Abstract
Successful medical diagnostic imaging tools satisfy three criteria; they produce useful information, they fulfill a diagnostic need and are financially viable. The present need is the development of more diagnostic modalities that display changes in the dynamic anatomy and function, “how things move or work, not just how things look”. Bringing compartmentalized modalities together in a complimentary, real time, combined way could produce images with sensitivity and specificity that a single mode cannot offer alone. Conceivably, a combined magnetic resonance imaging/computerized tomography (MRI/CT) system with an added blend of modalities such as electrocardiographs, nerve conduction studies and electroencephalographs, all on the same platform, all performed simultaneously, with the images combined and analyzed together, could overcome the limitations of individual tests.
1. Introduction
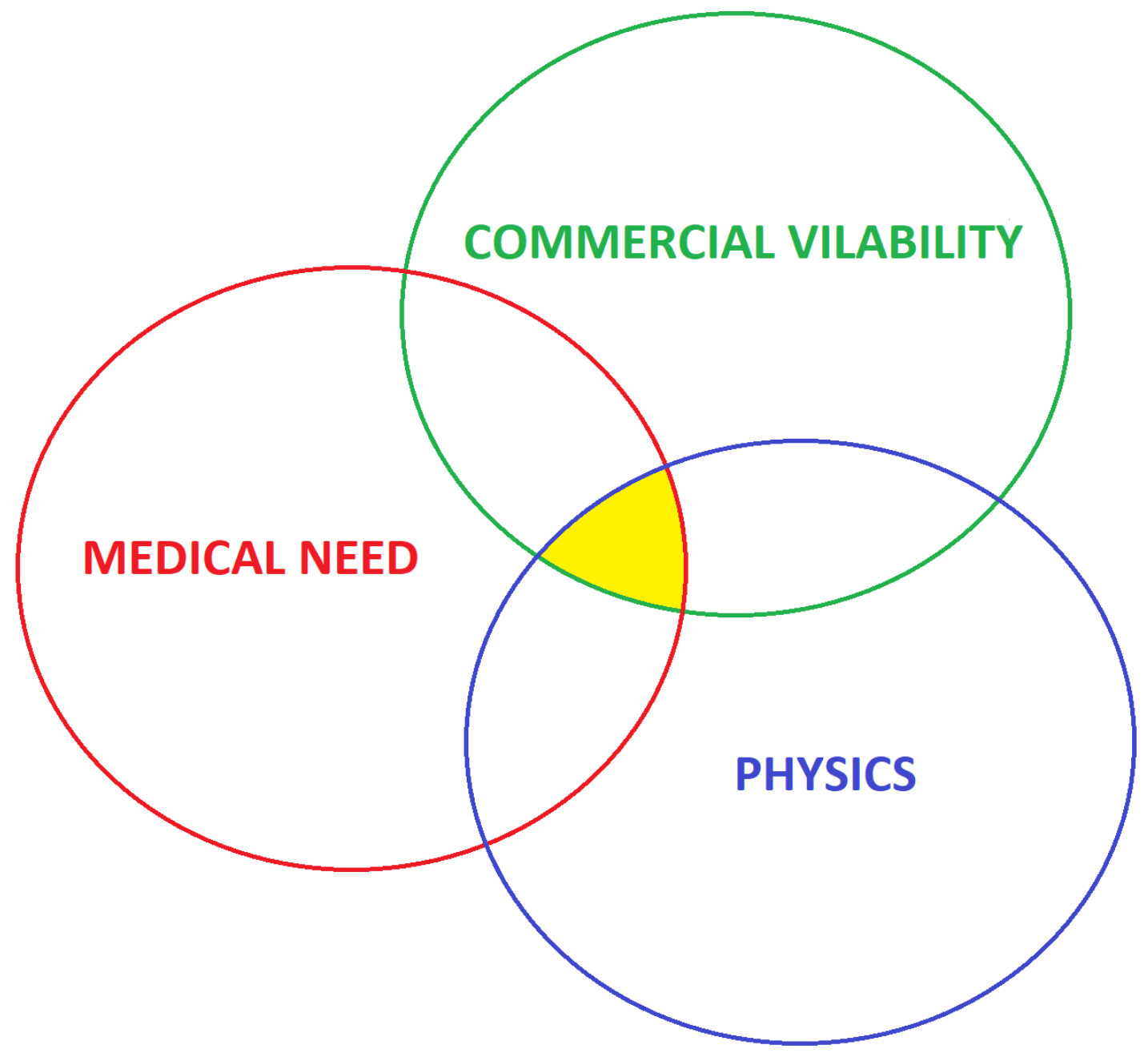
The proper implementation of medical practice needs information. In the diagnostic and management of patients, one starts with the history of the symptoms, followed by the physical examination. When the human senses are not sufficient, special tests come next. Medical diagnostic imaging is there to “see” when the examiner’s senses are not enough. Any diagnostic imaging tool that comes into common use satisfies three criteria; it can be produced, it fulfills a diagnostic need, and it is financially viable. The “sweet spot” is where the physics, medical need and commercial viability intersect (Figure 1).
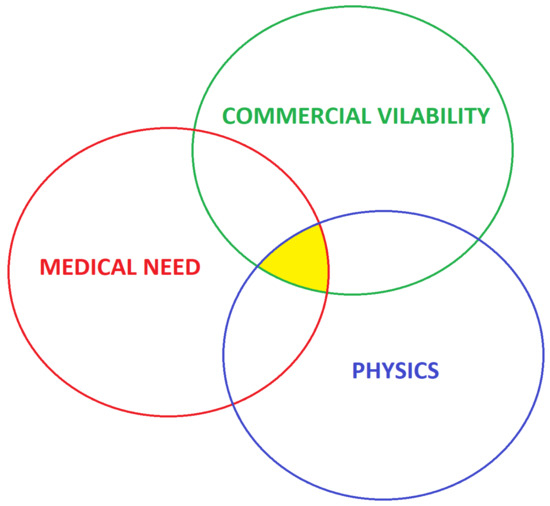
Figure 1.
The intersection between the physics, medical need and commercial viability is the “sweet spot” where the opportunity medical imaging innovation exists.
2. The Physics
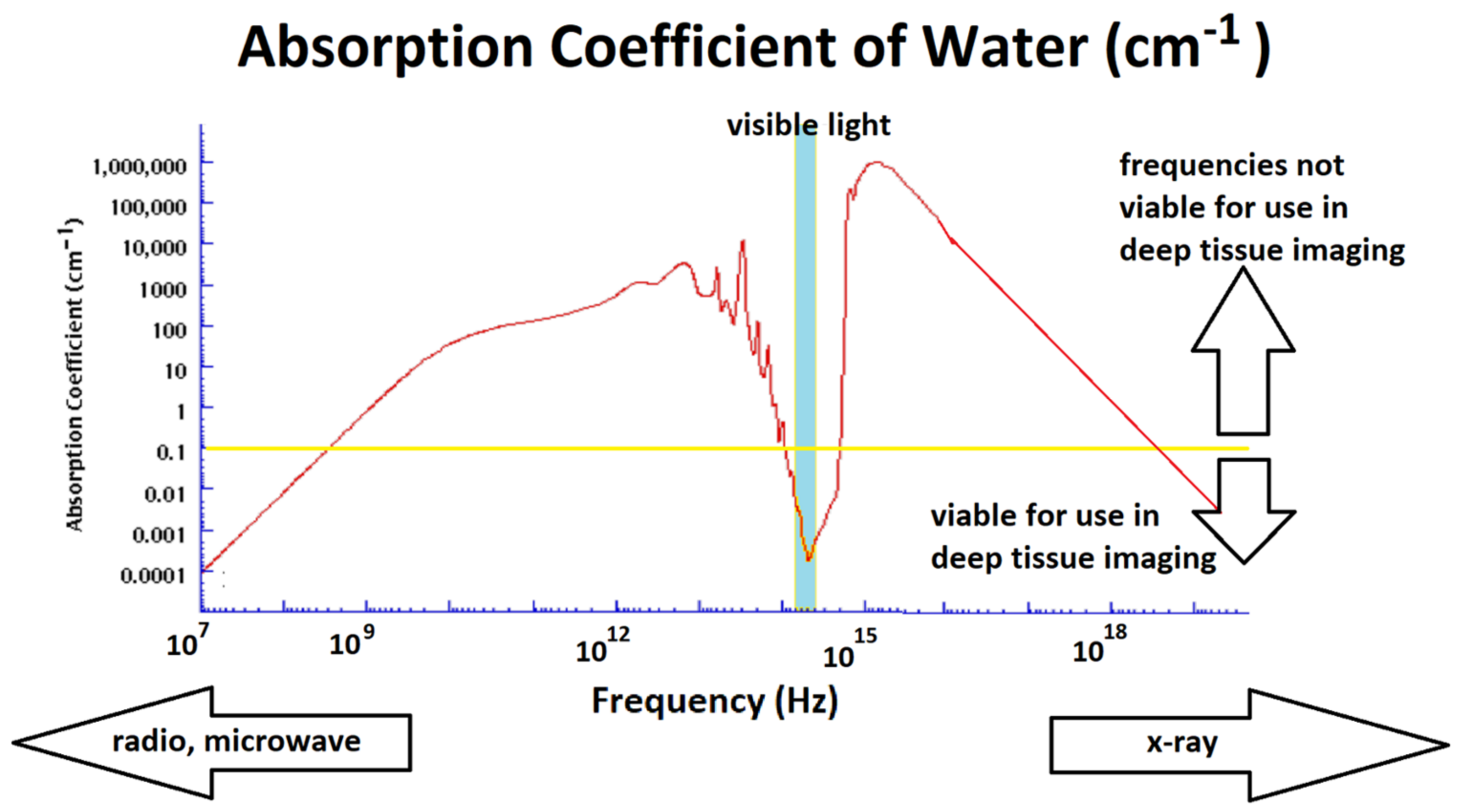
The dead hand of physics limits what is achievable. As Scotty from Star Trek was prone to say, “Ye cannae change the laws of physics”; medical diagnostic imaging tools are bound by what is physically possible. The realms of physics available for diagnostic use can be classified as electromagnetic waves, pressure waves and temperature. Humans are 60% to 65% water; thus, the physics of water becomes a dominant determinant. The absorption coefficient (α) of water, with respect to electromagnetic waves (in terms of cm−1), is presented in Figure 2. The penetration depth (Dp), the depth at which about 37% of the radiation into water survives, is given by Dp = 1/α. An α of 1.0 cm−1 gives a Dp of 1.0 cm, and for an α of 100 cm−1, the Dp is 0.01 cm. For electromagnetic radiation to be useful as a deep tissue diagnostic modality, it needs to traverse the body, which means an α of 0.1 cm−1 or less.
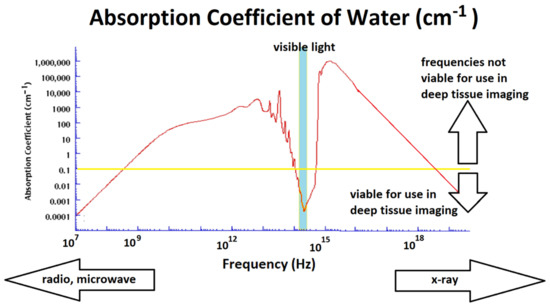
Figure 2.
The absorption coefficient of water at room temperature. Data under 1016 Hz rely on [1]; data above 1016 Hz are extrapolated from [2].
Only radio waves, microwaves, visible light and X-rays have the desired penetration depth to capture the image of deep tissues (α in these regions is under 0.1 cm−1, shown by the yellow line in Figure 2). Other electromagnetic frequencies may be useful for surface diagnostics. Radio waves and microwaves are utilized by electrocardiography, electroencephalography and magnetic resonance imaging (MRI), whist diagnostic X-rays, including computerized tomography (CT), use the X-ray spectrum. There are other constraints; these include the physics of the other chemical components in the body (which effectively rule out the visible spectrum for deep tissue studies), temperature limitations, radiation damage from X-rays, and even the psychological impact such as the panic caused by closed MRI in people who suffer from claustrophobia (%15 of the population). Image resolution, sensitivity (the capacity to resolve change) and specificity (the capacity to assign the change to a particular process) are also important considerations that are limited by physics. A similar analysis can be applied to pressure waves (sound and ultrasound). Sound attenuation is proportional to frequency (for tissue, the relationship ranges from linear to quadratic). Spatial resolution improves with higher frequency. This means there is a constant tradeoff between increasing the frequency to improve spatial resolution and lowering the frequency for better penetration depth in deep tissues. The usefulness of temperature differences is limited by the thermal diffusivity of the tissues.
3. Medical Need
The list of diagnostic imaging modalities that have found a lasting impact grows very slowly. Figure 3 is a photograph of a typical set of desk diagnostic tools in a medical doctor’s office (it is missing a peak flow meter, the weight scales and height measurement device). The newest tool, the pulse oximeter—the small blue item—is based on visible and infrared light. It was invented in 1972 by Takuo Aoyagi. It only found common office use in the past decade. Other items are incremental improvements, such as a better and faster thermometer (to the right of the pulse oximeter) and the electronic blood pressure cuff.

Figure 3.
A typical medical office toolkit. From the left: the electronic sphygmomanometer, stethoscope, tuning fork, otoscope, ophthalmoscope, pulse oximeter, ear thermometer, tendon hammer.
The unmet medical need in an office diagnostic setting is a core hydration meter. Children with a fever and people of all ages who have gastroenteritis would benefit from an estimation of their hydration status. There are a number of unmet diagnostic imaging needs suited to a specialist imaging center setting. Versions of existing modalities that have improved sensitivity and specificity, do not involve the present level of risk and need less expertise or interpretation are on the list. There is also a need for better modalities that display the dynamic anatomy—“how things move or work, not just how things look”. For example, there is a need to improve the contrast and accuracy of the capacity to detect meniscal cartilage lesions. One report puts the accuracy of MRI for knee cartilage lesions between 15% and 60% [3]. There are other gaps. Of the patients with a positive fecal occult blood (FOB) test, 58% will have normal colonoscopy, 39% will be diagnosed with a polyp and 3% will be diagnosed with a suspected cancer [4]. An anesthetic-free preliminary test that has better sensitivity than a FOB would be very welcome. It could reduce colonoscopies by 40% or more. Another example is the limitation put on diagnostic cardiac ultrasounds (echocardiography) due to the need for technicians with four years of training to perform the test. Cheaper, less “expertise intensive” imaging would enable greater access to these existing modalities that fill an existing need.
Some of the most difficult medical challenges revolve around episodic pain or other intermittent symptoms where no anatomical or biochemical anomalies can be found on any test. Diagnostic modalities that display changes in the dynamic anatomy in real time would be useful. Displaying changes in loose joints in the lumbar spine as they move or the motility of the stomach in response to a variety of foods would open new treatment options. Some attempts have been made in this direction, both with X-rays and MRIs. Both are limited by the field of view, and the X-ray modality is limited by the amount or radiation that can be used.
4. Commercial Viability
Any new device that has to be produced can needs to be justified in terms of its utility. An example of the failure of the financial criterion may be a plan for a new USD 1000 THz-based blood glucose monitor. There is definitely a clinical need for a blood glucose monitor, but that need has been filled. A complex finger prick-free continuous glucose monitor with mobile phone apps may cost $100. An example of the success of the commercial criterion is the MRI machine. It is complex, high maintenance and requires highly trained staff. Despite these factors, the medical need that MRI fulfills has made it a financially viable prospect.
5. Discussion, New Approaches and Conclusions
Physics is self-policing, meaning one cannot break its laws, but there are times when there are workarounds. Water absorbs GHz and THz frequency radiation too well to be useful in any non-surface imaging, but frozen water, ice, is 100 times more transparent at these frequencies. Freezing surface features or excised samples open the possibility of using GHz and THz frequency radiation as a diagnostic tool [5] for melanoma diagnosis or tissue ablation [6].
Ultrasound diagnostic devices are the most operator-dependent modalities. They can take a long time to acquire images and need trained people for both image acquisition and interpretation. Reducing the human factor via automation, the use of artificial intelligence and machine learning, would improve access and reduce cost.
Medical diagnostics is currently segregated. One uses either an MRI, a CT or an ultrasound. Often, a diagnostic report from one modality suggests further tests in another. It is time to bring the modalities together in a complimentary, combined way, with images fused to show sensitivity and specificity that neither mode can offer alone, in a faster time frame. Perhaps a combined MRI/CT system on the same platform, with the images combined and analyzed together, can be a solution. The idea is not novel [7], but as the unit cost of MRI machines fall, it may be the time for it to become a reality. Passive tests such as electrocardiographs and electroencephalographs could also be considered for inclusion in these combined modalities.
The best prospects for commercial success may be techniques that replace a procedural intervention with an imaging modality. The challenge with those is not to lose sensitivity or specificity.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Segelstein, D.J. The Complex Refractive Index of Water. Ph.D. Thesis, University of Missouri, Kansas City, MI, USA, 1981. [Google Scholar]
- Hill, R.; Holloway, L.; Baldock, C. A dosimetric evaluation of water equivalent phantoms for kilovoltage x-ray beams. Phys. Med. Biol. 2005, 50, N331. [Google Scholar] [CrossRef] [PubMed]
- Koch, J.; Ben-Elyahu, E.J.R.; Khateeb, B.; Ringart, M.; Nyska, M.; Ohana, N.; Mann, G.; Hetsroni, I. Accuracy measures of 1.5-tesla MRI for the diagnosis of ACL, meniscus and articular knee cartilage damage and characteristics of false negative lesions: A level III prognostic study. BMC Musculoskelet. Disord. 2021, 22, 124. [Google Scholar] [CrossRef] [PubMed]
- Parkin, C.J.; Bell, S.W.; Mirbagheri, N. Colorectal cancer screening in Australia. Aust. J. Gen. Pract. 2018, 47, 859–863. [Google Scholar] [PubMed]
- Vilagosh, Z.; Lajevardipour, A.; Wood, A.W. Computational phantom study of frozen melanoma imaging at 0.45 terahertz. Bioelectromagnetics 2019, 40, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Vilagosh, Z.; Lajevardipour, A.; Wood, A.W. Imaging and lesion ablation modeling in skin using freezing to enhance penetration depth of terahertz radiation. In Proceedings of the Photonics in Dermatology and Plastic Surgery, San Francisco, CA, USA, 2–3 February 2019; Volume 10851, pp. 29–37. [Google Scholar]
- Wang, G.; Feng Liu, F.; Liu, F.; Cao, G.; Gao, H.; Vannier, M.F. Design proposed for a combined MRI/computed-tomography scanner. SPIE Newsroom, 11 June 2013. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).