Design and Implementation of a Virtual Reality (VR) Urban Highway Driving Simulator for Exposure Therapy: An Interdisciplinary Project and Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Clinical Assessments
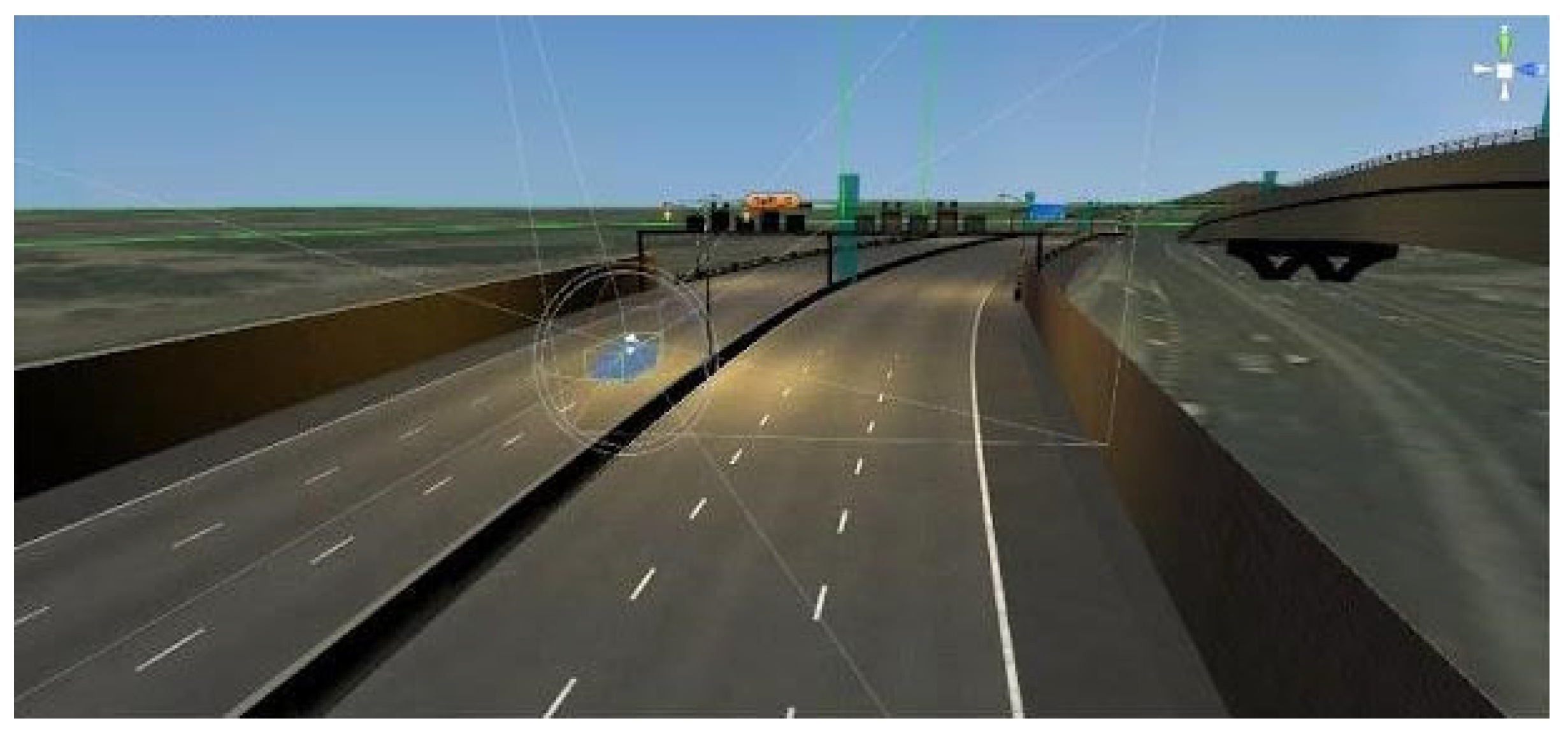
2.3. Devices and Design of VR Driving Simulation Program
- Time of day—daytime, sunset, nighttime.
- Weather—clear, cloudy, rainy.
- Traffic—light, moderate, heavy.
- Discrete events—presence of accidents, vehicles with sirens, reckless driving.
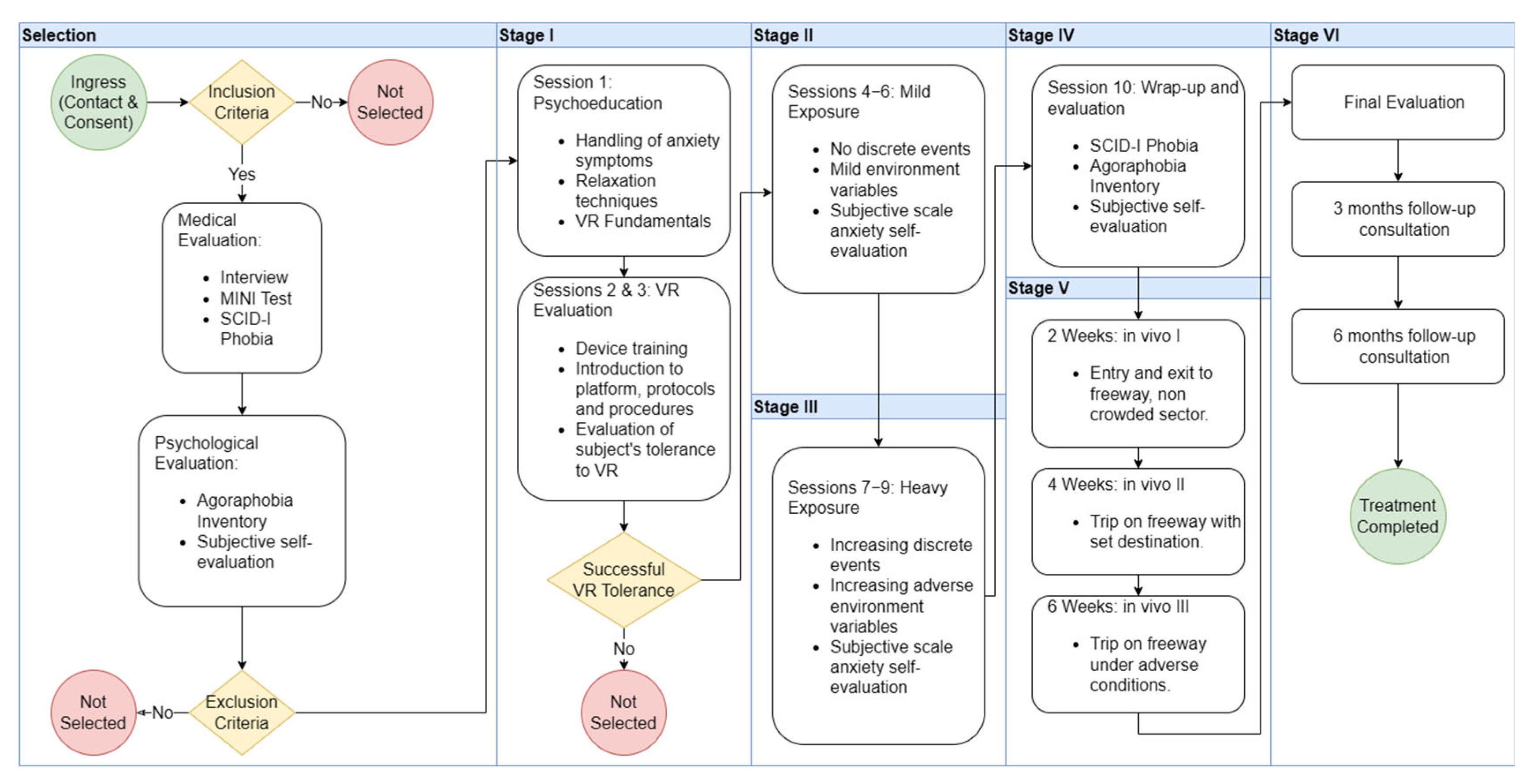
2.4. Clinical Protocol for VR-Based Exposure Therapy
- Psychoeducation and training (1 session): subjects are trained in VR use and educated in acute anxiety management and relaxation techniques.
- Trial runs (2 sessions): subjects are exposed to VR for short durations under supervision.
- Mild exposure (3 sessions): subjects are exposed to the VR environment under mild environment conditions and no discrete events.
- Heavy exposure (3 sessions): subjects are exposed to the VR environment under adverse weather conditions and with discrete traffic events.
- Evaluation and closure (1 session): subjects are evaluated using the SCID-I and IA scores, as well as the subjective 1–10 scale in order to assess improved anxiety response immediately after the end of the treatment.
2.5. Statistical Analysis
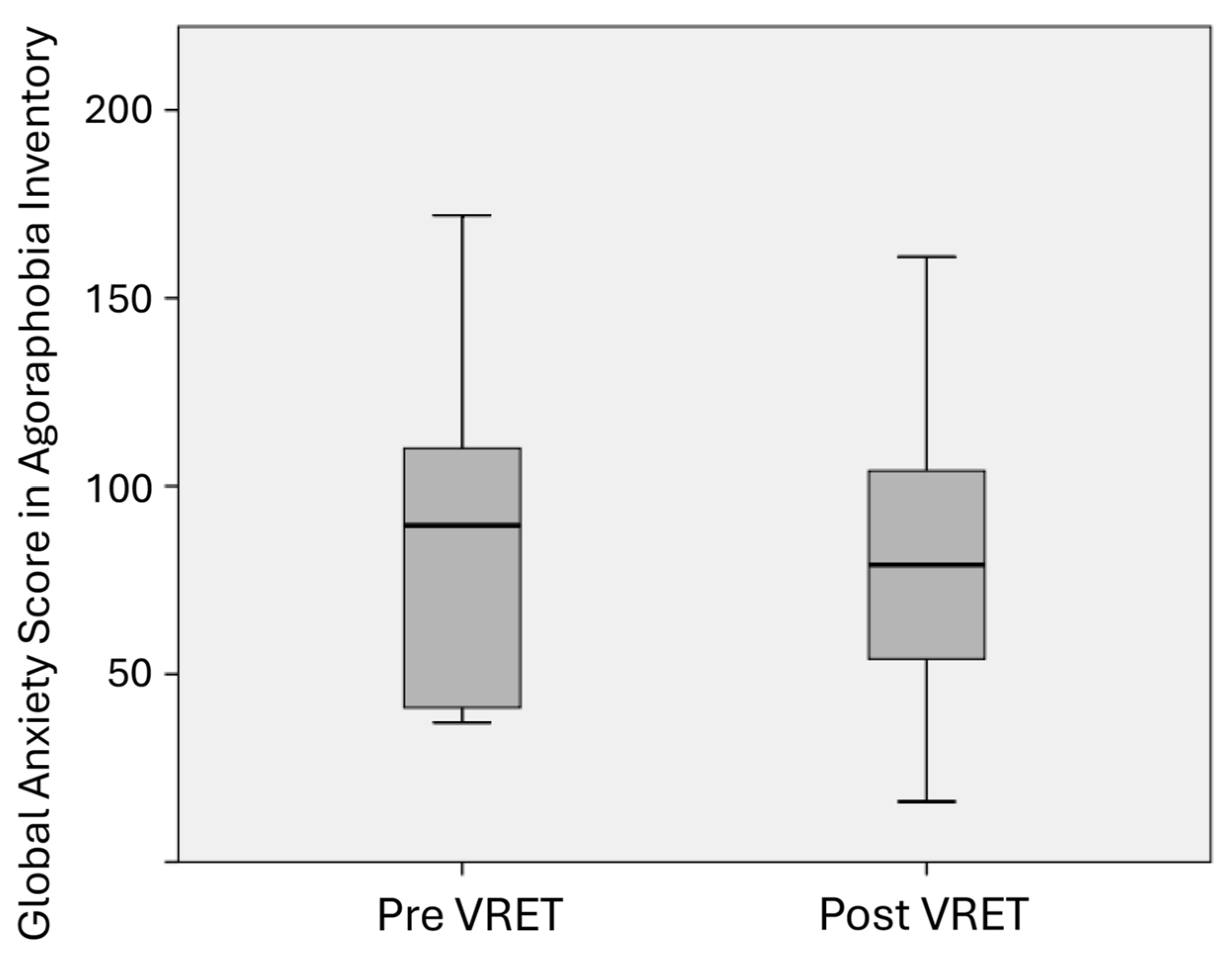
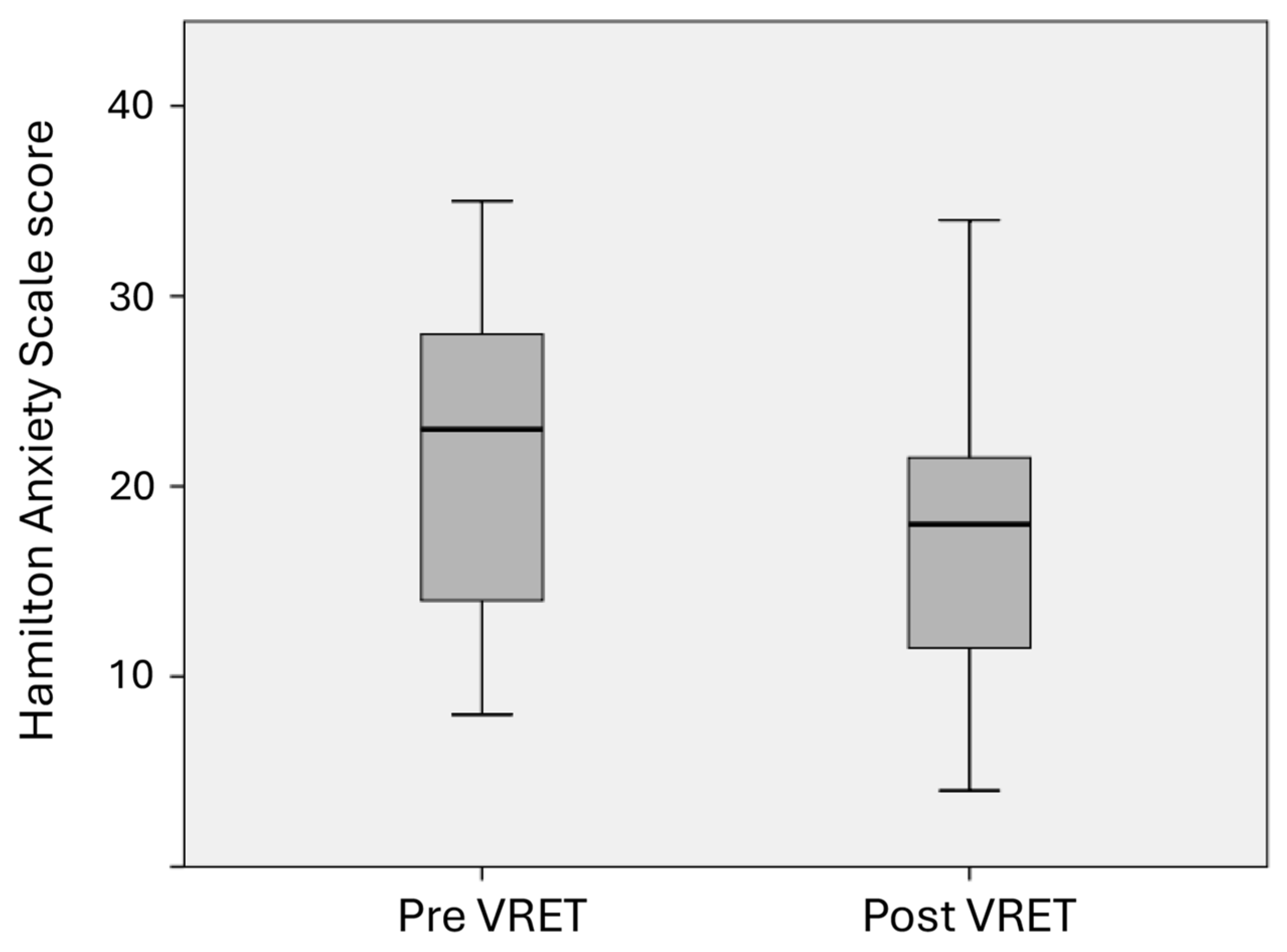
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013.
- Craske, M.G.; Stein, M.B.; Eley, T.C.; Milad, M.R.; Holmes, A.; Rapee, R.M.; Wittichen, H.U. Anxiety disorders. Nat. Rev. Dis. Primers 2017, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Chatterji, S.; Lee, S.; Ormel, J.; Ustün, T.B.; Wang, P.S. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiol. Psichiatr. Soc. 2009, 18, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Green, M.; Mora, R. Las autopistas urbanas concesionadas, una nueva forma de segregación. In ARQ (Santiago) Arquitectura De Infraestructura/Infrastructure Architecture; no. 60; Julio: Santiago, Chile, 2005; pp. 56–58. [Google Scholar] [CrossRef]
- Why We Fear Highways. Psychology Today. 2025. Available online: https://www.psychologytoday.com/ca/blog/extreme-fear/201002/why-we-fear-highways (accessed on 3 April 2025).
- Hamm, A.O. Specific phobias. Psychiatr. Clin. N. Am. 2009, 32, 577–591. [Google Scholar] [CrossRef]
- Grös, D.; Antony, M. The assessment and treatment of specific phobias: A review. Curr. Psychiatry Rep. 2006, 8, 298–303. [Google Scholar] [CrossRef]
- Antony, M.; Barlow, D. Specific phobias. In Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic; Barlow, D.H., Ed.; Guilford Publications: New York, NY, USA, 2001; pp. 380–417. [Google Scholar]
- Li, B.; Zhang, R.; Kuhl, S. Minication affects action-based distance judgments in oculus rift HMDs. In Proceedings of the ACM Symposium on Applied Perception (SAP 2014), Vancouver, BC, Canada, 9–10 August 2014; pp. 91–94. [Google Scholar]
- Shirtcliff, E.A.; Finseth, T.T.; Winer, E.H.; Glahn, D.C.; Conrady, R.A.; Drury, S.S. Virtual stressors with real impact: What virtual reality-based biobehavioral research can teach us about typical and atypical stress responsivity. Transl. Psychiatry 2024, 14, 441. [Google Scholar] [CrossRef]
- Monge, J.P.; López, G.; Guerrero, L.A. Supporting Phobia Treatment with Virtual Reality: Systematic Desensitization Using Oculus Rift. In Advances in Human Factors and Ergonomics in Healthcare, Proceedings of the AHFE 2016 International Conference on Human Factors and Ergonomics in Healthcare, Orlando, FL, USA, 27–31 July 2016; Duffy, V., Lightner, N., Eds.; Advances in Intelligent Systems and Computing; Springer: Cham, Switzerland, 2017; Volume 482. [Google Scholar]
- Carl, E.; Stein, A.; Levihn-Coon, A.; Pogue, J.; Rothbaum, B.; Emmelkamp, P.; Asmundson, G.; Carlbring, P.; Powers, M. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef]
- Pitti, C.T.; Peñate, W.; De La Fuente, J.; Bethencourt, J.M.; Roca-Sánchez, M.J.; Acosta, L.; Villaverde, M.L.; Gracia, R. The combined use of virtual reality exposure in the treatment of agoraphobia. Actas Esp. Psiquiatr. 2015, 43, 133–141. [Google Scholar]
- Castro, W.P.; Roca Sánchez, M.J.; Pitti González, C.T.; Bethencourt, J.M.; de la Fuente Portero, J.A.; Marco, R.G. Cognitive-behavioral treatment and antidepressants combined with virtual reality exposure for patients with chronic agoraphobia. Int. J. Clin. Health Psychol. 2014, 14, 9–17. [Google Scholar] [CrossRef]
- Malbos, E.; Rapee, R.M.; Kavakli, M. A controlled study of agoraphobia and the independent effect of virtual reality exposure therapy. Aust. N. Z. J. Psychiatry 2013, 47, 160–168. [Google Scholar] [CrossRef]
- Pelissolo, A.; Zaoui, M.; Aguayo, G.; Yao, S.N.; Roche, S.; Ecochard, R.; Gueyffier, F.; Pull, C.; Berthoz, A.; Jouvent, R.; et al. Virtual reality exposure therapy versus cognitive behavior therapy for panic disorder with agoraphobia: A randomized comparison study. J. Cyberther. Rehabil. 2012, 5, 35–43. [Google Scholar]
- Bouchard, S. Could virtual reality be effective in treating children with phobias? Expert. Rev. Neurother. 2011, 11, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.; Pérez-Ara, M.Á.; Bretón-López, J.; Quero, S.; García-Palacios, A.; Baños, R.M. In vivo versus augmented reality exposure in the treatment of small animal phobia: A randomized controlled trial. PLoS ONE 2016, 11, e0148237. [Google Scholar] [CrossRef] [PubMed]
- Miloff, A.; Lindner, P.; Hamilton, W.; Reuterskiöld, L.; Andersson, G.; Carlbring, P. Single-session gamified virtual reality exposure therapy for spider phobia vs traditional exposure therapy: Study protocol for a randomized controlled non-inferiority trial. Trials 2016, 17, 60. [Google Scholar] [CrossRef]
- Shiban, Y.; Schelhorn, I.; Pauli, P.; Mühlberger, A. Effect of combined multiple contexts and multiple stimuli exposure in spider phobia: A randomized clinical trial in virtual reality. Behav. Res. Ther. 2015, 71, 45–53. [Google Scholar] [CrossRef]
- Garcia-Palacios, A.; Hoffman, H.; Carlin, A.; Furness TA3rd Botella, C. Virtual reality in the treatment of spider phobia: A controlled study. Behav. Res. Ther. 2002, 40, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, R.; David, D. One session treatment of cognitive and behavioral therapy and virtual reality for social and specific phobias. Preliminary results from a randomized clinical trial. J. Evid.-Based Psychother. 2014, 14, 67–83. [Google Scholar]
- Triscari, M.T.; Faraci, P.; Catalisano, D.; D’Angelo, V.; Urso, V. Effectiveness of cognitive behavioral therapy integrated with systematic desensitization, cognitive behavioral therapy combined with eye movement desensitization and reprocessing therapy, and cognitive behavioral therapy combined with virtual reality exposure therapy methods in the treatment of flight anxiety: A randomized trial. Neuropsychiatr. Dis. Treat. 2015, 11, 2591–2598. [Google Scholar]
- Krijn, M.; Emmelkamp, P.M.; Biemond, R.; de Wilde de Ligny, C.; Schuemie, M.J.; van der Mast, C.A. Treatment of acrophobia in virtual reality: The role of immersion and presence. Behav. Res. Ther. 2004, 42, 229–239. [Google Scholar] [CrossRef]
- Morina, N.; Ijntema, H.; Meyerbröker, K.; Emmelkamp, P.M. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav. Res. Ther. 2015, 74, 18–24. [Google Scholar] [CrossRef]
- Schröder, D.; Wrona, K.J.; Müller, F.; Heinemann, S.; Fischer, F.; Dockweiler, C. Impact of virtual reality applications in the treatment of anxiety disorders: A systematic review and meta-analysis of randomized-controlled trials. J. Behav. Ther. Exp. Psychiatry 2023, 81, 101893. [Google Scholar] [CrossRef]
- Fischer, C.; Heider, J.; Schröder, A.; Taylor, J.E. “Help! I’m Afraid of Driving!” Review of Driving Fear and its Treatment. Cogn. Ther. Res. 2020, 44, 420–444. [Google Scholar] [CrossRef]
- Wald, J.; Taylor, S. Efficacy of virtual reality exposure therapy to treat driving phobia: A case report. J. Behav. Ther. Exp. Psychiatry 2000, 31, 249–257. [Google Scholar] [CrossRef]
- Wald, J.; Taylor, S. Preliminary research on the efficacy of virtual reality exposure therapy to treat driving phobia. Cyberpsychol. Behav. 2003, 6, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Walshe, D.; Elizabeth, L.; Kim, S.; O´Sullivan, K.; Wiederhold, B. Exploring the Use of Computer Games and Virtual Reality in Exposure Therapy for Fear of Driving Following a Motor Vehicle Accident. Cyberpsychol. Behav. 2003, 6, 3. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, R.; Carvalho, M.; Ribeiro, P.; Nardi, A. Virtual reality exposure therapy for fear of driving: Analysis of clinical characteristics, physiological response, and sense of presence. Braz. J. Psychiatry 2018, 40, 192–199. [Google Scholar] [CrossRef]
- Kaussner, Y.; Kuraszkiewicz, A.M.; Schoch, S.; Markel, P.; Hoffmann, S.; Baur-Streubel, R.; Kenntner-Mabiala, R.; Pauli, P. Treating patients with driving phobia by virtual reality exposure therapy—A pilot study. PloS ONE. 2020, 15, e0226937. [Google Scholar] [CrossRef]
- Elphinston, R.A.; Vaezipour, A.; Fowler, J.A.; Russell, T.G.; Sterling, M. Psychological therapy using virtual reality for treatment of driving phobia: A systematic review. Disabil. Rehabil. 2022, 45, 1582–1594. [Google Scholar] [CrossRef]
- Trappey, A.; Trappey, C.V.; Chang, C.M.; Tsai, M.C.; Kuo, R.R.T.; Lin, A.P.C. Virtual Reality Exposure Therapy for Driving Phobia Disorder (2): System Refinement and Verification. Appl. Sci. 2020, 11, 347. [Google Scholar] [CrossRef]
- First, M.B.; Spitzer, R.L.; Williams, J.B.; Gibbon, M. Structured Clinical Interview for DSM-IV (SCID-I). In Clinical Version (SCID-CV) (User’s Guide and Interview); American Psychiatric Press: Washington, DC, USA, 1997. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33; quiz 34–57. [Google Scholar]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef]
- Echeburúa, E.; Corral, P.; García, E.; Pérez, D.; Borda, M. Un nuevo Inventario de Agorafobia. Análisis Modif. Conducta 1992, 18, 101–102. [Google Scholar]
- Forno, M. Con un simulador de la Costanera Norte controlan el miedo a conducir por autopistas. Las Últimas Noticias, 29 December 2019. [Google Scholar]
- Howard, E.; LeWine, M.D. Phobia-Harvard Health. 2024. Available online: https://www.health.harvard.edu/a_to_z/phobia-a-to-z (accessed on 3 April 2025).



| Patient | Sessions | Follow-Up | Evaluation | Exposure | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 1 | 2 | 3 | |||
| 7 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 9 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | N | Y | N |
| 12 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y |
| 19 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | N | Y | N |
| 26 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y |
| 28 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 35 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 45 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| 47 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 48 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 49 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melis, F.; Sánchez, R.; González, L.M.; Pellegrini, P.; Fuentes, J.; Nieto, R. Design and Implementation of a Virtual Reality (VR) Urban Highway Driving Simulator for Exposure Therapy: An Interdisciplinary Project and Pilot Study. Psychiatry Int. 2025, 6, 58. https://doi.org/10.3390/psychiatryint6020058
Melis F, Sánchez R, González LM, Pellegrini P, Fuentes J, Nieto R. Design and Implementation of a Virtual Reality (VR) Urban Highway Driving Simulator for Exposure Therapy: An Interdisciplinary Project and Pilot Study. Psychiatry International. 2025; 6(2):58. https://doi.org/10.3390/psychiatryint6020058
Chicago/Turabian StyleMelis, Francisca, Ricardo Sánchez, Luz María González, Pablo Pellegrini, Jorge Fuentes, and Rodrigo Nieto. 2025. "Design and Implementation of a Virtual Reality (VR) Urban Highway Driving Simulator for Exposure Therapy: An Interdisciplinary Project and Pilot Study" Psychiatry International 6, no. 2: 58. https://doi.org/10.3390/psychiatryint6020058
APA StyleMelis, F., Sánchez, R., González, L. M., Pellegrini, P., Fuentes, J., & Nieto, R. (2025). Design and Implementation of a Virtual Reality (VR) Urban Highway Driving Simulator for Exposure Therapy: An Interdisciplinary Project and Pilot Study. Psychiatry International, 6(2), 58. https://doi.org/10.3390/psychiatryint6020058






