Neuropsychological Insights into Coping Strategies: Integrating Theory and Practice in Clinical and Therapeutic Contexts
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Classification of Coping
3.1.1. The Nature and Measurement of Coping Strategies
3.1.2. Tools for Systematic Understanding and Assessment
3.2. Coping Strategies in Neuropsychology: A Multifaceted Exploration
3.2.1. Stress Mechanisms and Coping
3.2.2. Coping Strategies via the Neuropsychological Approach
Cognitive Coping Strategies
- Mental and physical distraction: Focusing on constructive tasks such as counting, visualizing, writing, and reminiscing can draw attention away from anxiety [97,98]. Physical activities such as dancing, walking, or doing housework not only provide distraction but also improve the environment, providing both immediate and lasting therapeutic effects [99].
- Physical exercise: Recognized for its behavioral and mental health benefits, exercise also acts as a neuropsychological intervention [100,101]. It stimulates brain regions that are involved in memory and learning, and the release of endorphins after exercise improves one’s mood, linking physical and cognitive wellbeing [102,103,104].
- Mindfulness: This practice is increasingly recognized in neuropsychology for its effects on brain regions that are associated with attention and awareness [104]. By anchoring awareness in the present, mindfulness provides relief from repetitive negative thoughts and can improve coping with mental health problems [105]. These strategies demonstrate how targeted activities can engage the brain’s neuroplasticity and cognitive resources to counter stress and improve mental health.
Emotional Coping Strategies
3.3. Coping in Clinical Conditions
3.3.1. Coping with Chronic Pain
3.3.2. Coping in Neurodegenerative Diseases
4. Discussion
4.1. Implications for Practice
4.2. Limitations
- Heterogeneity of Studies: The studies included in this review vary in design, measures used, populations studied, and cultural contexts. While this diversity allows for a broad examination of coping strategies across different scenarios, it also poses challenges in directly comparing the effectiveness of coping mechanisms or generating meta-analytic conclusions.
- Publication Bias: As with any review, our conclusions are subject to the limitations of the existing literature. There is an inherent potential for publication bias, where studies with positive results are more likely to be published than those with negative or null results. Despite our efforts to include a wide range of studies, this bias could influence the overall findings.
- Cultural and Socioeconomic Representation: The majority of the studies that we re-viewed were conducted in Western, educated, industrialized, rich, and democratic (WEIRD) societies. Consequently, the coping strategies identified may not be universally applicable, especially in non-WEIRD populations that may employ different methods of coping.
- Temporal and Historical Context: The temporal span of the included studies ranges across several decades. Changes over time in societal norms, economic conditions, and healthcare systems may influence both the stressors that individuals face and the coping strategies that they employ. This review may not fully capture these dynamic shifts.
- Theoretical Frameworks: The theoretical frameworks guiding the studies in this review are varied, with some focusing on cognitive behavioral models of coping, while others may employ psychodynamic or humanistic perspectives. Our synthesis of findings must, therefore, be viewed within the context of these diverse theoretical underpinnings.
- Scope of Research: This review is limited by the scope of the available research, which may overlook important unpublished work or research in adjacent fields. Although we attempted to conduct a comprehensive search, there is always the possibility that relevant studies have been inadvertently omitted.
- Practical Application: While this review provides a synthesis of the research on coping strategies in clinical psychology and neuropsychology, the translation of these findings into practical clinical interventions was not the primary focus. Therefore, the review may not fully address how these strategies can be implemented in practice.
- Comorbidity and Individual Differences: The complexity of individual psychological experiences, including comorbid conditions and individual differences, is a critical factor in how coping strategies are selected and employed. The reviewed research often does not account for the nuanced ways in which these factors interact with coping mechanisms.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
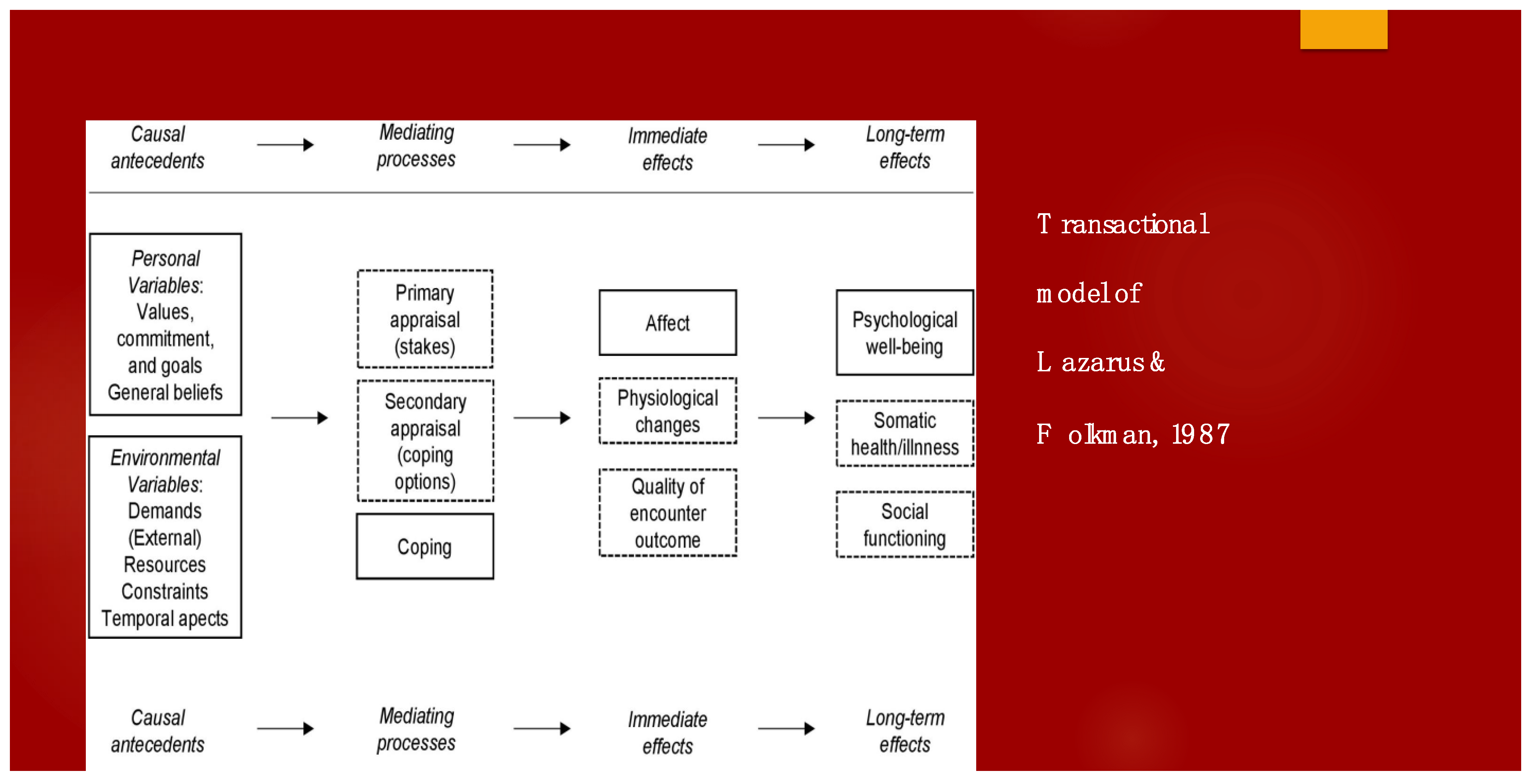
- Lazarus, R.S.; Folkman, S. The concept of coping. In Stress, Appraisal, and Coping; Lazarus, R.S., Folkman, S., Eds.; Springer Publishing Company: Berlin/Heidelberg, Germany, 1984; ISBN 0826141927. [Google Scholar]
- Pearlin, L.I.; Schooler, C. The structure of coping. J. Health Soc. Behav. 1978, 19, 2–21. [Google Scholar] [CrossRef]
- Kobasa, S.C. Stressful life events, personality, and health: An inquiry into hardiness. J. Personal. Soc. Psychol. 1979, 37, 1. [Google Scholar] [CrossRef]
- Billings, A.G.; Moos, R.H. Stressful life events and symptoms: A longitudinal model. Health Psychol. 1982, 1, 99–117. [Google Scholar] [CrossRef]
- Steptoe, A.; Feldman, P. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann. Behav. Med. 2001, 23, 177–185. [Google Scholar] [CrossRef]
- Schumm, J.; Briggs-Phillips, M.; Hobfoll, S. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. J. Trauma. Stress 2006, 19, 825–836. [Google Scholar] [CrossRef]
- Saklofske, D.H.; Austin, E.J.; Mastoras, S.M.; Beaton, L.; Osborne, S.E. Relationships of personality, affect, emotion-al intelligence and coping with student stress and academic success: Different patterns of association for stress and success. Learn. Individ. Differ. 2012, 22, 251–257. [Google Scholar] [CrossRef]
- Shanan, J.; Denour, A.; Garty, I. Effects of prolonged stress on coping style in terminal renal failure patients. J. Hum. Stress 1976, 2, 19. [Google Scholar] [CrossRef]
- Weigold, I.; Robitschek, C. Agentic personality characteristics and coping: Their relation to trait anxiety in college students. Am. J. Orthopsychiatry 2011, 81, 255–264. [Google Scholar] [CrossRef]
- Stevens, F.L. Emotional Regulation/Coping with Emotion. In Affective Neuroscience in Psychotherapy; Routledge: New York, NY, USA, 2021; pp. 112–117. [Google Scholar]
- Woodhead, E.L.; Cronkite, R.C.; Moos, R.H.; Timko, C. Coping Strategies Predictive of Adverse Outcomes among Community Adults. J. Clin. Psychol. 2013, 70, 1183–1195. [Google Scholar] [CrossRef]
- Hughes, J.W. Coping. In Encyclopedia of Clinical Neuropsychology; Springer International Publishing: Cham, Switzerland, 2018; p. 964. [Google Scholar]
- Snyder, C.R. Coping; Oxford University Press: New York, NY, USA, 2015. [Google Scholar]
- Theodoratou, M.M.; Arampatzi, K.; Tafiadis, D.; Mpoura, M. Coping Strategies of Greek Social Workers. Ann. Gen. Psychiatry 2006, 5, S241. [Google Scholar] [CrossRef]
- Theodoratou, M.M.; Plati, M.; Tsouxli, A.; Theodoridou, O.; Fotiadou, S.; Mpekos, V. Strategies Coping with Labour Stress from Speech Therapists in Greece. Ann. Gen. Psychiatry 2006, 5, S192. [Google Scholar] [CrossRef]
- Theodoratou, M.M.; Tafiadis, D.; Mpekos, V.; Skiloyanni, G. Coping Strategies by the Nurse Personnel Facing the Occupational Stress. Ann. Gen. Psychiatry 2006, 5, S242. [Google Scholar] [CrossRef]
- Łukasiewicz, J.; Kaczmarek, B.L.J. Health Care Workers Strategies For Coping with Stress. Acta Neuropsychol. 2023, 21, 387–394. [Google Scholar] [CrossRef]
- Riepenhausen, A.; Wackerhagen, C.; Reppmann, Z.C.; Deter, H.-C.; Kalisch, R.; Veer, I.M.; Walter, H. Positive Cognitive Reappraisal in Stress Resilience, Mental Health, and Well-Being: A Comprehensive Systematic Review. Emot. Rev. 2022, 14, 310–331. [Google Scholar] [CrossRef]
- Peter Terna, I., Sr. Vulnerability: Types, Causes, and Coping Mechanisms. Int. J. Sci. Manag. Stud. 2021, 4, 187–194. [Google Scholar] [CrossRef]
- Theodoratou, M.; Potoglou, A.; Tamiolaki, A.; Kalaitzaki, A. The Psychological Impact of Covid on Health Care Professionals during the Third Wave. Eur. Psychiatry 2023, 66, S412–S413. [Google Scholar] [CrossRef]
- Schmidt, S.; Power, M. Clinical Psychology. In Encyclopedia of Social Measurement; Elsevier: Amsterdam, The Netherlands, 2005; pp. 309–315. [Google Scholar] [CrossRef]
- Norcross, J.C.; VandenBos, G.R.; Freedheim, D.K. Apa Handbook of Clinical Psychology; American Psychological Association: Washington, DC, USA, 2016. [Google Scholar]
- Crespi, B.J. Evolutionary and genetic insights for clinical psychology. Clin. Psychol. Rev. 2020, 78, 101857. [Google Scholar] [CrossRef]
- Berlucchi, G. Neuropsychology. In Reference Module in Neuroscience and Biobehavioral Psychology; Elsevier: Amsterdam, The Netherlands, 2017. [Google Scholar] [CrossRef]
- Rogers, S.A.; Lowe, D.A. Neuropsychology. In Encyclopedia of Sciences and Religions; Springer: Dordrecht, The Netherlands, 2013; pp. 1500–1509. [Google Scholar] [CrossRef]
- Frydenberg, E. Coping Research: Historical Background, Links with Emotion, and New Research Directions on Adaptive Pro-cesses. Aust. J. Psychol. 2014, 66, 82–92. [Google Scholar] [CrossRef]
- Satterfield, J.M. Coping with stress: Problem-Focused and emotion-focused strategies. In Minding the Body: Workbook; Oxford University Press: New York, NY, USA, 2008; pp. 31–54. [Google Scholar] [CrossRef]
- Baker, J.P.; Berenbaum, H. Emotional Approach and Problem-Focused Coping: A Comparison of Potentially Adaptive Strategies. Cogn. Emot. 2007, 21, 95–118. [Google Scholar] [CrossRef]
- Fuster, J.M. Prefrontal cortex in decision-making. In Decision Neuroscience; Elsevier: Amsterdam, The Netherlands, 2017; pp. 95–105. [Google Scholar] [CrossRef]
- Martindale, S.L.; Morissette, S.B.; Kimbrel, N.A.; Meyer, E.C.; Kruse, M.I.; Gulliver, S.B.; Dolan, S.L. Neuropsychological functioning, coping, and quality of life among returning war veterans. Rehabil. Psychol. 2016, 61, 231–239. [Google Scholar] [CrossRef]
- Brands, I.; Köhler, S.; Stapert, S.; Wade, D.; Heugten, C. How flexible is coping after acquired brain injury? A 1-year prospective study investigating coping patterns and influence of self-efficacy, executive functioning and self-awareness. J. Rehabil. Med. 2014, 46, 869–875. [Google Scholar] [CrossRef]
- Krpan, K.M.; Levine, B.; Stuss, D.T.; Dawson, D.R. Executive function and coping at one-year post traumatic brain injury. J. Clin. Exp. Neuropsychol. 2007, 29, 36–46. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. Coping and Emotion. In Stress and Coping: An Anthology; Columbia University Press: New York, NY, USA, 1991; pp. 207–227. [Google Scholar]
- Cramer, P. Coping and Defense Mechanisms: What’s the Difference? J. Personal. 1998, 66, 919–946. [Google Scholar] [CrossRef]
- Maricutoiu, L.P.; Crasovan, D.I. Coping and Defence Mechanisms: What Are We Assessing? Int. J. Psychol. 2014, 51, 83–92. [Google Scholar] [CrossRef]
- Giuseppe, M.D.; Perry, J.C.; Prout, T.A.; Conversano, C. Recent Empirical Research and Methodologies in Defense Mechanisms; Frontiers Media SA: Lausanne, Switzerland, 2022. [Google Scholar]
- Vaillant, G.E. Defense Mechanisms: Their Assessment in the Laboratory and in the Clinic. Contemp. Psychol. A J. Rev. 1992, 37, 13–14. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Golden, G.Y. The Function of Denial in Stress, Coping, and Aging. In Aging; Elsevier: Amsterdam, The Netherlands, 1981; pp. 283–307. [Google Scholar]
- Folkman, S.; Lazarus, R.S. Ways of Coping Questionnaire (WAYS) [Database Record]; American Psychological Association: Washington, DC, USA, 1998. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. COPE Inventory; American Psychological Association: Washington, DC, USA, 1989. [Google Scholar] [CrossRef]
- Karademas, E. The adaptation of the Ways of Coping Questionnaire in the Greek language. Psychol. J. Hell. Psychol. Soc. 1998, 5, 261–273. [Google Scholar]
- Littman, J.A. The cope inventory: Dimensionality and relationships with approach- and avoidance-motives and positive and negative traits. Personal. Individ. Differ. 2006, 41, 273–284. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Esparbès, S.; Sordes-Ader, F.; Tap, P. Presentation del échelle de coping: Les stratégies de coping. Journées Du Labo 1994, 89–107. [Google Scholar]
- Stephenson, E.; DeLongis, A. Coping Strategies. Wiley Encycl. Health Psychol. 2020, 55–60. [Google Scholar] [CrossRef]
- Cheng, C.; Lau, H.-P.B.; Chan, M.-P.S. Coping Flexibility and Psychological Adjustment to Stressful Life Changes: A Meta-Analytic Review. Psychol. Bull. 2014, 140, 1582–1607. [Google Scholar] [CrossRef]
- Walker, T.; Lim, B.K. Defense/Coping Mechanism. In Encyclopedia of Cross-Cultural School Psychology; Clauss-Ehlers, C.S., Ed.; Springer: Boston, MA, USA, 2010. [Google Scholar] [CrossRef]
- Compas, B.E. An Agenda for Coping Research and Theory: Basic and Applied Developmental Issues. Int. J. Behav. Dev. 1998, 22, 231–237. [Google Scholar] [CrossRef]
- Steckler, T. The Neuropsychology of Stress. In Handbook of Stress and the Brain—Part 1: The Neurobiology of Stress; Steckler, Τ., Kalin, N.H., Reul, J.M.H.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2005; pp. 25–42. [Google Scholar]
- Sagici, O.; Ozdogar, A.T.; Aslan, T.; Ozakbas, S. Investigation of the Relationship Between Coping With the Disease and Affecting Cognitive, Physical, and Psychosocial Factors in People with Multiple Sclerosis. Arch. Clin. Neuropsychol. 2024, acad102. [Google Scholar] [CrossRef]
- Sutterer, M.J.; Tranel, D. Neuropsychology and cognitive neuroscience in the fMRI era: A recapitulation of localizationist and connectionist views. Neuropsychology 2017, 31, 972–980. [Google Scholar] [CrossRef]
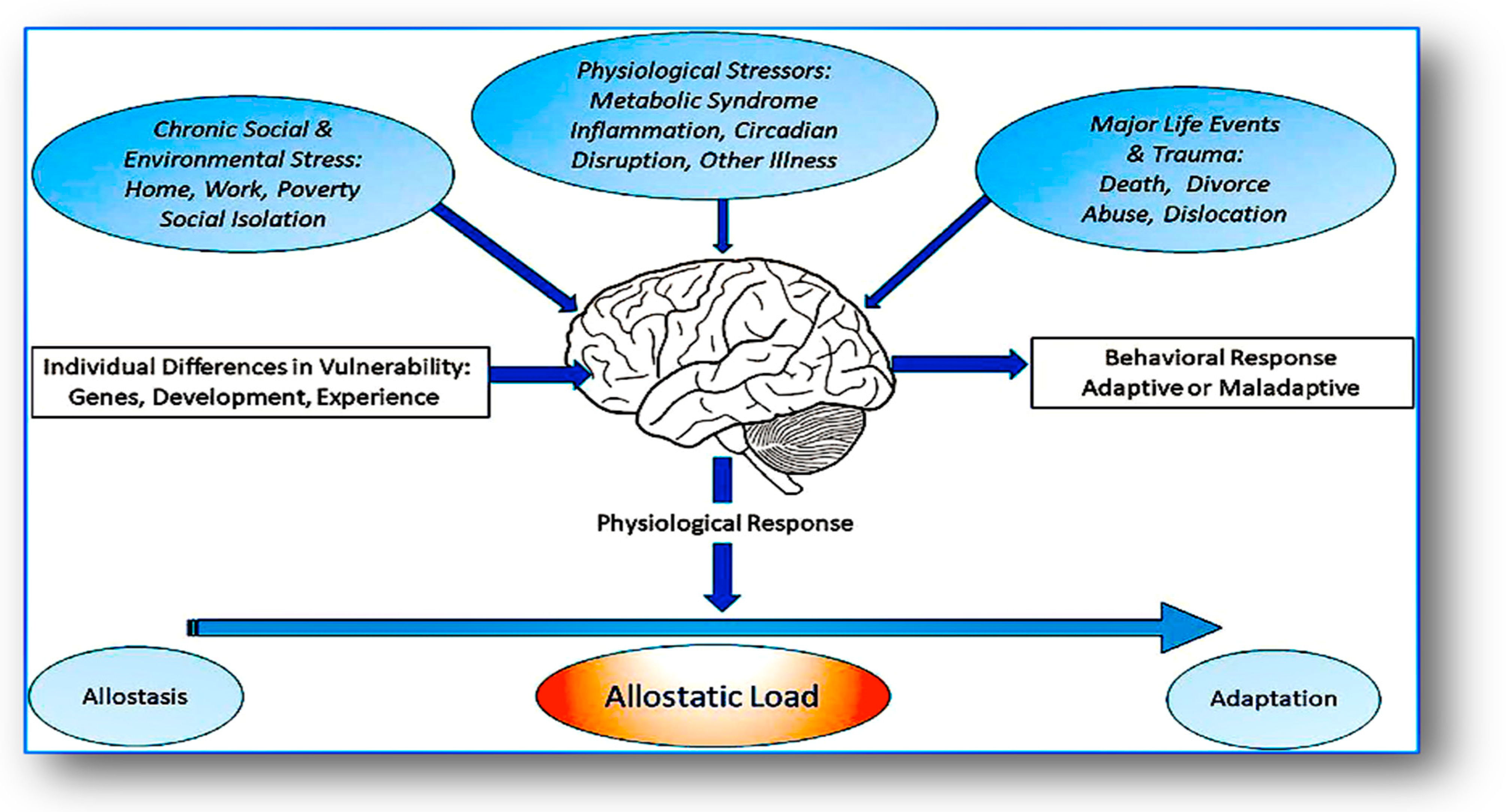
- Cohen, J.I. Stress and Mental Health: A Biobehavioral Perspective. Issues Ment. Health Nurs. 2000, 21, 185–202. [Google Scholar] [CrossRef]
- Hankin, B.L.; Snyder, H.R.; Gulley, L.D.; Schweizer, T.H.; Bijttebier, P.; Nelis, S.; Toh, G.; Vasey, M.W. Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Dev. Psychopathol. 2016, 28 Pt 1, 987–1012. [Google Scholar] [CrossRef]
- Wolff, M.; Enge, S.; Kräplin, A.; Krönke, K.; Bühringer, G.; Smolka, M.N.; Goschke, T. Chronic Stress, Executive Functioning, and Real-life Self-control: An Experience Sampling Study. J. Personal. 2020, 89, 402–421. [Google Scholar] [CrossRef]
- Lee, J.; Kim, E.; Wachholtz, A. The Effect of Perceived Stress on Life Satisfaction. Korean J. Youth Stud. 2016, 23, 29. [Google Scholar] [CrossRef]
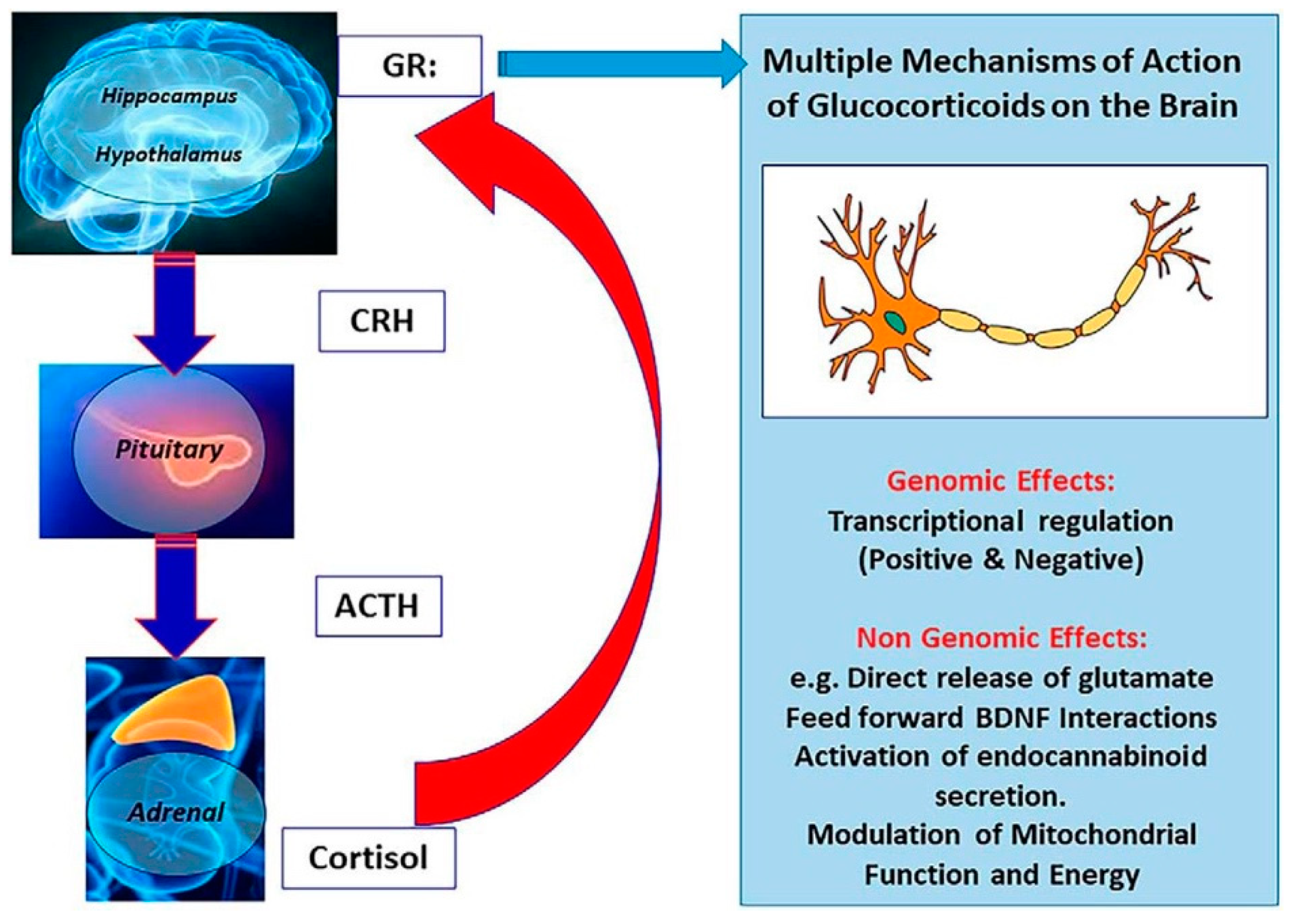
- McEwen, B.S.; Bowles, N.P.; Gray, J.D.; Hill, M.N.; Hunter, R.G.; Karatsoreos, I.N.; Nasca, C. Mechanisms of stress in the brain. Nat. Neurosci. 2015, 18, 1353–1363. [Google Scholar] [CrossRef]
- McEwen, B.S.; Gianaros, P.J. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann. N. Y. Acad. Sci. 2010, 1186, 190–222. [Google Scholar] [CrossRef]
- Girotti, M.; Adler, S.M.; Bulin, S.E.; Fucich, E.A.; Paredes, D.; Morilak, D.A. Prefrontal Cortex Executive Processes Affected by Stress in Health and Disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 85, 161–179. [Google Scholar] [CrossRef]
- Linthorst, A.C.E.; Reul, J.M. Stress and the Brain: Solving the Puzzle Using Microdialysis. Pharmacol. Biochem. Behav. 2008, 90, 163–173. [Google Scholar] [CrossRef]
- de Kloet, E.R.; Joëls, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef]
- MacDonald, K.; MacDonald, T.M. The peptide that binds: A systematic review of oxytocin and its prosocial effects in humans. Harv. Rev. Psychiatry 2010, 18, 1–21. [Google Scholar] [CrossRef]
- Ferris, C.F. Vasopressin/oxytocin and aggression. In Proceedings of the Novartis Foundation Symposium, Singapore, 26–27 September 2005; pp. 190–200. [Google Scholar] [CrossRef]
- Jurek, B.; Neumann, I.D. The Oxytocin Receptor: From Intracellular Signaling to Behavior. Physiol. Rev. 2018, 98, 1805–1908. [Google Scholar] [CrossRef]
- Heinrichs, M.; Baumgartner, T.; Kirschbaum, C.; Ehlert, U. Social support and oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biol. Psychiatry 2003, 54, 1389–1398. [Google Scholar] [CrossRef]
- Staudinger, M.R.; Erk, S.; Walter, H. Dorsolateral Prefrontal Cortex Modulates Striatal Reward Encoding during Reappraisal of Reward Anticipation. Cereb. Cortex 2011, 21, 2578–2588. [Google Scholar] [CrossRef]
- Pedersen, C.A. Oxytocin, Tolerance, and the Dark Side of Addiction. Int. Rev. Neurobiol. 2017, 136, 239–274. [Google Scholar]
- Theodoratou, M.; Kougioumtzis, G.A.; Yotsidi, V.; Sofologi, M.; Katsarou, D.; Megari, K. Neuropsychological Consequences of Massive Trauma: Implications and Clinical Interventions. Medicina 2023, 59, 2128. [Google Scholar] [CrossRef]
- Bradley, B.; Westen, D. The psychobiology of attachment and trauma: Some preliminary findings and implications for psychological research. J. Trauma Stress 2005, 18, 553–560. [Google Scholar]
- Meuret, A.E.; Twohig, M.P.; Rosenfield, D.; Hayes, S.C.; Craske, M.G. Brief cognitive-behavioral therapy for anxiety: A systematic review and meta-analysis. Clin. Psychol. Rev. 2012, 32, 425–443. [Google Scholar]
- Takayanagi, Y.; Onaka, T. Roles of Oxytocin in Stress Responses, Allostasis and Resilience. Int. J. Mol. Sci. 2021, 23, 150. [Google Scholar] [CrossRef]
- Holroyd, K.A.; Lazarus, R.S. Stress, coping, and somatic adaptation. In Handbook of Stress: Theoretical and Clinical Aspects; Goldberger, L., Breznitz, S., Eds.; The Free Press: New York, NY, USA, 1982. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Guilford: New York, NY, USA, 1984. [Google Scholar]
- Bremner, J.D. Traumatic stress: Effects on the brain. Dialogues Clin. Neurosci. 2006, 8, 445–461. [Google Scholar] [CrossRef]
- Cid-Jofré, V.; Moreno, M.; Reyes-Parada, M.; Renard, G.M. Role of Oxytocin and Vasopressin in Neuropsychiatric Disorders: Therapeutic Potential of Agonists and Antagonists. Int. J. Mol. Sci. 2021, 22, 12077. [Google Scholar] [CrossRef]
- Yeo, X.Y.; Cunliffe, G.; Ho, R.C.; Lee, S.S.; Jung, S. Potentials of Neuropeptides as Therapeutic Agents for Neurological Diseases. Biomedicines 2022, 10, 343. [Google Scholar] [CrossRef] [PubMed]
- Aguilera, G.; Rabadan-Diehl, C. Vasopressinergic regulation of the hypothalamic-pituitary-adrenal axis: Implications for stress adaptation. Regul. Pept. 2000, 96, 23–29. [Google Scholar] [CrossRef]
- Levy, I.; Schiller, D. Neural Computations of Threat. Trends Cogn. Sci. 2021, 25, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Bielsky, I.F.; Young, L.J. Oxytocin, vasopressin, and social recognition in mammals. Peptides 2004, 25, 1565–1574. [Google Scholar] [CrossRef] [PubMed]
- Argiolas, A.; Gessa, G.L. Central functions of oxytocin and vasopressin in mammals including humans. Med. Res. Rev. 1991, 11, 119–158. [Google Scholar]
- Aguilera, G.; Subburaju, S.; Young, S.; Chen, J. The parvocellular vasopressinergic system and responsiveness of the hypothalamic pituitary adrenal axis during chronic stress. Prog. Brain Res. 2008, 170, 29–39. [Google Scholar] [CrossRef]
- Neumann, I.D.; Landgraf, R. Balance of brain oxytocin and vasopressin: Implications for anxiety, depression, and social behaviors. Trends Neurosci. 2012, 35, 649–659. [Google Scholar] [CrossRef]
- Szczepanska-Sadowska, E.; Zera, T.; Sosnowski, P.; Cudnoch-Jedrzejewska, A.; Puszko, A.; Misicka, A. Vasopressin and related peptides; potential value in diagnosis, prognosis and treatment of clinical disorders. Curr. Drug Metab. 2017, 18, 306–345. [Google Scholar] [CrossRef] [PubMed]
- Ring, R.H. The central vasopressinergic system: Examining the opportunities for psychiatric drug development. Curr. Pharm. Des. 2005, 11, 205–225. [Google Scholar] [CrossRef] [PubMed]
- Hudson, K. Coping complexity model: Coping stressors, coping influencing factors, and coping responses. Psychology 2016, 7, 300–309. [Google Scholar] [CrossRef]
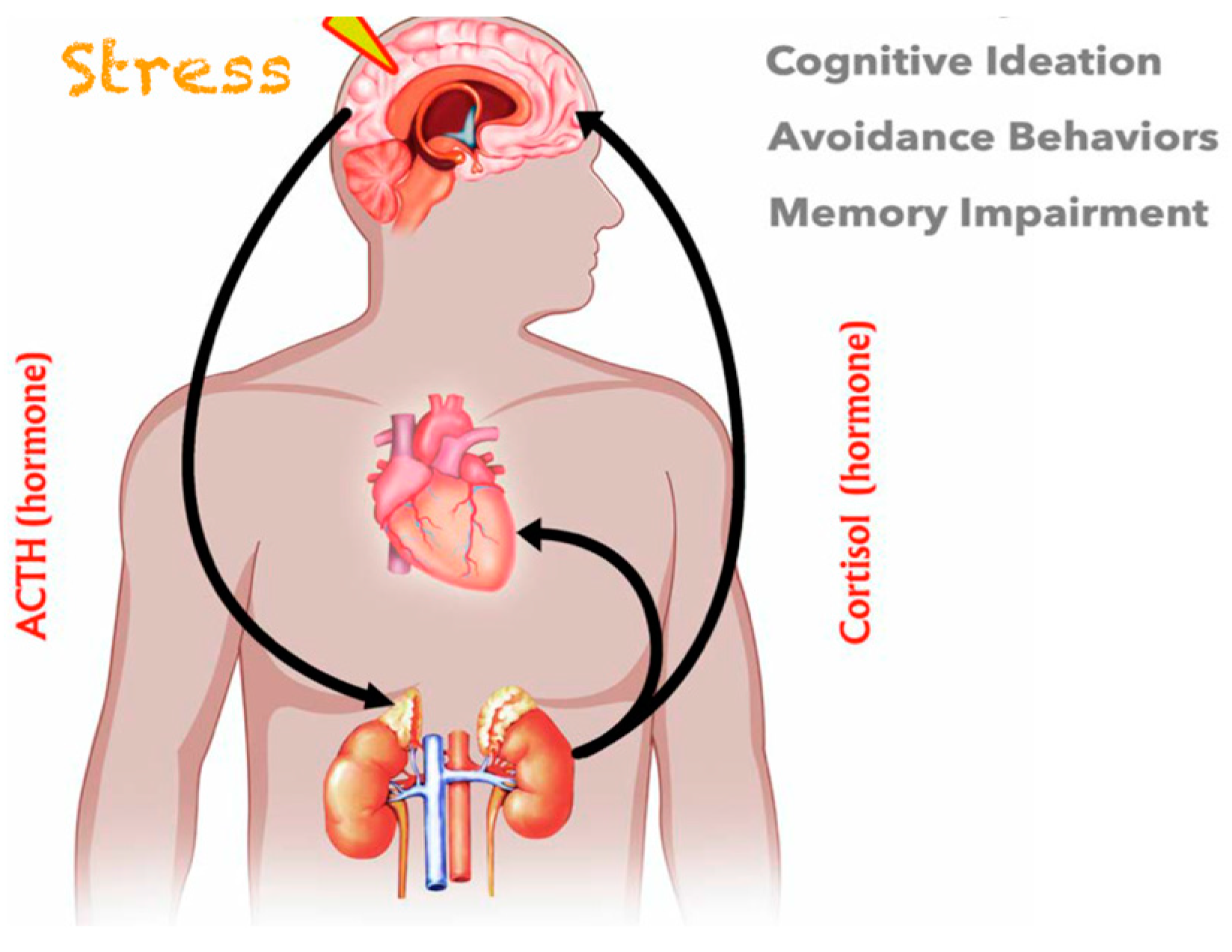
- James, K.A.; Stromin, J.I.; Steenkamp, N.; Combrinck, M.I. Understanding the relationships between physiological and psychosocial stress, cortisol and cognition. Front. Endocrinol. 2023, 14, 1085950. [Google Scholar] [CrossRef] [PubMed]
- Stephens, M.A.; Wand, G. Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol. Res. 2012, 34, 468–483. [Google Scholar]
- Godoy, L.D.; Rossignoli, M.T.; Delfino-Pereira, P.; Garcia-Cairasco, N.; de Lima Umeoka, E.H. A comprehensive overview on stress neurobiology: Basic concepts and clinical implications. Front. Behav. Neurosci. 2018, 12, 127. [Google Scholar] [CrossRef]
- Smith, S.M.; Vale, W.W. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin. Neurosci. 2006, 8, 383–395. [Google Scholar] [CrossRef]
- Compas, B.E. Psychobiological processes of stress and coping: Implications for resilience in children and adolescents–comments on the papers of Romeo & McEwen and Fisher et al. Ann. N. Y. Acad. Sci. 2006, 1094, 226–234. [Google Scholar]
- de Souza-Talarico, J.N.; Marin, M.-F.; Sindi, S.; Lupien, S.J. Effects of Stress Hormones on the Brain and Cognition: Evidence from Normal to Pathological Aging. Dement. Neuropsychol. 2011, 5, 8–16. [Google Scholar] [CrossRef]
- Wang, Y.-X.; Yin, B. A New Understanding of the Cognitive Reappraisal Technique: An Extension Based on the Schema Theory. Front. Behav. Neurosci. 2023, 17, 1174585. [Google Scholar] [CrossRef]
- Ferri, J.; Hajcak, G. Neural mechanisms associated with reappraisal and attentional deployment. Curr. Opin. Psychol. 2015, 3, 17–21. [Google Scholar] [CrossRef]
- Fenn, K.; Byrne, M. The key principles of cognitive behavioural therapy. InnovAiT 2013, 6, 579–585. [Google Scholar] [CrossRef]
- Gabrys, R.L.; Tabri, N.; Anisman, H.; Matheson, K. Cognitive Control and Flexibility in the Context of Stress and Depressive Symptoms: The Cognitive Control and Flexibility Questionnaire. Front. Psychol. 2018, 9, 2219. [Google Scholar] [CrossRef]
- Van Dillen, L.F.; Koole, S.L. Clearing the Mind: A Working Memory Model of Distraction from Negative Mood. Emotion 2007, 7, 715–723. [Google Scholar] [CrossRef]
- Berto, R. The Role of Nature in Coping with Psycho-Physiological Stress: A Literature Review on Restorativeness. Behav. Sci. 2014, 4, 394–409. [Google Scholar] [CrossRef]
- Olson, A.K.; Eadie, B.D.; Ernst, C.; Christie, B.R. Environmental Enrichment and Voluntary Exercise Massively Increase Neurogenesis in the Adult Hippocampus via Dissociable Pathways. Hippocampus 2006, 16, 250–260. [Google Scholar] [CrossRef]
- Pittman, C.M.; Karle, E.M. Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, & Worry; Echo Point Books & Media: Brattleboro, VT, USA, 2019. [Google Scholar]
- Tonarelli, A.; Cosentino, C.; Tomasoni, C.; Nelli, L.; Damiani, I.; Goisis, S.; Sarli, L.; Artioli, G. Expressive writing. A tool to help health workers of palliative care. Acta Biomed. Atenei Parm. 2018, 89 (Suppl. S6), 35–42. [Google Scholar] [CrossRef]
- Theodoratou, M.; Dritsas, I.; Saltou, M.; Dimas, V.; Spyropoulos, A.; Nikolopoulou, E.; Bekos, V.; Kloni, P.; Psychogioy, A.; Valsami, O. Physical Exercise and Students’ Mental Health. Eur. Psychiatry 2016, 33, s219. [Google Scholar] [CrossRef]
- Stein, E.; Crowley, S.; Dunnam, M.; Anderson-Hanley, C. B-64 Neuropsychological Benefits of Interactive Mental and Physical Exercise. Arch. Clin. Neuropsychol. 2014, 29, 561. [Google Scholar] [CrossRef]
- Silgailis, K. Physical Activity and Psychological Well-Being. Med. Sci. Sports Exerc. 2001, 33, 1246. [Google Scholar] [CrossRef]
- Manns, J.R.; Squire, L.R. Perceptual Learning, Awareness, and the Hippocampus. Hippocampus 2001, 11, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.M.; Litterini, A.J. Therapists’ Interventions among Practice Settings. In Physical Activity and Rehabilitation in Life-Threatening Illness; Routledge: London, UK, 2021; pp. 261–274. [Google Scholar] [CrossRef]
- Arenth, P.M. Mindfulness-Based Interventions in Neuropsychology. In Textbook of Clinical Neuropsychology, 2nd ed.; Taylor & Francis: New York, NY, USA; Routledge: London, UK, 2018; Volume 2017, pp. 1054–1067. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing Coping Strategies: A Theoretically Based Approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Kalaitzaki, A.E.; Tamiolaki, A.; Tsouvelas, G.; Theodoratou, M.; Konstantakopoulos, G. Gain from Pain: Exploring Vicarious Posttraumatic Growth and Its Facilitators among Health Care Workers across Two Consecutive Lockdowns during the COVID-19 Pandemic. Int. J. Stress Manag. 2024, 31, 20–31. [Google Scholar] [CrossRef]
- Öst, L.-G. Applied Relaxation: Description of a Coping Technique and Review of Controlled Studies. Behav. Res. Ther. 1987, 25, 397–409. [Google Scholar] [CrossRef]
- Goldwurm, G.F. Coping with Stress through Social Skills Training. In Perspectives on Research in Emotional Stress; Sudakov, K.V., Ganten, N.A., Nikolov, D., Eds.; Routledge: London, UK, 2022; pp. 251–264. [Google Scholar] [CrossRef]
- Han, M.; Jiang, G.; Luo, H.; Shao, Y. Neurobiological Bases of Social Networks. Front. Psychol. 2021, 12, 626337. [Google Scholar] [CrossRef]
- Wante, L.; Mezulis, A.; Van Beveren, M.-L.; Braet, C. The Mediating Effect of Adaptive and Maladaptive Emotion Regulation Strategies on Executive Functioning Impairment and Depressive Symptoms among Adolescents. Child Neuropsychol. 2016, 23, 935–953. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Hay, A.C. Rethinking Avoidance: Toward a Balanced Approach to Avoidance in Treating Anxiety Disorders. J. Anxiety Disord. 2018, 55, 14–21. [Google Scholar] [CrossRef]
- Franke, H.A. Toxic Stress: Effects, Prevention and Treatment. Children 2014, 1, 390–402. [Google Scholar] [CrossRef]
- Ong, W.-Y.; Stohler, C.S.; Herr, D.R. Role of the Prefrontal Cortex in Pain Processing. Mol. Neurobiol. 2018, 56, 1137–1166. [Google Scholar] [CrossRef]
- Pickering, G. Neuroplasticity in the Pain, Emotion, and Cognition Nexus. In Pain, Emotion and Cognition; Springer International Publishing: Cham, Switzerland, 2015; pp. 73–79. [Google Scholar]
- King, C.D.; Keil, A.; Sibille, K.T. Chronic Pain and Perceived Stress. In Stress: Concepts, Cognition, Emotion, and Behavior; Elsevier: Amsterdam, The Netherlands, 2016; pp. 413–421. [Google Scholar]
- Tait, R.C. Mind Matters: Psychological Interventions for Chronic Pain. Clin. J. Pain 2005, 21, 106–107. [Google Scholar] [CrossRef]
- Puri, B.K.; Theodoratou, M. The Efficacy of Psychoeducation in Managing Low Back Pain: A Systematic Review. Psychiatriki 2022, 34. [Google Scholar] [CrossRef]
- Hadjistavropoulos, T. Self-Management of Pain. In Promoting Self-Management of Chronic Health Conditions; Oxford University Press: New York, NY, USA, 2017; pp. 406–419. [Google Scholar]
- Scott, M. The CBT Treatment of Pain and Disability. In CBT for Common Trauma Responses; SAGE Publications Ltd.: London, UK, 2013; pp. 139–158. [Google Scholar]
- Harley, J. Bridging the Gap between Cognitive Therapy and Acceptance and Commitment Therapy (ACT). Procedia—Soc. Behav. Sci. 2015, 193, 131–140. [Google Scholar] [CrossRef]
- Brown, G.K.; Mandel, A.A.; Wright, J.H. Cognitive and Behavioral Models of Mental Function and Behavior. In Tasman’s Psychiatry; Tasman, A., Riba, M.B., Alarcón, R.D., Alfonso, C.A., Kanba, S., Ndetei, D.M., Ng, C.H., Schulze, T.G., Lecic-Tosevski, D., Eds.; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Hofmann, S.G. An Introduction to Modern CBT: Psychological Solutions to Mental Health Problems; John Wiley & Sons: Hoboken, NJ, USA, 2011; ISBN 1119951410. [Google Scholar]
- Clark, D.A. Cognitive Restructuring. Wiley Handb. Cogn. Behav. Ther. 2013, 1–22. [Google Scholar] [CrossRef]
- Ekers, D.; Webster, L.; Van Straten, A.; Cuijpers, P.; Richards, D.; Gilbody, S. Behavioural activation for depression: An update of meta-analysis of effectiveness and sub group analysis. PLoS ONE 2014, 9, e100100. [Google Scholar] [CrossRef]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing exposure therapy: An inhibitory learning approach. Behav. Res. Ther. 2014, 58, 10–23. [Google Scholar] [CrossRef]
- Lau, O.; Leung, L.; Wong, L. Cognitive behavioural techniques for changing the coping skills of patients with chronic pain. Hong Kong J. Occup. Ther. 2002, 12, 13–20. [Google Scholar] [CrossRef]
- Plumb Vilardaga, J.C.; Winger, J.G.; Teo, I.; Owen, L.; Sutton, L.M.; Keefe, F.J.; Somers, T.J. Coping Skills Training and Acceptance and Commitment Therapy for Symptom Management: Feasibility and Acceptability of a Brief Telephone-Delivered Protocol for Patients with Advanced Cancer. J. Pain Symptom Manag. 2020, 59, 270–278. [Google Scholar] [CrossRef]
- Vowles, K.E.; Fink, B.C.; Cohen, L.L. Acceptance and Commitment Therapy for Chronic Pain: A Diary Study of Treatment Process in Relation to Reliable Change in Disability. J. Context. Behav. Sci. 2014, 3, 74–80. [Google Scholar] [CrossRef]
- Michelson, D.; Hodgson, E.; Bernstein, A.; Chorpita, B.F.; Patel, V. Problem solving as an active ingredient in indicated prevention and treatment of Youth Depression and anxiety: An integrative review. J. Adolesc. Health 2022, 71, 390–405. [Google Scholar] [CrossRef]
- Theodoratou-Bekou, M.; Andreopoulou, O.; Andriopoulou, P.; Wood, B. Stress-Related Asthma and Family Therapy: Case Study. Ann. Gen. Psychiatry 2012, 11, 28. [Google Scholar] [CrossRef]
- Iribarren, S.; Siegel, K.; Hirshfield, S.; Olender, S.; Voss, J.; Krongold, J.; Luft, H.; Schnall, R. Self-Management Strategies for Coping with Adverse Symptoms in Persons Living with HIV with HIV Associated Non-AIDS Conditions. AIDS Behav. 2018, 22, 297–307. [Google Scholar] [CrossRef]
- Theodoratou, M.; Bekos, V.; Puri, B. Self-Management on Chronic Diseases: Literature Review Conference: 3D International Conference on Neurobiology, Psychopharmacology and Treatment Guidance. 2013, pp. 245–246. Available online: https://www.psychiatry.gr/3icnpepatg/abstract-book.pdf (accessed on 6 December 2023).
- Clare, L.; Teale, J.C.; Toms, G.; Kudlicka, A.; Evans, I.; Abrahams, S.; Goldstein, L.H.; Hindle, J.V.; Ho, A.K.; Jahanshahi, M.; et al. Cognitive rehabilitation, self-management, psychotherapeutic and caregiver support interventions in progressive neurodegenerative conditions: A scoping review. NeuroRehabilitation 2019, 43, 443–471. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Martel, M.O. Processes Underlying the Relation between Catastrophizing and Chronic Pain: Implications for Intervention. In From Acute to Chronic Back Pain; Oxford University Press: New York, NY, USA, 2012; pp. 251–267. [Google Scholar]
- Sullivan, M.J.L. The Communal Coping Model of Pain Catastrophising: Clinical and Research Implications. Can. Psychol./Psychol. Can. 2012, 53, 32–41. [Google Scholar] [CrossRef]
- Reilimo, M.; Kaila-Kangas, L.; Shiri, R.; Laurola, M.; Miranda, H. The Effect of Pain Management Group on Chronic Pain and Pain Related Co-Morbidities and Symptoms: A Stepped-Wedge Cluster Randomized Controlled Trial. A Study Protocol. Con-Tempor. Clin. Trials Commun. 2020, 19, 100603. [Google Scholar] [CrossRef]
- George, S.Z.; Wittmer, V.T.; Fillingim, R.B.; Robinson, M.E. Comparison of Graded Exercise and Graded Exposure Clinical Outcomes for Patients with Chronic Low Back Pain. J. Orthop. Sports Phys. Ther. 2010, 40, 694–704. [Google Scholar] [CrossRef]
- Vambheim, S.M.; Kyllo, T.M.; Hegland, S.; Bystad, M. Relaxation Techniques as an Intervention for Chronic Pain: A Systematic Review of Randomized Controlled Trials. Heliyon 2021, 7, e07837. [Google Scholar] [CrossRef]
- Golde, T.E. Alzheimer’s Disease—The Journey of a Healthy Brain into Organ Failure. Mol. Neurodegener. 2022, 17, 18. [Google Scholar] [CrossRef]
- Reul, J.M.H.M.; Collins, A.; Saliba, R.S.; Mifsud, K.R.; Carter, S.D.; Gutierrez-Mecinas, M.; Qian, X.; Linthorst, A.C.E. Glucocorticoids, epigenetic control and stress resilience. Neurobiol. Stress 2015, 1, 44–59. [Google Scholar] [CrossRef]
- de Kloet, E.R.; de Kloet, S.F.; de Kloet, C.S.; de Kloet, A.D. Top-down and Bottom-up Control of Stress-coping. J. Neuroendocrinol. 2018, 31, e12675. [Google Scholar] [CrossRef]
- Hill, A.R.; Spencer-Segal, J.L. Glucocorticoids and the Brain after Critical Illness. Endocrinology 2021, 162, bqaa242. [Google Scholar] [CrossRef]
- Aldao, A.; Jazaieri, H.; Goldin, P.R.; Gross, J.J. Adaptive and Maladaptive Emotion Regulation Strategies: Interactive Effects during CBT for Social Anxiety Disorder. J. Anxiety Disord. 2014, 28, 382–389. [Google Scholar] [CrossRef]
- Choi, E.; Gruman, J.A.; Leonard, C.M. A balanced view of mindfulness at work. Organ. Psychol. Rev. 2022, 12, 35–72. [Google Scholar] [CrossRef]
- Pierce, G.R.; Sarason, B.R.; Sarason, I.G.; Joseph, H.J.; Henderson, C.A. Conceptualizing and Assessing Social Support in the Context of the Family. In Handbook of Social Support and the Family; Springer: Boston, MA, USA, 1996; pp. 3–23. [Google Scholar]
- Agaibi, C.E.; Wilson, J.P. Trauma, PTSD, and Resilience. Trauma Violence Abus. 2005, 6, 195–216. [Google Scholar] [CrossRef]
- Sielski, R.; Rief, W.; Glombiewski, J.A. Efficacy of Biofeedback in Chronic Back Pain: A Meta-Analysis. Int. J. Behav. Med. 2016, 24, 25–41. [Google Scholar] [CrossRef]
- Kline, S.A.; Mega, M.S. Stress-Induced Neurodegeneration: The Potential for Coping as Neuroprotective Therapy. Am. J. Alzheimer’s Dis. Other Dement. 2020, 35, 153331752096087. [Google Scholar] [CrossRef]
- Cowell, A.-M.; Buckingham, J.C. Glucocorticoids and the HPA Axis. In Glucocorticoids; Birkhäuser: Basel, Switzerland, 2001; pp. 129–145. [Google Scholar]
- Kim, E.J.; Pellman, B.; Kim, J.J. Stress Effects on the Hippocampus: A Critical Review. Learn. Mem. 2015, 22, 411–416. [Google Scholar] [CrossRef]
- Sleiman, S.F.; Henry, J.; Al-Haddad, R.; El Hayek, L.; Abou Haidar, E.; Stringer, T.; Ulja, D.; Karuppagounder, S.S.; Holson, E.B.; Ratan, R.R.; et al. Exercise Promotes the Expression of Brain Derived Neurotrophic Factor (BDNF) through the Action of the Ketone Body β-Hydroxybutyrate. eLife 2016, 5, e15092. [Google Scholar] [CrossRef]
- Radley, J.; Morilak, D.; Viau, V.; Campeau, S. Chronic Stress and Brain Plasticity: Mechanisms Underlying Adaptive and Maladaptive Changes and Implications for Stress-Related CNS Disorders. Neurosci. Biobehav. Rev. 2015, 58, 79–91. [Google Scholar] [CrossRef]
- Laessle, R.; Schmidt, U. Stress Load, Stress Coping and Activity of HPA Axis in Adolescents with Major Depression. Austin Child Adolesc. Psychiatry 2021, 5, 1–4. [Google Scholar] [CrossRef]
- Cabib, S.; Campus, P.; Conversi, D.; Orsini, C.; Puglisi-Allegra, S. Functional and Dysfunctional Neuroplasticity in Learning to Cope with Stress. Brain Sci. 2020, 10, 127. [Google Scholar] [CrossRef] [PubMed]
- Monat, A.; Lazarus, R.S. (Eds.) Stress and Coping: An Anthology, 3rd ed.; Columbia University Press: New York, NY, USA, 1991. [Google Scholar]
- Theodoratou, M.; Kalpini-Papadopoulou, C.; Kiritsi, V.; Evagelatou, M.; Plitsi, A.; Andreopoulou, O. Novel Insights on Greek Students’ Coping Strategies. J. Psychol. Clin. Psychiatry 2017, 8, 473. [Google Scholar] [CrossRef]
- Flores-Kanter, P.E.; Moretti, L.; Medrano, L.A. A Narrative Review of Emotion Regulation Process in Stress and Recovery Phases. Heliyon 2021, 7, e07218. [Google Scholar] [CrossRef]
- Schultchen, D.; Reichenberger, J.; Mittl, T.; Weh, T.R.; Smyth, J.M.; Blechert, J.; Pollatos, O. Bidirectional relationship of stress and affect with physical activity and healthy eating. Br. J. Health Psychol. 2019, 24, 315–333. [Google Scholar] [CrossRef]
- Folkman, S. The Oxford Handbook of Stress, Health, and Coping; Oxford University Press: New York, NY, USA, 2011; ISBN 9780195375343. [Google Scholar]
- Carver, C.S. Stress, Coping, and Health. In Foundations of Health Psychology; Oxford University Press: New York, NY, USA, 2006; pp. 117–144. [Google Scholar]
- Lazarus, R.S.; Folkman, S. The Concept of Coping. Stress and Coping: An Anthology; Columbia University Press: New York, NY, USA, 1991; pp. 189–206. [Google Scholar]
- Guo, N.; Fuermaier, A.B.M.; Koerts, J.; Tucha, O.; Scherbaum, N.; Müller, B.W. Networks of Neuropsychological Functions in the Clinical Evaluation of Adult ADHD. Assessment 2022, 30, 1719–1736. [Google Scholar] [CrossRef]
- Kalaitzaki, A.; Tsouvelas, G.; Tamiolaki, A.; Theodoratou, M.; Konstantakopoulos, G. Secondary Traumatic Stress and Vicarious Posttraumatic Growth among nurses during three COVID-19 lockdowns in Greece. Eur. Psychiatry 2022, 65, S311–S312. [Google Scholar] [CrossRef]
- Parrott, W.G.; Schulkin, J. Neuropsychology and the Cognitive Nature of the Emotions. Cogn. Amp. Emot. 1993, 7, 43–59. [Google Scholar] [CrossRef]
- Grogans, S.E.; Bliss-Moreau, E.; Buss, K.A.; Clark, L.A.; Fox, A.S.; Keltner, D.; Cowen, A.S.; Kim, J.J.; Kragel, P.A.; MacLeod, C.; et al. The Nature and Neurobiology of Fear and Anxiety: State of the Science and Opportunities for Accelerating Discovery. Neurosci. Amp. Biobehav. Rev. 2023, 151, 105237. [Google Scholar] [CrossRef]
- Prezenski, S.; Brechmann, A.; Wolff, S.; Russwinkel, N. A Cognitive Modeling Approach to Strategy Formation in Dynamic Decision Making. Front. Psychol. 2017, 8, 1335. [Google Scholar] [CrossRef]
- Andolina, D.; Borreca, A. The Key Role of the Amygdala in Stress. In The Amygdala—Where Emotions Shape Perception, Learning and Memories; InTech: Nappanee, IN, USA, 2017. [Google Scholar]
- Lovallo, W.R. Central Nervous System Integration of the Psychological Stress Response. In Stress and Health: Biological and Psychological Interactions; Sage: Los Angeles, CA, USA, 2016. [Google Scholar]
- Quirin, M.; Kent, M.; Boksem, M.A.S.; Tops, M. Integration of negative experiences: A neuropsychological framework for human resilience. Behav. Brain Sci. 2015, 38. [Google Scholar] [CrossRef] [PubMed]
- Trambaiolli, L.R.; Biazoli, C.E., Jr.; Sato, J.R. Brain Imaging Methods in Social and Affective Neuroscience: A Machine Learning Perspective. In Social and Affective Neuroscience of Everyday Human Interaction; Springer International Publishing: Cham, Switzerland, 2022; pp. 213–230. [Google Scholar]
- Kim, T.-K.; Han, P.-L. Chronic stress and moderate physical exercise prompt widespread common activation and limited differential activation in specific brain regions. Neurochem. Int. 2016, 99, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Achnak, S.; Vantilborgh, T. Do individuals combine different coping strategies to manage their stress in the aftermath of psychological contract breach over time? A longitudinal study. J. Vocat. Behav. 2021, 131, 103651. [Google Scholar] [CrossRef]
- Lazarus, R.S. Emotion and Adaptation; Oxford University Press: New York, NY, USA, 1991; ISBN 9780190281786. [Google Scholar]
- Lim, T.; Thompson, J.; Tian, L.; Beck, B. A Transactional Model of Stress and Coping Applied to Cyclist Subjective Experiences. Transp. Res. Part F Traffic Psychol. Behav. 2023, 96, 155–170. [Google Scholar] [CrossRef]
- Morris, M.C.; Evans, L.D.; Rao, U.; Garber, J. Executive function moderates the relation between coping and depressive symptoms. Anxiety Stress Coping 2014, 28, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Shields, G.S.; Moons, W.G.; Slavich, G.M. Better executive function under stress mitigates the effects of recent life stress exposure on health in young adults. Stress 2017, 20, 92–102. [Google Scholar] [CrossRef]
- Malooly, A.M.; Genet, J.J.; Siemer, M. Individual differences in reappraisal effectiveness: The role of affective flexibility. Emotion 2013, 13, 302–313. [Google Scholar] [CrossRef]
- Fernandes, B.; Wright, M.; Essau, C.A. The Role of Emotion Regulation and Executive Functioning in the Intervention Outcome of Children with Emotional and Behavioural Problems. Children 2023, 10, 139. [Google Scholar] [CrossRef]
- Schmeichel, B.J.; Tang, D. Individual differences in executive functioning and their relationship to emotional processes and responses. Curr. Dir. Psychol. Sci. 2015, 24, 93–98. [Google Scholar] [CrossRef]
- van der Werff, S.J.A.; van den Berg, S.M.; Pannekoek, J.N.; Elzinga, B.M.; van der Wee, N.J.A. Neuroimaging resilience to stress: A review. Front. Behav. Neurosci. 2013, 7, 39. [Google Scholar] [CrossRef]
- Bell, A.C.; D’Zurilla, T.J. Problem-solving therapy for depression: A meta-analysis. Clin. Psychol. Rev. 2009, 29, 348–353. [Google Scholar] [CrossRef]
- Feder, A.; Fred-Torres, S.; Southwick, S.M.; Charney, D.S. The Biology of Human Resilience: Opportunities for Enhancing Resilience Across the Life Span. Biol. Psychiatry 2019, 86, 443–453. [Google Scholar] [CrossRef]
- Nechvatal, J.M.; Lyons, D.M. Coping changes the brain. Front. Behav. Neurosci. 2013, 7, 13. [Google Scholar] [CrossRef]
- Woo, J.; Whyne, E.Z.; Steinhardt, M.A. Psychological distress and self-reported mental disorders: The partially mediating role of coping strategies. Anxiety Stress Coping 2023, 37, 180–191. [Google Scholar] [CrossRef]
- Stümpel, J.; van Munster, M.; Grosjean, S.; Pedrosa, D.J.; Mestre, T.A. Coping Styles in Patients with Parkinson’s Disease: Consideration in the Co-Designing of Integrated Care Concepts. J. Pers. Med. 2022, 12, 921. [Google Scholar] [CrossRef]
- Simpkins, C.A.; Simpkins, A.M. Neuroscience for Clinicians Evidence, Models, and Practice; Springer: New York, NY, USA, 2013. [Google Scholar]
- Santarnecchi, E.; Sprugnoli, G.; Tatti, E.; Mencarelli, L.; Neri, F.; Momi, D.; Di Lorenzo, G.; Pascual-Leone, A.; Rossi, S.; Rossi, A. Brain functional connectivity correlates of coping styles. Cogn. Affect Behav. Neurosci. 2018, 18, 495–508. [Google Scholar] [CrossRef]
- Maki, P. Bridging the Gap Between Neuroscience and the Social World: Theory, Research, and Mechanisms in Social Neuroscience. J. Int. Neuropsychol. Soc. 2005, 11, 792–793. [Google Scholar] [CrossRef]
- Andolina, D.; Maran, D.; Valzania, A.; Conversi, D.; Puglisi-Allegra, S. Prefrontal/Amygdala System Determines Stress Coping Behavior Through 5-HT/GABA Connection. Neuropsychopharmacology 2013, 38, 2057–2067. [Google Scholar] [CrossRef] [PubMed]
- Keng, S.-L.; Smoski, M.J.; Robins, C.J. Effects of Mindfulness on Psychological Health: A Review of Empirical Studies. Clin. Psychol. Rev. 2011, 31, 1041–1056. [Google Scholar] [CrossRef] [PubMed]
- Tabibnia, G.; Radecki, D. Resilience Training That Can Change the Brain. Consult. Psychol. J. Pract. Res. 2018, 70, 59–88. [Google Scholar] [CrossRef]
- Mueller, C.; Wesenberg, S.; Nestmann, F.; Stubbs, B.; Bebbington, P.; Raymont, V. Interventions to Enhance Coping after Traumatic Brain Injury: A Systematic Review. Int. J. Ther. Rehabil. 2018, 25, 107–119. [Google Scholar] [CrossRef]
- Anshel, M.H. Coping with Stress. In Encyclopedia of the Sciences of Learning; Seel, N.M., Ed.; Springer: Boston, MA, USA, 2012. [Google Scholar] [CrossRef]
- Kalaitzaki, A.; Theodoratou, M.; Tsouvelas, G.; Tamiolaki, A.; Konstantakopoulos, G. Coping Profiles and Their Association with Vicarious Post-traumatic Growth among Nurses during the Three Waves of the COVID-19 Pandemic. J. Clin. Nurs. 2024, 33, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Theodoratou, M.; Vassilopoulou, C.; Giotsidi, V.; Tsitsas, G.; Flora, K.; Kougioumtzis, G. Psychological Distress and coping strategies of patients with Chronic Diseases. Eur. Psychiatry 2023, 66, S989–S990. [Google Scholar]
- Aldwin, C.M.; Brustrom, J. Theories of Coping with Chronic Stress. In Coping with Chronic Stress; Springer: Boston, MA, USA, 1997; pp. 75–103. [Google Scholar]
- Grassi-Oliveira, R.; Daruy-Filho, L.; Brietzke, E. New perspectives on coping in bipolar disorder. Psychol. Neurosci. 2010, 3, 161–165. [Google Scholar] [CrossRef]
- Taylor, S.E.; Stanton, A.L. Coping resources, coping processes, and mental health. Ann. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef] [PubMed]
- Theodoratou, M.; Andreopoulou, O.; Bekos, V.; Pierrakeas, C.; Skiadopoulos, S. Culture specific stress coping strategies used to alleviate occupational stress among Greek nursing personnel. J. Med. Psychol. 2009, 1, 21. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodoratou, M.; Argyrides, M. Neuropsychological Insights into Coping Strategies: Integrating Theory and Practice in Clinical and Therapeutic Contexts. Psychiatry Int. 2024, 5, 53-73. https://doi.org/10.3390/psychiatryint5010005
Theodoratou M, Argyrides M. Neuropsychological Insights into Coping Strategies: Integrating Theory and Practice in Clinical and Therapeutic Contexts. Psychiatry International. 2024; 5(1):53-73. https://doi.org/10.3390/psychiatryint5010005
Chicago/Turabian StyleTheodoratou, Maria, and Marios Argyrides. 2024. "Neuropsychological Insights into Coping Strategies: Integrating Theory and Practice in Clinical and Therapeutic Contexts" Psychiatry International 5, no. 1: 53-73. https://doi.org/10.3390/psychiatryint5010005
APA StyleTheodoratou, M., & Argyrides, M. (2024). Neuropsychological Insights into Coping Strategies: Integrating Theory and Practice in Clinical and Therapeutic Contexts. Psychiatry International, 5(1), 53-73. https://doi.org/10.3390/psychiatryint5010005






