Suicide Risk Assessment and Prevention Tools in the UK: Current Landscape and Future Directions
Abstract
1. Introduction
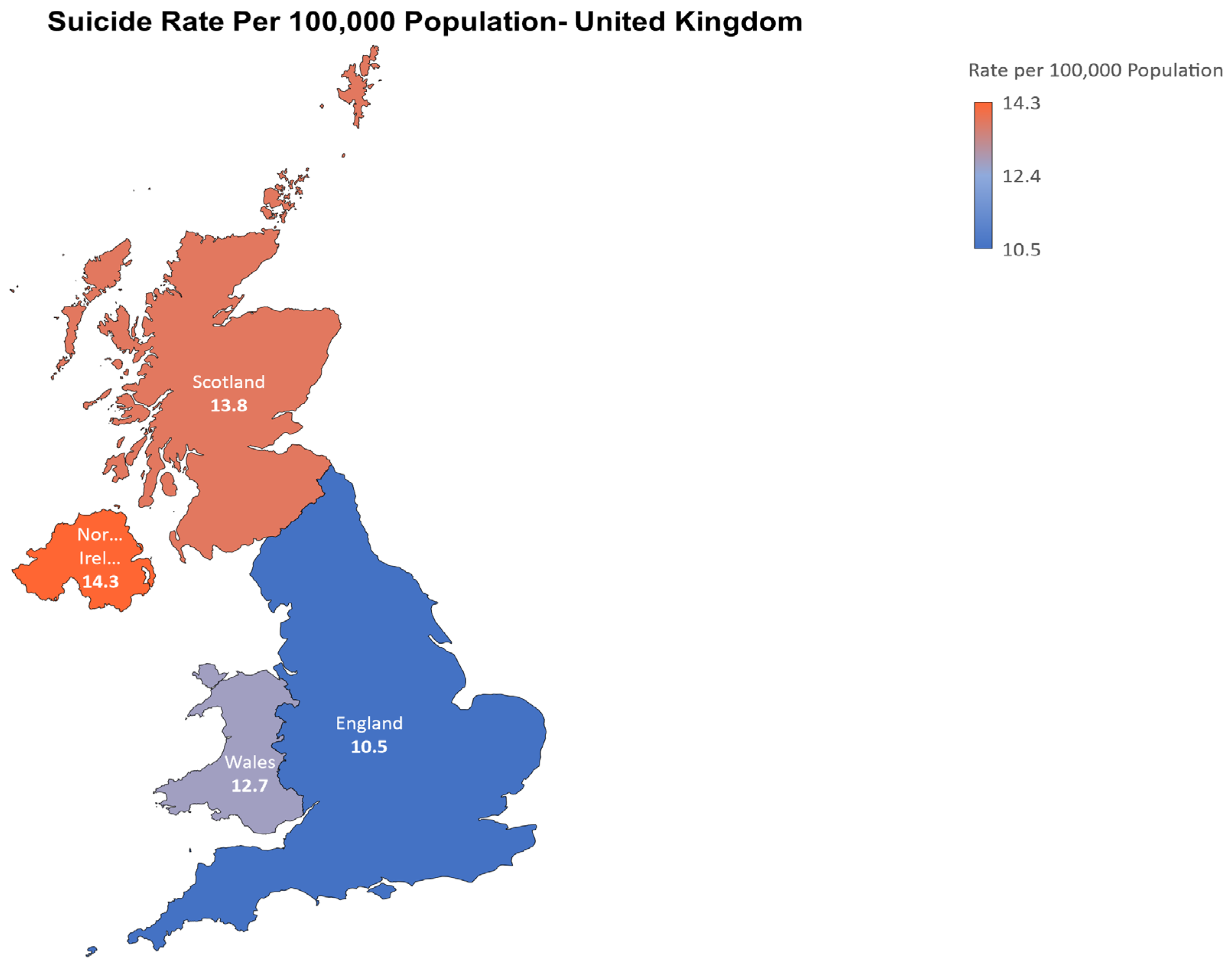
2. Epidemiology of Suicide in the UK
3. Risk Factors for Suicide
4. Screening and Assessment Tools
4.1. The Columbia-Suicide Severity Rating Scale (CSSRS)
4.2. Suicide Ideation Questionnaire (SIQ)
4.3. Beck Scale for Suicide Ideation (BSSI)
4.4. Manchester Self-Harm Rule (MSHR)
4.5. Ecological Momentary Assessment (EMA)
4.6. Other Assessment Tools
5. Machine Learning in Suicide Prevention
6. Mobile Applications for Suicide Prevention
7. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alves, V.M.; Francisco, L.C.; de Melo, A.R.; Novaes, C.R.; Belo, F.M.; Nardi, A.E. Trends in suicide attempts at an emergency department. Rev. Bras. Psiquiatr. 2017, 39, 55–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maguire, A.; Ross, E.; O’Reilly, D. Parental mental health and risk of poor mental health and death by suicide in offspring: A population-wide data-linkage study. Epidemiol. Psychiatr. Sci. 2022, 31, e25. [Google Scholar] [CrossRef] [PubMed]
- WHO; Saxena, S.; Krug, E.G.; Chestnov, O. Preventing Suicide: A Global Imperative; World Health Organization: Geneva, Switzerland, 2014; p. 92.
- Klonsky, E.D.; May, A.M.; Saffer, B.Y. Suicide, Suicide Attempts, and Suicidal Ideation. Annu. Rev. Clin. Psychol. 2016, 12, 307–330. [Google Scholar] [CrossRef] [PubMed]
- Harmer, B.; Lee, S.; Duong, T.V.H.; Saadabadi, A. Suicidal Ideation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK565877/ (accessed on 17 September 2023).
- Kannan, K.; Pillai, S.K.; Gill, J.S.; Hui, K.O.; Swami, V. Religious beliefs, coping skills and responsibility to family as factors protecting against deliberate self-harm. S. Afr. J. Psychiatry 2010, 16, 9. [Google Scholar] [CrossRef]
- Department of Health. Preventing Suicide in England—A Cross-Government Outcomes Strategy to Save Lives. 2012. Available online: www.dh.gov.uk/ (accessed on 19 July 2023).
- House of Commons Library. Suicide Prevention: Policy and Practice; House of Commons Library: London, UK, 2022. [Google Scholar]
- Office for National Statistics. Suicides in England and Wales 2021 Registrations; Office for National Statistics: Newport, Wales, 2022.
- Public Health Scotland. Suicide Statistics for Scotland Update of Trends for the Year 2021 A National Statistics Release for Scotland; Public Health Scotland: Glasgow, Scotland, 2022. [Google Scholar]
- Finalised Suicide Statistics in Northern Ireland 2015 to 2021. 2022. Available online: https://www.nisra.gov.uk/publications/suicide-statistics-2021 (accessed on 19 July 2023).
- NHS England. The Five Year forward View for Mental Health; NHS England: Leeds, UK, 2016.
- Stack, S. Contributing factors to suicide: Political, social, cultural and economic. Prev. Med. 2021, 152, 106498. [Google Scholar] [CrossRef]
- Turecki, G.; Brent, D.A.; Gunnell, D.; O’Connor, R.C.; Oquendo, M.A.; Pirkis, J.; Stanley, B.H. Suicide and suicide risk. Nat. Rev. Dis. Primers 2019, 5, 74. [Google Scholar] [CrossRef]
- Zakowicz, P.; Skibińska, M.; Wasicka-Przewoźna, K.; Skulimowski, B.; Waśniewski, F.; Chorzepa, A.; Różański, M.; Twarowska-Hauser, J.; Pawlak, J. Impulsivity as a Risk Factor for Suicide in Bipolar Disorder. Front. Psychiatry 2021, 12, 706933. [Google Scholar] [CrossRef]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef]
- Esang, M.; Ahmed, S. A Closer Look at Substance Use and Suicide. Am. J. Psychiatry Resid. J. 2018, 13, 6–8. [Google Scholar] [CrossRef]
- Arsenault-Lapierre, G.; Kim, C.; Turecki, G. Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry 2004, 4, 37. [Google Scholar] [CrossRef]
- Bertolote, J.M.; Fleischmann, A. Suicide and psychiatric diagnosis: A worldwide perspective. World Psychiatry 2002, 1, 181. [Google Scholar] [PubMed]
- Rezaei, Z.; Mohammadi, S.; Aghaei, A.; Pouragha, H.; Latifi, A.; Keshavarz-Mohammadi, N. Assessment of risk factors for suicidal behavior: Results from the Tehran University of Medical Sciences Employees’ Cohort Study. Front. Public Health 2023, 11, 1180250. [Google Scholar] [CrossRef] [PubMed]
- Pathirathna, M.L.; Nandasena, H.M.R.K.G.; Atapattu, A.M.M.P.; Weerasekara, I. Impact of the COVID-19 pandemic on suicidal attempts and death rates: A systematic review. BMC Psychiatry 2022, 22, 506. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.; Marano, G.; Del Castillo, A.G.; Chieffo, D.; Monti, L.; Janiri, D.; Moccia, L.; Sani, G. Intimate partner violence: A loop of abuse, depression and victimization. World J. Psychiatry 2021, 11, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef]
- Handley, T.; Rich, J.; Davies, K.; Lewin, T.; Kelly, B. The challenges of predicting suicidal thoughts and behaviours in a sample of rural Australians with depression. Int. J. Environ. Res. Public Health 2018, 15, 928. [Google Scholar] [CrossRef]
- Cleare, S.; Wetherall, K.; Clark, A.; Ryan, C.; Kirtley, O.J.; Smith, M.; O’Connor, R.C. Adverse childhood experiences and hospital-treated self-harm. Int. J. Environ. Res. Public Health 2018, 15, 1235. [Google Scholar] [CrossRef]
- Calati, R.; Ferrari, C.; Brittner, M.; Oasi, O.; Olié, E.; Carvalho, A.F.; Courtet, P. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J. Affect. Disord. 2019, 245, 653–667. [Google Scholar] [CrossRef]
- Joiner, T.E. Why People Die by Suicide; Harvard University Press: Cambridge, MA, USA, 2005. [Google Scholar]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.R.; Selby, E.A.; Joiner, T.E., Jr. The interpersonal theory of suicide. Psychol. Rev. 2010, 117, 575. [Google Scholar] [CrossRef]
- Durkheim, E. Suicide: A Study in Sociology [1897]; Spaulding, J.A., Simpson, G., Translators; The Free Press: Glencoe, IL, USA, 1951. [Google Scholar]
- Shaw, R.J.; Cullen, B.; Graham, N.; Lyall, D.M.; Mackay, D.; Okolie, C.; Pearsall, R.; Ward, J.; John, A.; Smith, D.J. Living alone, loneliness and lack of emotional support as predictors of suicide and self-harm: A nine-year follow up of the UK Biobank cohort. J. Affect. Disord. 2021, 279, 316–323. [Google Scholar] [CrossRef]
- Näher, A.-F.; Rummel-Kluge, C.; Hegerl, U. Associations of Suicide Rates With Socioeconomic Status and Social Isolation: Findings From Longitudinal Register and Census Data. Front. Psychiatry 2020, 10, 898. [Google Scholar] [CrossRef] [PubMed]
- Chikritzhs, T.; Livingston, M. Alcohol and the Risk of Injury. Nutrients 2021, 13, 2777. [Google Scholar] [CrossRef] [PubMed]
- Karapetian, K.; Jeon, S.M.; Kwon, J.-W.; Suh, Y.-K. Supervised Relation Extraction between Suicide-Related Entities and Drugs: Development and Usability Study of an Annotated PubMed Corpus. J. Med. Internet Res. 2023, 25, e41100. [Google Scholar] [CrossRef] [PubMed]
- Yuodelis-Flores, C.; Ries, R.K. Addiction and suicide: A review. Am. J. Addict. 2015, 24, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.J.; Norman, R.E.; Freedman, G.; Baxter, A.J.; Pirkis, J.E.; Harris, M.G.; Page, A.; Carnahan, E.; Degenhardt, L.; Vos, T. The burden attributable to mental and substance use disorders as risk factors for suicide: Findings from the Global Burden of Disease Study 2010. PLoS ONE 2014, 9, e91936. [Google Scholar] [CrossRef]
- Pavarin, R.M.; Fioritti, A. Mortality trends among cocaine users treated between 1989 and 2013 in northern Italy: Results of a longitudinal study. J. Psychoact. Drugs 2018, 50, 72–80. [Google Scholar] [CrossRef]
- Hasin, D.; Hatzenbuehler, M.L.; Keyes, K.; Ogburn, E. Substance use disorders: Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) and International Classification of Diseases, tenth edition (ICD-10). Addiction 2006, 101, 59–75. [Google Scholar] [CrossRef]
- Miyasato, K. The definition of drug dependence. Nihon Rinsho 2010, 68, 1431–1436. [Google Scholar]
- AL-Eitan, L.N.; Rababa’h, D.M.; Alghamdi, M.A. Genetic susceptibility of opioid receptor genes polymorphism to drug addiction: A candidate-gene association study. BMC Psychiatry 2021, 21, 5. [Google Scholar] [CrossRef]
- Bailey, J.; Kalk, N.J.; Andrews, R.; Yates, S.; Nahar, L.; Kelleher, M.; Paterson, S. Alcohol and cocaine use prior to suspected suicide: Insights from toxicology. Drug Alcohol Rev. 2021, 40, 1195–1201. [Google Scholar] [CrossRef]
- Haw, C.; Hawton, K.; Niedzwiedz, C.; Platt, S. Suicide Clusters: A Review of Risk Factors and Mechanisms. Suicide Life-Threat. Behav. 2013, 43, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Suicides in England and Wales 2020 Registrations; Office for National Statistics: Newport, Wales, 2021.
- Qin, P.; Syeda, S.; Canetto, S.S.; Arya, V.; Liu, B.; Menon, V.; Lew, B.; Platt, S.; Yip, P.; Gunnell, D. Midlife suicide: A systematic review and meta-analysis of socioeconomic, psychiatric and physical health risk factors. J. Psychiatr. Res. 2022, 154, 233–241. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, S.; Ennis, E.; Corry, C.; Bunting, B. Factors Associated with Suicide in Four Age Groups: A Population Based Study. Arch. Suicide Res. 2018, 22, 128–138. [Google Scholar] [CrossRef]
- Bond, K.S.; Cottrill, F.A.; Mackinnon, A.; Morgan, A.J.; Kelly, C.M.; Armstrong, G.; Kitchener, B.A.; Reavley, N.J.; Jorm, A.F. Effects of the Mental Health First Aid for the suicidal person course on beliefs about suicide, stigmatising attitudes, confidence to help, and intended and actual helping actions: An evaluation. Int. J. Ment. Health Syst. 2021, 15, 36. [Google Scholar] [CrossRef]
- Parameshwaraiah, S.T.; Manohar, S.; Thiagarajan, K. Suicide attempts and related risk factors in patients admitted to tertiary care centre in south india. J. Evol. Med. Dent. Sci. 2018, 7, 2916–2920. [Google Scholar] [CrossRef]
- Azizabadi, Z.; Aminisani, N.; Emamian, M.H. Socioeconomic inequality in depression and anxiety and its determinants in Iranian older adults. BMC Psychiatry 2022, 22, 761. [Google Scholar] [CrossRef] [PubMed]
- Spottswood, M.; Lim, C.T.; Davydow, D.; Huang, H. Improving Suicide Prevention in Primary Care for Differing Levels of Behavioral Health Integration: A Review. Front. Med. 2022, 9, 892205. [Google Scholar] [CrossRef]
- Raue, P.J.; Ghesquiere, A.R.; Bruce, M.L. Suicide Risk in Primary Care: Identification and Management in Older Adults. Curr. Psychiatry Rep. 2014, 16, 466. [Google Scholar] [CrossRef]
- Lavers, G.; Andriessen, K.; Krysinska, K. A Systematic Review of the Experiences and Support Needs of Informal Caregivers for People Who Have Attempted Suicide or Experienced Suicidal Ideation. Int. J. Environ. Res. Public Health 2022, 19, 5181. [Google Scholar] [CrossRef]
- Soja Santos, L.M.; Wesner, A.C.; Algeri, S.; Zarth, S.M. Knowledge of teachers about suicidal behavior in adolescents. Investig. Educ. Enferm. 2022, 40, e11. [Google Scholar] [CrossRef]
- Bohnert, A.S.B.; Roeder, K.; Ilgen, M.A. Unintentional overdose and suicide among substance users: A review of overlap and risk factors. Drug Alcohol Depend. 2010, 110, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Iovine-Wong, P.E.; Nichols-Hadeed, C.; Thompson Stone, J.; Gamble, S.; Cross, W.; Cerulli, C.; Levandowski, B.A. Intimate Partner Violence, Suicide, and Their Overlapping Risk in Women Veterans: A Review of the Literature. Mil. Med. 2019, 184, e201–e210. [Google Scholar] [CrossRef] [PubMed]
- Salvi, J. Columbia-Suicide Severity Rating Scale (C-SSRS). Emerg. Med. Pract. 2019, 21, CD3–CD4. [Google Scholar]
- Madan, A.; Frueh, B.C.; Allen, J.G.; Ellis, T.E.; Rufino, K.A.; Oldham, J.M.; Fowler, J.C. Psychometric Reevaluation of the Columbia-Suicide Severity Rating Scale: Findings from a Prospective, Inpatient Cohort of Severely Mentally Ill Adults. J. Clin. Psychiatry 2016, 77, 16125. [Google Scholar] [CrossRef]
- The Columbia Lighthouse Project. About the Protocol the Columbia Lighthouse Project. Available online: https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/about-the-scale/ (accessed on 17 September 2023).
- Posner, K.; Brent, D.; Lucas, C.; Gould, M.; Stanley, B.; Brown, G.; Fisher, P.; Zelazny, J.; Burke, A.; Oquendo, M. Columbia-Suicide Severity Rating Scale (C-SSRS); Columbia University Irving Medical Center: New York, NY, USA, 2008; Volume 10, p. 2008. [Google Scholar]
- Van Duijn, E.; Vrijmoeth, E.M.; Giltay, E.J.; Bernhard Landwehrmeyer, G. Suicidal ideation and suicidal behavior according to the C-SSRS in a European cohort of Huntington’s disease gene expansion carriers. J. Affect. Disord. 2018, 228, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.M.; Park, J.I.; Oh, K.Y.; Lee, K.H.; Kim, M.S.; Yoon, M.S.; Chung, Y.C. Predictors of suicidal ideation in a community sample: Roles of anger, self-esteem, and depression. Psychiatry Res. 2014, 216, 74–81. [Google Scholar] [CrossRef]
- Manning, J.C.; Carter, T.; Walker, G.; Coad, J.; Aubeeluck, A. Assessing risk of self-harm in acute paediatric settings: A multicentre exploratory evaluation of the CYP-MH SAPhE instrument. BMJ Open 2021, 11, e043762. [Google Scholar] [CrossRef]
- Lindh, Å.U.; Waern, M.; Beckman, K.; Renberg, E.S.; Dahlin, M.; Runeson, B. Short term risk of non-fatal and fatal suicidal behaviours: The predictive validity of the Columbia-Suicide Severity Rating Scale in a Swedish adult psychiatric population with a recent episode of self-harm. BMC Psychiatry 2018, 18, 319. [Google Scholar] [CrossRef]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Glenn Melvin, M.A.; Greenhill, L.; Shen, S.; et al. The Columbia-Suicide Severity Rating Scale: Initial Validity and Internal Consistency Findings from Three Multisite Studies with Adolescents and Adults. 2011. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893686/ (accessed on 19 July 2023).
- Giddens, J.M.; Sheehan, K.H.; Sheehan, D.V. The Columbia-Suicide Severity Rating Scale (C-SSRS): Has the “Gold Standard” Become a Liability? Innov. Clin. Neurosci. 2014, 11, 66–80. [Google Scholar]
- Pinto, A.; Whisman, M.A.; McCoy, K.J.M. Suicidal ideation in adolescents: Psychometric properties of the suicidal ideation questionnaire in a clinical sample. Psychol. Assess. 1997, 9, 63–66. [Google Scholar] [CrossRef]
- Jia, C.-X.; Wang, X.-T.; Zhao, Z.-T. Psychometric properties of the suicidal ideation questionnaire among Chinese high school students. Omega 2014, 70, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, W.M. Suicidal Ideation Questionnaire (SIQ); Psychological Assessment Resources: Odessa, FL, USA, 1987. [Google Scholar]
- McCauley, E.; Berk, M.S.; Asarnow, J.R.; Adrian, M.; Cohen, J.; Korslund, K.; Avina, C.; Hughes, J.; Harned, M.; Gallop, R.; et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide a randomized clinical trial. JAMA Psychiatry 2018, 75, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Esfahani, M.; Hashemi, Y.; Alavi, K. Psychometric assessment of beck scale for suicidal ideation (BSSI) in general population in Tehran. Med. J. Islam. Repub. Iran 2015, 29, 268. [Google Scholar] [PubMed]
- Beck, A.T.; Kovacs, M.; Weissman, A. Assessment of Suicidal Intention: The Scale for Suicide Ideation. J. Consult. Clin. Psychol. 1979, 47, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Brown, G.K. Psychometric properties of the scale for suicide ideation in China. Arch. Suicide Res. 2007, 11, 203–210. [Google Scholar] [CrossRef]
- Steeg, S.; Quinlivan, L.; Nowland, R.; Carroll, R.; Casey, D.; Clements, C.; Cooper, J.; Davies, L.; Knipe, D.; Ness, J.; et al. Accuracy of risk scales for predicting repeat self-harm and suicide: A multicentre, population-level cohort study using routine clinical data. BMC Psychiatry 2018, 18, 113. [Google Scholar] [CrossRef]
- Quinlivan, L.; Cooper, J.; Davies, L.; Hawton, K.; Gunnell, D.; Kapur, N. Which are the most useful scales for predicting repeat self-harm? A systematic review evaluating risk scales using measures of diagnostic accuracy. BMJ Open 2016, 6, e009297. [Google Scholar] [CrossRef]
- Cooper, J.; Kapur, N.; Dunning, J.; Guthrie, E.; Appleby, L.; Mackway-Jones, K. A Clinical Tool for Assessing Risk after Self-Harm. Ann. Emerg. Med. 2006, 48, 459–466. [Google Scholar] [CrossRef]
- Stone, A.A.; Shiffman, S. Ecological Momentary Assessment (Ema) in Behavioral Medicine. Ann. Behav. Med. 1994, 16, 199–202. [Google Scholar] [CrossRef]
- May, M.; Junghaenel, D.U.; Ono, M.; Stone, A.A.; Schneider, S. Ecological Momentary Assessment Methodology in Chronic Pain Research: A Systematic Review. J. Pain 2018, 19, 699–716. [Google Scholar] [CrossRef]
- Shiffman, S. Ecological momentary assessment (EMA) in studies of substance use. Psychol. Assess. 2009, 21, 486–497. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Strong, R.; Xu, I.; Fonseca, L.M.; Hawks, Z.; Grinspoon, E.; Jung, L.; Li, F.; Weinstock, R.S.; Sliwinski, M.J.; et al. Ecological Momentary Assessment of Cognition in Clinical and Community Samples: Reliability and Validity Study. J. Med. Internet Res. 2023, 25, e45028. [Google Scholar] [CrossRef] [PubMed]
- Kivelä, L.; van der Does, W.A.J.; Riese, H.; Antypa, N. Don’t Miss the Moment: A Systematic Review of Ecological Momentary Assessment in Suicide Research. Front. Digit. Health 2022, 4, 876595. [Google Scholar] [CrossRef] [PubMed]
- Gee, B.L.; Han, J.; Benassi, H.; Batterham, P.J. Suicidal thoughts, suicidal behaviours and self-harm in daily life: A systematic review of ecological momentary assessment studies. Digit. Health 2020, 6, 2055207620963958. [Google Scholar] [CrossRef]
- Sedano-Capdevila, A.; Porras-Segovia, A.; Bello, H.J.; Baca-García, E.; Luisa Barrigon, M.; Barrigon, M.L. Mood Disorders (E Baca-Garcia, Section Editor) Use of Ecological Momentary Assessment to Study Suicidal Thoughts and Behavior: A Systematic Review. Curr. Psychiatry Rep. 2021, 23, 41. [Google Scholar] [CrossRef]
- Cull, J.G.; Gill, W.S. Suicide Probability Scale. J. Consult. Clin. Psychol. 1988. [Google Scholar] [CrossRef]
- Go, H.-J.; Kim, D.-J.; Lee, H.-P. A validation study of the suicide probability scale for adolescents (SPS-A). J. Korean Neuropsychiatr. Assoc. 2000, 680–690. Available online: https://www.koreamed.org/SearchBasic.php?RID=2340469 (accessed on 16 September 2023).
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861. [Google Scholar] [CrossRef]
- Kim, S.; Lee, E.-H.; Hwang, S.-T.; Hong, S.-H.; Lee, K.; Kim, J.-H. Reliability and validity of the Korean version of the Beck Hopelessness Scale. J. Korean Neuropsychiatr. Assoc. 2015, 54, 84–90. [Google Scholar] [CrossRef]
- Cochrane-Brink, K.A.; Lofchy, J.S.; Sakinofsky, I. Clinical rating scales in suicide risk assessment11Information about the rating scales can be obtained from the author. Gen. Hosp. Psychiatry 2000, 22, 445–451. [Google Scholar] [CrossRef]
- Gutierrez, P.M.; Osman, A.; Barrios, F.X.; Kopper, B.A.; Baker, M.T.; Haraburda, C.M. Development of the reasons for living inventory for young adults. J. Clin. Psychol. 2002, 58, 339–357. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kang, E.; Jeong, J.-W.; Paik, J.-W. Korean suicide risk screening tool and its validity. J. Korea Contents Assoc. 2013, 13, 240–250. [Google Scholar] [CrossRef]
- Ko, S.; You, S. Development and validation of the suicidal imagery questionnaire. Korean J. Clin. Psychol. 2020, 39, 1–14. [Google Scholar] [CrossRef]
- Joiner, T., Jr.; Pfaff, J.J.; Acres, J.G. A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behav. Res. Ther. 2002, 40, 471–481. [Google Scholar] [CrossRef]
- Park, S.-W.; Lee, J.-H.; Lee, E.-K.; Song, J.-J.; Park, H.-S.; Hwang, S.-Y.; Lee, M.-S. Development of the suicide risk scale for medical inpatients. J. Korean Med. Sci. 2018, 33, e18. [Google Scholar] [CrossRef]
- Ghasemi, P.; Shaghaghi, A.; Allahverdipour, H. Measurement Scales of Suicidal Ideation and Attitudes: A Systematic Review Article. Health Promot. Perspect. 2015, 5, 156–168. [Google Scholar] [CrossRef]
- Baek, I.-C.; Jo, S.; Kim, E.J.; Lee, G.R.; Lee, D.H.; Jeon, H.J. A review of suicide risk assessment tools and their measured psychometric properties in Korea. Front. Psychiatry 2021, 12, 679779. [Google Scholar] [CrossRef]
- Arowosegbe, A.; Oyelade, T. Application of Natural Language Processing (NLP) in Detecting and Preventing Suicide Ideation: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 1514. [Google Scholar] [CrossRef]
- Jordan, M.I.; Mitchell, T.M. Machine learning: Trends, perspectives, and prospects. Science 2015, 349, 255–260. [Google Scholar] [CrossRef]
- Batta, M. Machine Learning Algorithms—A Review. Int. J. Sci. Res. 2019, 9, 381–386. [Google Scholar]
- Cliffe, C.; Seyedsalehi, A.; Vardavoulia, K.; Bittar, A.; Velupillai, S.; Shetty, H.; Schmidt, U.; Dutta, R. Using natural language processing to extract self-harm and suicidality data from a clinical sample of patients with eating disorders: A retrospective cohort study. BMJ Open 2021, 11, e053808. [Google Scholar] [CrossRef] [PubMed]
- Van Mens, K.; Elzinga, E.; Nielen, M.; Lokkerbol, J.; Poortvliet, R.; Donker, G.; Heins, M.; Korevaar, J.; Dückers, M.; Aussems, C.; et al. Applying machine learning on health record data from general practitioners to predict suicidality. Internet Interv. 2020, 21, 100337. [Google Scholar] [CrossRef] [PubMed]
- O’Dea, B.; Larsen, M.E.; Batterham, P.J.; Calear, A.L.; Christensen, H. A Linguistic Analysis of Suicide-Related Twitter Posts. Crisis 2017, 38, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Larsen, M.E.; Nicholas, J.; Christensen, H. A systematic assessment of smartphone tools for suicide prevention. PLoS ONE 2016, 11, e0152285. [Google Scholar] [CrossRef]
- Nuij, C.; van Ballegooijen, W.; Ruwaard, J.; de Beurs, D.; Mokkenstorm, J.; van Duijn, E.; de Winter, R.F.P.; O’Connor, R.C.; Smit, J.H.; Riper, H.; et al. Smartphone-based safety planning and self-monitoring for suicidal patients: Rationale and study protocol of the CASPAR (Continuous Assessment for Suicide Prevention And Research) study. Internet Interv. 2018, 13, 16–23. [Google Scholar] [CrossRef]
- NHS England. Stay Alive. Available online: https://www.england.nhs.uk/supporting-our-nhs-people/support-now/wellbeing-apps/stayalive/ (accessed on 2 August 2023).
- Martinengo, L.; Van Galen, L.; Lum, E.; Kowalski, M.; Subramaniam, M.; Car, J. Suicide prevention and depression apps’ suicide risk assessment and management: A systematic assessment of adherence to clinical guidelines. BMC Med. 2019, 17, 231. [Google Scholar] [CrossRef]
- Torok, M.; Han, J.; Baker, S.; Werner-Seidler, A.; Wong, I.; Larsen, M.E.; Christensen, H. Suicide prevention using self-guided digital interventions: A systematic review and meta-analysis of randomised controlled trials. Lancet Digit. Health 2020, 2, e25–e36. [Google Scholar] [CrossRef]
- Pham, K.T.; Nabizadeh, A.; Selek, S. Artificial Intelligence and Chatbots in Psychiatry. Psychiatr. Q. 2022, 93, 249–253. [Google Scholar] [CrossRef]
- Torous, J.; Bucci, S.; Bell, I.H.; Kessing, L.V.; Faurholt-Jepsen, M.; Whelan, P.; Carvalho, A.F.; Keshavan, M.; Linardon, J.; Firth, J. The growing field of digital psychiatry: Current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 2021, 20, 318–335. [Google Scholar] [CrossRef]
- Lin, A.P.C.; Trappey, C.V.; Luan, C.-C.; Trappey, A.J.C.; Tu, K.L.K. A Test Platform for Managing School Stress Using a Virtual Reality Group Chatbot Counseling System. Appl. Sci. 2021, 11, 9071. [Google Scholar] [CrossRef]
- Castillo-Sánchez, G.; Camargo-Henríquez, I.; Muñoz-Sánchez, J.L.; Franco-Martín, M.; De La Torre-Díez, I. Suicide Prevention Mobile Apps: Descriptive Analysis of Apps from the Most Popular Virtual Stores. JMIR Mhealth Uhealth 2019, 7, e13885. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Board on Neuroscience and Behavioral Health. Social and Cultural Factors in Suicide Risk. In Risk Factors for Suicide: Summary of a Workshop; National Academies Press: Washington, DC, USA, 2001. Available online: https://www.ncbi.nlm.nih.gov/books/NBK223752/ (accessed on 17 September 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arowosegbe, A.; Oyelade, T. Suicide Risk Assessment and Prevention Tools in the UK: Current Landscape and Future Directions. Psychiatry Int. 2023, 4, 354-369. https://doi.org/10.3390/psychiatryint4040032
Arowosegbe A, Oyelade T. Suicide Risk Assessment and Prevention Tools in the UK: Current Landscape and Future Directions. Psychiatry International. 2023; 4(4):354-369. https://doi.org/10.3390/psychiatryint4040032
Chicago/Turabian StyleArowosegbe, Abayomi, and Tope Oyelade. 2023. "Suicide Risk Assessment and Prevention Tools in the UK: Current Landscape and Future Directions" Psychiatry International 4, no. 4: 354-369. https://doi.org/10.3390/psychiatryint4040032
APA StyleArowosegbe, A., & Oyelade, T. (2023). Suicide Risk Assessment and Prevention Tools in the UK: Current Landscape and Future Directions. Psychiatry International, 4(4), 354-369. https://doi.org/10.3390/psychiatryint4040032





