Gut Microbiota Research in Bipolar Disorder and Possible Implications for Precision Psychiatry: A Systematic Review
Abstract
:1. Introduction
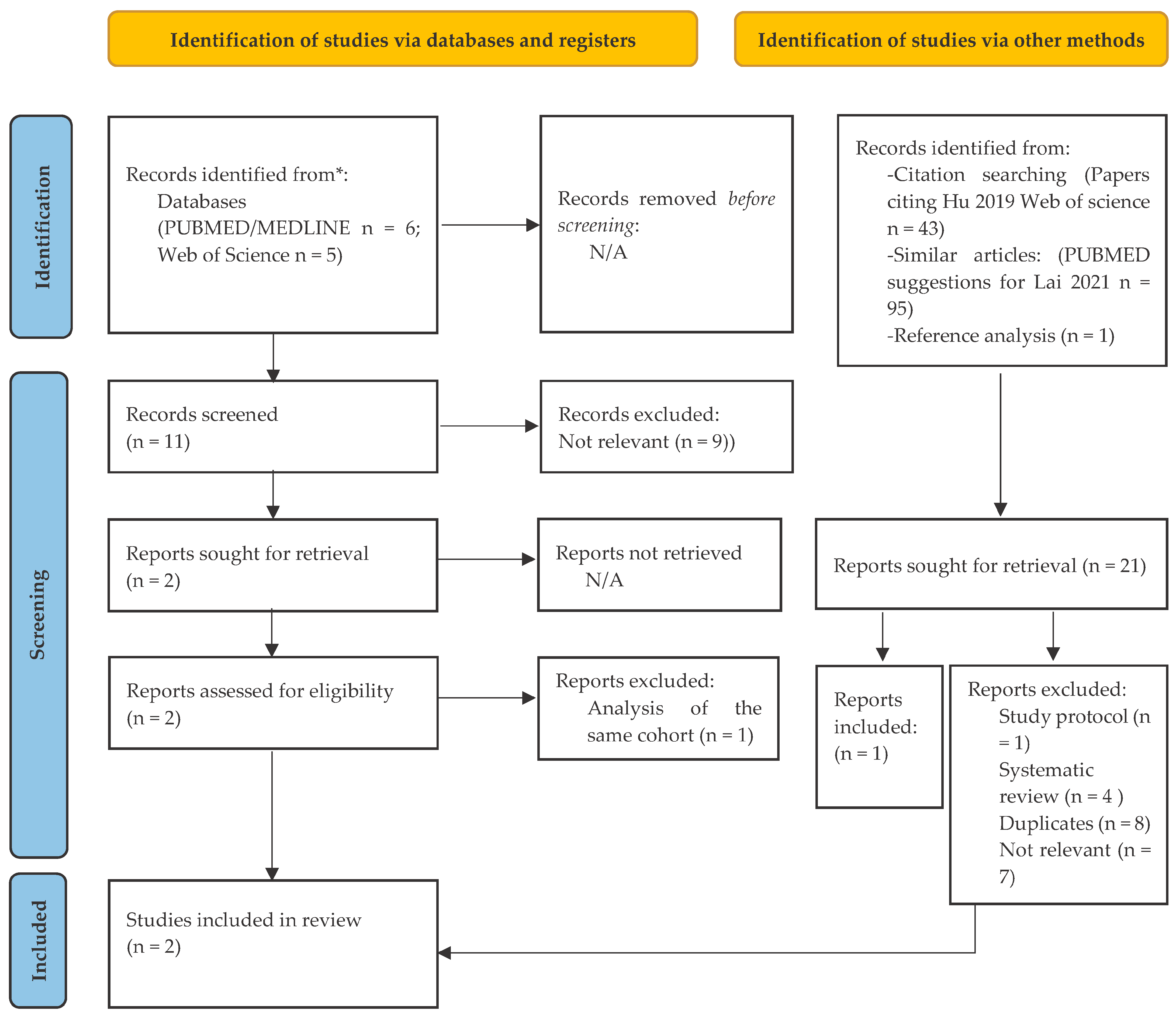
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrari, A.J.; Stockings, E.; Khoo, J.P.; Erskine, H.E.; Degenhardt, L.; Vos, T.; Whiteford, H.A. The prevalence and burden of bipolar disorder: Findings from the Global Burden of Disease Study 2013. Bipolar Disord. 2016, 18, 440–450. [Google Scholar] [CrossRef]
- Dome, P.; Rihmer, Z.; Gonda, X. Suicide Risk in Bipolar Disorder: A Brief Review. Medicina 2019, 55, 403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, B.I.; Baune, B.T.; Bond, D.J.; Chen, P.H.; Eyler, L.; Fagiolini, A.; Gomes, F.; Hajek, T.; Hatch, J.; McElroy, S.L.; et al. Call to action regarding the vascular-bipolar link: A report from the Vascular Task Force of the International Society for Bipolar Disorders. Bipolar Disord. 2020, 22, 440–460. [Google Scholar] [CrossRef]
- Leboyer, M.; Soreca, I.; Scott, J.; Frye, M.; Henry, C.; Tamouza, R.; Kupfer, D.J. Can bipolar disorder be viewed as a multi-system inflammatory disease? J. Affect. Disord. 2012, 141, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almeida, O.P.; McCaul, K.; Hankey, G.J.; Yeap, B.B.; Golledge, J.; Flicker, L. Risk of dementia and death in community-dwelling older men with bipolar disorder. Br. J. Psychiatry 2016, 209, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Chesney, E.; Goodwin, G.M.; Fazel, S. Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry 2014, 13, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bessonova, L.; Ogden, K.; Doane, M.J.; O’Sullivan, A.K.; Tohen, M. The Economic Burden of Bipolar Disorder in the United States: A Systematic Literature Review. Clin. Outcomes Res. CEOR 2020, 12, 481–497. [Google Scholar] [CrossRef]
- Ekman, M.; Granstrom, O.; Omerov, S.; Jacob, J.; Landen, M. The societal cost of bipolar disorder in Sweden. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, G.M.; Haddad, P.M.; Ferrier, I.N.; Aronson, J.K.; Barnes, T.; Cipriani, A.; Coghill, D.R.; Fazel, S.; Geddes, J.R.; Grunze, H.; et al. Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 2016, 30, 495–553. [Google Scholar] [CrossRef]
- Fountoulakis, K.N.; Vieta, E.; Young, A.; Yatham, L.; Grunze, H.; Blier, P.; Moeller, H.J.; Kasper, S. The International College of Neuropsychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 4: Unmet Needs in the Treatment of Bipolar Disorder and Recommendations for Future Research. Int. J. Neuropsychopharmacol. Off. Sci. J. Coll. Int. Neuropsychopharmacol. (CINP) 2017, 20, 196–205. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence [NICE]. Available online: https://www.nice.org.uk (accessed on 21 February 2022).
- Bowden, C.L.; Perlis, R.H.; Thase, M.E.; Ketter, T.A.; Ostacher, M.M.; Calabrese, J.R.; Reilly-Harrington, N.A.; Gonzalez, J.M.; Singh, V.; Nierenberg, A.A.; et al. Aims and results of the NIMH systematic treatment enhancement program for bipolar disorder (STEP-BD). CNS Neurosci. Ther. 2012, 18, 243–249. [Google Scholar] [CrossRef]
- Geddes, J.R.; Miklowitz, D.J. Treatment of bipolar disorder. Lancet 2013, 381, 1672–1682. [Google Scholar] [CrossRef]
- Yalin, N.; Young, A.H. Pharmacological Treatment of Bipolar Depression: What are the Current and Emerging Options? Neuropsychiatr. Dis. Treat. 2020, 16, 1459–1472. [Google Scholar] [CrossRef] [PubMed]
- Lubloy, A.; Kereszturi, J.L.; Nemeth, A.; Mihalicza, P. Exploring factors of diagnostic delay for patients with bipolar disorder: A population-based cohort study. BMC Psychiatry 2020, 20, 75. [Google Scholar] [CrossRef] [Green Version]
- Kessler, R.C.; Luedtke, A. Pragmatic Precision Psychiatry-A New Direction for Optimizing Treatment Selection. JAMA Psychiatry 2021, 78, 1384–1390. [Google Scholar] [CrossRef] [PubMed]
- Salagre, E.; Dodd, S.; Aedo, A.; Rosa, A.; Amoretti, S.; Pinzon, J.; Reinares, M.; Berk, M.; Kapczinski, F.P.; Vieta, E.; et al. Toward Precision Psychiatry in Bipolar Disorder: Staging 2.0. Front. Psychiatry 2018, 9, 641. [Google Scholar] [CrossRef] [Green Version]
- Denny, J.C.; Collins, F.S. Precision medicine in 2030-seven ways to transform healthcare. Cell 2021, 184, 1415–1419. [Google Scholar] [CrossRef] [PubMed]
- Ashley, E.A. Towards precision medicine. Nat. Rev. Genet. 2016, 17, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, E.; Hens, K. Microbiome in Precision Psychiatry: An Overview of the Ethical Challenges Regarding Microbiome Big Data and Microbiome-Based Interventions. AJOB Neurosci. 2021, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Zeng, B.; Zhou, C.; Liu, M.; Fang, Z.; Xu, X.; Zeng, L.; Chen, J.; Fan, S.; Du, X.; et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry 2016, 21, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Sampson, T.R.; Debelius, J.W.; Thron, T.; Janssen, S.; Shastri, G.G.; Ilhan, Z.E.; Challis, C.; Schretter, C.E.; Rocha, S.; Gradinaru, V.; et al. Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson’s Disease. Cell 2016, 167, 1469–1480.e12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, F.; Guo, R.; Wang, W.; Ju, Y.; Wang, Q.; Ma, Q.; Sun, Q.; Fan, Y.; Xie, Y.; Yang, Z.; et al. Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice. Mol. Psychiatry 2020, 25, 2905–2918. [Google Scholar] [CrossRef] [PubMed]
- Horsley, T.; Dingwall, O.; Sampson, M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst. Rev. 2011, MR000026. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.MR000026/full (accessed on 21 February 2022). [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ott. Ott. Hosp. Res. Inst. 2011, 2, 1–12. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Li, A.; Huang, T.; Lai, J.; Li, J.; Sublette, M.E.; Lu, H.; Lu, Q.; Du, Y.; Hu, Z.; et al. Gut Microbiota Changes in Patients with Bipolar Depression. Adv. Sci. 2019, 6, 1900752. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Li, A.; Jiang, J.; Yuan, X.; Zhang, P.; Xi, C.; Wu, L.; Wang, Z.; Chen, J.; Lu, J.; et al. Metagenomic analysis reveals gut bacterial signatures for diagnosis and treatment outcome prediction in bipolar depression. Psychiatry Res. 2022, 307, 114326. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Yang, J.; Li, Y.; Wu, J.; Liang, W.; Yin, B.; Tan, X.; Huang, Y.; Chai, T.; Zhang, H.; et al. Gut Microbial Signatures Can Discriminate Unipolar from Bipolar Depression. Adv. Sci. 2020, 7, 1902862. [Google Scholar] [CrossRef]
- Wells, P.M.; Adebayo, A.S.; Bowyer, R.C.E.; Freidin, M.B.; Finckh, A.; Strowig, T.; Lesker, T.R.; Alpizar-Rodriguez, D.; Gilbert, B.; Kirkham, B.; et al. Associations between gut microbiota and genetic risk for rheumatoid arthritis in the absence of disease: A cross-sectional study. Lancet Rheumatol. 2020, 2, e418–e427. [Google Scholar] [CrossRef]
- Painold, A.; Morkl, S.; Kashofer, K.; Halwachs, B.; Dalkner, N.; Bengesser, S.; Birner, A.; Fellendorf, F.; Platzer, M.; Queissner, R.; et al. A step ahead: Exploring the gut microbiota in inpatients with bipolar disorder during a depressive episode. Bipolar Disord. 2019, 21, 40–49. [Google Scholar] [CrossRef] [Green Version]
- Evans, S.J.; Bassis, C.M.; Hein, R.; Assari, S.; Flowers, S.A.; Kelly, M.B.; Young, V.B.; Ellingrod, V.E.; McInnis, M.G. The gut microbiome composition associates with bipolar disorder and illness severity. J. Psychiatr. Res. 2017, 87, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simpson, C.A.; Adler, C.; du Plessis, M.R.; Landau, E.R.; Dashper, S.G.; Reynolds, E.C.; Schwartz, O.S.; Simmons, J.G. Oral microbiome composition, but not diversity, is associated with adolescent anxiety and depression symptoms. Physiol. Behav. 2020, 226, 113126. [Google Scholar] [CrossRef]
- Nikolova, V.L.; Hall, M.R.B.; Hall, L.J.; Cleare, A.J.; Stone, J.M.; Young, A.H. Perturbations in Gut Microbiota Composition in Psychiatric Disorders: A Review and Meta-analysis. JAMA Psychiatry 2021, 78, 1343–1354. [Google Scholar] [CrossRef] [PubMed]
- Bengesser, S.A.; Morkl, S.; Painold, A.; Dalkner, N.; Birner, A.; Fellendorf, F.T.; Platzer, M.; Queissner, R.; Hamm, C.; Maget, A.; et al. Epigenetics of the molecular clock and bacterial diversity in bipolar disorder. Psychoneuroendocrinology 2019, 101, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Corlett, P.R.; Schoenbaum, G. Leveraging Basic Science for the Clinic-From Bench to Bedside. JAMA Psychiatry 2021, 78, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Zhang, P.; Jiang, J.; Mou, T.; Li, Y.; Xi, C.; Wu, L.; Gao, X.; Zhang, D.; Chen, Y.; et al. New Evidence of Gut Microbiota Involvement in the Neuropathogenesis of Bipolar Depression by TRANK1 Modulation: Joint Clinical and Animal Data. Front. Immunol. 2021, 12, 789647. [Google Scholar] [CrossRef] [PubMed]
- Payelleville, A.; Brillard, J. Novel Identification of Bacterial Epigenetic Regulations Would Benefit From a Better Exploitation of Methylomic Data. Front. Microbiol. 2021, 12, 685670. [Google Scholar] [CrossRef]
| First Author, Year | Lai et al., 2022 [28] | Zheng et al., 2020 [29] |
|---|---|---|
| Study characteristics |
|
|
| Studied variables |
|
|
| Region of studies | East Asia | East Asia |
| Main findings |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paribello, P.; Pinna, F.; Carpiniello, B.; Manchia, M. Gut Microbiota Research in Bipolar Disorder and Possible Implications for Precision Psychiatry: A Systematic Review. Psychiatry Int. 2022, 3, 114-121. https://doi.org/10.3390/psychiatryint3010009
Paribello P, Pinna F, Carpiniello B, Manchia M. Gut Microbiota Research in Bipolar Disorder and Possible Implications for Precision Psychiatry: A Systematic Review. Psychiatry International. 2022; 3(1):114-121. https://doi.org/10.3390/psychiatryint3010009
Chicago/Turabian StyleParibello, Pasquale, Federica Pinna, Bernardo Carpiniello, and Mirko Manchia. 2022. "Gut Microbiota Research in Bipolar Disorder and Possible Implications for Precision Psychiatry: A Systematic Review" Psychiatry International 3, no. 1: 114-121. https://doi.org/10.3390/psychiatryint3010009
APA StyleParibello, P., Pinna, F., Carpiniello, B., & Manchia, M. (2022). Gut Microbiota Research in Bipolar Disorder and Possible Implications for Precision Psychiatry: A Systematic Review. Psychiatry International, 3(1), 114-121. https://doi.org/10.3390/psychiatryint3010009







