Abstract
Background: Piperazines, synthetic compounds known for their stimulant and hallucinogenic effects, have gained prominence among novel psychoactive substances (NPS) and are frequently associated with adverse psychiatric outcomes, including psychosis. Methods: A systematic review of the literature available up to 23 May 2024 was conducted, using the PubMed, Scopus, and Web of Science databases, in addition to the related gray literature, utilizing the following search strategy: “piperazines” AND (“psychosis” OR “hallucination” OR “delusion” OR “schizophrenia” OR “delusional” OR “schizoaffective”) NOT review NOT animal. Data collection adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The research methods were registered with PROSPERO (CRD42024549204). Results: Out of a total of 4547 articles identified, 4 met the inclusion criteria. We observed an important relationship between piperazine abuse and the onset of acute psychotic episodes, marked by symptoms such as paranoia, auditory, and visual hallucinations. Conclusion: The complex polyreceptor action mechanism of piperazines may explain these psychopathological effects, similar to those observed with other NPS. Although studies confirm a link between piperazine use and psychosis, data on long-term outcomes are limited. Recovery is common following cessation and treatment. Further research into the effects of piperazine abuse and the development of specific treatment protocols for substance-induced psychosis is necessary.
Keywords:
NPS; piperazine; psychosis; drug misuse; drug abuse; schizophrenia; substance induced-psychosis 1. Introduction
The misuse of psychoactive substances has escalated into a major public health concern globally in recent years. Alongside traditional substances of abuse, the prevalence of New Psychoactive Substances (NPS) has been increasingly documented [1,2]. NPS encompass a varied array of unregulated compounds engineered to replicate the effects of regulated drugs such as cannabis, cocaine, ecstasy, and lysergic acid diethylamide (LSD) [3]. These substances are frequently synthesized to circumvent existing drug laws, complicating their detection and regulation [4]. The primary groups of NPS include aminoindanes (e.g., MDAI), synthetic cannabinoids, synthetic cathinones, phencyclidine-type substances, phenethylamines, piperazines, tryptamines, and plant-based substances (e.g., kratom, salvia divinorum, and khat). Additionally, this category can also encompass substances derived from fauna or animal body parts, such as lizard tails and the venom of specific reptiles or amphibians (e.g., bufotenin) [5,6,7].
From the 1950s and 1960s onward, a distinct “drug culture” emerged, forming a subculture centered on the shared experience of substance use, with its own unique values, beliefs, customs, and language. This culture gained traction through various channels, such as music and art, which often glamorized the associated lifestyle. For instance, marijuana was linked with jazz musicians in the 1920s, and MDMA with the rave scene in the 1990s. These subcultures provide social support and reinforce drug use behaviors, creating a strong sense of identity and belonging for those who feel marginalized by mainstream society [8]. In recent decades, a distinct subtype of “drug culture” has emerged, referred to as the “psychonauts”. Psychonauts, or “e-psychonauts”, are individuals who intentionally induce altered states of consciousness through the use of various psychoactive substances, aiming to explore their own minds and address spiritual or existential questions. These individuals typically possess high levels of pharmacological and pharmaceutical knowledge and are deeply involved in the online dissemination of their drug experiences [9]. This behavior aligns with broader postmodern cultural tendencies characterized by individualization, an emphasis on the present moment, and a significant influence of the internet on social and cultural practices [10,11]. In this context, the phenomenon of “psychonauts” has emerged as a unique aspect of contemporary substance use. NPS also play a significant role in two distinct phenomena characteristic of postmodern “drug culture”; their use in chemsex, particularly within the LGBTQ community [12,13], and their use as “club drugs” to enhance the experience at parties and raves [14,15].
The internet plays a crucial role in the behavior and practices of psychonauts. They utilize the internet as a primary platform for the exchange of information regarding the use of psychoactive substances [9,16]. Online forums, social media platforms, and specialized websites enable these individuals to share detailed accounts of their experiences, provide advice on safe usage, and discuss the effects of various substances. This digital interaction fosters a global community where psychonauts can access a vast repository of knowledge and insights that would otherwise be inaccessible [16,17].
Moreover, the internet facilitates the availability of novel psychoactive substances (NPS) by providing easy access to online pharmacies and marketplaces that sell these substances. The anonymity and convenience of online purchasing further encourage psychonautic exploration [16]. This digital ecosystem supports the continuous evolution of substance use trends, as psychonauts experiment with new compounds and share their findings in real-time, contributing to a dynamic and rapidly changing landscape of psychoactive substance use [17]. The easy availability of NPS on the internet is likely one of the major factors that contributed to their widespread use during the COVID-19 pandemic, where forced isolation and difficulties in mobility and access to illegal substances significantly impacted the behavior of drug users [18,19].
The rapid expansion of NPS, propelled by the Internet and online marketplaces, has created a constantly changing drug abuse environment, presenting unique challenges to law enforcement and healthcare providers [20,21,22]. NPS have emerged as a global issue, with reports from 141 countries and territories worldwide indicating the presence of one or more NPS. By November 2023, a total of 1230 substances have been reported to the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) on NPS by various governments, laboratories, and partner organizations [23]. These consist of various classes of substances such as synthetic cannabinoids, synthetic cathinones, tryptamines, phenethylamines, synthetic opioids, phencyclidine-like dissociatives, and piperazines [1].
Accompanying the proliferation of NPS is the phenomenon known as “pharming”. This term denotes the recreational use of prescription and over-the-counter (OTC) drugs, either singly or in combination with other substances, including NPS [24]. Pharming has become popular, particularly among youths and vulnerable groups, due to an easy access to these medications and the belief that they are safer than illicit drugs. Nonetheless, the misuse of these substances can result in severe health consequences such as dependence, overdose, and the development of psychiatric disorders [24,25].
An especially alarming aspect of these new substance abuse trends is the profound psychopathological impact these substances exert [26], with risks of developing psychotic disorders [26,27], self-harm and suicide [28], dependence and withdrawal [29], and death from intoxication and poisoning [30,31]. In particular, the development of psychotic disorders poses a significant concern, especially regarding the induction of ex novo psychosis in vulnerable individuals [26,32] and the potential to trigger schizophrenia or other disorders within the psychotic spectrum [33]. Additionally, concerns persist regarding enduring substance-induced psychoses, known as SREP (Substance-Related Exogenous Psychosis) [10].
Among the various classes of these substances, piperazines are a group of synthetic compounds with significant psychoactive effects [20]. Piperazine (1,4-hexahydropyrazine) is a cyclic organic compound characterized by a six-membered heterocyclic ring containing two nitrogen atoms positioned opposite each other. This structure serves as the foundation for various piperazine derivatives, which are commonly used as recreational drugs and typically include an aromatic ring attachment. Piperazine derivatives can be categorized into two main types: benzyl-piperazines, where a methyl group links the piperazine to an aromatic ring, and phenyl-piperazines, where a phenyl group is attached to the piperazine structure [34]. Initially synthesized for potential therapeutic applications and marketed as an anthelmintic [35], piperazines such as benzylpiperazine (BZP) and trifluoromethylphenylpiperazine (TFMPP), as well as more than 20 analogs, had gained popularity as recreational drugs due to their stimulant and especially euphoric properties until the first decade of the 2000s [36,37]. The appeal of piperazines as recreational substances stems from their ability to cause the cumulative release of dopamine and serotonin, producing effects similar to those of amphetamines and methylenedioxymethamphetamine (MDMA), including increased energy, sociability, euphoria, and hallucinogenic effects [34,38]. However, these perceived benefits are overshadowed by numerous adverse effects. Acute intoxication can manifest as agitation, anxiety, nausea, and hallucinations instead, and chronic use has been linked to serious psychological and physiological issues, including dependence, cognitive deficits, and cardiovascular problems [20,36,37]. One of the most concerning psychopathological consequences of NPS abuse is their potential to induce psychotic symptoms, such as delusions, hallucinations, and disorganized thinking [28]. Although the precise mechanisms through which piperazines provoke psychosis are not fully understood, it is speculated that their interaction with serotonin and dopamine receptors plays a pivotal role [26].
Aims of the study: This article aims to explore the relationship between piperazine abuse and the onset of psychosis, drawing on the existing literature and clinical reports; by examining the pharmacological properties of piperazines, their patterns of abuse, and the resultant psychological effects, we aim to elucidate the underlying mechanisms and potential risk factors contributing to piperazine-induced psychosis. In particular, the current review, aimed to achieve the following: (i) examine the association between piperazine abuse and psychosis; (ii) characterize these psychotic episodes from a psychopathological perspective; (iii) investigate the outcomes to determine whether this psychotic symptomatology represents a form of substance-induced transient psychosis or if there is a risk of transition to schizophrenia or another chronic form of psychosis.
2. Materials and Methods
2.1. Systematic Review Procedures
A systematic electronic search was performed on 23 May 2024 on the PubMed, Scopus, and Web of Science (WoS) databases. AMo combined the search strategy of free text terms with an expanded range of MeSH headings related to piperazine and psychotic disorders. These include Schizophrenia Spectrum Disorders, particularly schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, Substance-induced psychotic disorder, as well as affective psychoses. The following search strategies were used, respectively, in PubMed and WoS: “piperazines” AND (“psychosis” OR “hallucination” OR “delusion” OR “schizophrenia” OR “delusional” OR “schizoaffective”) NOT review NOT animal; in Scopus: (TITLE-ABS-KEY (“piperazines”) AND TITLE-ABS-KEY (“psychosis”) OR TITLE-ABS-KEY (“hallucination”) OR TITLE-ABS-KEY (“schizophrenia”) OR TITLE-ABS-KEY (“delusional”) OR TITLE-ABS-KEY (“schizoaffective”) AND NOT TITLE-ABS-KEY (animals) AND NOT TITLE-ABS-KEY (review).
The systematic review was structured following PRISMA [39,40] and PROSPERO [41] guidelines. Identified studies were assessed at the title/abstract and the full text screening against eligibility criteria. The eligibility criteria included the selection of exclusively original articles written in English that report data on the correlation between piperazine and psychosis (delusion, hallucination, or schizophrenia spectrum disorders or affective psychoses). All studies that are not original, not written in English, report the misuse of other substances, or do not relate to psychosis were excluded.
2.2. Data Synthesis Strategy
The selection and eligibility phase of the articles was carried out independently by n = 3 investigators (AMi, GM, and CC), then subjected to a last cross-check by AMo and SC. All discordant cases were evaluated by PM, GM, and FS. Any unsolved doubts by the team on any of the topics covered in the article were clarified directly from the author, if contactable. The data were collected in a Word table that included the first author’s name, year of publication, study design, demographic variables (gender, age, and psychiatric and medical history), details of the substance used (specific molecule, dosage, and route of administration), and information on poly-abuse. Additionally, it captured non-psychotic psychiatric symptoms (e.g., depression, anxiety), types of thought and ideation disturbances, presence and type of hallucinations, and presence or absence (yes or no) of a psychedelic experience to distinguish a true psychotic episode from a sensory-perceptual alteration of psychedelic nature. Finally, the outcome was noted to differentiate between an acute psychosis with remission and a chronic form of psychosis. The exclusion criteria for both selection phases were as follows: (1) non-original research (e.g., review, metanalysis, commentary, editorial, letter to the editor without data available, and book chapter); (2) non-full-text articles (e.g., meeting abstract); (3) language other than English; (4) animal/in vitro studies; (5) articles not dealing with the misuse of piperazines; and (6) articles not dealing with psychotic symptom or schizophrenic spectrum disorder. The selection process utilized Excel spreadsheets.
All these research methods were approved by PROSPERO (identification code CRD42024549204). For Supplementary Materials, see the relevant section.
3. Results
Removing duplicate articles (n = 1532) from a total of 4547 papers (PubMed = 1590; Scopus = 1381; WoS = 1576), 3015 records were screened, and, among these, some 2105 were irrelevant to the subject reading title and abstract (animal/in vitro studies; articles not dealing with the misuse of piperazines; no psychotic symptoms reported; a number of 304 were not written in English; and 347 were non-original articles (e.g., review, metanalysis, commentary, letter to the editor without data available, and book chapter)). Of the 259 full-text articles assessed for eligibility, some 255 did not match the inclusion criteria for our review. Finally, four articles were included (Figure 1; Table 1).
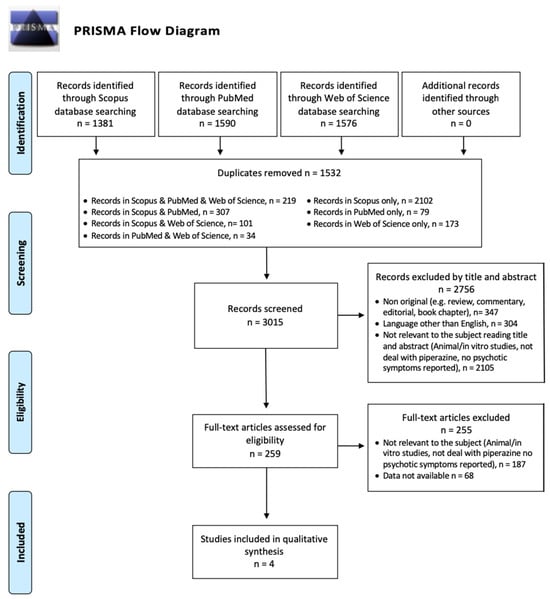
Figure 1.
PRISMA flow diagram.
Within the four articles selected for evaluation, the types included two observational studies [42,43], one case report [44], and one randomized, double-blind, placebo-controlled trial [45]. Regarding the substances abused, BZP and TFMPP were reported in three articles [42,44,45], and meta-chlorophenylpiperazine (mCPP) in another. Demographically, most subjects were males aged between 20 and 24 years [44,45], with two articles omitting sociodemographic data [42,43]. No pre-existing psychiatric or medical comorbidities were reported. Administration was oral except in one study where it was not specified [42]. Regarding polydrug use, BZP was combined with cannabis and nitrous oxide in one instance [44], and piperazines were taken with alcohol and benzodiazepines in another [45]. The most commonly reported non-psychotic psychiatric symptoms were anxiety [43,44,45], followed by agitation [43,45], and insomnia [42,45]. Notably, irritability, feelings of aggression, and suicidal thoughts were reported in one case [42]. All articles described thought and ideation disturbances, particularly paranoia and persecution delusions [42,43,44]; one did not specify the type of thought alteration [45], and one reported poisonous delirium [46]. Hallucinations were mentioned in all articles; specifically, auditory and visual in two studies [42,44], unspecified hallucinations in two [42,45], and olfactory in one [44]. Three out of four cases described a psychedelic experience due to piperazine use [42,43,44]. In terms of outcomes, two cases were noted as acute psychosis with remission, indicative of substance-induced psychosis [44,45], while the other two did not report any outcomes.

Table 1.
Summary of retrieved studies.
Table 1.
Summary of retrieved studies.
| Name, Year | Substance | Study Design | Population (N, M, F) | MA ± Standard Deviation | Psychiatric Comorbidity | Medical Comorbidity (Yes/No) | Administration | Poly-Abuse (Substance) | Non-Psychotic Psychiatric Symptoms | Thought and Ideation Disturbances | Hallucinations | Psychedelic Experience (Yes/No) | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Austin and Monasterio et al., 2004 [44] | “Rapture” (BZP) in addition to small quantities of cannabis and nitrous oxid | Case report | M = 1 | 20 | No | NA | Oral | Cannabis, nitrous oxide | Anxiety | Persecution delusions, poisonous delirium | Auditory, visual, and olfactory hallucinations | Yes | Acute psychosis with remission |
| Bossong et al., 2010 [43] | mCPP | Observational study | N = 79 | NA | NA | NA | Oral | NA | Anxiety, dizziness, agitation | Unspecified delusion, paranoia | Unspecified hallucinations | NA | NA |
| Thompson et al., 2010 [45] | BZP, TFMPP | Randomized, double-blind, placebo-controlled trial | N = 35 (M = 22 F = 13) | MA = 24 | No | No | Oral | Alcohol, benzodiazepines | Anxiety, agitation, insomnia | Present but unspecified | Unspecified hallucinations | Yes | Acute psychosis with remission |
| Wilkins et al., 2008 [42] | BZP and TFMPP | Observational study | NA | NA | NA | NA | NA | NA | Mood swings, insomnia, poor appetite, hot/cold flushes, heavy sweating, confusion, irritability, feelings of aggression, suicidal thoughts | Paranoia | Auditory and visual hallucinations | Yes | NA |
Abbreviation: BZP: benzylpiperazine; F: female; M: male; MA: mean age; mCPP: meta-chlorophenylpiperazine; NA: not applicable; TFMPP: trifluorophenylmethylpiperazine.
4. Discussion
To the best of our knowledge, this work represents the first review to investigate the association between piperazine abuse and psychosis. This systematic review highlights an important relationship between piperazine abuse and the onset of psychosis, affirming the need for heightened awareness and understanding within both clinical and public health domains. Our research demonstrates that the misuse of piperazines is associated with psychotic episodes featuring paranoia, as well as auditory and visual hallucinations. This corroborates the existing literature that highlights paranoia as a typical consequence of NPS usage [26] and identifies both types of hallucinations as frequent symptoms of their abuse, especially with other drugs [10]. The outcomes of these studies mirror those observed with other NPS due to similar interactions with serotonin and dopamine receptors [38,46]. Indeed, the literature consistently highlights that NPS significantly affect psychopathology [26], presenting substantial risks for substance-induced psychosis [26,32] and the potential to trigger schizophrenia or other disorders within the psychotic spectrum [33]. Moreover, enduring concerns about substance-induced psychoses, known as SREP (Substance-Related Exogenous Psychosis) [10], are notably exemplified by synthetic cannabinoids, often referred to as “Spiceophrenia” [33], or by methamphetamine, which is capable of inducing Methamphetamine-Associated Psychosis (MAP) [47,48].
Our findings indicate that piperazines are more commonly associated with substance-induced psychotic episodes, with substantial recovery upon cessation of the substance and appropriate clinical treatment. Unfortunately, the outcomes of psychotic episodes were not documented in all the articles included in our review; in fact, we could not assess the outcome in half of the cases. Thus, although a significant association between piperazine abuse and the onset of psychosis is clear, we are unable to definitively determine whether, in addition to substance-induced episodes, piperazines can trigger the onset of a psychotic spectrum disorder or lead to chronic SREP. In this context, it is important to note that the pharmacological properties of piperazines, particularly their effects on neurotransmitters, highlight the risks they pose especially to individuals with pre-existing psychiatric vulnerabilities [37]. In this analysis, more than half of the cases involved polydrug use, combining piperazines with substances such as cannabis, nitrous oxide, alcohol, and benzodiazepines [44,45]. This pattern of polydrug use likely enhanced the psychopathological effects of piperazines and increased the risk of psychosis [38]. Additionally, demographic data indicate that young adults are especially susceptible to piperazine misuse, a vulnerability attributed to prevalent recreational drug use and ongoing brain development during early adulthood. Despite some countries’ efforts to regulate piperazines, their legal status remains a contentious issue, with ongoing debates about their classification and the adequacy of existing drug laws to manage new psychoactive substances effectively [27,46]. The ease of accessing these drugs through online platforms complicates enforcement efforts and underscores the need for robust international cooperation in monitoring and regulation [20].
The abuse pattern, often characterized by polydrug use and high dosages as observed in the reviewed studies, increases risk factors significantly. The literature consistently notes that the typical pattern of piperazine abuse, involving polydrug use (like alcohol, cannabis, and benzodiazepines) and high doses, not only complicates the clinical presentation but also markedly exacerbates the severity of ensuing psychosis [38]. Furthermore, demographic data indicating a higher prevalence among young adults suggests that this group may be particularly at risk, likely due to a combination of greater recreational drug use and developmental brain changes that occur during this life stage, underscoring the need for targeted educational and preventative interventions [49].
The current literature points to a critical gap in longitudinal research concerning the long-term psychiatric impacts of piperazine use. There is a pressing need for studies that explore both the acute and sustained psychiatric disorders associated with these substances, but also explore the effectiveness of specific interventions for piperazine-induced psychosis, aiding in the development of evidence-based treatment protocols [38]. Additionally, future research should focus on the chronic effects of these substances, particularly the potential for developing sustained psychotic disorders beyond initial use.
Currently, specific treatments for NPS-induced psychosis are lacking. Therefore, the authors refer clinicians to therapeutic recommendations from the literature on dual diagnosis [50,51,52,53] as well as on managing acute substance-induced psychosis [54,55,56].
Given the severe outcomes associated with piperazine abuse, there is an urgent need for targeted interventions. Healthcare providers need training to better recognize and manage substance-induced psychosis, particularly in emergency settings where individuals with acute presentations are likely to initially present [57]. Public health strategies should include education campaigns focused on the risks of NPS use, especially highlighting the potential for enduring psychotic disorders [58]. Addressing the proliferation of Novel Psychoactive Substances (NPS) requires comprehensive legislative and social management strategies due to the rapid development and dissemination of these substances. Traditional regulatory frameworks struggle to keep pace with new compounds, leading to significant public health challenges [59].
The effective management of NPS necessitates a multi-faceted approach. Legislatively, this includes the implementation of flexible drug scheduling laws that can quickly adapt to new substances. Governments and regulatory bodies must enhance their capacity for real-time monitoring and rapid response to emerging NPS trends, leveraging international cooperation to tackle the global distribution of NPS [60].
Socially, public education campaigns are crucial to raise awareness about the dangers of NPS. Healthcare providers and emergency services need specialized training to effectively recognize and manage NPS-related incidents. Additionally, online platforms play a pivotal role in both the spread and mitigation of NPS use, making collaboration with tech companies essential to monitor and regulate the sale and promotion of NPS online [61,62].
The European Union (EU) has implemented measures to improve the detection, risk assessment, and regulation of NPS. These legislative actions include temporary bans and the categorization of NPS based on risk levels, facilitating quicker responses to emerging threats. Public health strategies focus on harm reduction, such as public awareness campaigns and evidence-based interventions. However, despite these efforts, there remains a need for greater harmonization of policies across EU member states and more proactive risk minimization measures to effectively address the challenges posed by NPS [61]. In the United States, similar challenges are addressed through the Controlled Substances Act and the temporary scheduling of new substances by the Drug Enforcement Administration (DEA). Furthermore, global initiatives led by the United Nations Office on Drugs and Crime (UNODC) aim to standardize NPS regulation and promote international cooperation. Much work remains to be carried out to fully contain the problem [63]. It is also important to note that some of these substances, such as MDMA and psychedelics, are being explored for therapeutic applications [64,65,66]. This development could potentially shift the paradigm of “drug culture”, leading to a new balance in the perception of these substances, navigating between the reinforcement of drug use behaviors, stigma, and legitimate therapeutic uses [8]. Despite these concerted efforts, continuous advancements in legislation, education, and international collaboration are essential to mitigate the evolving risks associated with NPS and to protect public health effectively.
Study Limitations
The reviewed articles primarily rely on observational data and case reports which, although important, restrict the ability to gather comprehensive data and develop accurate psychopathological insights. Furthermore, the inconsistency in the purity and composition of street drugs marketed as piperazines further challenges the generalization of these results.
5. Conclusions
Piperazine abuse poses a significant risk for the induction of psychosis, with strong implications for mental health services and policy. It represents a significant public health issue, with substantial implications for mental health services and societal well-being. Addressing this emerging threat requires a concerted effort from clinicians, researchers, and policymakers to mitigate the impact of these substances on public health. Enhanced surveillance, research, and educational outreach are crucial steps toward understanding and managing the risks associated with piperazine and other NPS.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/psychiatryint5030040/s1.
Author Contributions
Conceptualization, A.M. (Alessio Mosca) and S.C.; methodology, A.M. (Andrea Miuli) and A.M. (Alessio Mosca); data curation, S.C., A.M. (Alessio Mosca), C.C. and G.M. (Gianluca Mancusi); writing—original draft preparation, S.C., A.M. (Alessio Mosca) and C.C.; writing—review and editing, A.M. (Alessio Mosca), C.C., J.M.C., L.M. and S.C.; supervision, G.M. (Giovanni Martinotti), M.P. and F.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
F.S. was a member of the UK Advisory Council on the Misuse of Drugs (ACMD; 2011–2019) and is currently a member of the EMA Advisory Board (Psychiatry). JMC is a co-opted member of the ACMD’s NPS and Technical Committees. G.M. has been a consultant and/or a speaker and/or has received research grants from Angelini, Doc Generici, Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Servier, and Recordati. A.M., S.C., C.C., G.M., M.P., and A.Mi., have nothing to declare.
References
- Schifano, F.; Orsolini, L.; Duccio Papanti, G.; Corkery, J.M. Novel psychoactive substances of interest for psychiatry. World Psychiatry 2015, 14, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, N.D.; Cottler, L.B.; Palamar, J.J. Public health surveillance of new psychoactive substances: Recent developments. Curr. Opin. Psychiatry 2024, 37, 270–276. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA Operating Guidelines for the European Union Early Warning System on New Psychoactive Substances; Publications Office of the European Union: Luxembourg, 2019; ISBN 978-92-9497-460-0. [Google Scholar] [CrossRef]
- Baumeister, D.; Tojo, L.M.; Tracy, D.K. Legal highs: Staying on top of the flood of novel psychoactive substances. Ther. Adv. Psychopharmacol. 2015, 5, 97–132. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Chatterjee, S.S.; Mitra, S. “A tale of tail”: A case of lizard tail abuse. Indian J. Psychiatry 2020, 62, 454–455. [Google Scholar] [CrossRef]
- Jadav, D.; Shedge, R.; Meshram, V.P.; Kanchan, T.; Shekhawat, R.S. Snake venom—An unconventional recreational substance for psychonauts in India. J. Forensic Leg. Med. 2022, 91, 102398. [Google Scholar] [CrossRef]
- United Nations: Office on Drugs and Crime [Internet]. UNODC Annual Report. Available online: https://www.unodc.org/unodc/en/about-unodc/annual-report.html (accessed on 25 August 2024).
- Treatment (US) C for SA. Drug Cultures and the Culture of Recovery. In Improving Cultural Competence; [Internet]; Substance Abuse and Mental Health Services Administration (US): Rockville, MD, USA, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK248421/ (accessed on 25 August 2024).
- Davey, Z.; Schifano, F.; Corazza, O.; Deluca, P.; on behalf of the Psychonaut Web Mapping Group. e-Psychonauts: Conducting research in online drug forum communities. J. Ment. Health 2012, 21, 386–394. [Google Scholar] [CrossRef]
- Martinotti, G.; De Risio, L.; Vannini, C.; Schifano, F.; Pettorruso, M.; Di Giannantonio, M. Substance-related exogenous psychosis: A postmodern syndrome. CNS Spectr. 2021, 26, 84–91. [Google Scholar] [CrossRef]
- Whitley, R. Postmodernity and Mental Health. Harv. Rev. Psychiatry 2008, 16, 352–364. [Google Scholar] [CrossRef]
- Pichini, S.; Di Trana, A.; Torrens, M.; Scherbaum, N.; Zaami, S. Editorial: New Trends of Substance Abuse: Looking for New Psychotropic Effects of Chem Sex Drugs, Cognitive Enhancers, and New Psychoactive Substances. Front. Psychiatry 2020, 11, 612192. [Google Scholar] [CrossRef]
- Schuler, M.S.; Ramchand, R. Examining Inhalant Use Among Sexual Minority Adults in a National Sample: Drug-Specific Risks or Generalized Risk? LGBT Health 2023, 10, 80–85. [Google Scholar] [CrossRef]
- di Giannantonio, M.; Negri, A.; Schiavone, S.; Vannini, C.; Pettorruso, M.; De-Giorgio, F.; Verrastro, V.; Trabace, L.; Corbo, M.; Gottardo, R.; et al. Prescription Drug Misuse in “Clubbers” and Disco Goers in Ibiza. Front. Psychiatry 2020, 11, 592594. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, K.; Neogi, R.; Basu, D. Club drugs: Review of the ‘rave’ with a note of concern for the Indian scenario. Indian J. Med. Res. 2011, 133, 594–604. [Google Scholar] [PubMed]
- Schifano, F.; Chiappini, S.; Corkery, J.M.; Scherbaum, N.; Guirguis, A. The e-psychonaut drugs’ psychopharmacology. Curr. Opin. Pharmacol. 2021, 57, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Orsolini, L.; St John-Smith, P.; McQueen, D.; Papanti, D.; Corkery, J.; Schifano, F. Evolutionary Considerations on the Emerging Subculture of the E-psychonauts and the Novel Psychoactive Substances: A Comeback to the Shamanism? Curr. Neuropharmacol. 2017, 15, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Zaami, S.; Marinelli, E.; Varì, M.R. New Trends of Substance Abuse During COVID-19 Pandemic: An International Perspective. Front. Psychiatry 2020, 11, 700. [Google Scholar] [CrossRef]
- Catalani, V.; Arillotta, D.; Corkery, J.M.; Guirguis, A.; Vento, A.; Schifano, F. Identifying New/Emerging Psychoactive Substances at the Time of COVID-19; A Web-Based Approach. Front. Psychiatry 2020, 11, 632405. [Google Scholar] [CrossRef]
- Schifano, F.; Chiappini, S.; Corkery, J.; Guirguis, A. Abuse of Prescription Drugs in the Context of Novel Psychoactive Substances (NPS): A Systematic Review. Brain Sci. 2018, 8, 73. [Google Scholar] [CrossRef]
- Miliano, C.; Margiani, G.; Fattore, L.; De Luca, M. Sales and Advertising Channels of New Psychoactive Substances (NPS): Internet, Social Networks, and Smartphone Apps. Brain Sci. 2018, 8, 123. [Google Scholar] [CrossRef]
- Schifano, F.; Leoni, M.; Martinotti, G.; Rawaf, S.; Rovetto, F. Importance of Cyberspace for the Assessment of the Drug Abuse Market: Preliminary Results from the Psychonaut 2002 Project. Cyberpsychol. Behav. 2003, 6, 405–410. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2024: Trends and Developments; [Internet]; LU: Publications Office: Luxembourg, 2024; Available online: https://data.europa.eu/doi/10.2810/161905 (accessed on 14 June 2024).
- Chiappini, S.; Schifano, F. What about “Pharming”? Issues Regarding the Misuse of Prescription and Over-the-Counter Drugs. Brain Sci. 2020, 10, 736. [Google Scholar] [CrossRef]
- Schifano, F.; Chiappini, S.; Miuli, A.; Mosca, A.; Santovito, M.C.; Corkery, J.M.; Guirguis, A.; Pettorruso, M.; Di Giannantonio, M.; Martinotti, G. Focus on Over-the-Counter Drugs’ Misuse: A Systematic Review on Antihistamines, Cough Medicines, and Decongestants. Front. Psychiatry 2021, 12, 657397. [Google Scholar] [CrossRef] [PubMed]
- Schifano, F.; Napoletano, F.; Chiappini, S.; Guirguis, A.; Corkery, J.M.; Bonaccorso, S.; Ricciardi, A.; Scherbaum, N.; Vento, A. New/emerging psychoactive substances and associated psychopathological consequences. Psychol. Med. 2021, 51, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, R.; Bersani, G.; Marinelli, E.; Zaami, S. The rise of new psychoactive substances and psychiatric implications: A wide-ranging, multifaceted challenge that needs far-reaching common legislative strategies. Hum. Psychopharmacol. Clin. Exp. 2020, 35, e2727. [Google Scholar] [CrossRef]
- Chiappini, S.; Mosca, A.; Miuli, A.; Santovito, M.C.; Orsolini, L.; Corkery, J.M.; Guirguis, A.; Pettorruso, M.; Martinotti, G.; Di Giannantonio, M.; et al. New Psychoactive Substances and Suicidality: A Systematic Review of the Current Literature. Medicina 2021, 57, 580. [Google Scholar] [CrossRef]
- Hasin, D.S.; O’Brien, C.P.; Auriacombe, M.; Borges, G.; Bucholz, K.; Budney, A.; Compton, W.M.; Crowley, T.; Ling, W.; Petry, N.M.; et al. DSM-5 Criteria for Substance Use Disorders: Recommendations and Rationale. Am. J. Psychiatry 2013, 170, 834–851. [Google Scholar] [CrossRef] [PubMed]
- Webb, L.; Shi, X.; Goodair, C.; Cheeta, S. Trends in Mortality from Novel Psychoactive Substances as “Legal Highs”: Gender Differences in Manner of Death and Implications for Risk Differences for Women. Front. Psychiatry 2022, 13, 890840. [Google Scholar] [CrossRef]
- Schifano, F.; Orsolini, L.; Papanti, D.; Corkery, J. NPS: Medical Consequences Associated with Their Intake. In Neuropharmacology of New Psychoactive Substances (NPS); [Internet]; Current Topics in Behavioral Neurosciences; Baumann, M.H., Glennon, R.A., Wiley, J.L., Eds.; Springer International Publishing: Cham, Switzerland, 2016; Volume 32, pp. 351–380. Available online: https://link.springer.com/10.1007/7854_2016_15 (accessed on 14 June 2024).
- Fiorentini, A.; Sara Volonteri, L.; Dragogna, F.; Rovera, C.; Maffini, M.; Carlo Mauri, M.; Altamura, C.A. Substance-Induced Psychoses: A Critical Review of the Literature. Curr. Drug Abus. Rev. 2011, 4, 228–240. [Google Scholar] [CrossRef]
- Papanti, D.; Schifano, F.; Botteon, G.; Bertossi, F.; Mannix, J.; Vidoni, D.; Impagnatiello, M.; Pascolo-Fabrici, E.; Bonavigo, T. “Spiceophrenia”: A systematic overview of “Spice”-related psychopathological issues and a case report. Hum. Psychopharmacol. Clin. Exp. 2013, 28, 379–389. [Google Scholar] [CrossRef]
- Gee, P.; Schep, L.J. Chapter12-1-Benzylpiperazine and other piperazine-based stimulants. In Novel Psychoactive Substances, 2nd ed.; [Internet]; Dargan, P., Wood, D., Eds.; Academic Press: Boston, MA, USA, 2022; pp. 301–332. Available online: https://www.sciencedirect.com/science/article/pii/B9780128187883000097 (accessed on 25 August 2024).
- Cavier, R. Anthelmintic properties of piperazine and its derivatives. Ann. Pharm. Fr. 1955, 13, 539–556. [Google Scholar]
- De Boer, D.; Bosman, I.J.; Hidvégi, E.; Manzoni, C.; Benkö, A.A.; Dos Reys, L.J.A.L.; Maes, R.A.A. Piperazine-like compounds: A new group of designer drugs-of-abuse on the European market. Forensic Sci. Int. 2001, 121, 47–56. [Google Scholar] [CrossRef]
- Arbo, M.D.; Bastos, M.L.; Carmo, H.F. Piperazine compounds as drugs of abuse. Drug Alcohol Depend. 2012, 122, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Welz, A.; Koba, M. Piperazine derivatives as dangerous abused compounds. Acta Pharm. 2020, 70, 423–441. [Google Scholar] [CrossRef] [PubMed]
- PRISMA-P Group; Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Bernardo, W.M. PRISMA statement and PROSPERO. Int. Braz J Urol Off. J. Braz. Soc. Urol. 2017, 43, 383–384. [Google Scholar] [CrossRef]
- Wilkins, C.; Sweetsur, P.; Girling, M. Patterns of benzylpiperazine/trifluoromethylphenylpiperazine party pill use and adverse effects in a population sample in New Zealand. Drug Alcohol Rev. 2008, 27, 633–639. [Google Scholar] [CrossRef]
- Bossong, M.; Brunt, T.; Van Dijk, J.; Rigter, S.; Hoek, J.; Goldschmidt, H.; Niesink, R. mCPP: An undesired addition to the ecstasy market. J. Psychopharmacol. 2010, 24, 1395–1401. [Google Scholar] [CrossRef]
- Austin, H.; Monasterio, E. Acute Psychosis Following Ingestion of ‘Rapture’. Australas. Psychiatry 2004, 12, 406–408. [Google Scholar] [CrossRef]
- Thompson, I.; Williams, G.; Caldwell, B.; Aldington, S.; Dickson, S.; Lucas, N.; McDowall, J.; Weatherall, M.; Robinson, G.; Beasley, R. Randomised double-blind, placebo-controlled trial of the effects of the ‘party pills’ BZP/TFMPP alone and in combination with alcohol. J. Psychopharmacol. 2010, 24, 1299–1308. [Google Scholar] [CrossRef]
- Staack, R.F. Piperazine designer drugs of abuse. Lancet 2007, 369, 1411–1413. [Google Scholar] [CrossRef]
- Chiang, M.; Lombardi, D.; Du, J.; Makrum, U.; Sitthichai, R.; Harrington, A.; Shukair, N.; Zhao, M.; Fan, X. Methamphetamine-associated psychosis: Clinical presentation, biological basis, and treatment options. Hum. Psychopharmacol. Clin. Exp. 2019, 34, e2710. [Google Scholar] [CrossRef] [PubMed]
- Grant, K.M.; LeVan, T.D.; Wells, S.M.; Li, M.; Stoltenberg, S.F.; Gendelman, H.E.; Carlo, G.; Bevins, R.A. Methamphetamine-associated psychosis. J. Neuroimmune Pharmacol. Off. J. Soc. NeuroImmune Pharmacol. 2012, 7, 113–139. [Google Scholar] [CrossRef]
- Orsolini, L.; Chiappini, S.; Corkery, J.M.; Guirguis, A.; Papanti, D.; Schifano, F. The use of new psychoactive substances (NPS) in young people and their role in mental health care: A systematic review. Expert Rev. Neurother. 2019, 19, 1253–1264. [Google Scholar] [CrossRef] [PubMed]
- Martinotti, G.; Chiappini, S.; Mosca, A.; Miuli, A.; Santovito, M.C.; Pettorruso, M.; Skryabin, V.; Sensi, S.L.; Giannantonio, M.D. Atypical Antipsychotic Drugs in Dual Disorders: Current Evidence for Clinical Practice. Curr. Pharm. Des. 2022, 28, 2241–2259. [Google Scholar] [CrossRef]
- Chiappini, S.; Mosca, A.; Miuli, A.; Di Carlo, F.; d’Andrea, G.; Napolitano, A.; Santangelo, M.; Esposito, C.; Rosazza, A.; Haefele, E.; et al. Aripiprazole once monthly as a maintenance treatment for patients with schizophrenia and alcohol/substance use disorder: An observational, real-world study. Adv. Dual Diagn. 2023, 16, 185–198. [Google Scholar] [CrossRef]
- Chiappini, S.; Cavallotto, C.; Mosca, A.; Di Carlo, F.; Piro, T.; Giovannetti, G.; Pasino, A.; Vicinelli, M.; Lorenzini, C.; Di Paolo, M.; et al. Investigating the Effectiveness of Brexpiprazole in Subjects with Schizophrenia Spectrum Illness and Co-Occurring Substance Use Disorder: A Prospective, Multicentric, Real-World Study. Pharmaceuticals 2024, 17, 535. [Google Scholar] [CrossRef]
- Cavallotto, C.; Chiappini, S.; Mosca, A.; d’Andrea, G.; Di Carlo, F.; Piro, T.; Susini, O.; Stefanelli, G.; Di Cesare, A.; Ricci, V.; et al. Examining Lurasidone Efficacy in Patients with Schizophrenia Spectrum Illness and Concurrent Alcohol and Substance Use Disorder: A Prospective, Multicentric, Real-World Investigation. J. Clin. Med. 2024, 13, 2206. [Google Scholar] [CrossRef] [PubMed]
- Baldaçara, L.; Ramos, A.; Castaldelli-Maia, J.M. Managing drug-induced psychosis. Int. Rev. Psychiatry 2023, 35, 496–502. [Google Scholar] [CrossRef]
- Abdel-Baki, A.; Thibault, D.; Medrano, S.; Stip, E.; Ladouceur, M.; Tahir, R.; Potvin, S. Long-acting antipsychotic medication as first-line treatment of first-episode psychosis with comorbid substance use disorder. Early Interv. Psychiatry 2020, 14, 69–79. [Google Scholar] [CrossRef]
- Green, A.I.; Tohen, M.F.; Hamer, R.M.; Strakowski, S.M.; Lieberman, J.A.; Glick, I.; Scott Clark, W. First episode schizophrenia-related psychosis and substance use disorders: Acute response to olanzapine and haloperidol. Schizophr. Res. 2004, 66, 125–135. [Google Scholar] [CrossRef]
- Simonato, P.; Corazza, O.; Santonastaso, P.; Corkery, J.; Deluca, P.; Davey, Z.; Blaszko, U.; Schifano, F. Novel psychoactive substances as a novel challenge for health professionals: Results from an Italian survey. Hum. Psychopharmacol. Clin. Exp. 2013, 28, 324–331. [Google Scholar] [CrossRef]
- Orsolini, L.; Chiappini, S.; Papanti, D.; De Berardis, D.; Corkery, J.M.; Schifano, F. The Bridge Between Classical and “Synthetic”/Chemical Psychoses: Towards a Clinical, Psychopathological, and Therapeutic Perspective. Front. Psychiatry 2019, 10, 851. [Google Scholar] [CrossRef] [PubMed]
- Neicun, J.; Steenhuizen, M.; Van Kessel, R.; Yang, J.C.; Negri, A.; Czabanowska, K.; Corazza, O.; Roman-Urrestarazu, A. Mapping novel psychoactive substances policy in the EU: The case of Portugal, the Netherlands, Czech Republic, Poland, the United Kingdom and Sweden. PLoS ONE 2019, 14, e0218011. [Google Scholar] [CrossRef] [PubMed]
- Santos-Toscano, R.; Guirguis, A.; Davidson, C. How preclinical studies have influenced novel psychoactive substance legislation in the UK and Europe. Br. J. Clin. Pharmacol. 2020, 86, 452–481. [Google Scholar] [CrossRef]
- Nutt, D. New psychoactive substances: Pharmacology influencing UK practice, policy and the law. Br. J. Clin. Pharmacol. 2020, 86, 445–451. [Google Scholar] [CrossRef]
- Vicknasingam, B.; Narayanan, S.; Singh, D.; Corazza, O. Global strategy for New Psychoactive Substances: An update. Curr. Opin. Psychiatry 2020, 33, 295–300. Available online: https://pubmed.ncbi.nlm.nih.gov/32398543/ (accessed on 2 September 2024). [CrossRef]
- Wood, D.M.; Dargan, P.I. The challenge of the novel psychoactive substances: How have we responded and what are the implications of this response? Br. J. Clin. Pharmacol. 2020, 86, 407–409. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.L. Perspectives on the therapeutic potential of MDMA: A nation-wide exploratory survey among substance users. Front. Psychiatry 2023, 14, 1096298. [Google Scholar] [CrossRef]
- Australia to Allow MDMA-Assisted Therapy for PTSD-Alcohol and Drug Foundation [Internet]. Available online: https://adf.org.au/insights/mdma-ptsd/ (accessed on 25 August 2024).
- Mosca, A.; Chiappini, S.; Miuli, A.; Mancusi, G.; Santovito, M.C.; Di Carlo, F.; Pettorruso, M.; Corkery, J.M.; Canessa, C.; Martinotti, G.; et al. Ibogaine/Noribogaine in the Treatment of Substance Use Disorders: A Systematic Review of the Current Literature. Curr. Neuropharmacol. 2023, 21, 2178–2194. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).