Abstract
Alcohol use disorder (AUD) is a chronic and relapsing biopsychosocial condition that leads to various medical, psychological, social, economic, and personal issues. This study evaluated how sociodemographic characteristics, clinical variables, impulsivity dimensions, and cognitive functions were associated with quality of life (QoL) among patients seeking treatment for AUD. Furthermore, the study investigated the predictors of QoL among patients seeking treatment for AUD based on attention, cognitive instability, motor impulsiveness, perseverance, and self-control dimensions of trait impulsivity. This study also investigated the potential mediating effect of anxiety and alcohol use severity in this relationship. After an initial assessment, the participants underwent comprehensive evaluations, including sociodemographic data, clinical history, and QoL domains. The evaluations also covered AUD severity, impulsivity dimensions, cognitive functions, craving intensity, depression, anxiety, and self-efficacy. Multiple linear regression analyses were employed to identify associations between independent variables and QoL. The attention dimension of impulsivity and anxiety symptoms significantly predicted physical health domain of QoL. The self-control dimension and severity of alcohol use disorder predicted psychological domain of QoL. The indirect effect of attention dimension on physical health was significant [effect = −1.082, 95% CI (−2.008, −0.3598)]. The significance of impulsivity in influencing QoL for individuals with AUD has profound clinical implications. These findings underscore the importance of addressing anxiety and impulsivity in managing AUD, given their considerable impact, particularly on QoL, ultimately shaping treatment outcomes.
1. Introduction
Alcohol use disorder (AUD) is a chronic and relapsing biopsychosocial condition that leads to various medical, psychological, social, economic, and personal issues. This complex challenge not only affects physical health but also psychological well-being and overall quality of life. Problematic alcohol use is associated with various health problems such as liver cirrhosis, cardiovascular diseases, mental disorders, and increased risks of accidents and injuries [1]. In the year 2020, 1.03 billion males and 312 million females worldwide consumed harmful amounts of alcohol in excess of the non-drinker equivalence (NDE) and contributing to a total of 1.78 million deaths in the same year. Notably, alcohol consumption has emerged as the primary risk factor for mortality among males aged 15–49 years [2].
In 2016, approximately 43% of the global population aged 15 years and above were identified as current drinkers. This also contributed to the loss of 132.6 million disability-adjusted life years (DALYs), equivalent to 5.1% of the total DALYs for that year. Globally, harmful alcohol use ranks as the seventh leading cause of premature death and disability [3]. It is worth noting that the mortality caused by problematic alcohol use surpasses that caused by diseases such as tuberculosis, HIV/AIDS, and diabetes [1].
The goal of AUD recovery is not only to stop heavy drinking or to achieve abstinence but also to improve biopsychosocial functioning and quality of life. A sustained recovery process requires progress in these areas that are indicators of progress in recovery [4,5,6]. Therefore, researchers have expanded their studies to explore the impacts of AUD treatment on quality of life and nondrinking outcomes, beyond mere reductions in drinking [7]. The integration of behavioral and medical services, along with resilience and well-being, is increasingly being recognized as important to addressing chronic relapses in substance use disorders [8]. Consequently, improving quality of life (QoL) is now gaining attention in AUD treatment [7].
QoL is defined by the World Health Organization as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” [9]. Studies have found significant impairments of QoL in individuals with alcohol use disorder, particularly with respect to their physical health and psychological domains, compared with the general population [10,11]. The predictors of QoL among patients with alcohol use disorder under treatment have also been studied. Several factors predict baseline QoL, such as severity of alcohol use disorder, marital status, employment status, age, and personality disorders [12,13,14]. Recent studies have highlighted impulsivity, positive affect, anxiety, and craving as predictors of quality of life during treatment for AUD [15,16,17,18]. There is also evidence that various dimensions of impulsivity, including non-planning, attentional impulsivity, and motor impulsivity, are associated with well-being and health-related quality of life (HRQoL) in individuals recently detoxified from AUD [19].
Researchers have also found a relationship between the outcome of AUD treatment and quality of life, and they report that poorer outcomes are often associated with lower quality of life and more alcohol-related problems [20]. Improved outcomes during treatment are associated with improved QoL scores [21,22]. Studies indicate that behavioral interventions combined with anti-craving medication maintenance can improve treatment outcomes by improving QoL [14,23]. It appears that the outcome of treatment and QoL may be bidirectional, both during and after the treatment process.
Numerous behavioral models of impulsivity have been proposed in research. A comprehensive definition that encompasses these various viewpoints characterizes impulsivity as a tendency for quick, unplanned behaviors, disregarding the possible adverse outcomes [24]. The concept of impulsivity aligns with a few indicators of alcohol dependence and use disorder, outlined in both the International Classification of Diseases, Tenth Revision (ICD-10) and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (DSM-5) criteria. These indicators involve consuming more alcohol than initially intended and continuing to drink despite awareness of potential adverse outcomes.
Recent research suggests that impulsivity is a complex concept that can be viewed from different perspectives. It can be seen as a consistent personality trait or as a behavioral indicator of decision-making and actions. “Trait impulsivity” refers to a relatively stable form of impulsivity that is part of a person’s character. This aspect is usually evaluated using self-report questionnaires. On the other hand, “behavioral impulsivity” refers to patterns of impulsive behavior, assessed through objective measurements in various situations, often involving tasks [25,26]. The Barratt Impulsiveness Scale (BIS) developed by Patton et al. (1995) [27] and the Urgency-Premeditation-Perseverance-Sensation Seeking-Positive Urgency (UPPS-P) mpulsive Behavior Scale by Whiteside and Lynam (2001) [28] are self-report questionnaires used to assess impulsivity as a personality trait. These scales also identify various subcategories of impulsive traits through specific subsections. People with alcohol use disorder score higher on BIS than those without the disorder [29,30]. Earlier research has demonstrated a positive link between trait impulsivity and alcohol consumption [31,32,33]. Studies have also indicated a bidirectional relationship between impulsivity and alcohol use [34]. Individuals diagnosed with alcohol use disorder (AUD) who also exhibit comorbid gambling symptoms were found to have elevated levels of trait impulsivity and a propensity for non-planning behaviors. This association remains significant irrespective of factors such as intelligence, age, and psychopathological symptoms [35].
Impulsivity appears to play a significant role in the onset and progression of substance use disorder, either as an underlying susceptibility or because of prolonged substance abuse [36]. Moreover, there is evidence indicating that alcohol can influence impulsivity patterns over time [37]. Moreover, it has been observed that all three facets of impulsivity, encompassing ‘trait impulsivity’, ‘motor impulsivity’, and ‘impulsive choice impulsivity’, are associated with AUD relapse [38]. Cognitive behavioral therapies focused on addressing impulsivity can augment individuals’ ability to manage their alcohol consumption, thereby resulting in enhanced treatment outcomes. However, the absence of premeditation and the presence of high negative urgency have been associated with less favorable results in psychotherapy for substance use disorder (SUD) [39].
In AUD recovery, the emphasis on successful outcomes has primarily revolved around traditional measures such as decreased alcohol and drug consumption during treatment. However, there is a growing realization that overall QoL is a crucial aspect of recovery. Current AUD treatment and medication trials have focused on endpoints such as abstinence and reduced heavy drinking days. Hence, there is a need to assess the association between sociodemographic characteristics such as age, education, employment status, family type, marital status, and quality of life among individuals with AUD. Additionally, it is important to evaluate the correlation between clinical variables, including age at alcohol onset, duration of alcohol use, AUD severity, impulsivity dimensions, cognitive functions, craving intensity, depression, anxiety, self-efficacy, and quality of life (QoL). Identifying variables that can predict the quality of life during and after treatment for AUD would be beneficial for enhancing interventions and improving the treatment process.
This study evaluated how sociodemographic characteristics, clinical variables, impulsivity dimensions, and cognitive functions were associated with QoL among patients seeking treatment for AUD.
Furthermore, the study investigated the predictors of QoL among patients seeking treatment for AUD based on attention, cognitive instability, motor impulsiveness, perseverance, and self-control dimensions of trait impulsivity. This study also investigated the potential mediating effect of anxiety and alcohol use severity in this relationship. This study hypothesized that the attention, cognitive instability, motor impulsiveness, perseverance, and self-control dimensions of trait impulsivity would be predictive of all four domains of QoL. The second hypothesis was that anxiety and severity of alcohol use would mediate the effects of impulsivity dimensions on QoL.
2. Materials and Methods
2.1. Study Setting and Participants
This study was conducted at a leading substance use disorder treatment center in India. The 50-bed center is staffed by well-qualified multidisciplinary faculty and staff to provide various treatments. Recruitment for this study occurred between December 2018 and June 2020. At the time of recruitment, all patients were undergoing detoxification and remained in treatment as inpatients. Ethical approval was obtained from the Institute Ethics Committee of the All India Institute of Medical Sciences, New Delhi. Written informed consent was obtained from all study participants.
2.2. Inclusion and Exclusion
Inclusion criteria were as follows: (1) age between 18 and 60 years, (2) ability to read and write, (3) diagnosis of alcohol use disorder (AUD) as per the DSM-5, using the Mini-International Neuropsychiatric Interview (MINI)-Plus, (4) inpatient with a score of <7 on Clinical Institute Withdrawal Assessment of Alcohol Revised Scale (CIWA-Ar), and (5) a willingness to participate in the study. The exclusion criteria were as follows: (1) comorbid chronic physical illness, (2) comorbid psychotic or bipolar disorder, and (3) substance use disorders other than nicotine and alcohol, as per the DSM-5.
We recruited healthy controls who were matched with the study subjects in terms of age, sex, and socioeconomic status. The exclusion criteria were as follows: current or past psychiatric disorders, any substance use disorders other than nicotine, comorbid chronic physical illnesses, and Alcohol Use Disorders Identification Test (AUDIT) scores of 8 or higher. These control subjects were selected from the same neighborhoods or from within the close circle of friends of our study subjects, ensuring a suitable comparison group for the study.
2.3. Procedure
Before obtaining their informed consent, all participants were provided with a comprehensive overview of the entire research protocol. Following this, a thorough screening process was conducted to determine adherence to the specified inclusion and exclusion criteria. Once all criteria were met, patients were officially enrolled in the study. Subsequently, we conducted detailed assessments to collect the following information: all participants were assessed for sociodemographic data, including their name, age, gender, educational qualifications, occupation, family type, and residence type, and clinical characteristics including age at onset of alcohol use and duration and quantity of alcohol use.
Quality of life assessment: the World Health Organization Quality of Life-BREF (WHOQOL-BREF) questionnaire was used to evaluate participants’ quality of life.
Alcohol use disorder severity evaluation: the Alcohol Use Disorders Identification Test (AUDIT) was used to measure the severity of alcohol use disorder among participants.
Impulsivity measurement: the Barratt Impulsiveness Scale-11 (BIS-11) was administered to assess the levels of impulsivity exhibited by the participants.
Cognitive function assessment: cognitive functions were evaluated using the National Institute of Mental Health and Neuro Sciences (NIMHANS) Battery, which is a comprehensive battery of cognitive tests.
Craving evaluation: at baseline, the Obsessive Compulsive Drinking Scale (OCDS) was employed to measure the intensity of craving in relation to alcohol consumption.
Depressive symptom assessment: the Hamilton Depression Rating Scale (HAM-D) was used to quantify the presence and severity of depressive symptoms.
Anxiety symptom evaluation: the Hamilton Anxiety Rating Scale (HAM-A) was used to measure the extent and intensity of anxiety symptoms.
Self-efficacy examination: the Alcohol Abstinence Self-Efficacy (AASE) questionnaire was administered to assess participants’ beliefs regarding their ability to abstain from alcohol consumption.
- Instruments
- World Health Organization Quality of Life Brief Version (WHOQOL) Group, 1998) [9].
QoL was assessed using the World Health Organization Quality of Life Brief Version. This self-report tool comprises 25 items, measuring QoL across the following four domains: physical health, psychological social relationships, and environment. Responses are rated on a 5-point Likert scale, with higher scores indicating improved QoL. The WHOQOL-BREF has shown strong reliability and validity in previous studies.
- Barratt Impulsiveness Scale (BIS) [27]
The BIS is widely used to measure impulsivity in psychiatric studies. The BIS-11 version assesses three impulsivity domains, namely motor, cognitive, and non-planning. The study identified the following six first-order factors through principal component analysis (PCA): attention, motor, self-control, cognitive complexity, perseverance, and cognitive instability. A subsequent analysis revealed the following three higher-order factors: “motor impulsiveness”, “non-planning impulsiveness”, and “attentional impulsiveness”. While the BIS-11 (α = 0.83) and some factors demonstrated good reliability, such as non-planning impulsiveness (α = 0.72) and attentional impulsiveness (α = 0.74), motor impulsiveness had a lower reliability (α = 0.59). Among the first-order factors, only attention (α = 0.72) and self-control (α = 0.72) showed good reliability.
- Alcohol Use Disorders Identification Test (AUDIT) [40]
The AUDIT is a comprehensive assessment tool, comprising 10 items, which was meticulously crafted by the World Health Organization (WHO). This instrument was designed to thoroughly evaluate patterns of alcohol consumption, behaviors related to drinking, and the presence of alcohol-associated issues. Each of the 10 questions within the AUDIT framework is accompanied by a scale of responses, ranging from 0 to 4. Notably, questions 9 and 10 deviate slightly, offering responses on a scale of 0, 2, and 4. The scoring spectrum spans from 0 to 40, encompassing the gamut of potential responses. According to the discerning guidelines set forth by the World Health Organization (WHO), a score of 1 to 7 indicates consumption patterns associated with minimal risk. In contrast, scores between 8 and 14 signify a potential for hazardous or harmful alcohol use, whereas a score of 15 or higher raises concerns about the prospect of alcohol dependence, indicating a moderate to severe alcohol use disorder. Notably, individuals with the most profound severity, as classified by the DSM-5, consistently manifest notably elevated mean scores on the AUDIT, distinguishing them from those exhibiting less severe manifestations.
- Obsessive Compulsive Drinking Scale (OCDS) [41]
The OCDS is a 14-item questionnaire. It is a widely used tool to measure cravings for alcohol. It is a quick and reliable test that gives you a total score and two scores: one for obsessive cravings (based on questions 1–6) and another for compulsive cravings (based on questions 7–14). The OCDS has been tested in adults who have issues with alcohol use. The test–retest correlation for the OCDS total score was 0.96, and the test–retest correlations for the obsessive and compulsive subscales were 0.94 and 0.86, respectively. The internal consistency of the items in the OCDS is high (0.86).
- Alcohol Abstinence Self-Efficacy Scale (AASE) [42]
The AASE is a 20-item questionnaire that measures an individual’s self-confidence in abstaining from drinking in a range of situations. AASE demonstrated a solid subscale structure and strong indices of reliability and validity. The four 5-item subscales measured the types of relapse precipitants, labeled negative affect, social positive, physical and other concerns, and withdrawal and urges. Both in terms of structure and mean scores, the AASE demonstrated no substantive gender differences. AASE appears to represent a brief, easily usable, and psychometrically sound measure of an individual’s self-efficacy to abstain from drinking.
- NIMHANS Neuropsychological Battery for Cognitive Functions [43]
Cognitive functions were assessed using the NIMHANS Battery, including the Auditory Verbal Learning Test, Complex Figure Test, Verbal N Back Test, Digit Symbol Substitution Test, Animal Names Test, Stroop Test, and Wisconsin Card Sorting Test.
- Hamilton Anxiety Rating Scale (HAM-A) [44]
The HAM-A was one of the first tools created to measure the severity of anxiety symptoms. It is still used a lot today, in both medical and research settings. The tool has 14 questions, each describing a set of symptoms. It measures two types of anxiety: mental anxiety (feeling restless or distressed) and physical anxiety (having physical problems because of anxiety). The HAM-A does not have set questions for the person being tested. Even so, the results show that different testers achieve similar scores, which is good. Each question receives a score from 0 (no problem) to 4 (very serious). The total score can range from 0 to 56. Scores under 17 indicate mild anxiety, scores between 18 and 24 indicate mild to medium anxiety, and scores between 25 and 30 indicate medium to serious anxiety.
- Hamilton Depression Rating Scale (HAM-D) [45]
The HAM-D is the pre-eminent tool for evaluating depression under the guidance of clinicians. Comprising a set of 17 items, this assessment scale delves into the spectrum of depressive symptoms experienced over the previous week. The methodology for scoring varies across different iterations of the scale. In the context of HAM-D, a score ranging from 0 to 7 is conventionally interpreted as indicative of a state within the normal range or clinical remission. Conversely, a score of 20 or higher, denoting at least a moderate level of severity, is typically the threshold for eligibility in clinical trial enrollment.
2.4. Statistical Analysis
The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 25.0. p values < 0.05 were considered significant. Continuous variables were presented as mean and standard deviation (SD), whereas categorical variables were expressed as percentages. Within the WHOQOL-BREF scores (ranging from 0 to 100), an assessment was conducted for each domain, encompassing physical, psychological, social relationships, and environmental domains. To compare QoL scores between individuals with alcohol use disorder and non-user controls, an independent t-test was used, with significance set at a p value below 0.05. Categorical variables on sociodemographic and clinical characteristics were evaluated between the two groups using a chi-squared (X2) test, where significance was considered at a p value less than 0.05. A multiple linear regression analysis was performed to examine the relationship between the independent variables and QoL. Variables that exhibited a p value of less than 0.2 during the initial unadjusted analysis were simultaneously entered into the model using the “Enter” method, and unstandardized beta coefficients were estimated. Significance in this analysis was recognized as a p value of less than 0.05. Mediation analysis was conducted using the PROCESS Macro Model 4. The focus of this analysis was the physical health domain of QoL, with attention factor scores from the BIS-11 serving as the predictor variable and anxiety scores from the HAM-A serving as the mediator variable. The outcome of the analysis was assessed in terms of statistical significance.
2.5. Sample Size
In one scenario, assuming a pooled standard deviation of 3.95 units (raw score on WHOQOL-BREF scale for the physical health domain) and a design effect (DEFF) of 1.4, the study would require a sample size of 83 for the test group (individuals with alcohol use disorder) and 42 for the control group (i.e., a total sample size of 125, to ensure that the control group is 0.5 times larger than the test group) to achieve a power of 80% and a level of significance of 5% (two-sided), for detecting a true difference in means between the test and the control group of −2.5 (i.e., 21.45–23.95) units (raw score on WHOQOL-BREF scale for the physical health domain) [46]
In a second scenario, assuming a pooled standard deviation of 3.27 units (raw score on WHOQOL-BREF scale for the psychological health domain) and a design effect (DEFF) of 1.4, the study would require a sample size of 84 for the test group and 42 for the reference group (i.e., a total sample size of 126; to ensure that the reference group is 0.5 times larger than the test group) to achieve a power of 80% and a level of significance of 5% (two-sided), for detecting a true difference in means between the test and the reference group of −2.05 (i.e., 18.39–20.44) units (raw score on WHOQOL-BREF scale for the psychological health domain) [46].
Furthermore, we have conscientiously considered the recommendations regarding sample size, as put forth by Green (1991) [47]. Green’s guidance suggests that, for testing multiple correlation, a sample size of N > 50 + 8 m is advisable, with ‘m’ denoting the number of independent variables in question. This recommendation takes into account the expectation of a medium-sized relationship.
We chose to focus on the physical health and psychological domains of the WHOQOL-BREF scale as our variables of interest, based on a comprehensive review of existing literature. Consequently, following these calculations, we arrived at a total of 88 participants for the AUD group and 44 for the non-alcohol user healthy controls group.
In our study analysis, we converted WHOQOL-BREF raw scores into transformed scores on a scale of 0–100.
2.6. Ethical Approval
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Ethics Committee, All India Institute of Medical Sciences, New Delhi. The committee reference number was IEC-278/01.06.2018, RP-31/2018 dated 19 June 2018.
3. Results
All participants (n = 88) with alcohol use disorder were males, because no females with alcohol use disorder were admitted during the study period. Consequently, we were unable to recruit any female participants.
Table 1 and Table 2 present information obtained from participants with alcohol use disorder and non-alcohol user healthy controls. These tables compare the sociodemographic characteristics of non-alcohol user healthy controls and individuals with alcohol use disorder, as well as the QoL domains and BIS-11 dimensions between the two groups. The differences in QoL between individuals with alcohol use disorder and healthy controls were found to be statistically significant across the domains of physical health, psychology, and social relationships. However, no statistically significant difference was observed in the domain of the environment.

Table 1.
Comparison of demographic characteristics between non-alcohol user healthy controls and individuals with alcohol use disorder.

Table 2.
Comparison of QoL domains and BIS-11 dimensions between non-alcohol user healthy controls and individuals with alcohol use disorder.
Table 3 presents the sociodemographic characteristics of the participants with AUD and their association with QoL. Various variables were in relation to different domains of QoL. The average age of the participants with AUD was 37.55 years, with a standard deviation of 8.31. Among the participants, 43.2% (38) had received a school education, whereas 56.8% (50) had a college education. In terms of employment status, 36.4% (32) were unemployed, while 63.6% (56) were employed. Additionally, 45.5% (40) lived in joint family setups, while 54.5% (48) lived in nuclear family setups. Marital status indicated that 31.8% (28) were unmarried, and 63.6% (60 individuals) were married. Significant associations were observed between marital status and the social relationship domain of QoL. The mean QoL score for the social relationship domain was 47.29 (SD = 27.15) for unmarried individuals and 77.27 (SD = 15.98) for married individuals. This association was found to be statistically significant (p = 0.004). In addition, significant associations were observed between marital status and the psychological health domain of QoL. Additionally, no significant association was found between sociodemographic characteristics and the four domains of quality of life in non-alcohol-using healthy controls.

Table 3.
Sociodemographic characteristics of the participants with AUD and their association with quality of life (QoL) (measured with the WHOQOL-BREF) (n = 88).
Table 4 displays the descriptive statistics and correlation matrix for the study variables in participants with AUD. The table provides means, standard deviations (SD), and correlation coefficients between different variables. Correlations are denoted by coefficients ranging from −1 to 1, with positive values indicating a positive relationship and negative values indicating a negative relationship. Correlation coefficients marked with ** are significant at the 0.01 level (two-tailed), whereas those marked with * are significant at the 0.05 level (two-tailed). The table helps to understand the relationships between different variables and provides insights into potential associations between factors such as quality of life, impulsiveness, psychological measures, cognitive function, and alcohol-related assessments. The BIS-11 first order factor of attention exhibited significant correlations with the physical health (r = −0.655) and environment (r = −0.547) domains of QoL. Similarly, the BIS-11 first order factor of self-control demonstrated significant correlations with the domains of physical health (r = −0.343) and psychological health (r = −0.406) in the context of QoL. Scores on the Hamilton Depression Rating Scale (HAM-D) and Hamilton Anxiety Rating Scale (HAM-A) exhibited significant correlations with all four domains of QoL. Furthermore, the total scores from the Alcohol Use Disorders Identification Test were significantly correlated with the psychological health domain (r = −0.325) of QoL. The scores from the Obsessive Compulsive Drinking Scale displayed significant correlations with the environment (r = −0.388) and physical health (r = −0.388) domains of QoL. There were no significant correlations between any cognitive test assessment and the four QoL domains. The mean age of onset of alcohol use was found to be 20.11 years, with a standard deviation of 5.33. However, our study did not find a significant correlation between the age of onset of alcohol use and impulsivity. Furthermore, the scores derived from the Alcohol Abstinence Self-Efficacy Scale (Confident) demonstrated significant associations with both the psychological health domain (r = 0.345) and the relationships domain (r = 0.436) of QoL. Table 5 presents the correlation matrix for study variables in non-alcohol user healthy controls (n = 44). We did not find any significant correlations between various impulsivity dimensions and the four QoL domains in non-alcohol-using healthy controls. The findings from this study have been added to Table 3 for better clarity. In addition, no significant association was found between sociodemographic characteristics and the four domains of quality of life in non-alcohol-using healthy controls.

Table 4.
Descriptive statistics and correlation matrix of study variables in individuals with alcohol use disorder (n = 88).

Table 5.
Correlation matrix for study variables in non-alcohol user healthy controls (n = 44).
Table 6 presents the univariate and multivariate linear regression analyses used to identify predictors of quality of life (WHOQOL-BREF) among individuals undergoing detoxification for alcohol use disorder.

Table 6.
Univariate and multivariate linear regression analyses to identify predictors of quality of life (WHOQOL-BREF) among individuals undergoing detoxification for alcohol use disorder (n = 88).
A multiple linear regression analysis was conducted to predict the physical health domain of QoL. The predictor variables included the attention dimension scores of the BIS-11, the self-control dimension scores of the BIS-11, and scores from the HAM-A and HAM-D scales. The results revealed a statistically significant regression equation (F(4, 83) = 13.87, p < 0.000), with an R-squared value of 0.587. Both attention dimension scores of BIS and anxiety scores of HAM-A were significant predictors of the physical health domain of QoL. These predictors demonstrated that higher scores on attention dimension of the BIS-11 and elevated anxiety scores of HAM-A were associated with lower scores in the physical health domain of QoL. Mediation analysis was performed using PROCESS Macro. The outcome variable for analysis was physical health domain of QoL. The predictor variable for the analysis was attention dimension scores of BIS-11. The mediator variable for the analysis was anxiety scores of HAM-A. The indirect effect of the attention dimension scores from BIS -11 on the physical health domain of QoL was found to be statistically significant [effect = −1.082, 95% CI (−2.008, −0.3598)], and the results are comprehensively presented in Table 7. Importantly, these effects were found to be partially mediated by anxiety scores, as depicted in Figure 1.

Table 7.
Results of mediation analysis performed using PROCESS Macro.
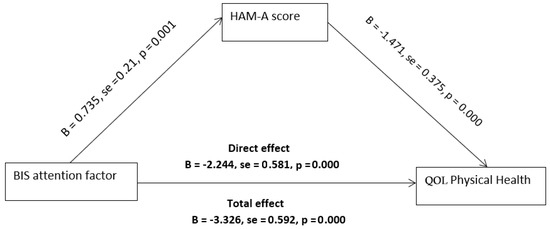
Figure 1.
Mediation analysis: BIS—attention -> HAM-A score -> QoL—physical health.
A multiple linear regression analysis was conducted to predict the psychological health domain of quality of life. The predictor variables included attention dimension scores of BIS-11, self-control dimension scores of BIS-11, scores from the HAM-A scale, scores from the HAM-D scale, and total scores from the AUDIT. The analysis revealed a statistically significant regression equation (F(5, 82) = 5.258, p < 0.001), with an R-squared value of 0.409. Both self-control factor scores on BIS and AUDIT scores were significant predictors of the psychological health domain of quality of life. This indicated that higher self-control dimension scores on the BIS-11 and greater severity of alcohol use, as indicated by higher AUDIT scores, were linked to lower scores on the psychological health domain of quality of life. The mediation analysis was performed using PROCESS Macro. The outcome variable for analysis was the psychological health domain of QoL. The predictor variable for the analysis was self-control dimension scores of BIS-11. The mediator variable for the analysis was alcohol use severity measured by AUDIT. The indirect effect of self-control dimension scores of BIS-11 on the psychological health domain of QoL was not found to be statistically significant [effect = 0.303 95% (−0.273, 0.900)], as demonstrated in Figure 2. The results are comprehensively presented in Table 5.
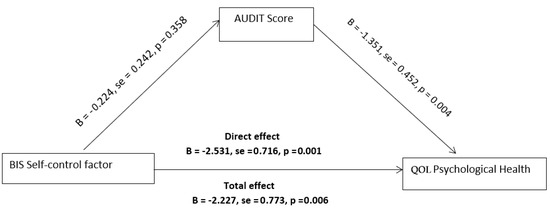
Figure 2.
Mediation analysis: BIS—self-control -> AUDIT score -> QOL—psychological health.
A multiple linear regression analysis was conducted to predict the quality of life within the social relationships domain. The predictive factors included scores from the attention dimension of BIS-11, HAM-A scores, HAM-D scores, and marital status. The results revealed a statistically significant regression equation (F(4, 83) = 3.655, p < 0.013) with an R-squared value of 0.273. The predicted quality of life score in the social relationships domain of QoL for participants was estimated using the following formula: 51.526 − 1.332 (BIS—attention) − 1.903 (HAM-D) − 0.123 (HAM-A) + 18.1 (marital status). It is important to note that all independent variables were measured on a continuous scale, except for marital status, which was coded as one for unmarried and two for married participants. Remarkably, marital status emerged as the sole significant predictor of quality of life in the social relationships domain. Married participants exhibited a notable increase of 18.1 points in their quality of life in social relationships domain scores compared with unmarried participants.
A multiple linear regression analysis was conducted to assess the relationship between the quality of life in the environment domain of QoL and several variables, including the attention dimension scores from BIS-11, self-control dimension scores from BIS-11, HAM-A scores, HAM-D scores, OCDS scores, and AASE scores. The results revealed a statistically significant regression equation (F(6, 81) = 7.235, p < 0.001), with an R-squared value of 0.540. The predicted environment domain QoL score for participants can be calculated using the following equation: 104.098 − 0.887 (BIS—attention) − 1.041 (BIS—self-control) − 0.475 (HAM-D) − 1.360 (HAM-A) − 0.090 (OCDS score) + 0.140 (AASE), where all the independent variables were measured on a continuous scale. No independent variables were found to be significant predictors of quality of life in the environment domain.
4. Discussion
This study evaluated how sociodemographic characteristics, clinical variables, impulsivity dimensions, and cognitive functions were associated with quality of life (QoL) among patients seeking treatment for AUD. Furthermore, the study investigated the predictors of QoL among patients seeking treatment for AUD based on attention, cognitive instability, motor impulsiveness, perseverance, and self-control dimensions of trait impulsivity. This study also investigated the potential mediating effect of anxiety and alcohol use severity in this relationship. These scores were then compared with those of demographically matched healthy individuals who did not consume alcohol. We also explored the correlations between domains of QoL and sociodemographic, cognitive, and clinical factors, to identify the most significant predictors of QoL.
The differences in QoL between individuals with alcohol use disorder and healthy controls who did not consume alcohol were found to be statistically significant across domains of physical health, psychological, and social relationships. However, no statistically significant difference was observed in the domain of environment. The psychological health domain exhibited the lowest mean score, followed by the mean score in the physical health domain among individuals with alcohol use disorder. These findings are consistent with previous studies that have documented diminished scores in the psychological and physical health domains [12,18,48]. However, a deviation from these findings was observed in a separate study by Olickal et al. (2021), which reported the highest mean (SD) score in the physical domain when compared to other QoL domains [18]. This discrepancy in our findings could be attributed to variations in the study setting and the characteristics of the study subjects, including the inclusion of patients experiencing severe addiction and undergoing inpatient detoxification. Patients with AUD demonstrated higher mean scores on impulsivity factors assessed by the BIS-11 compared with the control group, aligning with findings from prior research [29,30].
Marital status exhibited a significant association with the social relationships domain of QoL among individuals with alcohol use disorder. Married individuals with AUD showed a notable positive effect on the social relationships domain of QoL. This observation aligns with prior research that highlights the beneficial effects of cohabitation with a partner on the social functioning aspect of QoL [49,50]. Conversely, factors such as age and education did not demonstrate any correlation with the various domains of QoL within this study, which is consistent with findings from earlier investigations [50]. It is worth noting, however, that, contrary to these results, other studies have presented evidence indicating that advancing age [51] and lower educational attainment [14] do indeed exert a negative impact on QoL.
Our findings did not show any significant correlation between cognitive abilities and QoL. In prior studies, the relationship between anxiety/depressive symptoms and QoL in individuals with AUD was examined. These studies indicated that both depression and anxiety could contribute to diminished QoL among patients with AUD [17,52,53]. Consistent with these findings, we observed a significant correlation between anxiety/depressive symptoms and various QoL domains. Thus, individuals with AUD who experience more pronounced symptoms of depression and anxiety are likely to have a lower QoL. Consistent with prior research conducted in the context of AUD and binge drinking, our study revealed a significant correlation between the psychological health domain of QoL and the AUDIT scores. However, in contrast to earlier studies, we did not identify any significant correlation between the age of onset of alcohol use and QoL [54,55]. This relationship indicates that the extent of AUD severity is negatively correlated with the psychological domain of QoL.
A multivariate linear regression was conducted, using the four domains of QoL as dependent variables to identify the predictors of QoL. Notably, the dimensions of impulsivity that showed significant predictive power were the attention and self-control dimensions of impulsivity.
The predictive equation for participants’ scores of their physical health domain of quality of life was determined as follows: Y = 92.111 − 2.272 (BIS—attention) − 0.101 (BIS—self-control) − 0.393 (HAM-D) − 1.642 (HAM-A), where all independent variables were measured as continuous on a scale. Notably, a one-unit increase in attention factor scores on BIS-11 led to a significant decrease of 2.272 units in the participants’ predicted scores for physical health domain of quality of life. Similarly, a one-unit increase in HAM-A scores resulted in a substantial decrease in 1.642 units in the predicted score for the physical health domain of quality of life. Both the attention factor scores of BIS-11 and the anxiety score of HAM-A were significant predictors of the physical health domain of quality of life. The equation representing the prediction of participants’ psychological domain of quality of life was determined as follows: predicted psychological health = 116.30 − 0.083 (BIS—attention) − 1.941 (BIS—self-control) − 0.188 (HAM-D) − 1.112 (HAM-A) − 1.053 (AUDIT score). All independent variables were measured as continuous values on a scale. Notably, a one-unit increase in self-control factor scores on the BIS-11 led to a significant decrease of 1.941 units in participants’ predicted scores for the physical health domain of quality of life. Similarly, a one-unit increase in AUDIT scores decreased 1.053 units in the predicted score for the psychological domain of quality of life.
Specifically, attention dimension was found to be a predictor of physical QoL, whereas self-control was associated with psychological QoL. This finding aligns with a previous study [17,19]. It is worth mentioning that the study’s results diverged from those of Reichl et al. (2022) [19], as the motor dimension of impulsivity did not emerge as a significant predictor across QoL domains. This discrepancy could potentially be attributed to methodological differences in measurement tools—our study employed the BIS-11, whereas Reichl et al. (2022) [19] utilized alternative tasks for assessment. A plausible explanation for how the attention and self-control dimensions of impulsivity are linked to a diminished quality of life is as follows: the inability to plan ahead and involve oneself in intricate tasks (self-control impulsivity) can pose challenges in making purposeful choices and restoring a stable overall functioning, encompassing aspects such as employment and financial stability. Concurrently, a deficiency in focus (attentional impulsivity) may hinder an individual’s ability to stay present and prevent persistent rumination. Nevertheless, it is essential for future research endeavors to validate this conjecture.
Anxiety symptoms, as measured by the HAM-A scale, were found to predict the physical domain of QoL. This finding aligns with previous research, which indicated that both impulsivity and anxiety were predictors of QoL among individuals with AUD [17]. Moreover, using PROCESS Model 4 analysis, a significant indirect correlation was established. This link correlated the attention dimension of impulsivity with the physical QoL domain through anxiety symptoms. It is important to note that the partial mediation effect was notable specifically for the physical health domain of QoL. Therefore, higher scores on the attention dimension of impulsivity could result in heightened anxiety symptoms, subsequently increasing the likelihood of a lower level of physical health domain of QoL. Studies have shown that anxiety significantly affects the quality of life in individuals with AUD [56]. Anxiety and AUD can influence each other in a two-way manner. Some people with anxiety disorders may turn to alcohol as a way to self-medicate and manage their symptoms. This can, in turn, increase the risk of developing AUD [57]. On the other hand, research has also demonstrated that AUD can lead to the emergence of anxiety symptoms [58,59]. As a result, addressing anxiety becomes a crucial consideration when treating individuals with AUD. Moreover, it has been noted that several proximal factors are associated with regular alcohol consumption. These factors include emotional regulation and early tobacco use. Addressing these determinants could significantly aid the management of individuals with AUD [60].
The severity of AUD as measured by AUDIT was found to predict the psychological domain of QoL. However, being married was found to have a positive impact, acting as a protective factor for the social relationship domain of QoL. There was an observed negative correlation between QoL scores and AUDIT scores, with the AUDIT score standing out as a predictor of the psychological health domain of QoL. However, we did not identify a significant indirect correlation between the self-control dimension of impulsivity and the psychological domain of QoL through the severity of AUD.
There are a few notable limitations associated with this study. First, the use of a small sample size poses a significant constraint. Such small sample sizes can substantially diminish the statistical power of the study findings, necessitating a cautious interpretation of the results. Additionally, the study’s limitation arises from the fact that it was conducted at a single center, to which no female individuals with alcohol use disorder were admitted during the study period. Therefore, we could not recruit any female participants in our research. This limitation raises concerns about the representativeness of the study of a wider population and more diverse settings.
These limitations hinder the external validity and generalizability of the findings and necessitate a careful interpretation of the results. To mitigate these limitations, future research endeavors should consider employing a larger sample size and adopting a multicentric approach. By doing so, researchers can bolster the statistical power of their studies, thereby enhancing the reliability and generalizability of the results. In conclusion, future investigations in this area should involve a commitment to larger and more diverse samples, ultimately enabling a more comprehensive understanding of the subject matter.
Clinical Implications
Furthermore, the role of impulsivity in determining QoL for patients with AUD is highly significant from a clinical standpoint. Notably, various studies have indicated that impulsivity is not only linked to the initial development of AUD [61], but also contributes to the likelihood of relapse [62], even following periods of abstinence [63]. Given these findings, when dealing with AUD, it is essential to consider both anxiety and impulsivity due to their impact, particularly through their influence on QoL, on the outcome of treatment. Along with medications, various approaches, such as engaging in physical activity [64] or practicing meditation [65], could be suggested, to help control anxiety and impulsivity in people with AUD.
5. Conclusions
AUD is a chronic biopsychosocial condition that leads to various health and life challenges. The study, conducted at a prominent Indian treatment centre from December 2018 to June 2020, gathered data on demographics, AUD severity, impulsivity, cognitive function, craving, emotional well-being, and self-efficacy. The analysis showed that the attention dimension of impulsivity and anxiety predicted the physical health domain of QoL, while the self-control dimension and the severity of alcohol use disorder predicted the psychological domain of QoL. The attention dimension of impulsivity indirectly affected the physical health domain of QoL. The significance of impulsivity in influencing QoL for individuals with AUD holds substantial clinical importance. Remarkably, impulsivity plays a dual role—it is not only intertwined with the initial onset of AUD but also exerts a notable influence on the probability of relapse. These findings underscore the imperative of considering both anxiety and impulsivity in the context of AUD management. This consideration becomes pivotal because of their profound effects, notably through their sway over QoL, ultimately shaping the treatment outcomes.
Author Contributions
P.D.: funding acquisition, conceptualization, methodology, project administration, formal analysis, resources, validation, writing—original draft, writing—review and editing. G.S.K.: methodology (supporting) and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by a research grant (DST/CSRI/2017/149) from the Department of Science and Technology, Government of India under the Cognitive Science Research Initiative (CSRI).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Institute Ethics Committee of the All India Institute of Medical Sciences, New Delhi. Committee Reference number: IEC-278/01.06.2018, RP-31/2018, dated 19 June 2018.
Informed Consent Statement
All subjects gave their informed consent for inclusion before they participated in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Acknowledgments
We want to thank all patients who agreed to participate in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018.
- GBD 2020 Alcohol Collaborators. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: A systematic analysis for the Global Burden of Disease Study 2020. Lancet 2022, 400, 185–235. [Google Scholar] [CrossRef] [PubMed]
- BD 2016 Alcohol Collaborators. Alcohol use and burden for195 countries and territories, 1990–2016: A systematic analysis forthe Global Burden of Disease Study 2016. Lancet 2016, 392, 1015–1035. [Google Scholar]
- Hagman, B.T.; Falk, D.; Litten, R.; Koob, G.F. Defining recovery from alcohol use disorder: Development of an NIAAA research definition. Am. J. Psychiatry 2022, 179, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.F.; Greene, M.C.; Bergman, B.G. Beyond abstinence: Changes inindices of quality of life with time in recovery in a nationally rep-resentative sample of US adults. Alcohol Clin. Exp. Res. 2018, 42, 770–780. [Google Scholar] [CrossRef]
- Laudet, A.B. The case for considering quality of life in addiction research and clinical practice. Addict. Sci. Clin. Pract. 2011, 6, 44–55. [Google Scholar] [PubMed]
- Kirouac, M.; Stein, E.R.; Pearson, M.R.; Witkiewitz, K. Viability of the World Health Organization quality of life measure to assess changes in quality of life following treatment for alcohol use disorder. Qual. Life Res. 2017, 26, 2987–2997. [Google Scholar] [CrossRef]
- Dennis, M.; Scott, C.K. Managing addiction as a chronic condition. Addict. Sci. Clin. Pract. 2007, 4, 45. [Google Scholar] [CrossRef]
- Group WHOQOL. Measuring Quality of Life; The World Health Organization: Geneva, Switzerland, 1997; pp. 1–13. [Google Scholar]
- Donovan, D.; Mattson, M.E.; Cisler, R.A.; Longabaugh, R.; Zweben, A. Quality of life as an outcome measure in alcoholism treatment research. J. Stud. Alcohol. Suppl. 2005, 15, 119–139. [Google Scholar] [CrossRef]
- Volk, R.J.; Cantor, S.B.; Steinbauer, J.R.; Cass, A.R. Alcohol use disorders, consumption patterns, and health-related quality of life of primary care patients. Alcohol Clin. Exp. Res. 1997, 21, 899–905. [Google Scholar] [CrossRef]
- Colpaert, K.; De Maeyer, J.; Broekaert, E.; Vanderplasschen, W. Impact of addiction severity and psychiatric comorbidity on the quality of life of alcohol-, drug-and dual-dependent persons in residential treatment. Eur. Addict. Res. 2012, 19, 173–183. [Google Scholar] [CrossRef]
- Goldstein, R.B.; Dawson, D.A.; Smith, S.M.; Grant, B.F. Antisocial behavioral syndromes and 3-year quality-of-life outcomes in United States adults. Acta Psychiatr. Scand. 2012, 126, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M.Y.; Landron, F.; Lehert, P.; New European AlcoholismTreatment Study Group. Improvement in quality of life after treatment for alcohol dependence with acamprosate and psychosocialsupport. Alcohol Clin. Exp. Res. 2004, 28, 64–77. [Google Scholar] [CrossRef]
- Carlon, H.A.; Hurlocker, M.C.; Witkiewitz, K. Mechanisms of quality-of-life improvement in treatment for alcohol use disorder. J. Consult. Clin. Psychol. 2022, 90, 601–612. [Google Scholar] [CrossRef]
- Chamberlain, S.R.; Grant, J.E. Relationship between quality of life in young adults and impulsivity/compulsivity. Psychiatry Res. 2019, 271, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Lahbairi, N.; Laniepce, A.; Segobin, S.; Cabé, N.; Boudehent, C.; Vabret, F.; Rauchs, G.; Pitel, A.L. Determinants of health-related quality of life in recently detoxified patients with severe alcohol use disorder. Health Qual. Life Outcomes 2022, 20, 149. [Google Scholar] [CrossRef]
- Olickal, J.J.; Saya, G.K.; Selvaraj, R.; Chinnakali, P. Association of alcohol use with quality of life (QoL): A community based study from Puducherry, India. Clin. Epidemiol. Glob. Health 2021, 10, 100697. [Google Scholar] [CrossRef]
- Reichl, D.; Enewoldsen, N.; Weisel, K.K.; Fuhrmann, L.; Lang, C.; Saur, S.; Berking, M.; Zink, M.; Ahnert, A.; Falkai, P.; et al. Association of impulsivity with quality of life and well-being after alcohol withdrawal treatment. J. Clin. Psychol. 2022, 78, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- LoCastro, J.S.; Youngblood, M.; Cisler, R.A.; Mattson, M.E.; Zweben, A.; Anton, R.F.; Donovan, D.M. Alcohol treatment effects on secondary nondrinking outcomes and quality of life: The COMBINE Study. J. Stud. Alcohol Drugs 2009, 70, 186–197. [Google Scholar] [CrossRef]
- Daeppen, J.-B.; Faouzi, M.; Sanchez, N.; Rahhali, N.; Bineau, S.; Bertholet, N. Quality of life depends on the drinking pattern in alcohol-dependent patients. Alcohol Alcohol. 2014, 49, 457–465. [Google Scholar] [CrossRef]
- Witkiewitz, K.; Kranzler, H.R.; Hallgren, K.A.; O’Malley, S.S.; Falk, D.E.; Litten, R.Z.; Hasin, D.S.; Mann, K.F.; Anton, R.F. Drinking risk level reductions associated with improvements in physical health and quality of life among individuals with alcohol use disorder. Alcohol Clin. Exp. Res. 2018, 42, 2453–2465. [Google Scholar] [CrossRef]
- Prisciandaro, J.J.; DeSantis, S.M.; Bandyopadhyay, D. Simultaneous modeling of the impact of treatments on alcohol consumption and quality of life in the COMBINE study: A coupled hidden Markov analysis. Alcohol Clin. Exp. Res. 2012, 36, 2141–2149. [Google Scholar] [CrossRef]
- Moeller, F.G.; Barratt, E.S.; Dougherty, D.M.; Schmitz, J.M.; Swann, A.C. Psychiatric Aspects of Impulsivity. Am. J. Psychiatry 2001, 158, 1783–1793. [Google Scholar] [CrossRef] [PubMed]
- Broos, N.; Schmaal, L.; Wiskerke, J.; Kostelijk, L.; Lam, T.; Stoop, N.; Weierink, L.; Ham, J.; de Geus, E.J.C.; Schoffelmeer, A.N.M.; et al. The relationship between impulsive choice and impulsive action: A cross-species translational study. PLoS ONE 2012, 7, e36781. [Google Scholar] [CrossRef]
- Herman, A.M.; Critchley, H.D.; Duka, T. The role of emotions and physiological arousal in modulating impulsive behaviour. Biol. Psychol. 2018, 133, 30–43. [Google Scholar] [CrossRef]
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor structure of the Barratt Impulsiveness Scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Whiteside, S.P.; Lynam, D.R. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personal. Individ. Differ. 2001, 30, 669–689. [Google Scholar] [CrossRef]
- Ketzenberger, K.E.; Forrest, L. Impulsiveness and compulsiveness in alcoholics and nonalcoholics. Addict. Behav. 2007, 25, 791–795. [Google Scholar] [CrossRef]
- von Diemen, L.; Bassani, D.G.; Fuchs, S.C.; Szobot, C.M.; Pechansky, F. Impulsivity, age of first alcohol use and substance use disorders among male adolescents: A population based case-control study. Addiction 2008, 103, 1198–1205. [Google Scholar] [CrossRef]
- Adams, Z.W.; Kaiser, A.J.; Lynam, D.R.; Charnigo, R.J.; Milich, R. Addictive Behaviors drinking motives as mediators of the impulsivity-substance use relation: Pathways for negative urgency, lack of premeditation, and sensation seeking. Addict. Behav. 2012, 37, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Coskunpinar, A.; Dir, A.L.; Cyders, M.A. Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcohol Clin. Exp. Res. 2013, 37, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Stephan, R.A.; Alhassoon, O.M.; Allen, K.E.; Wollman, S.C.; Hall, M.; Thomas, W.J.; Gamboa, J.M.; Kimmel, C.; Stern, M.; Sari, C.; et al. Meta-analyses of clinical neuropsychological tests of executive dysfunction and impulsivity in alcohol use disorder. Am. J. Drug Alcohol Abus. 2017, 43, 24–43. [Google Scholar] [CrossRef] [PubMed]
- De Wit, H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addict. Biol. 2009, 14, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kovács, I.; Demeter, I.; Janka, Z.; Demetrovics, Z.; Maraz, A.; Andó, B. Different aspects of impulsivity in chronic alcohol use disorder with and without comorbid problem gambling. PLoS ONE 2020, 15, e0227645. [Google Scholar] [CrossRef]
- Jentsch, J.D.; Ashenhurst, J.R.; Cervantes, M.C.; Groman, S.M.; James, A.S.; Pennington, Z.T. Dissecting impulsivity and its relationships to drug addictions. Ann. N. Y. Acad. Sci. 2015, 1327, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, A.; Bonsu, J.A.; Charnigo, R.J.; Milich, R.; Lynam, D.R. Impulsive personality and alcohol use: Bidirectional relations over one year. J. Stud. Alcohol Drugs 2016, 77, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Sliedrecht, W.; Roozen, H.G.; Witkiewitz, K.; de Waart, R.; Dom, G. The Association Between Impulsivity and Relapse in Patients With Alcohol Use Disorder: A Literature Review. Alcohol Alcohol. 2021, 56, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Hershberger, A.R.; Um, M.; Cyders, M.A. The relationship between the UPPS-P impulsive personality traits and substance use psychotherapy outcomes: A meta-analysis. Drug Alcohol Depend. 2017, 178, 408–416. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De la Fuente, J.R.; Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Anton, R.F. Obsessive–compulsive aspects of craving: Development of the Obsessive Compulsive Drinking Scale. Addiction 2000, 95, 211–217. [Google Scholar] [CrossRef]
- DiClemente, C.C.; Carbonari, J.P.; Montgomery, R.P.; Hughes, S.O. The Alcohol Abstinence Self-Efficacy scale. J. Stud. Alcohol 1994, 55, 141–148. [Google Scholar] [CrossRef]
- Gopukumar, K.; Rao Shobini, L.; Subbakrishna, D.K. NIMHANS neuropsychology battery. Natl. Inst. Ment. Health Neuro Sci. Bangalore 2004. [Google Scholar]
- Hamilton, M. Hamilton anxiety rating scale (HAM-A). J. Med. 1959, 61, 81–82. [Google Scholar]
- Hamilton, M. Hamilton Rating Scale for Depression (HRSD)-17 items. Br. J. Soc. Clin. Psychol. 1967, 6, 278–296. [Google Scholar] [CrossRef]
- Srivastava, S.; Bhatia, M.S. Quality of life as an outcome measure in the treatment of alcohol dependence. Ind. Psychiatry J. 2013, 22, 41–46. [Google Scholar] [CrossRef]
- Green, S.B. How Many Subjects Does It Take To Do A Regression Analysis. Multivar. Behav. Res. 1991, 26, 499–510. [Google Scholar] [CrossRef]
- Chen, C.Y.; Storr, C.L. Alcohol use and health-related quality of life among youth in Taiwan. J. Adolesc. Health 2006, 39, 752.e9–752.e16. [Google Scholar] [CrossRef]
- Nogueira, J.M.; Rodríguez-Míguez, E. Using the SF-6D to measure the impact of alcohol dependence on health-related quality of life. Eur. J. Health Econ. 2015, 16, 347–356. [Google Scholar] [CrossRef]
- Manning, V.; Gomez, B.; Guo, S.; Low, Y.D.; Koh, P.K.; Wong, K.E. An Exploration of Quality of Life and its Predictors in Patients with Addictive Disorders: Gambling, Alcohol and Drugs. Int. J. Ment. Health Addict. 2012, 10, 551–562. [Google Scholar] [CrossRef]
- Lahmek, P.; Berlin, I.; Michel, L.; Berghout, C.; Meunier, N.; Aubin, H.-J. Determinants of improvement in quality of life of alcohol-dependent patients during an inpatient withdrawal programme. Int. J. Med. Sci. 2009, 6, 160–167. [Google Scholar] [CrossRef]
- Anker, J.J.; Kushner, M.G. Co-Occurring Alcohol Use Disorder and Anxiety: Bridging Psychiatric, Psychological, and Neurobiological Perspectives. Alcohol Res. 2019, 40, arcr.v40.1.03. [Google Scholar] [CrossRef]
- Saatcioglu, O.; Yapici, A.; Cakmak, D. Quality of life, depression and anxiety in alcohol dependence. Drug Alcohol Rev. 2008, 27, 83–90. [Google Scholar] [CrossRef]
- Fischer, J.A.; Najman, J.M.; Plotnikova, M.; Clavarino, A.M. Quality of life, age of onset of alcohol use and alcohol use disorders in adolescence and young adulthood: Findings from an Australian birth cohort. Drug Alcohol Rev. 2015, 34, 388–396. [Google Scholar] [CrossRef]
- Solomon, M.A.T.; Sabari, S.O.T.; Srinivasan, B. Correlation between Age of Alcohol Dependence and Quality of Life—A Hospital Based Cross Sectional Study. 2018. Available online: https://imsear.searo.who.int/jspui/handle/123456789/187032 (accessed on 14 December 2020).
- Choi, S.W.; Na, R.H.; Kim, H.O.; Choi, S.B.; Choi, Y.S. The relationship between quality of life and psycho-socio-spiritual characteristics in male patients with alcohol dependence. J. Korean Neuropsychiatr. Assoc. 2006, 45, 459–467. [Google Scholar]
- Smith, J.P.; Randall, C.L. Anxiety and alcohol use disorders: Comorbidity and treatment considerations. Alcohol Res. 2012, 34, 414–431. [Google Scholar]
- Flensborg-Madsen, T.; Mortensen, E.L.; Knop, J.; Becker, U.; Sher, L.; Grønbaek, M. Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: Results from a Danish register-based study. Compr. Psychiatry 2009, 50, 307–314. [Google Scholar] [CrossRef]
- Schneier, F.R.; Foose, T.E.; Hasin, D.S.; Heimberg, R.G.; Liu, S.M.; Grant, B.F.; Blanco, C. Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2010, 40, 977–988. [Google Scholar] [CrossRef]
- Heijdra Suasnabar, J.M.; Nadkarni, A.; Palafox, B. Determinants of alcohol use among young males in two Indian states: A population-based study. Trop. Med. Int. Health 2023, 28, 660–676. [Google Scholar] [CrossRef]
- Shin, S.H.; Hong, H.G.; Jeon, S.-M. Personality and Alcohol Use: The Role of Impulsivity. Addict. Behav. 2012, 37, 102–107. [Google Scholar] [CrossRef]
- Petit, G.; Cimochowska, A.; Kornreich, C.; Hanak, C.; Verbanck, P.; Campanella, S. Neurophysiological correlates of response inhibition predict relapse in detoxified alcoholic patients: Some preliminary evidence from event-related potentials. Neuropsychiatr. Dis. Treat. 2014, 10, 1025–1037. [Google Scholar] [PubMed]
- Salgado, J.V.; Malloy-Diniz, L.F.; Campos, V.R.; Abrantes, S.S.C.; Fuentes, D.; Bechara, A.; Correa, H. Neuropsychological assessment of impulsive behavior in abstinent alcohol-dependent subjects. Rev. Bras. Psiquiatr. 2009, 31, 4–9. [Google Scholar] [CrossRef][Green Version]
- Cabé, N.; Lanièpce, A.; Pitel, A.L. Physical activity: A promising adjunctive treatment for severe alcohol use disorder. Addict. Behav. 2021, 113, 106667. [Google Scholar] [CrossRef]
- Gallo, G.G.; Curado, D.F.; Opaleye, E.S.; Donate, A.P.G.; Scattone, V.V.; Noto, A.R. Impulsivity and Mindfulness among Inpatients with Alcohol Use Disorder. Subst. Use Misuse 2020, 24, 25–32. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).