1. Introduction
The seasonality of admissions for severe mental illness has been consistently demonstrated, with statistically significant peaks for patients with affective [
1,
2] and schizophrenia [
3,
4] disorders. Severe mental illness is also associated with involuntary admissions, as schizophrenia and bipolar disorders are the most frequent diagnoses among involuntary admitted patients [
5].
The involuntary treatment of psychiatric disorders has been controversial [
6] as coercive practices are not consistent with human-rights-based mental healthcare, and the use of involuntary admissions can also be traumatic not only for patients but their relatives too [
7]. Despite the efforts of the World Health Organization to internationally standardize strategies for mental health care delivery [
5], mental health legislation varies considerably from one country to the other [
8].
The conditions of involuntary hospitalization in Greece, as defined by legal framework (Law 2071/1992), are the following: (i) a person suffers from mental illness, (ii) due to the mental illness, the person is unable to look after itself, and (iii) the disorder will not subside if untreated and, as a result, the person’s life or the life of others is at threat [
9].
The present study aims to describe the seasonal and long-term influences on involuntary mental health admissions in Attica, Greece, focusing on the sociodemographic (sex, age) and diagnostic characteristics of the participants, who may be affected by the impact of seasonality.
2. Materials and Methods
The study sample comprised 6853 individuals who came for assessment from 1 January 2010 to 31 December 2017 at the Psychiatric Hospital of Attica “Dafni” in Attica region, Greece, and were involuntarily hospitalized with a mental disorder diagnosis. Patients with insufficient information regarding their residency (e.g., migrants, refugees, unknown residence, and homeless) and those who were less than 18 years old were excluded from the study (n = 3302).
Data were summarized using absolute (N) and relative (%) frequencies for categorical variables, while for continuous ones, medians and interquartile ranges (IQR; 25th and 75th percentile) were used. Daily numbers of hospitalizations were summarized using their mean and standard deviation (SD) as their distribution was approaching normality while their small values rendered the use of median and IQR less informative. Descriptive measures are given overall and by demographic characteristics, diagnosis, or month of hospitalization. Comparisons between groups for categorical variables were performed using chi-square tests, whereas for continuous variables, non-parametric tests (Mann–Whitney or Kruskal–Wallis as appropriate) were used.
Due to the irregularity of the time series data (data were available for approximately two days per week when the hospital was on call), typical methods of time series analysis could not be used. Thus, all analyses were based on Poisson models for counts, but seasonality effects, long-term trends, differences in the size of the underlying populations (by sex or by age group), and potential violations of the models’ assumptions were taken into account.
Periodic trends within each calendar year (seasonality) were allowed by including appropriate Fourier terms (i.e., pairs of cosine and sine functions with period of 1, 1/2, 1/3 … years) in the models. Formal investigation, using information criteria and likelihood ratio tests, revealed that Fourier terms of degree >1 were not statistically significant, thus all models included one pair of 1-year period cosine and sine functions. Long-term trends were investigated by including either restricted cubic spline functions or a linear time term. Both formal and graphical assessment supported the use of just one linear time term for modeling long-term trends. The size of the population at risk by sex and by age group was used as an offset term after logarithmic transformation. Relevant data were retrieved from the Hellenic Statistical Authority (2011 census). In all models, robust standard errors were used, and in cases where more than one observation per day were analyzed (e.g., in the analysis of number of daily hospitalizations by sex), generalized estimating equations were used with an exchangeable correlation matrix to account for potential correlation between multiple observations during the same day. All model-related p-values were derived using Wald-type tests.
p-values less than 0.05 were considered as indicating statistical significance. All analyses were performed using Stata version 14 (Stat Corp., College Station, TX, USA).
3. Results
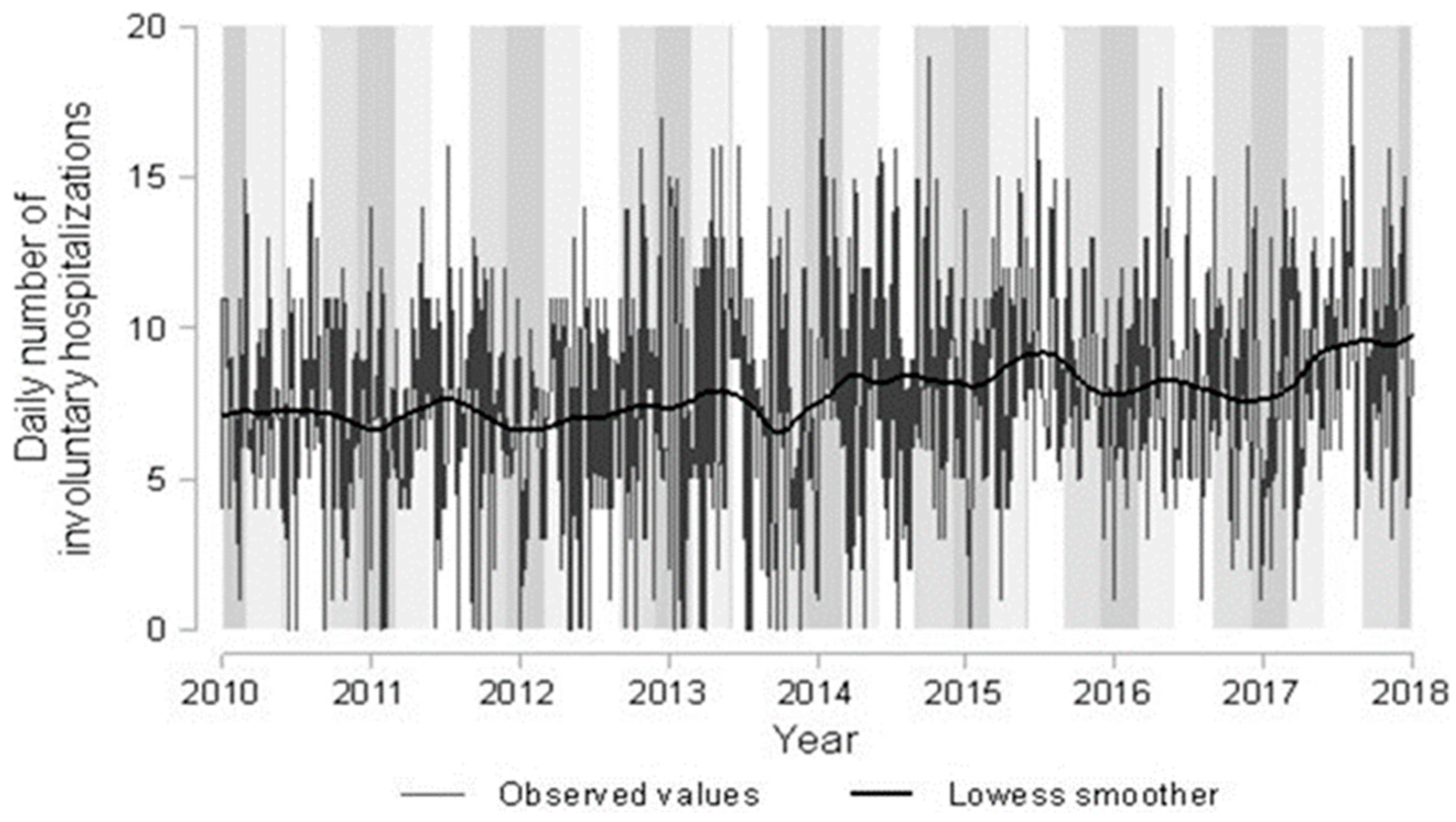
The daily numbers of involuntary hospitalizations are graphically presented, over the whole study period, in
Figure 1 and summarized per month (overall and by sex) in
Table 1.
Figure 1 reveals substantial day-to-day variation, with the daily numbers of involuntary hospitalizations ranging from 0 (in 38/882 days) to 20 (35/882 days with ≥15 involuntary hospitalizations). The same figure shows a potential increasing trend over the years as the average numbers seem to increase from approximately 7 in the beginning of 2010 to 10 at the end of 2017. The superimposed smoothing curve in this figure shows also that there are probably some peaks coinciding in most cases with the end of spring and start of summer, while most nadirs seem to happen in the middle of winter.
Table 1 (column “Overall”) also supports some seasonal variation, with the highest average numbers corresponding to May and June and the lowest to December and January.
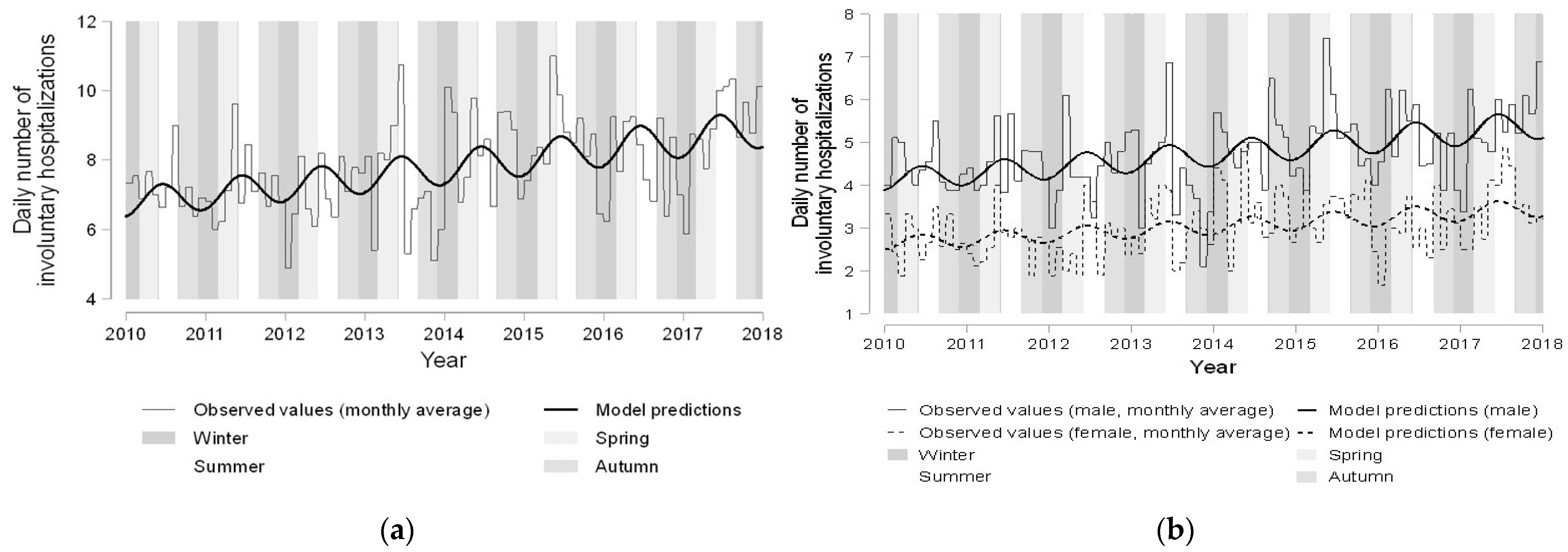
Modeling of the daily numbers of involuntary hospitalizations verified the presence of both long-term and seasonal variation. The long-term trend was highly significant (p < 0.001), and the model’s estimate corresponded to a 4% increase in the number of involuntary hospitalizations per year. The seasonality terms were also statistically significant (p = 0.017). According to the model’s results, the maximum numbers of involuntary hospitalizations within each year are expected on the 14th of June and the minimum on the 13th of December, on average, with the corresponding differences relative to the mean year values being +6.5% and −6.1%, respectively.
Predictions of this model along with monthly averages of hospitalization numbers are shown in
Figure 2a. In this Figure, the model seems to track the long-term trend very well. Tracking of the seasonality effects is adequate, but it is obvious that there is no perfect periodicity in all years, with the zeniths and nadirs occurring earlier in some years and later in others compared with the average predictions of the model. Seasonality and long-term trends were also investigated according to patients’ sex, age, and diagnosis.
Table 1 (columns “Male” and “Female”) shows average numbers of daily involuntary hospitalizations separately for men and women. The overall pattern for higher numbers in late spring or early summer and lower numbers in winter seems to persist in both men and women. The modeling results showed that both seasonality and long-term trends did not differ significantly between men and women (
p-values 0.241 and 0.675, respectively), thus the findings of the previous overall model practically hold for both sexes. However, as expected by the descriptive measures discussed earlier, the incidence of involuntary hospitalizations was significantly (
p < 0.001) lower in women (relative difference−41.5%;). Predictions of this model along with monthly averaged values of daily numbers of involuntary hospitalizations by sex are graphically presented in
Figure 2b.
Similar analyses were performed for differences by age and diagnosis (
Table 2). Regarding the monthly averaged numbers, the low number of patients in the youngest or oldest age category (and similarly for those with diagnoses other than F20–F29) render those results unstable, and any seasonality effects within these subgroups are difficult to identify. The modeling results showed that any differences regarding seasonality patterns were not significant across age groups nor across groups of patients with different diagnoses. However, long-term trends differed significantly both across age (
p < 0.001) and diagnoses groups (
p < 0.001).
Model predictions of only the long-term trends are shown in
Figure 3. The frequency of involuntary hospitalization increases in the oldest (above 65 years old) and youngest (16–29 years old) groups along with those aged 50 to 64, whereas for those aged between 30 and 49, estimates indicate stability or even decreasing trends. The estimated (95% CI;
p-value) relative changes in the frequency of involuntary hospitalization per year were 4.6% (
p = 0.004), −0.8% (
p = 0.472), 1.7% (
p = 0.137), 5.1% (
p < 0.001), and 12.4% (
p < 0.001) for those aged 16–29, 30–39, 40–49, 50–64, and 65+ years old, respectively (
Figure 3a). Regarding differences in long-term trends by diagnosis, the most common groups of F20–F29 and F30–F39 seem to increase very slowly, but the less common F11–F19 and especially F00–F09 tend to increase much faster over the years (
Figure 3b). The estimated (95% CI;
p-value) relative changes in the frequency of involuntary hospitalization per year were 1.3% (
p = 0.080), 18.7% (
p < 0.001), 3.3% (
p = 0.384), 7.3% (
p = 0.002), and 2.8% (0.0% to 5.7%;
p = 0.05) for diagnoses F20–F29, F00–F09, F10, F11–F19, and F30–F39, respectively.
4. Discussion
This study supports previous findings of a spring/summer peak for total severe mental admissions, mainly for schizophrenia and affective disorders. The results indicate seasonal influences on involuntary admissions, with late spring (May) and early summer (June) peaks and the nadir in the middle of winter (December and January). These findings strengthen previous evidence that patients with involuntary hospitalizations showed a higher prevalence of admission in spring and summer, with a significant peak in June, especially for bipolar-related disorders [
10]. Schizophrenia disorder total admissions also showed a peak in June, but a seasonal significant pattern was not found [
11].
Although our study showed the same late spring–early summer seasonal pattern for involuntary admissions for both sexes, other studies for affective disorder total admissions [
1,
2] found a different seasonal pattern or no seasonal peak for males and females. The results from other studies for total schizophrenia admissions are inconclusive, as hospitalizations for both sexes followed the same [
12] or a different [
13] seasonal pattern.
Regarding long-term trends by diagnosis, unlike previous findings for total admissions [
14], a slow increase in F20–F29 (schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders) and F30–F39 (mood [affective] disorders) groups and a much faster increase in F11–F19 (mental and behavioral disorders due to psychoactive substance use) and especially F00–F09 (organic, including symptomatic, mental disorders) diagnostic groups of involuntary admissions was observed over the years. Moreover, in terms of long-term trends by age, involuntary admissions showed an increase for patients above 65 years old and those between 16 and 29 years of age.
The seasonal variability and different results which appeared in the scientific research are probably due to that, in addition to seasonal factors, biological, psychological, and social factors are involved in causing mental health disorders [
15], which may differ not only among but also within countries. There is also evidence that seasonal effects may have more pronounced variations within climatic zones in the northern hemisphere [
16].
This is an eight-year retrospective time series study with a large number of admissions; the diagnostic criteria did not change over the study period. Our study had several limitations: the findings are based on hospital admission data rather than the actual onset of the acute episode; factors that could contribute to the onset of an acute psychiatric episode have not been taken into consideration; the seasonal pattern of involuntary admitted patients may differ from those who are voluntary hospitalized; and we did not exclude readmissions of the same patient within the time period of the study.
Notwithstanding these limitations, this study is one of the first steps to investigate the effect of seasonality on involuntary hospitalization as we identified seasonal patterns for total sample and for both sexes and significant long-term trend increases in the number of involuntary hospitalizations per year by age and diagnoses.
Author Contributions
Conceptualization, I.R. and A.D.; methodology, N.P. and K.L.; software, N.P.; validation, R.G., E.M. and A.D.; formal analysis, N.P.; investigation, N.P. and A.D.; resources, I.R. and E.M.; data curation, R.G. and K.L.; writing—original draft preparation, I.R.; writing—review and editing, I.R., R.G., K.L. and A.D.; visualization, I.R. and E.M.; supervision, A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The research proposal of the study was formally approved by the Hospital Board and the Ethics Committee of Psychiatric Hospital of Attica “Dafni” (protocol code 4990/13-02-2020 and date of approval 8 April 2020).
Informed Consent Statement
Patient consent was waived due to the fact that patients’ data were anonymous before they were used (data from a public hospital register).
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Whitney, D.K.; Sharma, V.; Kueneman, K. Seasonality of manic depressive illness in Canada. J. Affect. Disord. 1999, 55, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Dominiak, M.; Swiecicki, L.; Rybakowski, J. Psychiatric hospitalizations for affective disorders in Warsaw, Poland: Effect of season and intensity of sunlight. Psychiatry Res. 2015, 229, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Hinterbuchinger, B.; König, D.; Gmeiner, A.; Listabarth, S.; Fellinger, M.; Thenius, C.; Pruckner, N. Seasonality in schizophrenia-An analysis of a nationwide registry with 110,735 hospital admissions. Eur. Psychiatry 2020, 63. [Google Scholar] [CrossRef] [PubMed]
- Shiloh, R.; Shapira, A.; Potchter, O.; Hermesh, H.; Popper, M.; Weizman, A. Effects of climate on admission rates of schizophrenia patients to psychiatric hospitals. Eur. Psychiatry 2005, 20, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.P.; Chiu, C.C.; Yang, T.H.; Liu, T.H.; Wu, C.Y.; Chou, P. The low proportion and associated factors of involuntary admission in the psychiatric emergency service in Taiwan. PLoS ONE 2015, 10, e0129204. [Google Scholar] [CrossRef] [PubMed]
- Douzenis, A.; Michopoulos, I. Involuntary admission: The case of anorexia nervosa. Int. J. Law Psych. 2015, 39, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Sashidharan, S.P.; Mezzina, R.; Puras, D. Reducing coercion in mental healthcare. Epidemiol. Psychiatr. Sci. 2019, 28, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Douzenis, A.; Michopoulos, I.; Economou, M.; Rizos, E.; Christodoulou, C.; Lykouras, L. Involuntary admission in Greece: A prospective national study of police involvement and client characteristics affecting emergency assessment. Int. J. Soc. Psychiatry 2012, 58, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Stylianidis, S.; Peppou, L.E.; Drakonakis, N.; Douzenis, A.; Panagou, A.; Tsikou, K.; Pantazi, A.; Rizavas, Y.; Saraceno, B. Mental health care in Athens: Are compulsory admissions in Greece a one-way road? Int. J. Law Psych. 2017, 52, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Aguglia, A.; Moncalvo, M.; Solia, F.; Maina, G. Involuntary admissions in Italy: The impact of seasonality. Int. J. Psychiatry Clin. Pract. 2016, 20, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz, I.; Heitzman, J.; Gardyńska-Ziemba, E. Involuntary psychiatric holds-the structure of admissions on the example of Institute of Psychiatry and Neurology in Warsaw. Psychiatr. Pol. 2016, 50, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Takei, N.; Murray, R.M. Gender difference of schizophrenia in seasonal admissions in Scotland. Br. J. Psychiatry 1993, 162, 272–273. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Mellsop, G.; Brink, J.; Wang, X. Involuntary admission and treatment of patients with mental disorder. Neurosci. Bull. 2015, 31, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Medici, C.R.; Vestergaard, C.H.; Hadzi-Pavlovic, D.; Munk-Jørgensen, P.; Parker, G. Seasonal variations in hospital admissions for mania: Examining for associations with weather variables over time. J. Affect. Disord. 2016, 205, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Lykouras, L.; Douzenis, A. Do psychiatric departments in general hospitals have an impact on the physical health of mental patients? Curr. Opin. Psychiatry 2008, 21, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Geoffroy, P.A.; Bellivier, F.; Scott, J.; Etain, B. Seasonality and bipolar disorder: A systematic review, from admission rates to seasonality of symptoms. J. Affect. Disord. 2014, 168, 210–223. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).