Are Complete Blood Count Parameters Associated with Climate and Environmental Factors? A Retrospective Study in the General Population of Fokis, Greece (Athens, 2023) †
Abstract
1. Introduction
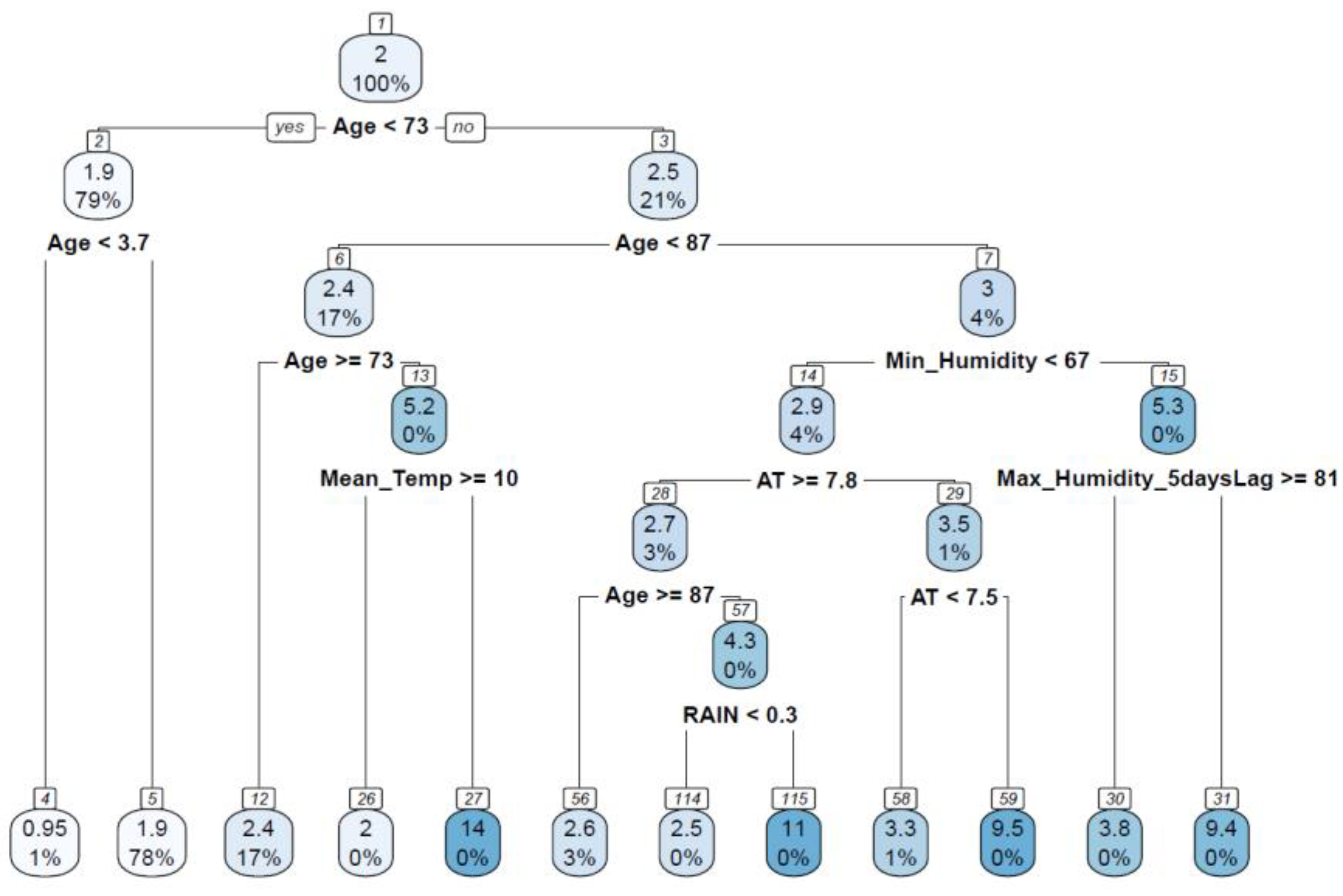
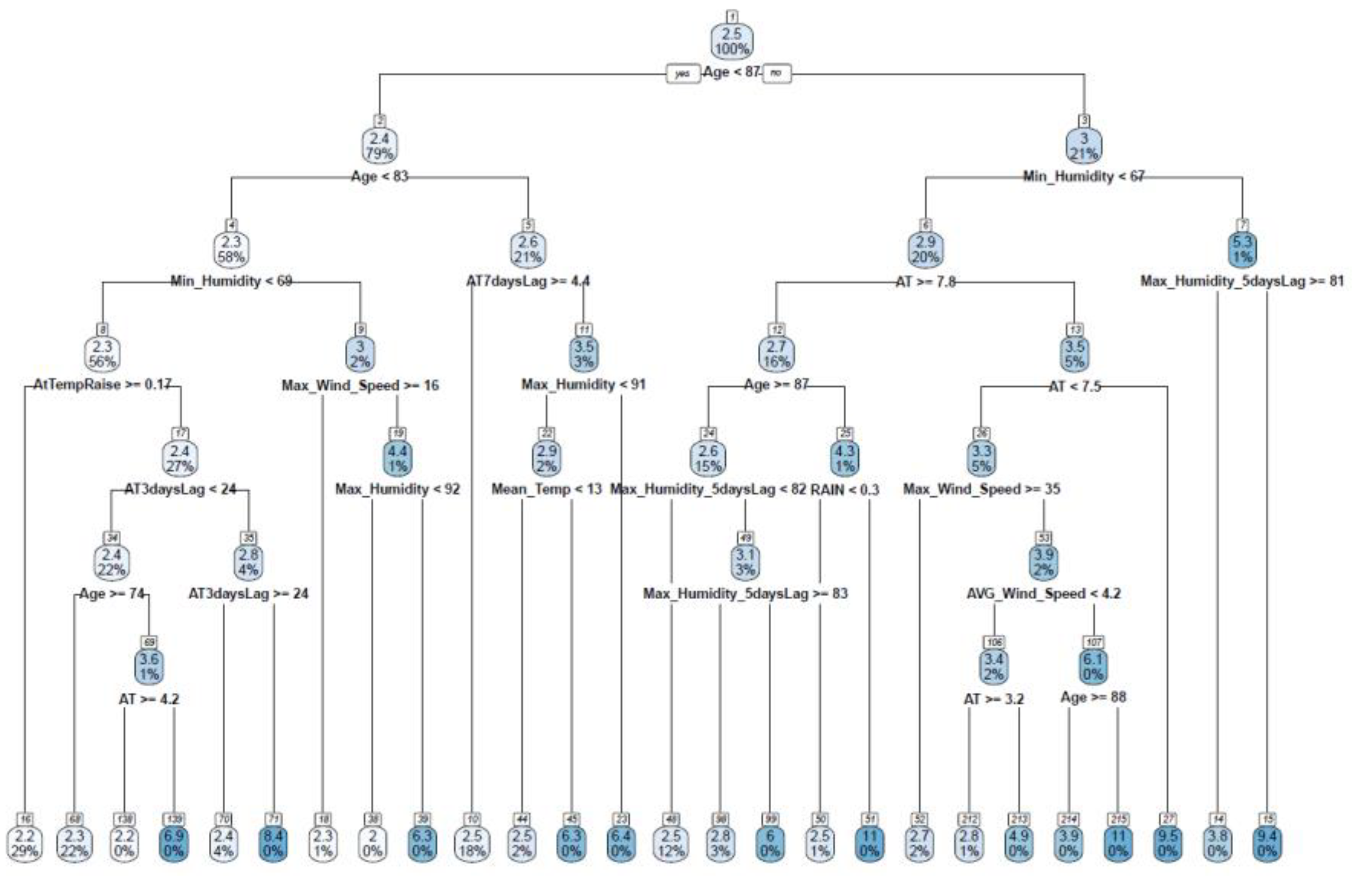
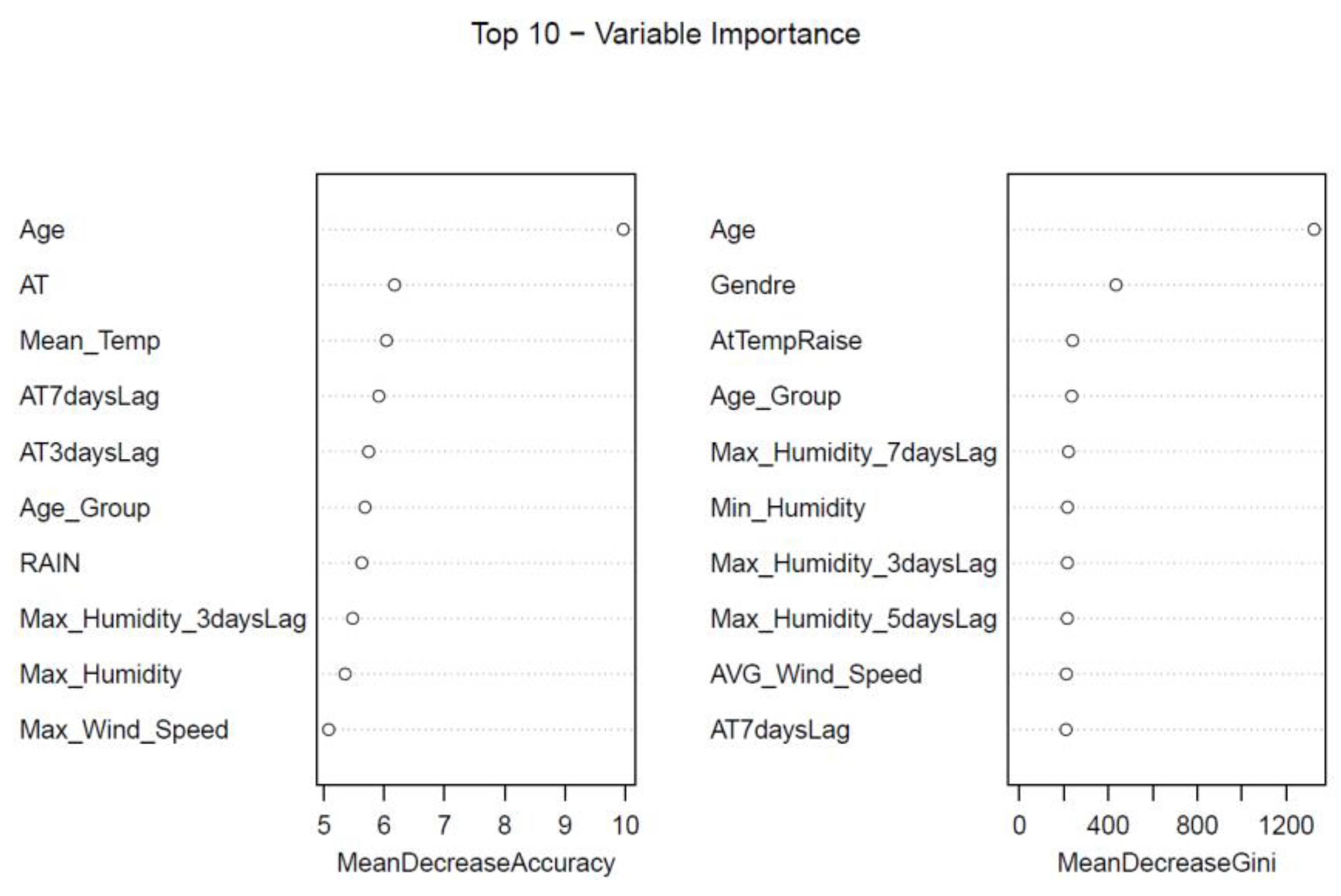
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Varela, M.L.; Mogildea, M.; Moreno, I.; Lopes, A. Acute Inflammation and Metabolism. Inflammation 2018, 41, 1115–1127. [Google Scholar] [CrossRef]
- Wang, Q.; Zhao, Q.; Wang, G.; Wang, B.; Zhang, Y.; Zhang, J.; Li, N.; Zhao, Y.; Qiao, H.; Li, W.; et al. The association between ambient temperature and clinical visits for inflammation-related diseases in rural areas in China. Environ. Pollut. 2020, 261, 114128. [Google Scholar] [CrossRef] [PubMed]
- Pawłowska, M.; Mila-Kierzenkowska, C.; Boraczyński, T.; Boraczyński, M.; Szewczyk-Golec, K.; Sutkowy, P.; Wesołowski, R.; Budek, M.; Woźniak, A. The Influence of Ambient Temperature Changes on the Indicators of Inflammation and Oxidative Damage in Blood after Submaximal Exercise. Antioxidants 2022, 11, 2445. [Google Scholar] [CrossRef]
- Schneider, A.; Panagiotakos, D.; Picciotto, S.; Katsouyanni, K.; Löwel, H.; Jacquemin, B.; Lanki, T.; Stafoggia, M.; Bellander, T.; Koenig, W.; et al. Air temperature and inflammatory responses in myocardial infarction survivors. Epidemiology 2008, 19, 391–400. [Google Scholar] [CrossRef]
- Basu, R.; May Wu, X.; Malig, B.J.; Broadwin, R.; Gold, E.B.; Qi, L.; Derby, C.; Jackson, E.A.; Green, R.S. Estimating the associations of apparent temperature and inflammatory, hemostatic, and lipid markers in a cohort of midlife women. Environ. Res. 2017, 152, 322–327. [Google Scholar] [CrossRef]
- De Figueiredo, E.C.; Figueiredo, G.C.; Dantas, R.T. Influence of meteorological elements on osteoarthritis pain: A review of the literature. Rev. Bras. Reumatol. 2011, 51, 622–628. [Google Scholar] [CrossRef]
- Bongers, J.; Vandenneucker, H. The influence of weather conditions on osteoarthritis and joint pain after prosthetic surgery. Acta Orthop. Belg. 2020, 86, 1–9. [Google Scholar] [PubMed]
- Zahorec, R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl. Lek. Listy 2021, 122, 474–488. [Google Scholar] [CrossRef]
- Novellino, F.; Donato, A.; Malara, N.; Madrigal, J.L.; Donato, G. Complete blood cell count-derived ratios can be useful biomarkers for neurological diseases. Int. J. Immunopathol. Pharmacol. 2021, 35, 20587384211048264. [Google Scholar] [CrossRef]
- Buonacera, A.; Stancanelli, B.; Colaci, M.; Malatino, L. Neutrophil to Lymphocyte Ratio: An Emerging Marker of the Relationships between the Immune System and Diseases. Int. J. Mol. Sci. 2022, 23, 3636. [Google Scholar] [CrossRef]
- Lin, N.; Li, J.; Yao, X.; Zhang, X.; Liu, G.; Zhang, Z.; Weng, S. Prognostic value of neutrophil-to-lymphocyte ratio in colorectal cancer liver metastasis: A meta-analysis of results from multivariate analysis. Int. J. Surg. 2022, 107, 106959. [Google Scholar] [CrossRef]
- Kourilovitch, M.; Galarza–Maldonado, C. Could a simple biomarker as neutrophil-to-lymphocyte ratio reflect complex processes orchestrated by neutrophils? J. Transl. Autoimmun. 2022, 6, 100159. [Google Scholar] [CrossRef]
- Bhikram, T.; Sandor, P. Neutrophil-lymphocyte ratios as inflammatory biomarkers in psychiatric patients. BrainBehav. Immun. 2022, 105, 237–246. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, L.; Lei, R.; Li, P.; Li, S. Effects and Interaction of Meteorological Parameters on Influenza Incidence During 2010-2019 in Lanzhou, China. Front. Public Health 2022, 10, 833710. [Google Scholar] [CrossRef]
- Kotecki, P.; Więckowska, B.; Stawińska-Witoszyńska, B. The Impact of Meteorological Parameters and Seasonal Changes on Reporting Patients with Selected Cardiovascular Diseases to Hospital Emergency Departments: A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 4838. [Google Scholar] [CrossRef]
- Chiu, Y.M.; Chebana, F.; Abdous, B.; Bélanger, D.; Gosselin, P. Cardiovascular Health Peaks and Meteorological Conditions: A Quantile Regression Approach. Int. J. Environ. Res. Public Health 2021, 18, 13277. [Google Scholar] [CrossRef]
- Azzouzi, H.; Ichchou, L. Seasonal and Weather Effects on Rheumatoid Arthritis: Myth or Reality? Pain. Res. Manag. 2020, 2020, 5763080. [Google Scholar] [CrossRef]
- Morimoto, H. A probabilistic approach for links between rheumatic diseases and weather. Int. Med. Care 2017, 1, 1–14. [Google Scholar] [CrossRef][Green Version]
- Bongioanni, P.; Del Carratore, R.; Corbianco, S.; Diana, A.; Cavallini, G.; Masciandaro, S.M.; Dini, M.; Buizza, R. Climate change and neurodegenerative diseases. Environ. Res. 2021, 201, 111511. [Google Scholar] [CrossRef]
- Hahad, O.; Lelieveld, J.; Birklein, F.; Lieb, K.; Daiber, A.; Münzel, T. Ambient Air Pollution Increases the Risk of Cerebrovascular and Neuropsychiatric Disorders through Induction of Inflammation and Oxidative Stress. Int. J. Mol. Sci. 2020, 21, 4306. [Google Scholar] [CrossRef]
- Charlson, F.; Ali, S.; Benmarhnia, T.; Pearl, M.; Massazza, A.; Augustinavicius, J.; Scott, J.G. Climate Change and Mental Health: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 4486. [Google Scholar] [CrossRef] [PubMed]
- Clayton, S. Climate Change and Mental Health. Curr. Environ. Health Rep. 2021, 8, 1–6. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, G.; Chong-Neto, H.J.; Monge Ortega, O.P.; Vitale, C.; Ansotegui, I.; Rosario, N.; Haahtela, T.; Galan, C.; Pawankar, R.; Murrieta-Aguttes, M.; et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef] [PubMed]
- Eguiluz-Gracia, I.; Mathioudakis, A.G.; Bartel, S.; Vijverberg, S.J.H.; Fuertes, E.; Comberiati, P.; Cai, Y.S.; Tomazic, P.V.; Diamant, Z.; Vestbo, J.; et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy 2020, 75, 2170–2184. [Google Scholar] [CrossRef] [PubMed]
- Kantor, R.; Silverberg, J.I. Environmental risk factors and their role in the management of atopic dermatitis. Expert. Rev. Clin. Immunol. 2017, 13, 15–26. [Google Scholar] [CrossRef]
- Nguyen, G.H.; Andersen, L.K.; Davis, M.D.P. Climate change and atopic dermatitis: Is there a link? Int. J. Dermatol. 2019, 58, 279–282. [Google Scholar] [CrossRef]
- Khafaie, M.A.; Salvi, S.S.; Ojha, A.; Khafaie, B.; Gore, S.S.; Yajnik, C.S. Systemic inflammation (C-reactive protein) in type 2 diabetic patients is associated with ambient air pollution in Pune City, India. Diabetes Care 2013, 36, 625–630. [Google Scholar] [CrossRef]
- Pilz, V.; Wolf, K.; Breitner, S.; Rückerl, R.; Koenig, W.; Rathmann, W.; Cyrys, J.; Peters, A.; Schneider, A.; KORA-Study Group. C-reactive protein (CRP) and long-term air pollution with a focus on ultrafine particles. Int. J. Hyg. Environ. Health 2018, 221, 510–518. [Google Scholar] [CrossRef]
- Liu, C.C.; Ko, H.J.; Liu, W.S.; Hung, C.L.; Hu, K.C.; Yu, L.Y.; Shih, S.C. Neutrophil-to-lymphocyte ratio as a predictive marker of metabolic syndrome. Medicine 2019, 98, e17537. [Google Scholar] [CrossRef]
- Niu, Y.; Gao, Y.; Yang, J.; Qi, L.; Xue, T.; Guo, M.; Zheng, J.; Lu, F.; Wang, J.; Liu, Q. Short-term effect of apparent temperature on daily emergency visits for mental and behavioral disorders in Beijing, China: A time-series study. Sci. Total Environ. 2020, 733, 139040. [Google Scholar] [CrossRef]
- Lin, B.D.; Hottenga, J.J.; Abdellaoui, A.; Dolan, C.V.; De Geus, E.J.C.; Kluft, C.; Boomsma, D.I.; Willemsen, G. Causes of variation in the neutrophil-lymphocyte and platelet-lymphocyte ratios: A twin-family study. Biomark. Med. 2016, 10, 1061–1072. [Google Scholar] [CrossRef]

| Anova with Full Dataset | Age ≤ 73 | Age > 73 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F value | Pr(>F) | F value | Pr(>F) | F value | Pr(>F) | ||||
| Gender | 0.27 | 0.605 | 7.13 | 0.008 | ** | 29.86 | <0.001 | *** | |
| Age | 259.72 | <0.001 | *** | 15.89 | <0.001 | *** | 34.82 | <0.001 | *** |
| Mean_Temp | 21.77 | <0.001 | *** | 23.17 | <0.001 | *** | 3.53 | 0.061 | . |
| Max_Humidity | 1.12 | 0.291 | 0.00 | 0.983 | 1.34 | 0.248 | |||
| Min_Humidity | 2.21 | 0.137 | 1.52 | 0.218 | 0.94 | 0.333 | |||
| RAIN | 0.43 | 0.513 | 0.40 | 0.526 | 1.48 | 0.225 | |||
| AVG_Wind_Speed | 6.49 | 0.011 | * | 5.12 | 0.024 | * | 1.54 | 0.215 | |
| Max_Wind_Speed | 0.56 | 0.454 | 0.10 | 0.757 | 0.08 | 0.777 | |||
| AT | 1.52 | 0.217 | 0.25 | 0.62 | 1.50 | 0.22 | |||
| AT3daysLag | 0.43 | 0.511 | 0.27 | 0.601 | 1.99 | 0.159 | |||
| AT5daysLag | 3.77 | 0.052 | . | 1.78 | 0.182 | 1.56 | 0.212 | ||
| AT7daysLag | 1.10 | 0.295 | 0.50 | 0.48 | 0.44 | 0.506 | |||
| Max_Humidity_3daysLag | 0.35 | 0.552 | 0.78 | 0.376 | 0.18 | 0.675 | |||
| Max_Humidity_5daysLag | 4.06 | 0.044 | * | 4.83 | 0.028 | * | 0.30 | 0.585 | |
| Max_Humidity_7daysLag | 4.01 | 0.045 | * | 4.55 | 0.033 | * | 0.38 | 0.54 | |
| TempCategory | 0.40 | 0.526 | 0.25 | 0.62 | 1.16 | 0.281 | |||
| RaiseCategory | <0.01 | 0.952 | 0.16 | 0.685 | 0.13 | 0.715 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sergounioti, A.; Rigas, D.; Paplomatas, P.; Vrahatis, A.; Lagouvardos, K. Are Complete Blood Count Parameters Associated with Climate and Environmental Factors? A Retrospective Study in the General Population of Fokis, Greece (Athens, 2023). Environ. Sci. Proc. 2023, 26, 163. https://doi.org/10.3390/environsciproc2023026163
Sergounioti A, Rigas D, Paplomatas P, Vrahatis A, Lagouvardos K. Are Complete Blood Count Parameters Associated with Climate and Environmental Factors? A Retrospective Study in the General Population of Fokis, Greece (Athens, 2023). Environmental Sciences Proceedings. 2023; 26(1):163. https://doi.org/10.3390/environsciproc2023026163
Chicago/Turabian StyleSergounioti, Athanasia, Dimitris Rigas, Petros Paplomatas, Aristidis Vrahatis, and Konstantinos Lagouvardos. 2023. "Are Complete Blood Count Parameters Associated with Climate and Environmental Factors? A Retrospective Study in the General Population of Fokis, Greece (Athens, 2023)" Environmental Sciences Proceedings 26, no. 1: 163. https://doi.org/10.3390/environsciproc2023026163
APA StyleSergounioti, A., Rigas, D., Paplomatas, P., Vrahatis, A., & Lagouvardos, K. (2023). Are Complete Blood Count Parameters Associated with Climate and Environmental Factors? A Retrospective Study in the General Population of Fokis, Greece (Athens, 2023). Environmental Sciences Proceedings, 26(1), 163. https://doi.org/10.3390/environsciproc2023026163







