Abstract
Background and objectives. Symptoms of Attention Deficit Hyperactivity Disorder (ADHD) are frequently present in university students, even without a clinical diagnosis, and may be aggravated by various factors. This study analyzes the relationship between these symptoms and the use of alcohol, tobacco, cannabis, and other drugs by young university students. Materials and methods. A cross-sectional study was conducted with 397 university students using an anonymous online questionnaire. ADHD symptoms were assessed with the Adult ADHD Self-Report Scale (ASRS), alcohol use with the Alcohol Use Disorders Identification Test (AUDIT-C), nicotine dependence with the Fagerström test, cannabis use with the Cannabis Abuse Screening Test (CAST), and the use of other substances with an adaptation of the latter. Results. The mean age was 21.4 years, and most participants (76.6%) were women. Of the participants, 46.1% presented symptoms compatible with ADHD according to the ASRS. The most frequent items were difficulty maintaining attention during boring tasks (77.3%), avoiding tasks that require mental effort (76.8%), and being easily distracted by noise or external activity (73.8%). Significant differences were found between ASRS scores and gender, with scores being higher and more consistent among those students who identified themselves as non-binary gender (male or female) (p < 0.01). A significant association was also found between smoking and a higher ASRS score (p < 0.01). Although no significant associations with body mass index were detected, a trend toward greater symptomatology was observed in obese individuals. In multivariate analysis, still gender and smoking significantly (p = 0.12 and p = 0.031, respectively) predicted ADHD symptoms (ASRS score). The model R = 0.228 (R squared = 0.052, F = 1.62, p = 0.077). No statistically significant differences were found between ADHD symptoms and the use of alcohol, cannabis, or other substances in either bivariate or multivariate analyses. Conclusions. This study underscores the importance of early detection of ADHD symptoms in the university setting, considering factors such as gender and smoking habit. Future research should focus on aggravating factors such as academic stress and problematic technology use.
Keywords:
ADHD; university students; ASRS; substances of abuse; smoking; gender; obesity; mental health 1. Introduction
According to the DSM-V, Attention Deficit Hyperactivity Disorder (ADHD) is characterized by a persistent pattern of inattention and/or hyperactivity–impulsivity that significantly affects the individual’s development and social, academic or occupational functioning [1]. Inattention involves problems maintaining concentration, following instructions, organizing activities, avoiding distractions and remembering daily tasks, which creates difficulties in the daily performance of those tasks. Hyperactivity and impulsivity are also reflected in behaviors such as constant restlessness, difficulty remaining seated, excessive talking, interrupting conversations or activities and an inability to wait turns. These symptoms must be present for at least six months, to a degree that does not correspond to the expected level of development [1].
Several studies have shown that certain external factors can influence the appearance of ADHD-like symptoms in people without a formal diagnosis [2,3]. Symptoms of inattention, impulsivity, and hyperactivity are not exclusive to those diagnosed with ADHD, but may also manifest under specific conditions related to the environment and adopted habits [2,3] even if the clinical criteria for an ADHD diagnosis are not met.
These symptoms have been shown to appear in specific populations, such as university students, whose high academic and social demands create an environment conducive to these characteristics. Difficulties maintaining attention, organizing tasks or regulating behavior become more evident in contexts that require a constant capacity for planning and concentration [2,4].
These manifestations may not be permanent, but they have a significant impact on the performance of those affected [3,4,5,6,7]. For example, impulsive behaviors or attention lapses can interfere with academic performance [3,8,9,10,11] and interpersonal relationships [4,11,12,13], even among people who have presented similar symptoms at other stages in their lives [3,4].
Among the most notable factors that have been associated with the appearance or exacerbation of these symptoms are the abuse of new technologies [14,15,16,17] and substance abuse [18,19]. Recent research has found that these habits not only intensify attention and impulsivity problems, but also create a negative feedback loop in which the capacity for self-regulation is further compromised [2,3]. These behaviors, which are common among university students, could act as key triggers in the manifestation of symptoms [2,3,14,15,16,17,18,19]. Alcohol is one of the most widely consumed substances by university students, and their intensive consumption pattern, known as binge drinking, is of particular concern [20,21,22]. Cannabis, another of the most commonly used substances among university students, is consistently associated with cognitive [23,24] and behavioral deficits [25]. Frequent cannabis use has been shown to be linked to alterations in working memory, sustained attention, and decision-making ability [26,27,28].
Furthermore, cannabis may have a bidirectional effect in this population [20]. On the one hand, people who present symptoms of inattention or impulsivity may use cannabis as a form of self-medication, seeking to relieve stress, although this not only does not resolve the underlying problems, but may exacerbate them [29]. Meanwhile, chronic use of this substance can increase pre-existing symptoms, creating a vicious circle that increases vulnerability to emotional and cognitive difficulties [26,29].
The simultaneous use of alcohol and cannabis, a common practice among university students, has a cumulative effect in exacerbating ADHD-like symptoms [29]. While alcohol primarily affects impulsivity and judgment, cannabis impacts functions such as attention and memory, creating a symptomatic profile that significantly interferes with executive abilities and emotional stability [26].
Although alcohol and cannabis are the most commonly used substances among university students in Spain [30], illicit drugs such as cocaine, amphetamines and non-prescribed stimulants also influence the onset and exacerbation of these symptoms [20,31,32].
A study of European university students taking health sciences courses found that 6.8% had used illicit substances other than alcohol and cannabis [31]. Another study of nursing students at the University of Valencia found that 5.5% of participants admitted to using drugs to “get high” [20]. The use of these illicit substances is linked to impulsive behavior, deficits in inhibitory control, and alterations in attention [29].
The hypothesis posed in this study is that symptoms of inattention and hyperactivity–impulsivity are associated with substance abuse in university students without a prior ADHD diagnosis. The overall objectives are as follows:
- To analyze the relationship between ADHD symptoms and substance abuse in college students.
- To assess whether ADHD symptoms differ by age, gender, type of the knowledge area, body-mass index categories, and the type of substance abuse.
2. Materials and Methods
2.1. Design and Participants
A cross-sectional study with a quantitative approach was conducted to analyze the relationship between substance use and ADHD symptoms in university students.
The study was approved by the Human Research Ethics Committee of the University of Valencia (Spain), ensuring its suitability and compliance with current ethical regulations (protocol 2298864, dated 13 October 2022).
The study involved students enrolled in various university programs during the 2024–2025 academic year. The only inclusion criterion was enrollment in a university program. Exclusion criteria were refusal to participate after being informed about the study objectives, or having been diagnosed with ADHD.
The study used an anonymous digital Google Forms ad hoc questionnaire as the primary data collection tool. The questionnaire began with an informative text setting out the study’s objectives, the importance of participation, and the potential inconvenience associated with completing the questionnaire. The questionnaire included a digital informed consent form, which had to be accepted in order to continue. The questionnaire’s design guaranteed the anonymity of the responses, and contained no identifying information related to the student. Participation was entirely voluntary, with no financial incentives.
2.2. Sociodemographic Data
Sociodemographic data and aspects related to personal and academic background were collected. Variables considered included age, country of residence, gender, weight and height (to calculate the Body Mass Index), and current university degree.
2.3. Assessment of ADHD Symptoms
Behavior and concentration patterns were assessed using the Spanish version of the Adult ADHD Self-Report Scale (ASRS), developed by the World Health Organization (WHO) in collaboration with clinical experts in adult ADHD. The ASRS is a brief screening scale designed to assess symptoms of inattention and hyperactivity–impulsivity according to DSM-IV criteria, and is used in both community and clinical studies [33]. This scale has been validated in Spanish [34].
The ASRS consists of 18 items, each assessing symptoms related to inattention (9 items) and hyperactivity–impulsivity (9 items). Furthermore, the questionnaire distributes its 18 items into two DSM-IV-aligned symptom domains: items 1–4 and 7–11 assess the inattention domain, while items 5–6 and 12–18 are assigned to the hyperactivity/impulsivity domain [35].
The participants responded to the frequency of symptoms over the past six months using a five-category scale: never, rarely, sometimes, often, and very often [1,36].
Section A of the ASRS questionnaire, consisting of six questions, acts as an initial filter to detect potentially relevant symptoms. Accordingly, those who score 4, 5, or 6 points on these questions are considered to be in an alarming situation.
The ASRS has demonstrated strong psychometric properties. Its Cronbach’s alpha was 0.88, indicating high internal consistency, reflecting that the items are highly correlated and consistently measure ADHD symptoms [35]. The Kappa coefficient was 0.76, indicating substantial agreement between ASRS scores and those obtained from a clinician-administered scale [33]. Furthermore, the ASRS showed a sensitivity of 68.7% and a specificity of 99.5%, demonstrating its ability to correctly identify both positive and negative cases [35].
2.4. Evaluation of Alcohol Consumption
Alcohol consumption was assessed using the shortened version of the Alcohol Use Disorders Identification Test (AUDIT-C) [37]. The AUDIT-C is a screening tool composed of three items that assess the frequency and quantity of alcohol consumption, as well as episodes of heavy drinking [38]. Each item is scored from 0 to 4, generating a total score ranging from 0 to 12, with higher scores presenting a greater risk of problematic alcohol use [37]. Although no studies focusing exclusively on the validation of the AUDIT-C in Spanish have been found, one study evaluated its psychometric properties in 1309 university students in Spain [39]. The results confirmed its good internal consistency (α = 0.75) and its ability to detect risky consumption [39]. This scale can therefore be considered valid in Spanish [39].
The AUDIT-C has demonstrated robust psychometric properties in university students. Internal consistency, as measured by Cronbach’s alpha, was 0.76, reflecting acceptable reliability and confirming that the three items are related and consistently measure the same construct [14]. The Spearman–Brown correlation coefficient was used to assess score stability, yielding a value of 0.88, indicating a high positive correlation between the questionnaire halves and therefore stability in the measurements [37].
The Kappa coefficient, used to measure the agreement between the AUDIT-C cut-off points (4/5 and 5/7), was 0.53, indicating moderate agreement. This means that the classifications made with both cut-off points coincide to a reasonable degree, although they are not completely identical [37]. Furthermore, the proposed cut-off points for identifying risky consumption in university students are ≥5 for women and ≥7 for men, which are values that maximize both sensitivity and specificity [38].
2.5. Assessment of Tobacco Use
Smoking was assessed using the Fagerström Test for Nicotine Dependence (FTND), a widely used tool for measuring physical dependence on nicotine. The FTND is a revised version of the Fagerström Tolerance Questionnaire (FTQ), designed to simplify its administration and improve its psychometric validity [40]. This scale has been validated in Spanish [41].
The FTND consists of six items that assess factors such as the number of cigarettes smoked daily, the time elapsed between waking and smoking the first cigarette, and the difficulty abstaining from smoking in situations where it is prohibited. The total score ranges from 0 to 10, with higher scores indicating greater nicotine dependence [40]. In a study of Peruvian university students, a cut-off score of 2.5 was recommended to identify nicotine dependence [42].
The FTND has been shown to be a reliable and valid instrument. Previous studies have shown a Cronbach’s alpha of 0.75, indicating good internal consistency, and that the test items are correlated and consistently measure nicotine dependence [43]. Furthermore, research has found that the test, or its earlier version (FTQ), is significantly correlated with biomarkers of smoking. Exhaled carbon monoxide, with a correlation of r = 0.88, shows that as the FTND score increases, so do levels of this physiological marker [44]. Salivary cotinine levels, with a correlation of r = 0.70, reflect that FTND scores adequately measure physical nicotine use [44].
Although specific sensitivity and specificity values are not reported, these results support the validity of the FTND as a suitable tool for measuring physical dependence on nicotine [40,43].
2.6. Evaluation of Cannabis and Other Substances of Abuse
Harmful substance use was assessed using a questionnaire based on the Cannabis Abuse Screening Test (CAST), an internationally validated tool for detecting problematic cannabis use. Although no studies focused exclusively on the validation of the CAST in Spanish young people were found, one study evaluated its psychometric properties in 241 young cannabis users in Spain [45]. The results confirmed its reliability (α > 0.71) and its ability to detect cannabis use disorders according to the DSM-IV and DSM-V criteria [45]. This scale can therefore be considered validated in Spanish [45].
The CAST consists of six items that assess the frequency of behaviors related to cannabis use in the past 12 months, including use before noon, use when alone, memory problems associated with use, recommendations from friends or family to cut down or quit, unsuccessful attempts to quit, and use-related problems such as fights, accidents, or poor academic performance. The responses are scored on a 5-point Likert scale, ranging from 0 (never) to 4 (very often), yielding a total score ranging from 0 to 24 [46,47].
The CAST has demonstrated good psychometric properties. In a study of patients hospitalized for cannabis use disorders, a sensitivity of 93.0% and a specificity of 66.7% were reported, with a 6-point cut-off point for detecting problematic use according to DSM-IV criteria. For identifying more severe cases, such as cannabis dependence, a 9-point cut-off point showed a specificity of 83.3% [47]. Furthermore, in studies with adolescents, the CAST showed an internal consistency (Cronbach’s alpha) of 0.78, indicating that the test items are related and consistently measure the same construct [46,48].
The questionnaire was adapted to assess the use of other substances, including cocaine, LSD and MDMA, replacing the term “cannabis” with the appropriate substance and maintaining the same structure.
2.7. Statistical Analysis
The data collected from the questionnaires were initially entered into an MS Excel spreadsheet for organization. They were then exported and analyzed using the Jamovi statistical software package (version 2.6.17). The participants’ characteristics were first described by calculating frequencies for categorical variables, as well as measures of central tendency and dispersion (including the mean, range, and standard deviation (SD)) for the continuous variables. For bivariate analysis, the differences between the categorical variables were assessed using Pearson’s chi-square test. The continuous variables were tested for normality using the Shapiro–Wilk test (for n < 50) or the Kolmogorov–Smirnov test (for n > 50). Since the assumption of normality was not met with any of the variables, nonparametric statistical tests were used. In this context, comparisons between groups were performed using the Mann–Whitney U test, the Kruskal–Wallis test, and Spearman’s correlation coefficient. A linear regression model was applied to examine the relationship between ADHD symptoms and independent variables such substance use (nicotine, cannabis, alcohol and other psychostimulants), age, gender, field of study (dichotomized as health sciences versus others) and BMI category. Statistical significance was set at p < 0.05.
3. Results
3.1. Sample Characteristics
The study sample consisted of a total of 397 participants: 314 women, representing 76.6% of the sample; 90 men, constituting 22.0%; and 1.4% identifying with another gender. The participants’ mean age was 21.4 ± 4.7 years (17–50).
For this study, university degree courses were classified into two categories: health sciences (n = 250, 61.0%) and others (n = 160, 39.0%). This categorization enables a comparison of the relationship between patterns of inattention, hyperactivity–impulsivity, and substance abuse based on academic background. Furthermore, 67.2% of the health sciences group were enrolled on the Nursing course (n = 168).
The Body Mass Index (BMI) of the participants presented an average of 22.3 ± 3.2 kg/m2 (14.3–37.0). The BMI of the sample was categorized into four groups according to the established criteria: underweight (BMI < 18.5), normal weight (BMI between 18.5 and 24.9), overweight (BMI between 25 and 29.9) and obesity (BMI ≥ 30) [49]. As a result, 40 people (9.8%) were identified as underweight, 302 people (73.7%) as normal weight, 57 people (13.9%) as overweight, and 11 people (2.7%) as obese.
3.2. Assessment of Inattention and Hyperactivity–Impulsivity Symptoms
The mean total score of the ASRS questionnaire for the 397 participants is 9.5 ± 4.3 (0–18) points. Frequency of responses to ASRS items is reported in Figure 1.
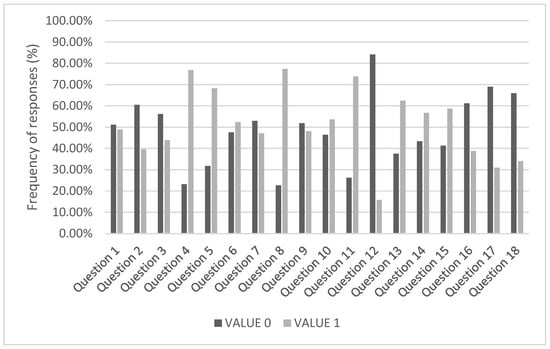
Figure 1.
Frequency of responses to ASRS items among university students, differentiating between “Never” and “Rarely” (value 0, in dark gray) and “Sometimes,” “Often,” and “Very often” (value 1, in light gray). The horizontal axis represents the 18 questions in the questionnaire, while the vertical axis indicates the percentage of responses.
Questions 4 (“When you have to do a task that requires a lot of thinking, how often do you avoid or delay starting it?”), 8 (“How often do you have difficulty maintaining attention when doing boring or repetitive work?”), and 11 (“How often are you distracted by the activity or noise around you?”) have the highest prevalences of positive answer for ADHD symptoms (76.8%, 77.3%, 73.8%, respectively), indicating that these aspects manifest more recurrently. Item 12 (“How often do you leave your seat in meetings or other situations in which you are expected to remain seated?”) has the lowest percentage, with only 15.9% of responses taking the positive answer.
According to the ASRS questionnaire alarm criteria (score ≥ 4 in Section A of the ASRS), 46.1% of students without ADHD present relevant symptoms, while the remaining 53.9% do not present worrying signs.
3.3. Evaluation of the Pattern of Consumption of Substances of Abuse
In our sample, 22.9% of the students are smokers. According to the AUDIT-C questionnaire’s risk criteria, 5.7% engage in risky alcohol use. According to the CAST criteria, 26.2% of students display problematic cannabis use. No students were found to be dependent on the use of marijuana or other drugs of abuse.
3.4. Association Between ADHD Symptoms and Sociodemographic Variables
Statistically significant differences were observed between the ASRS Section A score and gender (p = 0.019, Kruskal–Wallis test), as well as with the total questionnaire score (p = 0.004, Kruskal–Wallis test) and gender (Figure 2).
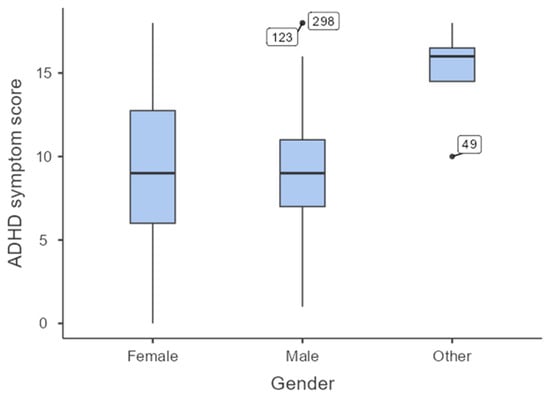
Figure 2.
Distribution of total ASRS scores by gender. The box plots show the median, interquartile range, and outliers by gender.
Figure 2 shows differences in the distribution of the total ASRS questionnaire score by gender. The “Other” group includes those students which identify themselves as both male and female at one time, as different genders at different times, as no gender at all, or dispute the very idea of only two genders.
On the other hand, no statistically significant differences were observed between age and the scores obtained in Section A (p = 0.098, Mann–Whitney U test) and in the total ASRS score (rho = 0.096, p = 0.052, Spearman correlation test).
No significant differences were observed when comparing the knowledge area with the scores obtained in Section A of the questionnaire (p = 0.360, Pearson Chi Square test) and the total ASRS score (p = 0.942, Kruskal–Wallis test).
Significant differences were observed between the categorized BMI and the total ASRS score (p = 0.036, Kruskal–Wallis test) (Figure 3).
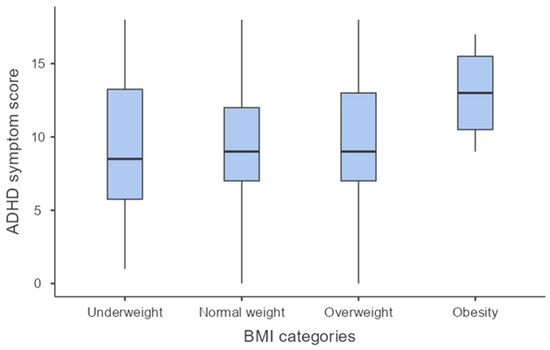
Figure 3.
Distribution of total ASRS scores by BMI category. Box plots show the median, interquartile range, and outliers.
3.5. Association Between ADHD Symptoms and Substance Abuse
Next, we analyzed the associations between ADHD symptoms and each type of substance abuse.
Two variables derived from the ASRS questionnaire were used to study the relationship between smoking and ADHD symptoms in this part of the sample: alarm activation in Section A and the total score. The results were therefore not statistically significant for the relationship between smoking and alarm activation in Section A of the questionnaire (p = 0.226, Pearson’s Chi-square test). In contrast, the results were significant when comparing the total ASRS score between smokers and non-smokers (p = 0.008, Mann–Whitney U test) (Figure 4).
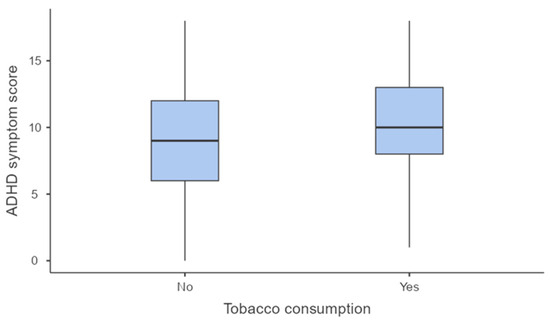
Figure 4.
Distribution of ASRS total scores for smokers and non-smokers. The median, interquartile range, and outliers are shown for the two groups.
The possible relationship between alcohol consumption and ADHD symptoms in the previously undiagnosed population was analyzed, considering both the alarm activation in Section A of the ASRS questionnaire and the total score. The results were not statistically significant in either case (p = 0.570, Pearson’s chi-square test and p = 0.850, Mann–Whitney U test, respectively).
The relationship between problematic alcohol use identified by the AUDIT-C questionnaire and the same ASRS variables was also examined. The association with both the ASRS alarm (p = 0.814, Pearson’s chi-square test) and the total score (p = 0.890, Mann–Whitney U test) of the questionnaire was not significant.
Marijuana use was compared with two ASRS variables: the presence of alarm symptoms in Section A, and the total score. The results were not statistically significant in either case (p = 0.107, Pearson’s chi-square test and p = 0.100, Mann–Whitney U test, respectively). No clear relationship between marijuana use and an increased risk of ADHD symptoms can therefore be established in this sample.
For addictive substances other than marijuana, no statistically significant differences were found between their consumption and the presence of alarm in section A (p = 0.072, Pearson Chi Square test), or with the total ASRS score (p = 0.758, Mann–Whitney U test).
In the sample analyzed, no statistically significant differences were found between ASRS indicators and the type of marijuana use. The presence of alarm in section A of the questionnaire did not show a significant association with problematic use (p = 0.216, Pearson chi-square test) or with dependent use (p = 0.167, Pearson chi-square test). Likewise, the total ASRS score was not significantly associated with problematic use (p = 0.295, Mann–Whitney U test) or dependent use (p = 0.123, Mann–Whitney U test).
In the case of problematic use of addictive substances other than marijuana, no statistically significant differences were observed for the ASRS questionnaire indicators. Neither the presence of alarm in section A (p = 0.262, Pearson’s chi-square test) nor the total questionnaire score (p = 0.187, Mann–Whitney U test) showed any significant association with this type of use. No analysis of dependent use was performed, as no individuals without ADHD in the sample reported this level of use.
In order to confirm the association between ADHD symptoms and the investigated variables A linear regression model was applied to examine the relationship between ADHD symptoms (ASRS score) as dependent variable and the independent variables that have led to significant results in bivariate analyses. As shown in Table 1, gender and smoking significantly (p = 0.12 and p = 0.031, respectively) predicted ADHD symptoms (ASRS score). The model R = 0.228 (R squared = 0.052, F = 1.62 (gl1 = 13, Gl2 383) p = 0.077).

Table 1.
Linear regression analysis predictor of ADHD symptoms (ASRS score).
4. Discussion
In our study, 46.1% of students without a previous diagnosis of ADHD scored ≥4 points in Part A of the ASRS questionnaire, indicating the presence of relevant symptoms in almost half of the university students. Although this result does not constitute a diagnostic DAHD criterion in itself, as the diagnosis must be performed by a qualified healthcare professional, it does indicate the presence of significant symptoms that warrant clinical evaluation as the students with a high burden of symptoms could benefit from a formal assessment to determine whether they meet the diagnostic criteria for the disorder and, if appropriate, receive appropriate pharmacological and non-pharmacological therapeutic interventions to improve their academic, social, and emotional functioning.
In our context in Spain, the pioneer study by Rodríguez Molinero et al. (2009) in Spain using a big sample of 1095 schoolchildren aged 6 to 16 years reported “suspected” ADHD with a prevalence of 6.7%, and 6.5% in secondary school students [50]. A systematic review and meta-analysis of 14 cross-sectional observational studies in the Spanish child and adolescent population (n = 13,026; <18 years) found an overall prevalence of ADHD of 6.8% [51].
In our study, the ASRS items with the most affirmative responses in the population were items 4, 8, and 11, all of which fall into the inattention domain. This pattern is consistent with the structure of the ASRS v1.1, which places items 1–4 and 7–11 in the inattention domain and items 5–6 and 12–18 in the hyperactivity/impulsivity domain [35].
This predominance of inattention symptoms was also observed by Garnier-Dykstra et al. (2010) [52], who assessed 1080 students (972 without ADHD, 54 diagnosed without pharmacological treatment, and 54 diagnosed and medicated) using the ASRS. Inattention symptoms were more prevalent than hyperactivity symptoms in all three subgroups [52].
Gender analysis of the population without diagnosed ADHD showed statistically significant differences in ASRS scores for both Section A and the total score. The “Other” group had a higher mean and less dispersion, which could suggest greater symptomatology.
In comparison with other studies, the work of Gómez-Benito et al. (2015) with a sample of 902 young people from Spain and the United States using the CAARS scale (Caterino’s Adult ADHD Rating Scale) found no significant differences between men and women in the Spanish subsample, although they did find them in the American subsample, in which men scored higher [53].
This is similar to the ADORE study (Attention-Deficit/Hyperactivity Disorder Observational Research in Europe), a longitudinal study conducted in 10 European countries that included 1478 children aged 6–18 years with ADHD symptoms without prior ADHD diagnosis [54]. The results showed that the female gender suffered more emotional symptoms and greater prosocial behavior, while the male gender scored higher for hyperactivity and inattention [54].
Rucklidge [55] conducted a narrative review of the literature published to date on ADHD and gender. Most of the studies reviewed used screening instruments based on the DSM-IV diagnostic criteria and standardized scales such as the Conners’ Rating Scale or the ADHD Rating Scale-IV [55].
Considering symptoms by gender, the review concluded that boys with ADHD tend to present more frequently with symptoms of hyperactivity and impulsivity, while girls tend to manifest predominantly inattentive symptoms. This pattern was observed in both childhood and adulthood. The study also notes that girls with ADHD present higher levels of internalizing problems such as anxiety and depression, while boys display more externalizing behaviors such as aggression and conduct disorders.
Interestingly, none of the three studies consider a gender category other than “Male” or “Female” which could limit the ability to analyze the diversity of identities that can influence the manifestation and perception of ADHD symptoms.
Regarding the effects of gender differences on ADHD symptoms, our results are in line with several others performed in younger students where transgender and gender diverse (TGD) individuals had a higher prevalence of ADHD compared to the cisgender population ([56] for review). Becerra-Culqui et al. (2018), reported taht TGD adolescents were 4.7 to 12.6 times more likely to be diagnosed with ADHD than their cisgender peers [57].
Kuper et al. (2019) pointed out that adolescents with TGD reported more ADHD symptoms than those perceived by their parents, which could indicate underreporting by their environment or an underestimation of their discomfort [58].
The study by Hartung et al. (2025), with a sample of young adults, analyzed the symptoms of ADHD and internalizing disorders as a function of sex, gender identity, and sexual orientation [59]. Three groups were compared, e.g., heterosexual cisgender women, heterosexual cisgender men, and people with non-normative gender identities and sexual orientations. The results showed that the latter group had significantly higher scores for ADHD symptoms than the cisgender groups [59]. Ignatova et al. (2025) examined the relationship between gender identity and ADHD symptoms in a representative sample (10,277 adolescents aged 11 to 15 years) of American adolescents [60].
The results showed that both the transgender (1% of sample) and gender-questioning (1.1% of the sample) groups reported higher ADHD symptom scores than the cisgender adolescents. However, the association was no longer statistically significant after adjusting for stress and depression, which suggests that these factors may mediate the relationship between gender identity and ADHD symptoms. In our study, we have not evaluated these comorbid symptoms and the mediation role of depressive and stress symptoms on ADHD symptoms need to be evaluated in the future.
This difference could be influenced, at least in part, by factors such as minority stress, stigmatization, and clinical underdiagnosis. Our findings reinforce this line of research, and provide preliminary evidence from a university sample that includes gender identities beyond the traditional gender binary.
Regarding BMI categories, we observed a trend towards higher ADHD symptoms in students with obesity. Cortese et al. [61] conducted a systematic review and meta-analysis to estimate the association between ADHD and obesity. Forty-two studies were included, with a total of 728,136 participants, of whom 48,161 had ADHD. The diagnostic criteria used included both DSM-based clinical interviews and validated symptom scales and diagnostic self-reports [61]. The study found a significantly higher prevalence of obesity in adults with ADHD (28.2%) compared to those without (16.4%) [61]. Binge eating disorder partly explained this association, suggesting that problems with emotional regulation and impulse control may underlie the link between ADHD and excess weight [62,63] being women more vulnerable compared to men [64]. An overall prevalence of ADHD of 27.4%, which increased to 42.6% has been found among individuals with extreme obesity (BMI ≥ 40) [65].
Despite the fact that substance use, especially alcohol and cannabis, is significantly linked to the development of ADHD-like symptoms in college students [26], our results support previous studies’ results [2,66,67] that reported inconclusive findings relating ADHD to drug and alcohol use. These equivocal findings may be related to the high comorbidity of ADHD and conduct problems, such as oppositional defiant disorder (ODD) or conduct disorder (CD), as upward of 30% of individuals with ADHD also have ODD or CD and these individuals often have the most deleterious outcomes [68]. Despite this high comorbidity, few studies have controlled for CD/ODD when examining ADHD and substance use, and confusion about the relative contributions of ADHD and CD/ODD to substance use remain. Thus, additional research examining whether ADHD symptoms confer increased risk for substance use beyond the effects of CD/ODD is warranted. Future studies examining ADHD symptoms and illicit drug use should include comorbid symptoms and assess illicit drug use in greater depth (e.g., current vs. lifetime use, quantity/frequency of illicit drug use among college students (smoking cigarettes is performed on a daily base while alcohol drinking and other illicit drugs can be performed either on daily base or during the weekends). The analyses of these variables would help to explain apparent discrepancies between ADHD symptoms as a continuous variable versus students with established clinical diagnosis of ADHD and illicit drug of abuse (daily versus weekend pattern of exposure).
Finally, the relationship between smoking and ADHD symptoms was explored. Although no significant differences were found in ASRS alarm activation, they were found in the total ASRS score, which was higher in smokers.
A study performed in 8110 university students aged 18–30 analyzed reported that 26.5% of students with elevated ADHD symptoms smoked more than 10 cigarettes per day, compared to only 14.5% of those who did not present those symptoms. This difference was especially clear in cases with a predominance of inattention symptoms, compared to those of hyperactivity or impulsivity [69].
In the study by Zamboni et al. [70] the relationship between smoking and ADHD symptoms was assessed in a sample of 389 young adults aged 18–22 years from 14 schools in Northern Italy. The research used a self-administered questionnaire that included sociodemographic questions, questions on substance use and gambling behaviors, as well as the ASRS v1.1 scale (Section A only, six items), establishing a cut-off point of ≥4 points to consider the presence of symptoms compatible with ADHD [70].
The results revealed that 15.2% of the sample scored positive on the ASRS, and that smokers were twice as likely to reach this threshold compared to non-smokers. Furthermore, this association was statistically significant, both for the number of cigarettes smoked per day (especially among those who smoked between 1 and 10 cigarettes per day) and among those who had been smoking for more than a year.
The reported association between ADHD symptoms and smoking could also be due to other mediating factors such as trait impulsivity and baseline anxiety and depressive symptoms that have been previously reported to mediate the relationship between ADHD symptoms and various outcomes [71,72,73]. Previously reported, inattention is associated with an increased risk of depression as a direct effect, as well as slightly increased risk of smoking/drinking behaviors by an indirect effect of depression [73]. Anxiety can mediate the impact of ADHD symptoms on functional impairment and even contribute to the development of comorbid conditions [74]. Hyperactivity–impulsivity symptoms have a significant impact on smoking and drinking behaviors, while being mediated by anxiety and depression [73]. In addition, impulsivity can influence behaviors like substance use and social media engagement [75,76,77].
This study had limitations that could be taken into account and that limits generalization of these results. First, given that we used self-administered questionnaires, there is a risk of selection bias in this study. Specifically, students who choose to participate may possess characteristics that differ from those of students who decline to participate. To mitigate this bias, we encouraged open participation by ensuring that all responses would be anonymous and confidential. Additionally, to avoid temporal bias, we refrained from conducting the study during examination periods and opted for calm periods instead (November-December and February). This approach allowed us to reduce the impact of varying academic stressors that may arise during exams’ period. The complex interplay between ADHD symptoms and substance abuse were not controlled by other possible intervening factors such as psychopathological comorbidity or clinical diagnosis, and socioeconomic status which need explored in future studies. Even the data about the use of “other drugs” did not lead to any significant results in terms of its association with ADHD symptoms, we should take into account as a limitation of the study, that the use of CAST adapted for other drugs, besides cannabis, represents a limitation as it lacks psychometric validation (reliability and validity). Finally, the cross-sectional design of the study cannot allow to infer about causal relationship among ADHD symptoms and substance abuse and thus, requires future longitudinal studies.
5. Conclusions
In conclusion, a considerable proportion of university students present symptoms consistent with ADHD, highlighting the urgent need to strengthen screening and early detection mechanisms in the academic environment. Given that these symptoms appear to be influenced by factors such as gender, smoking, and nutritional status, addressing them cannot be limited to the individual level, but must instead be framed within a comprehensive approach to public health. As key spaces for the young people’s education and well-being, universities should incorporate structured prevention programs, psychological support, and mental health education, paying special attention to their students’ gender diversity and lifestyles. In parallel, future research should focus on identifying modifiable risk factors that foster the persistence or worsening of these symptoms, including the impact of academic stress and the intensive use of digital technologies.
Author Contributions
Conceptualization, D.I.-T. and O.C.; methodology, D.I.-T.; formal analysis, D.I.-T.; research, D.I.-T. and O.C.; data collection, D.I.-T. and O.C.; writing: preparation of the original draft, D.I.-T.; writing: review and editing, O.C.; supervision, O.C. All authors have read and agreed to the published version of the manuscript.
Funding
The study received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Human Research Ethics Committee of the University of Valencia (Spain) (protocol 2298864, dated 13 October 2022).
Informed Consent Statement
Informed consent was obtained from all subjects participating in the study.
Data Availability Statement
The data used to support this study’s findings are available by contacting the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- DSM-5. Manual Diagnóstico y Estadístico de los Trastornos Mentales|España. Available online: https://www.medicapanamericana.com/es-ES/libros/dsm-5-manual-diagnostico-y-estadistico-de-los-trastornos-mentales (accessed on 19 January 2025).
- Glass, K.; Flory, K. Are Symptoms of ADHD Related to Substance Use among College Students? Psychol. Addict. Behav. 2012, 26, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.; Rouchy, E.; Galéra, C.; Tzourio, C.; Michel, G. The Relation between ADHD Symptoms, Perceived Stress and Binge Drinking in College Students. Psychiatry Res. 2020, 284, 112689. [Google Scholar] [CrossRef] [PubMed]
- Bidwell, L.C.; Henry, E.A.; Willcutt, E.G.; Kinnear, M.K.; Ito, T.A. Childhood and Current ADHD Symptom Dimensions Are Associated with More Severe Cannabis Outcomes in College Students. Drug Alcohol Depend. 2014, 135, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Küpper, T.; Haavik, J.; Drexler, H.; Ramos-Quiroga, J.A.; Wermelskirchen, D.; Prutz, C.; Schauble, B. The Negative Impact of Attention-Deficit/Hyperactivity Disorder on Occupational Health in Adults and Adolescents. Int. Arch. Occup. Environ. Health 2012, 85, 837–847. [Google Scholar] [CrossRef]
- Schein, J.; Cloutier, M.; Gauthier-Loiselle, M.; Bungay, R.; Guerin, A.; Childress, A. Symptoms Associated with ADHD/Treatment-Related Adverse Side Effects and Their Impact on Quality of Life and Work Productivity in Adults with ADHD. Curr. Med. Res. Opin. 2023, 39, 149–159. [Google Scholar] [CrossRef]
- Stewart, C.M.; Master, A.; Mire, S.S.; Hassett, K.S.; Smith, B.H. Perceptions of Academic Performance, Impairment, and Mental Health in University Students With and Without ADHD. J. Atten. Disord. 2024, 28, 1746–1759. [Google Scholar] [CrossRef]
- Torres Sandoya, N.G. TDAH Y Su Incidencia en El Rendimiento Académico de Estudiantes de la Ue Francisco Huerta Rendón, Babahoyo.2022. Bachelor’s Thesis, Universidad Técnica de Babahoyo, Babahoyo, Ecuador, 2023. [Google Scholar]
- González-Maya, M.V. La Alteración en las Funciones Ejecutivas en el TDAH y su Relación con el Rendimiento Académico. Master’s Thesis, Universidad Internacional de La Rioja, Logroño, Spain, 2015. [Google Scholar]
- Aravena, C.; Román, S.; Rossi, A.; Sepúlveda, A. Efecto de las funciones ejecutivas en el rendimiento académico de niños/as con trastorno por déficit de atención con hiperactividad: Una revisión sistemática. CienciAmérica 2025, 14, 1–17. [Google Scholar] [CrossRef]
- Ortiz León, S.; Jaimes Medrano, A.L.; Ortiz León, S.; Jaimes Medrano, A.L. Trastorno por déficit de atención en la edad adulta y en universitarios. Rev. Fac. Med. 2016, 59, 6–14. [Google Scholar]
- Pardos, A.; Fernández-Jaén, A.; Fernández-Mayoralas, D.M. Social skills in attention deficit hyperactivity disorder. Rev. Neurol. 2009, 48 (Suppl. 2), S107–S111. [Google Scholar] [CrossRef]
- Sacchetti, G.M.; Lefler, E.K. ADHD Symptomology and Social Functioning in College Students. J. Atten. Disord. 2017, 21, 1009–1019. [Google Scholar] [CrossRef]
- Small, G.W.; Lee, J.; Kaufman, A.; Jalil, J.; Siddarth, P.; Gaddipati, H.; Moody, T.D.; Bookheimer, S.Y. Brain Health Consequences of Digital Technology Use. Dialogues Clin. Neurosci. 2020, 22, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.J.; Cho, S.C.; Ha, J.; Yune, S.K.; Kim, S.J.; Hwang, J.; Chung, A.; Sung, Y.H.; Lyoo, I.K. Attention Deficit Hyperactivity Symptoms and Internet Addiction. Psychiatry Clin. Neurosci. 2004, 58, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Andreassen, C.S.; Billieux, J.; Griffiths, M.D.; Kuss, D.J.; Demetrovics, Z.; Mazzoni, E.; Pallesen, S. The Relationship between Addictive Use of Social Media and Video Games and Symptoms of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. Psychol. Addict. Behav. 2016, 30, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Yen, J.-Y.; Ko, C.-H.; Yen, C.-F.; Wu, H.-Y.; Yang, M.-J. The Comorbid Psychiatric Symptoms of Internet Addiction: Attention Deficit and Hyperactivity Disorder (ADHD), Depression, Social Phobia, and Hostility. J. Adolesc. Health 2007, 41, 93–98. [Google Scholar] [CrossRef]
- Gudjonsson, G.H.; Sigurdsson, J.F.; Sigfusdottir, I.D.; Young, S. An Epidemiological Study of ADHD Symptoms among Young Persons and the Relationship with Cigarette Smoking, Alcohol Consumption and Illicit Drug Use. J. Child Psychol. Psychiatry 2012, 53, 304–312. [Google Scholar] [CrossRef]
- Kalbag, A.S.; Levin, F.R. Adult ADHD and Substance Abuse: Diagnostic and Treatment Issues. Subst. Use Misuse 2005, 40, 1955–1981. [Google Scholar] [CrossRef]
- Tejedor-Cabrera, C.; Cauli, O. Alcohol and Cannabis Intake in Nursing Students. Medicina 2019, 55, 628. [Google Scholar] [CrossRef]
- Jones, S.A.; Lueras, J.M.; Nagel, B.J. Effects of Binge Drinking on the Developing Brain. Alcohol Res. 2018, 39, 87–96. [Google Scholar]
- Harris, J.S.; Stewart, D.G.; Krzyzaniak, S.L.; Charuhas, J.P.; Moon, K.C.; Holdren, A.L.; Manuel, J.A.; Davis, C.L.; Joy, S.A. Binge Drinking Despite Consequences: The Role of Psychological Dysregulation. J. Child Adolesc. Subst. Abuse 2017, 26, 103–110. [Google Scholar] [CrossRef]
- Bourque, J.; Potvin, S. Cannabis and Cognitive Functioning: From Acute to Residual Effects, From Randomized Controlled Trials to Prospective Designs. Front. Psychiatry 2021, 12, 596601. [Google Scholar] [CrossRef]
- Scott, J.C.; Slomiak, S.T.; Jones, J.D.; Rosen, A.F.G.; Moore, T.M.; Gur, R.C. Association of Cannabis With Cognitive Functioning in Adolescents and Young Adults: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2018, 75, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Cortés, M.E.; Veloso, B.C.; Cortés, M.E.; Veloso, B.C. Alteraciones Conductuales En Adolescentes Que Consumen Cannabis y Motivos de Su Consumo. Rev. Méd. Chile 2020, 148, 1696–1697. [Google Scholar] [CrossRef] [PubMed]
- Mochrie, K.D.; Whited, M.C.; Cellucci, T.; Freeman, T.; Corson, A.T. ADHD, Depression, and Substance Abuse Risk among Beginning College Students. J. Am. Coll. Health 2020, 68, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Cano, R.A.; Rubio, M.J.G.; Sánchez, I.C.M. Efectos del cannabis en una muestra universitaria: Atención, memoria, creatividad y ansiedad. Int. J. Dev. Educ. Psychol. 2011, 5, 123–132. [Google Scholar]
- Verdejo-García, A. Efectos Neuropsicológicos Del Consumo de Cannabis. Trastor. Adict. 2011, 13, 97–101. [Google Scholar] [CrossRef]
- Chamberlain, S.R.; Lust, K.; Grant, J.E. Cocaine Use in University Students: Relationships with Demographics, Mental Health, Risky Sexual Practices, and Trait Impulsivity. CNS Spectr. 2021, 26, 501–508. [Google Scholar] [CrossRef]
- Martín-Montañez, E.; Barón-López, F.J.; Rubio Lamia, L.O.; Pavía Molina, J.; Miranda Páez, J.; Santos Amaya, I.M. Consumo de alcohol, tabaco, cannabis y otras sustancias psicoactivas en estudiantes de la Universidad de Málaga. Trastor. Adict. 2011, 13, 160–166. [Google Scholar] [CrossRef]
- Colomer-Pérez, N.; Chover-Sierra, E.; Navarro-Martínez, R.; Andriusevičienė, V.; Vlachou, E.; Cauli, O. Alcohol and Drug Use in European University Health Science Students: Relationship with Self-Care Ability. Int. J. Environ. Res. Public Health 2019, 16, 5042. [Google Scholar] [CrossRef]
- Ohlmeier, M.D.; Peters, K.; Wildt, B.T.T.; Zedler, M.; Ziegenbein, M.; Wiese, B.; Emrich, H.M.; Schneider, U. Comorbilidad de la Dependencia a Alcohol y Drogas y el Trastorno por Déficit de Atención e Hiperactividad (TDAH); Universidad de La Rioja: Logroño, Spain, 2009. [Google Scholar]
- Adler, L.A.; Spencer, T.; Faraone, S.V.; Kessler, R.C.; Howes, M.J.; Biederman, J.; Secnik, K. Validity of Pilot Adult ADHD Self- Report Scale (ASRS) to Rate Adult ADHD Symptoms. Ann. Clin. Psychiatry 2006, 18, 145–148. [Google Scholar] [CrossRef]
- Ramos-Quiroga, J.A.; Daigre Blanco, C.; Valero, S.; Bosch Munsó, R.; Nogueira, G.; Palomar, G.; Gómez Barros, N.; Roncero, C.; Casas Brugué, M. Validación al español de la escala de cribado del trastorno por déficit de atención/hiperactividad en adultos (ASRS v. 1.1): Una nueva estrategia de puntuación. Rev. Neurol. 2009, 48, 449–452. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.; Ames, M.; Demler, O.; Faraone, S.; Hiripi, E.; Howes, M.J.; Jin, R.; Secnik, K.; Spencer, T.; et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): A Short Screening Scale for Use in the General Population. Psychol. Med. 2005, 35, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Ustun, B.; Adler, L.A.; Rudin, C.; Faraone, S.V.; Spencer, T.J.; Berglund, P.; Gruber, M.J.; Kessler, R.C. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry 2017, 74, 520–527. [Google Scholar] [CrossRef]
- Barry, A.E.; Chaney, B.H.; Stellefson, M.L.; Dodd, V. Evaluating the Psychometric Properties of the AUDIT-C among College Students. J. Subst. Use 2015, 20, 1–5. [Google Scholar] [CrossRef]
- Campbell, C.E.; Maisto, S.A. Validity of the AUDIT-C Screen for at-Risk Drinking among Students Utilizing University Primary Care. J. Am. Coll. Health 2018, 66, 774–782. [Google Scholar] [CrossRef] [PubMed]
- García Carretero, M.A. Validación del Test Para la Identificación de Trastornos por Uso de Alcohol (Audit) en Población Universitaria: Resultados de la Versión Breve (Audit-C) y Completa (Audit); Universidad de Cádiz: Cádiz, Spain, 2013; Available online: http://purl.org/dc/dcmitype/Text (accessed on 2 May 2025).
- Fagerstrom, K.O.; Schneider, N.G. Measuring Nicotine Dependence: A Review of the Fagerstrom Tolerance Questionnaire. J. Behav. Med. 1989, 12, 159–182. [Google Scholar] [CrossRef]
- Becoña, E.; Vázquez, F.L. The Fagerström Test for Nicotine Dependence in a Spanish Sample. Psychol. Rep. 1998, 83, 1455–1458. [Google Scholar] [CrossRef]
- Arias-Gallegos, W.L.; Huamani-Cahua, J.C.; Choque-Vera, R. Análisis Psicométrico Del Test de Fagerström de Dependencia a La Nicotina En Una Muestra de Estudiantes Universitarios de Arequipa, Perú. Acta Méd. Peru. 2018, 35, 174–179. [Google Scholar] [CrossRef]
- Nonnemaker, J.M.; Homsi, G. Measurement Properties of the Fagerström Test for Nicotine Dependence Adapted for Use in an Adolescent Sample. Addict. Behav. 2007, 32, 181–186. [Google Scholar] [CrossRef]
- Etter, J.F.; Duc, T.V.; Perneger, T.V. Validity of the Fagerström Test for Nicotine Dependence and of the Heaviness of Smoking Index among Relatively Light Smokers. Addiction 1999, 94, 269–281. [Google Scholar] [CrossRef]
- Cuenca-Royo, A.M.; Sánchez-Niubó, A.; Forero, C.G.; Torrens, M.; Suelves, J.M.; Domingo-Salvany, A. Psychometric Properties of the CAST and SDS Scales in Young Adult Cannabis Users. Addict. Behav. 2012, 37, 709–715. [Google Scholar] [CrossRef]
- Legleye, S.; Piontek, D.; Kraus, L. Psychometric Properties of the Cannabis Abuse Screening Test (CAST) in a French Sample of Adolescents. Drug Alcohol Depend. 2011, 113, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Legleye, S.; Kraus, L.; Piontek, D.; Phan, O.; Jouanne, C. Validation of the Cannabis Abuse Screening Test in a Sample of Cannabis Inpatients. Eur. Addict. Res. 2012, 18, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Royo, A.M.C.; Niubò, A.S.; Melich, M.T.; Joanxich, J.M.S.; Salvany, A.D. La entrevista Cannabis Abuse Screening Test (CAST) para el diagnóstico de trastornos psiquiátricos en jóvenes consumidores de cannabis. Adicciones Rev. Socidrogalcohol 2013, 25, 87–88. [Google Scholar] [CrossRef]
- Manuel Moreno, G. Definición y clasificación de la obesidad. Rev. Med. Clin. Condes 2012, 23, 124–128. [Google Scholar] [CrossRef]
- Rodríguez Molinero, L.; López Villalobos, J.A.; Garrido Redondo, M.; Sacristán Martín, A.M.; Martínez Rivera, M.T.; Ruiz Sanz, F. Estudio Psicométrico-Clínico de Prevalencia y Comorbilidad Del Trastorno Por Déficit de Atención Con Hiperactividad En Castilla y León (España). Pediatr. Atenc. Prim. 2009, 11, 251–270. [Google Scholar] [CrossRef][Green Version]
- Catalá-López, F.; Peiró, S.; Ridao, M.; Sanfélix-Gimeno, G.; Gènova-Maleras, R.; Catalá, M.A. Prevalence of Attention Deficit Hyperactivity Disorder among Children and Adolescents in Spain: A Systematic Review and Meta-Analysis of Epidemiological Studies. BMC Psychiatry 2012, 12, 168. [Google Scholar] [CrossRef]
- Garnier-Dykstra, L.M.; Pinchevsky, G.M.; Caldeira, K.M.; Vincent, K.B.; Arria, A.M. Self-Reported Adult Attention-Deficit/Hyperactivity Disorder Symptoms among College Students. J. Am. Coll. Health 2010, 59, 133–136. [Google Scholar] [CrossRef]
- Gómez-Benito, J.; Van de Vijver, F.J.R.; Balluerka, N.; Caterino, L. Cross-Cultural and Gender Differences in ADHD Among Young Adults. J. Atten. Disord. 2019, 23, 22–31. [Google Scholar] [CrossRef]
- Nøvik, T.S.; Hervas, A.; Ralston, S.J.; Dalsgaard, S.; Rodrigues Pereira, R.; Lorenzo, M.J.; ADORE Study Group. Influence of Gender on Attention-Deficit/Hyperactivity Disorder in Europe-ADORE. Eur. Child Adolesc. Psychiatry 2006, 15 (Suppl. 1), I15–I24. [Google Scholar] [CrossRef]
- Rucklidge, J.J. Gender Differences in Attention-Deficit/Hyperactivity Disorder. Psychiatr. Clin. N. Am. 2010, 33, 357–373. [Google Scholar] [CrossRef]
- Goetz, T.G.; Adams, N. The Transgender and Gender Diverse and Attention Deficit Hyperactivity Disorder Nexus: A Systematic Review. J. Gay Lesbian Ment. Health 2024, 28, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Becerra-Culqui, T.A.; Liu, Y.; Nash, R.; Cromwell, L.; Flanders, W.D.; Getahun, D.; Giammattei, S.V.; Hunkeler, E.M.; Lash, T.L.; Millman, A.; et al. Mental Health of Transgender and Gender Nonconforming Youth Compared With Their Peers. Pediatrics 2018, 141, e20173845. [Google Scholar] [CrossRef] [PubMed]
- Kuper, L.E.; Mathews, S.; Lau, M. Baseline Mental Health and Psychosocial Functioning of Transgender Adolescents Seeking Gender-Affirming Hormone Therapy. J. Dev. Behav. Pediatr. 2019, 40, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Hartung, C.M.; Lefler, E.K.; Abu-Ramadan, T.M.; Stevens, A.E.; Serrano, J.W.; Miller, E.A.; Shelton, C.R. A Call to Analyze Sex, Gender, and Sexual Orientation in Psychopathology Research: An Illustration with ADHD and Internalizing Symptoms in Emerging Adults. J. Psychopathol. Behav. Assess. 2025, 47, 18. [Google Scholar] [CrossRef]
- Ignatova, E.; Balasubramanian, P.; Raney, J.H.; Ganson, K.T.; Testa, A.; He, J.; Baker, F.C.; Nagata, J.M. Transgender Identity and Attention Deficit Hyperactivity Disorder Symptoms: Findings From the Adolescent Brain Cognitive Development Study. J. Adolesc. Health 2025, 76, 396–400. [Google Scholar] [CrossRef]
- Cortese, S.; Moreira-Maia, C.R.; St Fleur, D.; Morcillo-Peñalver, C.; Rohde, L.A.; Faraone, S.V. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am. J. Psychiatry 2016, 173, 34–43. [Google Scholar] [CrossRef]
- Pagoto, S.L.; Curtin, C.; Lemon, S.C.; Bandini, L.G.; Schneider, K.L.; Bodenlos, J.S.; Ma, Y. Association between Adult Attention Deficit/Hyperactivity Disorder and Obesity in the US Population. Obesity 2009, 17, 539–544. [Google Scholar] [CrossRef]
- Karhunen, V.; Bond, T.A.; Zuber, V.; Hurtig, T.; Moilanen, I.; Järvelin, M.-R.; Evangelou, M.; Rodriguez, A. The Link between Attention Deficit Hyperactivity Disorder (ADHD) Symptoms and Obesity-Related Traits: Genetic and Prenatal Explanations. Transl. Psychiatry 2021, 11, 455. [Google Scholar] [CrossRef]
- Aguirre Castaneda, R.L.; Kumar, S.; Voigt, R.G.; Leibson, C.L.; Barbaresi, W.J.; Weaver, A.L.; Killian, J.M.; Katusic, S.K. Childhood Attention-Deficit/Hyperactivity Disorder, Sex, and Obesity: A Longitudinal Population-Based Study. Mayo Clin. Proc. 2016, 91, 352–361. [Google Scholar] [CrossRef]
- Altfas, J.R. Prevalence of Attention Deficit/Hyperactivity Disorder among Adults in Obesity Treatment. BMC Psychiatry 2002, 2, 9. [Google Scholar] [CrossRef]
- Disney, E.R.; Elkins, I.J.; McGue, M.; Iacono, W.G. Effects of ADHD, Conduct Disorder, and Gender on Substance Use and Abuse in Adolescence. Am. J. Psychiatry 1999, 156, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Wilens, T.E. Attention-Deficit/Hyperactivity Disorder and the Substance Use Disorders: The Nature of the Relationship, Subtypes at Risk, and Treatment Issues. Psychiatr. Clin. N. Am. 2004, 27, 283–301. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.S.; Hinshaw, S.P.; Kraemer, H.C.; Lenora, N.; Newcorn, J.H.; Abikoff, H.B.; March, J.S.; Arnold, L.E.; Cantwell, D.P.; Conners, C.K.; et al. ADHD Comorbidity Findings from the MTA Study: Comparing Comorbid Subgroups. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Galéra, C.; Salla, J.; Montagni, I.; Hanne-Poujade, S.; Salamon, R.; Grondin, O.; Guichard, E.; Bouvard, M.P.; Tzourio, C.; Michel, G. Stress, Attention Deficit Hyperactivity Disorder (ADHD) Symptoms and Tobacco Smoking: The i-Share Study. Eur. Psychiatry 2017, 45, 221–226. [Google Scholar] [CrossRef]
- Zamboni, L.; Marchetti, P.; Congiu, A.; Giordano, R.; Fusina, F.; Carli, S.; Centoni, F.; Verlato, G.; Lugoboni, F. ASRS Questionnaire and Tobacco Use: Not Just a Cigarette. A Screening Study in an Italian Young Adult Sample. Int. J. Environ. Res. Public Health 2021, 18, 2920. [Google Scholar] [CrossRef]
- Hare, C.; Panda, E.J.; Collins, T.K.; Segalowitz, S.J.; Tekok-Kilic, A. The Interaction of ADHD Traits and Trait Anxiety on Inhibitory Control. Psychophysiology 2025, 62, e14734. [Google Scholar] [CrossRef]
- Oh, Y.; Yoon, H.J.; Kim, J.-H.; Joung, Y.S. Trait Anxiety as a Mediator of the Association between Attention Deficit Hyperactivity Disorder Symptom Severity and Functional Impairment. Clin. Psychopharmacol. Neurosci. 2018, 16, 407–414. [Google Scholar] [CrossRef]
- Tong, L.; Shi, H.-J.; Zhang, Z.; Yuan, Y.; Xia, Z.-J.; Jiang, X.-X.; Xiong, X. Mediating Effect of Anxiety and Depression on the Relationship between Attention-Deficit/Hyperactivity Disorder Symptoms and Smoking/Drinking. Sci. Rep. 2016, 6, 21609. [Google Scholar] [CrossRef]
- van der Meer, D.; Hoekstra, P.J.; van Rooij, D.; Winkler, A.M.; van Ewijk, H.; Heslenfeld, D.J.; Oosterlaan, J.; Faraone, S.V.; Franke, B.; Buitelaar, J.K.; et al. Anxiety Modulates the Relation between Attention-Deficit/Hyperactivity Disorder Severity and Working Memory-Related Brain Activity. World J. Biol. Psychiatry 2018, 19, 450–460. [Google Scholar] [CrossRef]
- Kozak, K.; Lucatch, A.M.; Lowe, D.J.E.; Balodis, I.M.; MacKillop, J.; George, T.P. The Neurobiology of Impulsivity and Substance Use Disorders: Implications for Treatment. Ann. N. Y. Acad. Sci. 2019, 1451, 71–91. [Google Scholar] [CrossRef]
- Bishop, C.; Mulraney, M.; Rinehart, N.; Sciberras, E. An Examination of the Association between Anxiety and Social Functioning in Youth with ADHD: A Systematic Review. Psychiatry Res. 2019, 273, 402–421. [Google Scholar] [CrossRef]
- Urcelay, G.P.; Dalley, J.W. Linking ADHD, Impulsivity, and Drug Abuse: A Neuropsychological Perspective. Curr. Top. Behav. Neurosci. 2012, 9, 173–197. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).