Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality) †
Abstract
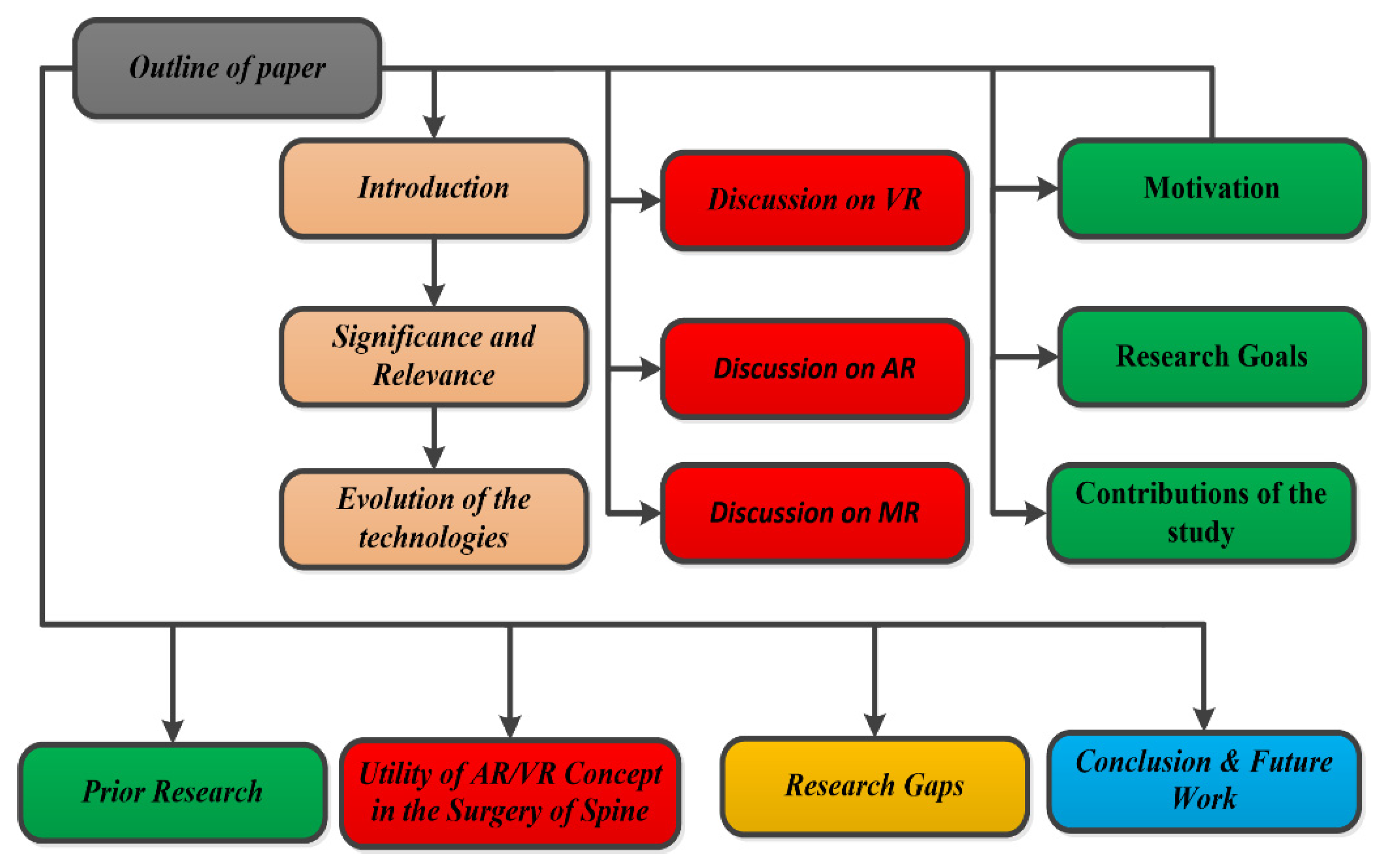
1. Introduction
Novelty
- This study presents various spinal surgery treatments through AR with substantial supportive data.
- AR, VR, and MR devices for spinal treatment are compared and presented with their efficacy.
- A rigorous survey was conducted, showing the growth of XR in healthcare regarding treatment and training.
2. Background Study
2.1. Discussion on Virtual Reality
Preoperative Steps
2.2. Discussion on Augmented Reality
2.2.1. Rod Bending
2.2.2. Quality Control in the Operating Room
2.2.3. Keyhole Spine Surgery
2.2.4. Facet Joint Injections
2.3. Discussion on Mixed Reality
- Motivation
- 2.
- Research Goals
3. Utility of AR/VR Concept in the Surgery of Spine
4. Research Gaps
4.1. Cost-Effectiveness
4.2. Effective Integration
4.3. Evidence of Improved Surgical Outcome
5. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jamison, R.N.; Ross, M.J.; Hoopman, P.; Griffin, F.; Levy, J.; Daly, M.; Schaffer, J.L. Assessment of postoperative pain management: Patient satisfaction and perceived helpfulness. Clin. J. Pain 1997, 13, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Hodgkinson, B.; Evans, D.; O’Neill, S. Knowledge Retention from Preoperative Patient Information; The Joanna Briggs Institute for Evidence-Based Nursing and Midwifery: Adelaide, Australia, 2000. [Google Scholar]
- Gordon, D.B.; Dahl, J.L.; Miaskowski, C.; McCarberg, B.; Todd, K.H.; Paice, J.A.; Lipman, A.G.; Bookbinder, M.; Sanders, S.H.; Turk, D.C.; et al. American Pain Society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch. Intern. Med. 2005, 165, 1574–1580. [Google Scholar] [CrossRef] [PubMed]
- Prouty, A.; Cooper, M.; Thomas, P.; Christensen, J.; Strong, C.; Bowie, L.; Oermann, M.H. Multidisciplinary patient education for total joint replacement surgery patients. Orthop Nurs. 2006, 25, 257–261. [Google Scholar] [CrossRef]
- Spalding, N.J. Reducing anxiety by pre-operative education: Make the future familiar. Occup. Ther. Int. 2003, 10, 278–293. [Google Scholar] [CrossRef] [PubMed]
- Stirling, E.R.; Lewis, T.L.; Ferran, N.A. Ferran Surgical skills simulation in trauma and orthopaedic training. J. Orthop. Surg. Res. 2014, 9, 126. [Google Scholar] [CrossRef]
- Zimmerman, T.G.; Lanier, J.; Blanchard, C.; Bryson, S.; Harvill, Y. A hand gesture interface device. In Proceedings of the SIGCHI/GI Conference on Human Factors in Computing Systems and Graphics Interface, Toronto, ON, Canada, 5–9 April 1987; pp. 189–192. [Google Scholar]
- PKalun, N.; Wagner, J.; Yan, M.T.; Nousiainen, R.R. Sonnadara Surgical simulation training in orthopaedics: Current insights. Adv. Med. Educ. Pract. 2018, 9, 125–131. [Google Scholar]
- Kim, Y.; Kim, H.; Kim, Y.O. Virtual reality and augmented reality in plastic surgery: A review. Arch. Plast. Surg. 2017, 44, 179–187. [Google Scholar] [CrossRef]
- Morgan, M.; Aydin, A.; Salih, A.; Robati, S.; Ahmed, K. Current status of simulation-based training tools in orthopedic surgery: A systematic review. J. Surg. Educ. 2017, 74, 698–716. [Google Scholar] [CrossRef]
- Hernandez, D.; Garimella, R.; Eltorai, A.E.M.; Daniels, A.H. Computer-assisted orthopaedic surgery. Orthop. Surg. 2017, 9, 152–158. [Google Scholar] [CrossRef]
- Wanivenhaus, F.; Neuhaus, C.; Liebmann, F.; Roner, S.; Spirig, J.M.; Farshad, M. Augmented reality-assisted rod bending in spinal surgery. Spine J. 2019, 19, 1687–1689. [Google Scholar] [CrossRef]
- Umebayashi, D.; Yamamoto, Y.; Nakajima, Y.; Fukaya, N.; Hara, M. Augmented Reality Visualization-guided Microscopic Spine Surgery: Transvertebral Anterior Cervical Foraminotomy and Posterior Foraminotomy. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e008. [Google Scholar] [CrossRef]
- Agten, C.A.; Dennler, C.; Rosskopf, A.B.; Jaberg, L.; Pfirrmann, C.W.; Farshad, M. Augmented Reality-Guided Lumbar Facet Joint Injections. Investig. Radiol. 2018, 53, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.S.; Patel, D.S.; Hrynewycz, N.M.; Brundage, T.S.; Singh, K. The utility of virtual reality and augmented reality in spine surgery. Ann. Transl. Med. 2019, 7 (Suppl. S5), S171. [Google Scholar] [CrossRef]
- Shelke, Y.; Chakraborty, C. Augmented Reality and Virtual Reality Transforming Spinal Imaging Landscape: A Feasibility Study. IEEE Comput. Graph. Appl. 2021, 41, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Sakai, D.; Joyce, K.; Sugimoto, M.; Horikita, N.; Hiyama, A.; Sato, M.; Devitt, A.; Watanabe, M. Augmented, virtual and mixed reality in spinal surgery: A real-world experience. J. Orthop. Surg. 2020, 28, 2309499020952698. [Google Scholar] [CrossRef]
- Viglialoro, R.M.; Condino, S.; Turini, G.; Carbone, M.; Ferrari, V.; Gesi, M. Augmented Reality, Mixed Reality, and Hybrid Approach in Healthcare Simulation: A Systematic Review. Appl. Sci. 2021, 11, 2338. [Google Scholar] [CrossRef]
- Khor, W.S.; Baker, B.; Amin, K.; Chan, A.; Patel, K.; Wong, J. Augmented and virtual reality in surgery-the digital surgical environment: Applications, limitations and legal pitfalls. Ann. Transl. Med. 2016, 4, 454. [Google Scholar] [CrossRef]
- Ghaednia, H.; Fourman, M.S.; Lans, A.; Detels, K.; Dijkstra, H.; Lloyd, S.; Sweeney, A.; Oosterhoff, J.H.F.; Schwab, J.H. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021, 21, 1617–1625. [Google Scholar] [CrossRef] [PubMed]
- Abhari, K.; Baxter, J.S.; Chen, E.C.; Khan, A.R.; Peters, T.M.; de Ribaupierre, S.; Eagleson, R. Training for planning tumour resection: Augmented reality and human factors. IEEE Trans. Biomed. Eng. 2015, 62, 1466–1477. [Google Scholar] [CrossRef] [PubMed]
- Moro, C.; Stromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Chytas, D.; Johnson, E.O.; Piagkou, M.; Mazarakis, A.; Babis, G.C.; Chronopoulos, E.; Nikolaou, V.S.; Lazaridis, N.; Natsis, K. The role of augmented reality in anatomical education: An overview. Ann. Anat. Anat. Anz. Off. Organ. Anat. Ges. 2020, 229, 151463. [Google Scholar] [CrossRef] [PubMed]
- Elmi-Terander, A.; Nachabe, R.; Skulason, H.; Pedersen, K.; Söderman, M.; Racadio, J.; Babic, D.; Gerdhem, P.; Edström, E. Feasibility and accuracy of thoracolumbar minimally invasive pedicle screw placement with augmented reality navigation technology. Spine 2018, 43, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Gasco, J.; Patel, A.; Ortega-Barnett, J.; Branch, D.; Desai, S.; Kuo, Y.F.; Luciano, C.; Rizzi, S.; Kania, P.; Matuyauskas, M.; et al. Virtual reality spine surgery simulation: An empirical study of its usefulness. Neurol. Res. 2014, 36, 968–973. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Hou, Y.; Lin, Y.; Chen, H.; Yuan, W. Role of Visuohaptic Surgical Training Simulator in Resident Education of Orthopedic Surgery. World Neurosurg. 2018, 111, e98–e104. [Google Scholar] [CrossRef] [PubMed]
- Costa, F. Economic study: A cost-effectiveness analysis of an intraoperative compared with a preoperative image-guided system in lumbar pediclescrew fixation. Spine J. 2014, 14, 1790–1796. [Google Scholar] [CrossRef] [PubMed]
- Carl, B.; Bopp, M.; Saß, B.; Voellger, B.; Nimsky, C. Implementation of augmented reality support in spine surgery. Eur. Spine J. 2019, 28, 1697–1711. [Google Scholar] [CrossRef]
- Peh, S.; Chatterjea, A.; Pfarr, J.; Schäfer, J.P.; Weuster, M.; Klüter, T.; Seekamp, A.; Lippross, S. Accuracy of augmented reality surgical navigation for minimally invasive pedicle screw insertion in the thoracic and lumbar spine with a new tracking device. Spine J. 2020, 20, 629–637. [Google Scholar] [CrossRef]

| Application Areas | Usage |
|---|---|
| Healthcare | Navigating features during surgery, providing experience (psychological) to patients, risk assessment, and medical education/training simulation. |
| Human Resources | Three-dimensional (3D) video recruiting; potential applicants are vetted by simulating and testing their talents, conducting meetings and webinars in VR mode to minimize the barrier of face-to-face communication, and training employees through VR simulators. |
| Travel Sector | Augmented tourist destinations, immersive 360-degree VR video of the destination, and 3D navigation for tourists. |
| Government | VR simulators to train government officials, seamless communication from remote locations; creating visual models of government projects. |
| Infrastructure | Flooring selection using AR applications, interior design, and 3D designs of buildings. |
| Number | Research Questions | Objectives |
|---|---|---|
| RQ-1 | How and where can AR/VR be introduced in healthcare? | Healthcare is a very sensitive issue because, here, someone’s life is affected; it is important to precisely decide what sections of treatment we can use AR/VR/MR. |
| RQ-2 | How can patients be convinced to use the AR/VR? | Prepare advantages and successful case studies for patients, so that patients do not have any issues while adopting the technology for their treatment. |
| RQ-3 | How can doctors be convinced to use AR/VR in healthcare to treat patients? | Doctors and surgeons are not technology-driven; they also require convincing evidence of success for adopting the concept in treatments. |
| RQ-4 | What are the devices required for patients and doctors to utilize AR/VR? | AR/VR/MR is fully device-driven technology. As uses change, the need for devices also changes. So, to adopt the concept in healthcare, it is important to know the devices that are required, along with their efficiency and error rates. |
| RQ-5 | What will be the impact of the system’s failure? | There should be a backup plan or no effect of technology failure during treatment; otherwise, there will be a barrier to using the technology from both patients’ and doctors’ perspectives. |
| Characteristics | VR | AR | MR |
|---|---|---|---|
| Imaging data of patients, e.g., CT and MRI scans | ✓ | ✓ | ✓ |
| User (surgeon) manipulation of real and computer-augmented images | ✖ | ✓ | ✓ |
| Spinal surgery training without patients (all parts of the spine can be computer-generated and arranged completely like in a real patient) | ✓ | ✖ | ✖ |
| Live help from an expert for the surgery (receive an expert’s suggestions during the surgery without their presence) | ✓ | ✓ | ✓ |
| Pedicle screw placement in spinal surgery | ✖ | ✓ | ✖ |
| Cervical spine treatment | ✓ | ✓ | ✖ |
| Surgery of an abnormal curve in the spine (deformity) | ✖ | ✓ | ✖ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garg, D.; Dubey, N.; Goel, P.; Ramoliya, D.; Ganatra, A.; Kotecha, K. Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality). Eng. Proc. 2023, 59, 186. https://doi.org/10.3390/engproc2023059186
Garg D, Dubey N, Goel P, Ramoliya D, Ganatra A, Kotecha K. Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality). Engineering Proceedings. 2023; 59(1):186. https://doi.org/10.3390/engproc2023059186
Chicago/Turabian StyleGarg, Dweepna, Nilesh Dubey, Parth Goel, Dipak Ramoliya, Amit Ganatra, and Ketan Kotecha. 2023. "Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality)" Engineering Proceedings 59, no. 1: 186. https://doi.org/10.3390/engproc2023059186
APA StyleGarg, D., Dubey, N., Goel, P., Ramoliya, D., Ganatra, A., & Kotecha, K. (2023). Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality). Engineering Proceedings, 59(1), 186. https://doi.org/10.3390/engproc2023059186







