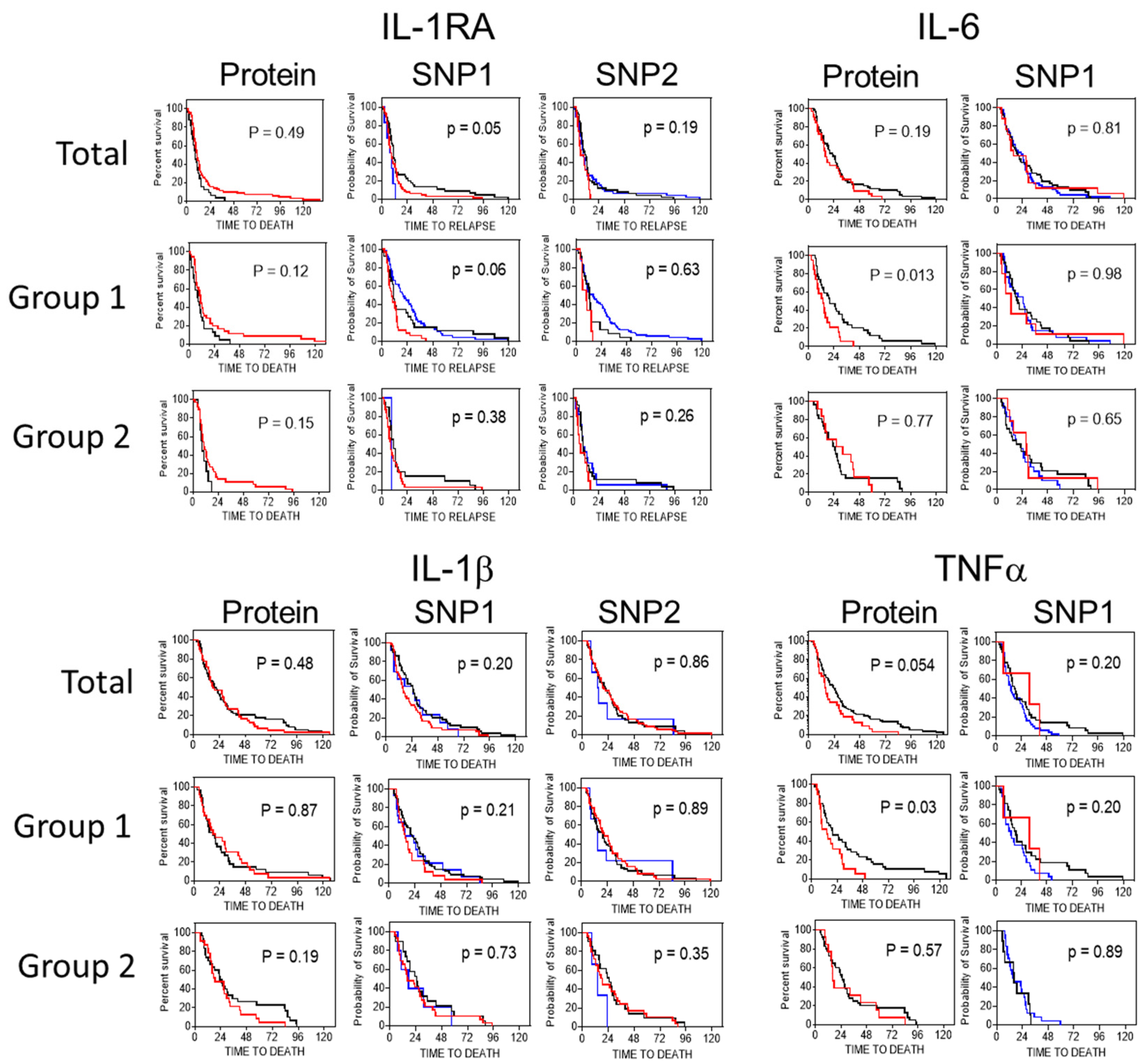
3. Results
3.1. Patient Characteristics
3.2. Plasma Biomarkers
3.3. Genotypic Frequencies of Polymorphisms
3.4. Comparison of Plasma Markers and Genetic Polymorphisms
3.5. Combination of Variant Genotypes and Survival
3.6. Cytokine Levels and Clinicopathological Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yako, Y.Y.; Kruger, D.; Smith, M.; Brand, M. Cytokines as biomarkers of pancreatic ductal adenocarcinoma: A systematic review. PLoS ONE 2016, 11, e01540162016. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Garcia, B.; Eiro, N.; Miranda, M.A.; Cid, S.; Gonzalez, L.O.; Dominiguez, F.; Vizoso, F.J. Prognostic significance of inflammatory factors expression by stroma from breast carcinomas. Carcinogenesis 2016, 37, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Rabi, Z.A.; Todorovic-Rakovic, N.; Vujasinovic, T.; Milovanovic, J.; Nikolic-Vukosavljevic, D. Markers of progression and invasion in short term follow up of untreated breast cancer patients. Cancer Biomark. 2015, 15, 745–754. [Google Scholar] [CrossRef]
- Goldberg, J.E.; Schwertfeger, K.L. Proinflammatory cytokines in breast cancer: Mechanisms of action and potential targets for therapeutics. Curr. Drug Targets 2010, 11, 1133–1146. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Park, S.K.; Hamajima, N.; Tajima, K.; Choi, J.Y.; Noh, D.; Ahn, S.H.; Yoo, K.; Hirvonen, A.; Kang, D. Genetic polymorphisms of interleukin-1 beta (IL-1B) and IL-1 receptor antagonist (IL-1RN) and breast cancer risk in Korean women. Breast Cancer Res. Treat. 2006, 96, 197–202. [Google Scholar] [CrossRef]
- Lewis, A.M.; Varghese, S.; Xu, H.; Alexander, H.R. Interleukin-1 and cancer progression: The emerging role of interleukin-1 receptor antagonist as a novel therapeutic agent in cancer treatment. J. Transl. Med. 2006, 4, 48. [Google Scholar] [CrossRef]
- Lee, H.M.; Lee, H.H.; Chang, J.E. Inflammatory cytokine: An attractive target for cancer treatment. Biomedicines 2022, 10, 2116. [Google Scholar] [CrossRef]
- Miller, L.J.; Kurtzman, S.H.; Anderson, K.; Wang, Y.; Stankus, M.; Renna, M.; Linquist, R.; Barrows, G.; Kreutzer, D.L. Interleukin-1 family expression in human breast cancer: Interleukin-1 receptor antagonist. Cancer Investig. 2000, 18, 293–302. [Google Scholar] [CrossRef]
- Lin, S.; Gan, Z.; Han, K.; Yao, Y.; Min, D. Interleukin-6 as a prognostic marker for breast cancer: A meta-analysis. Tumori 2015, 101, 535–541. [Google Scholar] [CrossRef]
- Won, H.S.; Kim, Y.A.; Lee, J.S.; Jeon, E.K.; An, H.J.; Sun, D.S.; Ko, Y.H.; Kim, J.S. Soluble interleukin-6 receptor is a prognostic marker for relapse-free survival in estrogen receptor-positive breast cancer. Cancer Investig. 2013, 31, 516–521. [Google Scholar] [CrossRef]
- Fuksiewicz, M.; Kowalska, M.; Kotowicz, B.; Rubach, M.; Chedklinska, M.; Pienkowski, T.; Kaminska, J. Serum soluble tumour necrosis factor receptor type I concentrations independently predict prognosis in patients with breast cancer. Clin. Chem. Lab. Med. 2010, 48, 1481–1486. [Google Scholar] [CrossRef] [PubMed]
- Tripsianis, G.; Papadopoulou, E.; Anagnostopoulos, K.; Botaitis, S.; Katotomichelakis, M.; Romainidis, K.; Kontomanolis, E.; Tentes, I.; Kortsaris, A. Coexpression of IL-6 and TNF-α: Prognostic significance on breast cancer outcome. Neoplasma 2014, 61, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Milovanovic, J.; Todorovic-Rakovic, N.; Radulovic, M. Interleukin-6 and interleukin-8 serum levels in prognosis of hormone-dependent breast cancer. Cytokine 2018, S1043–4666, 300065–300066. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Ammer, A.; Storr, S.J.; Green, A.R.; Rakha, E.; Els, I.Q.; Marin, S.G. IL-6 and IL-10 are associated with good prognosis in early stage invasive breast cancer patients. Immunol. Immunother. 2018, 67, 537–549. [Google Scholar] [CrossRef] [PubMed]
- Tripsianis, G.; Papadopoulou, E.; Romanidis, K.; Katotomichelakis, M.; Anagnostopoulos, K.; Kontomanolis, E.; Botaitis, S.; Tentes, I.; Kortasaris, A. Overall survival and clinicopathological characteristics of patients with breast cancer in relation to the expression pattern of HER-2, IL-6, TNF-α, and TGF-β1. Asian Pac. J. Cancer Prev. 2013, 14, 6813–6820. [Google Scholar] [CrossRef]
- Ma, Y.; Ren, Y.; Dai, Z.J.; Wu, C.J.; Ji, Y.; Xu, J. IL-6, IL-8 and TNF- levels correlate with disease stage in breast cancer patients. Adv. Clin. Exp. Med. 2017, 26, 421–426. [Google Scholar] [CrossRef]
- Domschke, C.; Schuetz, F.; Ge, Y.; Seibel, T.; Falk, C.; Brors, B.; Vlodavsky, I.; Sommerfeldt, N.; Sinn, H.P.; Kuhnle, M.C.; et al. Intratumoral cytokines and tumor cell biology determine spontaneous breast cancer-specific immune responses and their correlation to prognosis. Cancer Res. 2009, 69, 8420–8428. [Google Scholar] [CrossRef]
- Muraro, E.; Martorelli, D.; Turchet, E.; Miolo, G.; Scalone, S.; Comaro, E.; Talamini, R.; Mastorci, K.; Lombardi, D.; Perin, T.; et al. A different immunologic profile characterizes patients with HER-2 overexpressing and HER-2-negative locally advanced breast cancer: Implications for immune-based therapies. Breast Cancer Res. 2011, 13, R117. [Google Scholar] [CrossRef]
- Saglam, S.; Suzme, R.; Gurdol, R. Serum tumor necrosis factor-alpha and interleukin-2 concentrations in newly diagnosed ERBB2 (HER2/neu) positive breast cancer patients. Int. J. Biol. Markers 2009, 24, 142–146. [Google Scholar] [CrossRef]
- Li, L.; Chen, L.; Zhang, W.; Liao, Y.; Chen, J.; Shi, Y.; Luo, S. Serum cytokine profile in patients with breast cancer. Cytokine 2017, 89, 173–178. [Google Scholar] [CrossRef]
- Lv, M.; Xiaoping, X.; Cai, H.; Li, D.; Wang, J.; Fu, X.; Yu, F.; Sun, M.; Lv, Z. Cytokines as prognostic tool in breast carcinoma. Front. Biosci. 2011, 16, 2515–2526. [Google Scholar] [CrossRef] [PubMed]
- Quan, L.; Gong, Z.; Yao, S.; Bandera, E.V.; Zirpoli, G.; Hwang, H.; Roberts, M.; Ciupak, G.; Davis, W.; Sucheston, L.; et al. Cytokine and cytokine receptor genes of the adaptive immune response are differentially associated with breast cancer risk in American women of African and European ancestry. Int. J. Cancer 2014, 134, 1408–1421. [Google Scholar] [CrossRef] [PubMed]
- Woods, N.T.; Monteiro, A.N.; Thompson, Z.J.; Amankwah, E.K.; Naas, N.; Haura, E.B.; Beg, A.A.; Schabath, M.B. Interleukin polymorphisms associated with overall survival, disease-free survival, and recurrence in non-small cell lung cancer patients. Mol. Carcinog. Suppl. 2015, 1, E172–E184. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Z.; Yu, J.; Lei, G.; Wang, S. Three polymorphisms in interleukin-1beta gene and risk for breast cancer: A meta-analysis. Breast Cancer Res. Treat. 2010, 124, 821–825. [Google Scholar] [CrossRef]
- Grimm, C.; Kantelhardt, E.; Heinze, G.; Polerauer, S.; Zellinger, R.; Kolbl, H.; Reinthaller, A.; Hefler, L. The prognostic value of four interleukin-1 gene polymorphisms in Caucasian women with breast cancer: A multicentre study. BMC Cancer 2009, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Slattery, M.L.; Herrick, J.S.; Torres-Mejia, G.; John, E.M.; Giuliano, A.R.; Hines, L.M.; Stern, M.C.; Baumgartner, K.B.; Presson, A.P.; Wolff, R.K. Genetic variants in interleukin genes are associated with breast cancer risk and survival in a genetically admixed population: The Breast Cancer Health Disparities Study. Carcinogenesis 2014, 35, 1750–1759. [Google Scholar] [CrossRef] [PubMed]
- Snoussi, K.; Strosberg, A.D.; Bouaouina, N.; Ben Ahmesd, S.; Chouchane, L. Genetic variation in pro-inflammatory cytokines Iinterleukin-1beta, interleukin-1alpha and interleukin-6) associated with the aggressive forms, survival, and relapse prediction of breast carcinoma. Eur. Cytokine Netw. 2005, 16, 253–260. [Google Scholar]
- Xu, H.; Ding, Q.; Jiang, H.W. Genetic polymorphism of interleukin-1A(IL-1A), IL-1B, and IL-1 receptor antagonist (IL-RN) and prostate cancer risk. Asian Pac. J. Cancer Prev. 2014, 15, 8741–8747. [Google Scholar] [CrossRef]
- Reiner, A.P.; Wurfel, M.M.; Lange, L.A.; Carlson, C.S.; Nord, A.S.; Carty, C.L.; Rieder, M.J.; Desmarais, C.; Jenny, N.S.; Iribarren, C.; et al. Polymorphisms of the IL-1-Receptor antagonist gene (IL1RN) are associated with multiple markers of systemic inflammation. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 1401–1412. [Google Scholar] [CrossRef]
- Cherel, M.; Campion, L.; Bezieau, S.; Campone, M.; Charrier, J.; Gaschet, J.; Ricolleau, G.; Gouraud, W.; Charbonnel, C.; Jezequel, P. Molecular screening of interleukin-6 gene promoter and influence of -174G/C polymorphism on breast cancer. Cytokine 2009, 47, 214–223. [Google Scholar] [CrossRef]
- Kohaar, I.; Tiwari, P.; Kimar, R.; Nasare, V.; Thankur, N.; Das, B.C.; Bhardwaj, M. Association of single nucleotide polymorphisms (SNPs) in TNF-LTA locus with breast cancer risk in Indian population. Breast Cancer Res. Treat. 2009, 114, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Gaudet, M.M.; Egan, K.M.; Lissowska, J.; Newcomb, P.A.; Brinton, L.A.; Titus-Ernstoff, L.; Yeager, M.; Chanock, S.; Welch, R.; Peplonska, B.; et al. Genetic variation in tumour necrosis factor and lymphotoxin-alpha (TNF-LTA) and breast cancer risk. Hum. Genet. 2007, 121, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Zuloeta Ladd, A.M.; Arias Vasquez, A.; Witteman, J.; Uitterlinden, A.G.; Goebergh, J.W.; Hofman, A.; Stricker, B.H.; van Duijn, C.M. Interleukin-6 G-174-C polymorphism and breast cancer risk. Eur. J. Epidemiol. 2006, 21, 373–376. [Google Scholar] [CrossRef]
- Hu, X.B.; Ouyang, L.Z.; Tang, L.L. Interleukin-2 gene polymorphisms and prognosis of breast cancer. Genet. Test. Mol. Biomark. 2013, 17, 453–457. [Google Scholar] [CrossRef]
- Chen, H.; Wilkins, L.; Aziz, N.; Cannings, C.; Wyllie, D.H.; Bingle, C.; Rogus, J.; Beck, J.D.; Offenbacher, S.; Cork, M.J.; et al. Single nucleotide polymorphisms in the human interleukin-1B gene affect transcription according to haplotype context. Hum. Mol. Genet. 2006, 15, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Rafiq, S.; Stevens, K.; Hrust, A.J.; Murray, A.; Henley, W.; Weedon, M.N.; Bandinelli, S.; Corsi, A.M.; Guralnik, J.M.; Ferruci, L.; et al. Common genetic variation in the gene encoding inteleukin-1-receptor antagonist (IL-1RA) is associated with altered circulating IL-1RA levels. Genes Immun. 2007, 8, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Graziano, F.; Ruzzo, A.; Canestrari, E.; Loupakis, F.; Santini, D.; Rulli, E.; Humar, B.; Galluccio, N.; Bisonni, R.; Floriani, I.; et al. Variations in the interleukin-1 receptor antagonist gene impact on survival of patients with advanced colorectal cancer. Pharm. J. 2009, 9, 78–84. [Google Scholar] [CrossRef]
- DeMichele, A.; Marin, A.M.; Mick, R.; Gor, P.; Wray, L.; Klein-Cabral, M.; Athanasiadis, G.; Culligan, T.; Stadtmauer, E.; Weber, B. Interleukin-6 -174G-C polymorphism is associated with improved outcome in high-risk breast cancer. Cancer Res. 2003, 63, 8051–8056. [Google Scholar]
- Burzotta, F.; Iacoviello, L.; Di Castelnuovo, A.; Glieca, F.; Luciani, N.; Zamparelli, R.; Schiavello, R.; Donati, M.B.; Maseri, A.; Possati, G.; et al. Relation of the -174 G/C polymorphism of interleukin-6 to interleukin-6 plasma levels and to length of hospitalization after surgical coronary revascularization. Am. J. Cardiol. 2001, 88, 1125–1128. [Google Scholar] [CrossRef]
- Hajeer, A.H.; Hutchinson, I.V. Influence of TNFalpha gene polymorphisms on TNFalpha production and disease. Hum. Immunol. 2001, 62, 1191–1199. [Google Scholar] [CrossRef]
- Erichsen, H.C.; Chanock, S.J. SNPs in cancer research and treatment. Br. J. Cancer 2004, 90, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Gluck, S. Autologous transplantation for patients with advanced breast cancer with emphasis on bony metastasis. Can. J. Oncol. 1995, 5, 58–62. [Google Scholar] [PubMed]
- Gluck, S.; Germond, C.; Lopez, P.; Cano, P.; Doreen, M.; Koski, T.; Arnold, A.; Dulude, H.; Gallant, G. High dose paclitaxel, cyclophosphamide and mitoxantrone followed by autologous blood stem cell support for the treatment of metastatic breast cancer: A phase I trial. Eur. J. Cancer 1998, 34, 1008–1014. [Google Scholar] [CrossRef] [PubMed]
- Bewick, M.; Chadderton, T.; Gluck, S. Prognostic potential of C-erbB-2/HER2 over expression in patients with metastatic breast cancer undergoing high-dose chemotherapy and blood stem cell transplantation. Blood 1997, 90, 1029. [Google Scholar]
- Bewick, M.; Chadderton, T.; Conlon, M.; Lafrenie, R.; Morris, D.; Stewart, D.; Gluck, S. Expression of c-erbB-2/HER2 in patients with metastatic breast cancer undergoing high-dose chemotherapy and autologous blood stem cell support. Bone Marrow Transpl. 1999, 24, 377–384. [Google Scholar] [CrossRef]
- Bewick, M.; Conlon, M.; Gerard, S.; Lee, H.; Parissenti, A.M.; Zhang, L.; Gluck, S.; Lafrenie, R.M. HER-2 expression is a prognostic factor in patients with metastatic breast cancer treated with a combination of high-dose cyclophosphamide, mitoxantrone, paclitaxel and autologous stem cell support. Bone Marrow Transpl. 2001, 27, 847–854. [Google Scholar] [CrossRef]
- Kaplan, E.L.; Meier, P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Cox, D.R. Regression models and life-tables (with discussion). J. R. Statist. Soc. Ser. B 1972, 34, 187–220. [Google Scholar]
- Bewick, M.; Conlon, M.; Gerard, S.; Lee, H.; Parissenti, A.M.; Zhang, L.; Gluck, S.; Lafrenie, R.M. Evaluation of sICAM-1, sVCAM-1, and sE-selectin levels in patients with metastatic breast cancer receiving high-dose chemotherapy. Stem Cells Dev. 2004, 13, 281–294. [Google Scholar] [CrossRef]
- Zhang, G.J.; Adachi, I. Serum interleukin-6 levels correlate to tumor progression and prognosis in metastatic breast carcinoma. Anticancer Res. 1999, 19, 1427–1432. [Google Scholar]
- Zitvogel, L.; Apetoh, L.; Ghiringhelli, F.; Kroemer, G. Immunological aspects of cancer chemotherapy. Nat. Rev. Immunol. 2008, 8, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Bahiraee, A.; Ebrahimi, R.; Halabian, R.; Aghabozorgi, A.S.; Amani, J. The role of inflammation and its related microRNAs in breast cancer: A narrative review. J. Cell Physiol. 2019, 234, 19480–19493. [Google Scholar] [CrossRef] [PubMed]
- Pusztai, L.; Mendoza, T.R.; Reuben, J.M.; Marinez, M.M.; Wiley, J.S.; Lara, J.; Syed, A.; Fritsche, H.A.; Bruera, E.; Booser, D.; et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine 2004, 25, 94–102. [Google Scholar] [CrossRef] [PubMed]
- White, C.M.; Martin, B.K.; Lee, L.F.; Haskill, J.; Ting, J.P. Effects of paclitaxel on cytokine synthesis by unprimed human monocytes, T lymphocytes, and breast cancer cells. Cancer Immunol. Immunother. 1998, 46, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Wesolowski, R.; Duggan, M.C.; Stiff, A.; Markowitz, J.; Trikha, P.; Levine, K.M.; Schoenfield, L.; Abdel-Rasoul, M.; Layman, R.; Ramaswamy, B.; et al. Circulating myeloid-derived suppressor cells increase in patients undergoing neo-adjuvant chemotherapy for breast cancer. Cancer Immunol. Immunother. 2017, 66, 1437–1447. [Google Scholar] [CrossRef] [PubMed]
- Sevko, A.; Michels, T.; Vrohlings, M.; Umansky, L.; Beckhove, P.; Kato, M.; Shurin, G.V.; Shurin, M.R.; Umansky, V. Antitumor effect of paclitaxel is mediated by inhibition of myeloid-derived suppressor cells and chronic inflammation in the spontaneous melanoma model. J. Immunol. 2013, 190, 2464–2471. [Google Scholar] [CrossRef]
- Heylmann, D.; Bauer, M.; Becker, H.; van Gool, S.; Bacher, N.; Steinbrink, K.; Kaina, B. Human CD4+CD25+ regulatory T cells are sensitive to low dose cyclophosphamide: Implications for the immune response. PLoS ONE 2013, 8, e833842013. [Google Scholar] [CrossRef]
- Janelsins, M.C.; Mustian, K.M.; Palesh, O.G.; Mohile, S.G.; Peppone, L.J.; Sprod, L.K.; Heckler, C.E.; Roscoe, J.A.; Katz, A.W.; Williams, J.P.; et al. Differential expression of cytokines in breast cancer patients receiving different chemotherapies: Implications for cognitive impairment research. Support. Care Cancer 2012, 20, 831–839. [Google Scholar] [CrossRef]
- Vyas, D.; Laput, G.; Vyas, A.K. Chemotherapy-enhanced inflammation may lead to the failure of therapy and metastasis. OncoTargets Ther. 2014, 7, 1015–1023. [Google Scholar] [CrossRef]
- Bewick, M.; Conlon, M.; Parissenti, A.M.; Lee, H.; Zhang, L.; Gluck, S.; Lafrenie, R.M. Soluble Fas (CD95) is a prognostic factor in patients with metastatic breast cancer undergoing high-dose chemotherapy and autologous stem cell transplantation. J. Hematotherapy Stem Cell Transpl. 2001, 10, 759–768. [Google Scholar] [CrossRef]
- Bewick, M.A.; Conlon, M.S.; Lafrenie, R.M. Polymorphisms in manganese superoxide dismutatase, myeloperoxidase and glutathione-S-transferase and survival after treatment for metastatic breast cancer. Breast Cancer Res. Treat. 2008, 111, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Bewick, M.A.; Conlon, M.S.; Lafrenie, R.M. Polymorphisms in XRCC1, XRCC3, and CCND1 and survival after treatment for metastatic breast cancer. J. Clin. Oncol. 2006, 24, 5645–5651. [Google Scholar] [CrossRef] [PubMed]


| Clinical Characteristic | Total | Group 1 | Group 2 |
|---|---|---|---|
| (N = 130) | (N = 74) | (N = 56) | |
| Age | |||
| <40 | 32 | 21 | 11 |
| 40–49 | 66 | 39 | 27 |
| 50–59 | 32 | 14 | 18 |
| ER positive (n = 113) | 66 | 39 | 27 |
| PR positive (n = 108) | 57 | 37 | 20 |
| HER-2 positive (n = 117) | 54 | 29 | 25 |
| Number of Metastatic Sites | |||
| ID, 1 | 75 | 48 | 27 |
| ≥2 | 55 | 26 | 29 |
| Metastatic sites | |||
| Bone | 65 | 36 | 29 |
| Lung | 41 | 20 | 21 |
| Lymph Node | 42 | 21 | 21 |
| Liver | 21 | 11 | 10 |
| Other | 26 | 14 | 12 |
| HDC regimen | |||
| Mitox, Cyclo, Vin | 35 | 35 | |
| Mitox, Cyclo, Carbo | 29 | 29 | |
| Mitox, Cyclo, Paclitaxel | 56 | 56 | |
| Thiotepa, Cyclo, Carbo | 8 | 8 | |
| Mitox, Cyclo | 2 | 2 |
| Breast Cancer Specific Survival | |||||||||||||||
| Total | Group 1 | Group 2 | |||||||||||||
| Plasma Marker | N | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p | N | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p | N | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p |
| IL-RA1 | 105 | 16.3 vs. 24.9 | 2.08 (1.27–3.40) | 8.5 | 0.0036 | 60 | 14.4 vs. 25.1 | 2.08 (1.14–3.78) | 5.74 | 0.017 | 45 | 18.5 vs. 24.1 | 1.91 (0.781–4.66) | 2.1 | 0.16 |
| IL-1 | 113 | 19.9 vs. 19.6 | 0.87 (0.59–1.28) | 0.5 | 0.48 | 60 | 17.7 vs. 18.8 | 1.04 (0.26–1.75) | 0.2 | 0.88 | 53 | 24.1 vs. 18.6 | 0.67 (0.374–1.22) | 1.7 | 0.19 |
| TNF | 113 | 23.3 vs. 15.6 | 0.63 (0.40–1.00) | 3.8 | 0.05 | 60 | 19.9 vs. 14.3 | 0.65 (0.48–0.92) | 4.85 | 0.028 | 53 | 25.1 vs. 16.0 | 0.82 (0.422–1.61) | 0.32 | 0.57 |
| IL-6 | 94 | 21.4 vs. 17.4 | 0.72 (0.44–1.18) | 1.71 | 0.19 | 54 | 19.9 vs. 13.4 | 0.60 (0.43–0.84) | 6.12 | 0.013 | 40 | 22.9 vs. 29.5 | 1.31 (0.672–2.56) | 0.63 | 0.43 |
| IL-2 | 101 | 22.9 vs. 15.9 | 0872 (0.58–1.32) | 0.41 | 0.52 | 59 | 19.2 vs. 16.8 | 1.10 (0.58–1.69) | 0.0003 | 0.98 | 42 | 27.5 vs. 16.0 | 0.56 (0.283–1.12) | 2.71 | 0.1 |
| Progression free survival | |||||||||||||||
| IL-RA1 | 105 | 8.5 vs. 10.7 | 1.59 (1.01–2.51) | 3.9 | 0.049 | 60 | 8.5 vs. 10.7 | 1.56 (0.89–2.75) | 2.5 | 0.12 | 45 | 8.5 vs. 10.6 | 1.93 (0.74–4.71) | 2.1 | 0.15 |
| IL-1 | 113 | 9.8 vs. 9.3 | 0.81 (0.55–1.19) | 1.2 | 0.28 | 60 | 10.3 vs. 8.3 | 0.89 (0.59–1.56) | 0.19 | 0.67 | 53 | 9.7 vs. 9.3 | 0.82 (0.46–1.44) | 0.48 | 0.48 |
| TNF | 113 | 10.5 vs. 7.2 | 0.52 (0.32–0.83) | 7.3 | 0.0068 | 60 | 10.7 vs. 6.9 | 0.29 (0.14–0.59) | 11.5 | 0.007 | 53 | 10.6 vs. 9.2 | 0.84 (0.43–1.62) | 0.28 | 0.6 |
| IL-6 | 94 | 10.6 vs. 7.2 | 0.60 (0.36–1.01) | 3.8 | 0.052 | 54 | 10.7 vs. 4.7 | 0.29 (0.19–0.57) | 11.5 | 0.007 | 40 | 11.6 vs. 10.1 | 1.00 (0.48–2.08) | 5E-05 | 0.99 |
| IL-2 | 101 | 10.5 vs. 8.9 | 0.81 (0.54–1.23) | 0.97 | 0.32 | 59 | 10.2 vs. 7.4 | 0.77 (0.44–1.33) | 0.82 | 0.25 | 32 | 10.6 vs. 9.0 | 0.83 (0.43–1.58) | 0.33 | 0.57 |
| IL-1RA | IL-1β | IL-2 | IL-6 | |
|---|---|---|---|---|
| TNFα | 0.69 (<0.0001) | 0.79 (<0.0001) | 0.61 (<0.0001) | 0.83 (<0.0001) |
| IL-1RA | 0.68 (<0.0001) | 0.78 (<0.0001) | 0.65 (<0.0001) | |
| IL-1β | 0.74 (<0.0001) | 0.88 (<0.0001) | ||
| IL-2 | 0.64 (<0.0001) |
| Breast Cancer Specific Survival | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Population | Group I | Group 2 | |||||||||||||
| Variable | N | OS | N | OS | N | OS | |||||||||
| 130 | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p | 74 | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p | 56 | Median Survival (Months) | Hazard Ratio (95% CI) | X2 | p | |
| ILRA SNP 1 | 117 | 53 | 53 | ||||||||||||
| CC | 66 | 15.3 | 1 (reference) | 33 | 14.3 | 1 (reference) | 32 | 17.9 | 1 (reference) | ||||||
| CT | 45 | 26.6 | 1.60 (1.10–2.35) | 6 | 0.015 | 26 | 28.5 | 2.22 (1.28–3.84) | 8.1 | 0.004 | 20 | 25.1 | 1.33 (0.76–2.32) | 0.98 | 0.32 |
| TT | 6 | 12.8 | 0.40 (0.13–1.25) | 2.5 | 0.11 | 5 | 9.5 | 0.46 (0.14–1.55) | 1.6 | 0.21 | 1 | 16 | 0.57 (0.004–6.84) | 0.2 | 0.65 |
| CC | 66 | 15.3 | 1 (reference) | 33 | 14.3 | 1 (reference) | 17.9 | 1 (reference) | |||||||
| CT + TT | 51 | 25.3 | 1.46 (1.01–2.12) | 4.1 | 0.043 | 31 | 26.6 | 1.87 (1.11–3.17) | 5.5 | 0.019 | 24.9 | 1.29 (0.74–2.24) | 0.82 | 0.37 | |
| ILRA SNP 2 | 116 | 64 | 53 | ||||||||||||
| TT | 47 | 21.4 | 1 (reference) | 31 | 19.2 | 1 (reference) | 17 | 27.5 | 1 (reference) | ||||||
| CT | 50 | 20.1 | 1.06 (0.70–1.58) | 0.067 | 0.8 | 24 | 25.2 | 1.06 (0.61–1.83) | 0.042 | 0.84 | 26 | 17.1 | 1.09 (0.58–2.05) | 0.74 | 0.79 |
| CC | 19 | 14.4 | 1.44 (0.80–2.58) | 1.48 | 0.5 | 9 | 14.4 | 2.05 (0.82–5.14) | 2.3 | 0.13 | 10 | 20.4 | 1.11 (0.49–2.49) | 0.058 | 0.81 |
| TT | 47 | 21.4 | 1 (reference) | 31 | 19.2 | 1 (reference) | 17 | 27.5 | 1 (reference) | ||||||
| CT+CC | 69 | 18.6 | 1.14 (0.78–1.65) | 0.44 | 0.5 | 33 | 19.9 | 1.21 (0.73–2.00) | 0.53 | 0.46 | 36 | 18.8 | 1.09 (0.61–1.19) | 0.81 | 0.78 |
| TNF SNP | 89 | 57 | 32 | ||||||||||||
| GG | 50 | 14.4 | 1 (reference) | 27 | 14.3 | 1 (reference) | 23 | 15.1 | 1 (reference) | ||||||
| AG | 36 | 18.1 | 0.67 (0.43–1.04) | 3.1 | 0.076 | 27 | 19.2 | 0.59 (0.33–1.05) | 3.2 | 0.074 | 9 | 16 | 1.08 (0.48–2.41) | 0.36 | 0.85 |
| AA | 3 | 31.9 | 0.71 (0.26–1.93) | 0.45 | 0.5 | 3 | 31.9 | 0.70 (0.24–1.99) | 0.45 | 0.5 | 0 | ||||
| GG | 50 | 14.4 | 1 (reference) | 27 | 14.3 | 1 (reference) | |||||||||
| GG+AG | 39 | 18.5 | 0.67 (0.43–1.02) | 4.4 | 0.064 | 30 | 19.5 | 0.59 (0.33–1.03) | 3.5 | 0.063 | |||||
| IL-6 SNP | 117 | 65 | 52 | ||||||||||||
| GG | 47 | 22.9 | 1 (reference) | 27 | 24.8 | 1 (reference) | 20 | 20.8 | 1 (reference) | ||||||
| CG | 53 | 19.2 | 0.89 (0.60–34) | 0.29 | 0.58 | 29 | 19.2 | 0.99 (0.58–1.68) | 0.002 | 0.96 | 24 | 20.4 | 0.77 (0.41–1.44) | 0.68 | 0.41 |
| CC | 17 | 15.8 | 0.90 (0.51–1.58) | 0.13 | 0.71 | 9 | 13.4 | 1.00 (0.45–2.23) | 8E-05 | 0.99 | 8 | 27.8 | 0.78 (0.34–1.77) | 0.36 | 0.55 |
| GG | 47 | 22.9 | 1 (reference) | 27 | 24.8 | 1 (reference) | 20 | 20.8 | 1 (reference) | ||||||
| CG + CC | 70 | 18.9 | 0.89 (0.60–1.29) | 0.39 | 0.53 | 38 | 17.5 | 0.97 (0.59–1.59) | 0.19 | 0.89 | 32 | 22.9 | 0.77 (0.42–1.39) | 0.76 | 0.38 |
| IL-1B SNP1 | 117 | 64 | 53 | ||||||||||||
| CC | 54 | 15.9 | 1 (reference) | 25 | 15 | 1 (reference) | 29 | 16.3 | 1 (reference) | ||||||
| CT | 50 | 25.2 | 1.44 (0.97–2.14) | 3.3 | 0.07 | 31 | 25.7 | 1.68 (0.95–2.97) | 3.2 | 0.073 | 19 | 24.9 | 1.22 (0.68–2.18) | 0.45 | 0.5 |
| TT | 13 | 24.8 | 1.10 (0.60–2.00) | 0.087 | 0.77 | 8 | 25.7 | 1.33 (0.61–2.88) | 0.52 | 0.47 | 5 | 17.3 | 0.95 (0.36–2.53) | 0.009 | 0.93 |
| CC | 54 | 15.9 | 1 (reference) | 25 | 15 | 1 (reference) | 29 | 16.3 | 1 (reference) | ||||||
| CT + TT | 63 | 25.1 | 1.38 (0.93–2.00) | 2.7 | 0.098 | 39 | 25.7 | 1.64 (0.94–2.85) | 3.1 | 0.078 | 24 | 23.9 | 1.16 (0.67–2.01) | 0.28 | 0.6 |
| IL-1B SNP2 | 117 | 62 | 53 | ||||||||||||
| CC | 66 | 19.9 | 1 (reference) | 37 | 21.4 | 1 (reference) | 29 | 18.5 | 1 (reference) | ||||||
| CT | 45 | 21.4 | 0.83 (0.33–2.06) | 0.16 | 0.69 | 24 | 17.1 | 0.89 (0.53–1.51) | 0.18 | 0.67 | 21 | 24.1 | 1.11 (0.63–1.96) | 0.13 | 0.73 |
| TT | 6 | 14.6 | 0.99 (0.67–1.45) | 0.006 | 0.94 | 3 | 15 | 1.32 (0.44–3.85) | 0.25 | 0.62 | 3 | 14.1 | 0.37 (0.072–1.91) | 1.4 | 0.24 |
| CC | 66 | 19.9 | 1 (reference) | 37 | 21.4 | 1 (reference) | 29 | 18.5 | 1 (reference) | ||||||
| CT + TT | 51 | 19.9 | 0.97 (0.67–1.40) | 0.03 | 0.86 | 27 | 16.7 | 0.94 (0.56–1.56) | 0.067 | 0.8 | 24 | 23.1 | 1.03 (0.59–1.78) | 0.009 | 0.92 |
| Survial for the Number of “Risk” Measures of Cytokine | Logrank Test for Trend | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Measure | Outcome | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | chi2 | p |
| Total | Plasma | PFS | 11.5 | 11.1 | 8.7 | 9.7 | 7.6 | 2 | 6.9 | 0.0088 | ||
| BCSS | 28.9 | 19.9 | 13.8 | 13.8 | 23.3 | 5.8 | 6.2 | 0.012 | ||||
| SNP | PFS | 10.8 | 11.6 | 8.6 | 6.9 | 6.2 | 2 | 8.8 | 0.003 | |||
| BCSS | 28.4 | 25.3 | 16.1 | 12.1 | 10.4 | 13.4 | 11.8 | 0.0006 | ||||
| Plasma+SNP | PFS | 19.9 | 10.4 | 9.1 | 10.4 | 8.3 | 9.7 | 6.6 | 5.5 | 4.7 | 0.031 | |
| BCSS | 49 | 25.1 | 19.2 | 22.9 | 14.4 | 20.9 | 12.1 | 9.6 | 7.8 | 0.0051 | ||
| Group 1 | Plasma | PFS | 9.5 | 11.6 | 4.7 | 6.9 | 7.2 | 2 | 9.8 | 0.0001 | ||
| BCCS | 19.6 | 19.9 | 9.5 | 12.1 | 18.8 | 5.8 | 5.4 | 0.02 | ||||
| SNP | PFS | 10.8 | 11.3 | 8.7 | 6.7 | 4.7 | 6.1 | 0.013 | ||||
| BCSS | 28.4 | 26.1 | 17.5 | 10.8 | 7.9 | 8.3 | 0.004 | |||||
| Plasma+SNP | PFS | 27.3 | 10.1 | 9.1 | 12.3 | 9.5 | 4.7 | 6.2 | 5 | 9.2 | 0.0025 | |
| BCSS | 66.9 | 22.5 | 19.2 | 24.8 | 19.6 | 6.8 | 10.4 | 9.2 | 9 | 0.0026 | ||
| Group 2 | Plasma | PFS | 12.6 | 8.5 | 10.6 | 12.9 | 10.2 | - | 0.05 | 0.82 | ||
| BCSS | 30.4 | 18.6 | 14.4 | 15.4 | 29.5 | - | 0.75 | 0.39 | ||||
| SNP | PFS | 9.2 | 1.9 | 6.8 | 8.9 | 7.6 | 14.1 | 0.19 | 0.67 | |||
| BCSS | 16 | 22.9 | 12.4 | 12.3 | 17.7 | 14.1 | 0.7 | 0.4 | ||||
| Plasma+SNP | PFS | 12.4 | 12.8 | 10.5 | 8.3 | 10.6 | 16 | 14.1 | 1 | 0.32 | ||
| BCSS | 31.1 | 34.9 | 20.7 | 14.4 | 29.4 | 41.8 | 14.1 | 0.00008 | 0.99 | |||
| IL-RA1 | IL-1b | TNFa | IL-6 | IL-2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 130 | pos | % | p | pos | % | p | pos | % | p | pos | % | p | pos | % | p | |
| Age | ||||||||||||||||
| <40 | 32 | 18 | 75 | 0.67 | 11 | 42 | 0.53 | 10 | 39 | 0.77 | 6 | 30 | 0.75 | 11 | 48 | 0.81 |
| 40–49 | 66 | 34 | 64 | 25 | 43 | 16 | 28 | 18 | 37 | 20 | 40 | |||||
| 50–59 | 32 | 19 | 70 | 14 | 48 | 7 | 24 | 7 | 30 | 10 | 37 | |||||
| ER | ||||||||||||||||
| Negative | 47 | 25 | 69 | 0.86 | 15 | 36 | 0.44 | 13 | 32 | 0.32 | 11 | 32 | 0.93 | 16 | 43 | 0.67 |
| Positive | 66 | 34 | 67 | 26 | 47 | 13 | 24 | 15 | 33 | 20 | 40 | |||||
| PR | ||||||||||||||||
| Negative | 51 | 28 | 68 | 0.96 | 16 | 40 | 0.43 | 13 | 29 | 0.59 | 14 | 39 | 0.22 | 13 | 37 | 0.28 |
| Positive | 57 | 31 | 70 | 22 | 47 | 12 | 26 | 10 | 26 | 20 | 47 | |||||
| HER-2 (tissue or sHER-2) | ||||||||||||||||
| Negative | 63 | 38 | 69 | 0.75 | 24 | 41 | 0.37 | 16 | 27 | 0.61 | 15 | 30 | 0.48 | 21 | 39 | 0.83 |
| Positive | 54 | 29 | 64 | 25 | 50 | 16 | 32 | 16 | 38 | 19 | 44 | |||||
| Adjuvant endocrine therapy | ||||||||||||||||
| No | 83 | 50 | 71 | 0.11 | 34 | 45 | 0.31 | 23 | 30 | 0.54 | 26 | 41 | 0.001 | 26 | 39 | 0.75 |
| Yes | 44 | 20 | 61 | 14 | 48 | 10 | 28 | 5 | 18 | 15 | 45 | |||||
| Documented Sites of Metastases | ||||||||||||||||
| NED, 1 | 75 | 39 | 65 | 0.48 | 27 | 42 | 0.58 | 15 | 23 | 0.11 | 17 | 31 | 0.71 | 23 | 38 | 0.85 |
| ≥ 2 | 55 | 32 | 73 | 23 | 47 | 18 | 38 | 14 | 37 | 18 | 45 | |||||
| Bone Metastases | ||||||||||||||||
| No | 71 | 53 | 72 | >0.001 | 34 | 42 | 0.25 | 24 | 30 | 0.14 | 22 | 33 | 0.28 | 28 | 37 | 0.32 |
| Yes | 41 | 18 | 58 | 16 | 50 | 9 | 29 | 9 | 36 | 13 | 45 | |||||
| Lung Metastases | ||||||||||||||||
| No | 89 | 47 | 66 | 0.02 | 32 | 42 | 0.04 | 20 | 26 | 0.06 | 23 | 37 | 1.00 | 28 | 41 | 0.29 |
| Yes | 31 | 24 | 73 | 18 | 49 | 13 | 36 | 8 | 28 | 13 | 42 | |||||
| Liver Metastases | ||||||||||||||||
| No | 109 | 56 | 65 | 0.24 | 38 | 40 | 0.08 | 25 | 27 | 0.17 | 26 | 34 | 1.00 | 30 | 37 | 0.04 |
| Yes | 21 | 14 | 78 | 12 | 63 | 8 | 42 | 5 | 33 | 11 | 61 | |||||
| Lymph Node | ||||||||||||||||
| No | 89 | 48 | 70 | 0.85 | 33 | 45 | 0.71 | 21 | 29 | 0.67 | 19 | 31 | 0.38 | 28 | 42 | 0.95 |
| Yes | 42 | 24 | 67 | 17 | 44 | 12 | 31 | 12 | 40 | 13 | 38 | |||||
| Other sites | ||||||||||||||||
| No | 104 | 55 | 66 | 0.51 | 41 | 45 | 0.82 | 29 | 33 | 0.48 | 24 | 32 | 0.80 | 34 | 41 | 0.64 |
| Yes | 26 | 16 | 76 | 9 | 41 | 9 | 41 | 7 | 39 | 7 | 39 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lafrenie, R.; Bewick, M.; Buckner, C.; Conlon, M. Plasma Cytokine Levels and Cytokine Genetic Polymorphisms in Patients with Metastatic Breast Cancer Receiving High-Dose Chemotherapy. Immuno 2023, 3, 16-34. https://doi.org/10.3390/immuno3010002
Lafrenie R, Bewick M, Buckner C, Conlon M. Plasma Cytokine Levels and Cytokine Genetic Polymorphisms in Patients with Metastatic Breast Cancer Receiving High-Dose Chemotherapy. Immuno. 2023; 3(1):16-34. https://doi.org/10.3390/immuno3010002
Chicago/Turabian StyleLafrenie, Robert, Mary Bewick, Carly Buckner, and Michael Conlon. 2023. "Plasma Cytokine Levels and Cytokine Genetic Polymorphisms in Patients with Metastatic Breast Cancer Receiving High-Dose Chemotherapy" Immuno 3, no. 1: 16-34. https://doi.org/10.3390/immuno3010002
APA StyleLafrenie, R., Bewick, M., Buckner, C., & Conlon, M. (2023). Plasma Cytokine Levels and Cytokine Genetic Polymorphisms in Patients with Metastatic Breast Cancer Receiving High-Dose Chemotherapy. Immuno, 3(1), 16-34. https://doi.org/10.3390/immuno3010002







