Promoting Autonomy in Care: Combining Sensor Technology and Social Robotics for Health Monitoring †
Abstract
:1. Introduction and Related Work
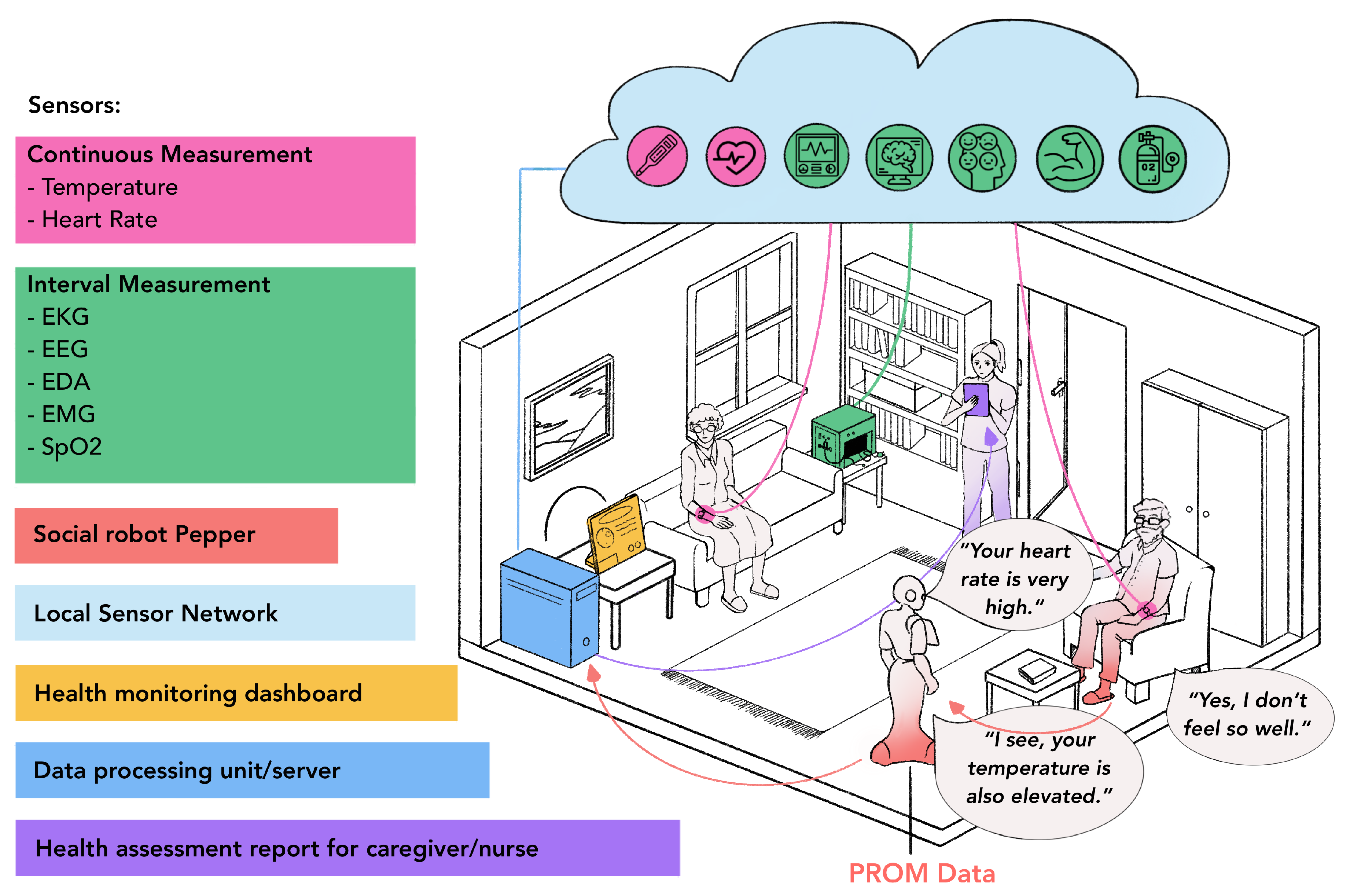
2. Sensor-Robot Ecosystem
2.1. Hardware Components
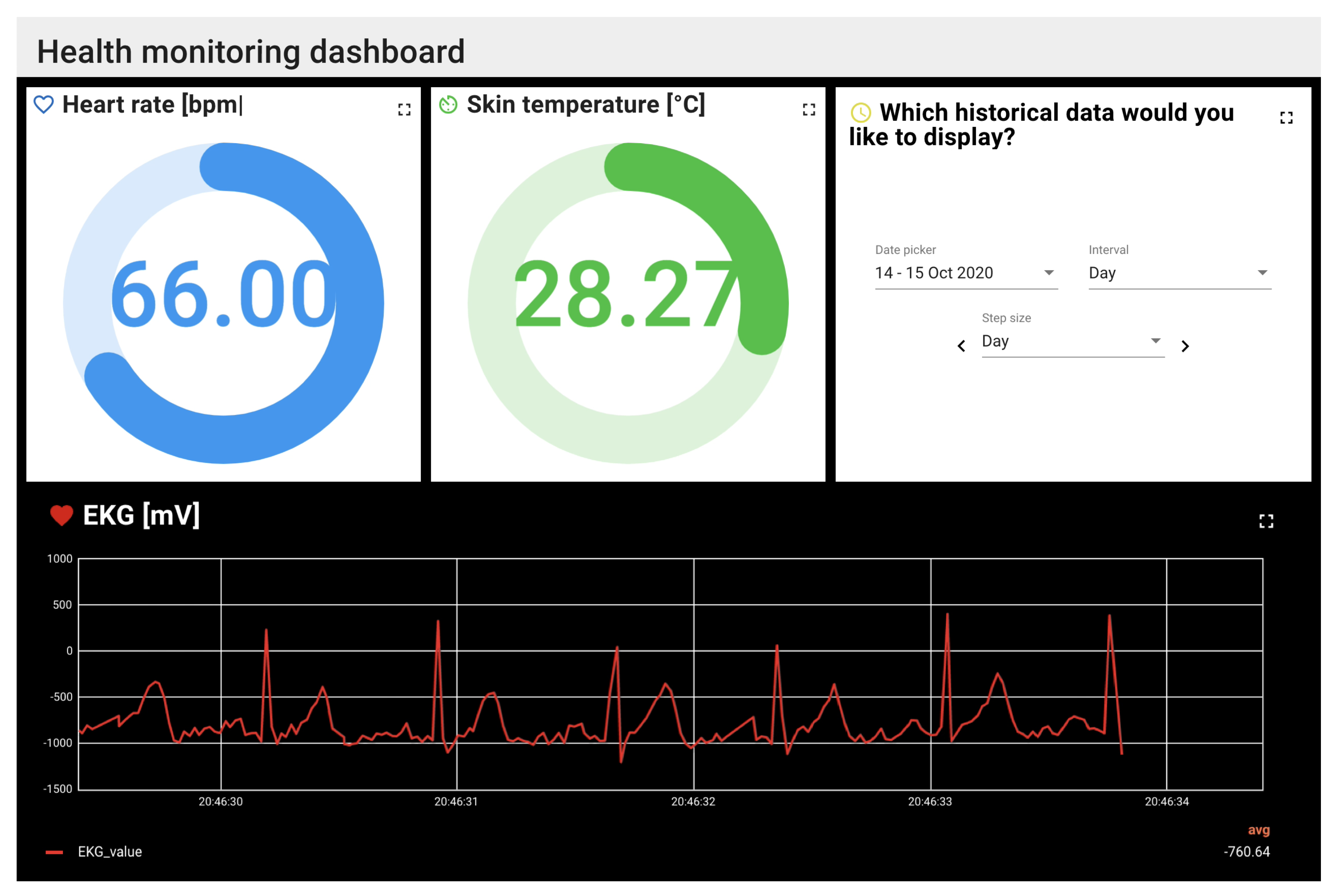
2.2. Software Components
3. Results and Discussion
- Which are the most important PROMs and sensors to detect specific health and care situations? How large are the differences between individual users?
- (How) can we combine PROMs and different sensors to increase the quality of care of elderly users in their homes?
- In which way, if at all, does this combination reduce the burden of care of both the elderly users and their caregivers (both trained and untrained)?
- To which degree can these results be transferred to other age groups and care situations (e.g., nursing homes)?
4. Conclusions and Future Work
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bundesministerium für Gesundheit (Federal Ministry of Health). Zahlen und Fakten zur Pflegeversicherung; Technical Report; Federal Ministry of Health (Germany): Bonn, Germany, 2020. [Google Scholar]
- Flake, R.; Kochskämper, S.; Risius, P.; Seyda, S. Fachkräfteengpass in der Altenpflege; Technical Report; German Economic Institute (IW): Cologne, Germany, 2018. [Google Scholar]
- Statistisches Bundesamt (Destatis). Mehr Pflegebedürftige; Technical Report; Federal Statistical Office (Germany): Wiesbaden, Germany, 2018. [Google Scholar]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Saner, H. Wearable Sensors for Assisted Living in Elderly People. Front. ICT 2018, 5, 1. [Google Scholar] [CrossRef]
- Donati, M.; Celli, A.; Ruiu, A.; Saponara, S.; Fanucci, L. A Telemedicine Service System Exploiting BT/BLE Wireless Sensors for Remote Management of Chronic Patients. Technologies 2019, 7, 13. [Google Scholar] [CrossRef]
- Serhani, M.A.; El Kassabi, H.T.; Ismail, H.; Nujum Navaz, A. ECG Monitoring Systems: Review, Architecture, Processes, and Key Challenges. Sensors 2020, 20, 1796. [Google Scholar] [CrossRef] [PubMed]
- Marques, G.; Pitarma, R.; Garcia, N.M.; Pombo, N. Internet of Things Architectures, Technologies, Applications, Challenges, and Future Directions for Enhanced Living Environments and Healthcare Systems: A Review. Electronics 2019, 8, 1081. [Google Scholar] [CrossRef]
- Coşar, S.; Fernandez-Carmona, M.; Agrigoroaie, R.; Pages, J.; Ferland, F.; Zhao, F.; Yue, S.; Bellotto, N.; Tapus, A. ENRICHME: Perception and Interaction of an Assistive Robot for the Elderly at Home. Int. J. Soc. Robot. 2020, 12, 779–805. [Google Scholar] [CrossRef]
- Loza-Matovelle, D.; Verdugo, A.; Zalama, E.; Gómez-García-Bermejo, J. An Architecture for the Integration of Robots and Sensors for the Care of the Elderly in an Ambient Assisted Living Environment. Robotics 2019, 8, 76. [Google Scholar] [CrossRef]
- Do, H.M.; Pham, M.; Sheng, W.; Yang, D.; Liu, M. RiSH: A Robot-Integrated Smart Home for Elderly Care. Robot. Auton. Syst. 2018, 101, 74–92. [Google Scholar] [CrossRef]
- Casaccia, S.; Revel, G.M.; Scalise, L.; Bevilacqua, R.; Rossi, L.; Paauwe, R.A.; Karkowsky, I.; Ercoli, I.; Artur Serrano, J.; Suijkerbuijk, S.; et al. Social Robot and Sensor Network in Support of Activity of Daily Living for People with Dementia. In Dementia Lab 2019. Making Design Work: Engaging with Dementia in Context; Brankaert, R., IJsselsteijn, W., Eds.; Communications in Computer and Information Science; Springer International Publishing: Cham, Switzerland, 2019; pp. 128–135. [Google Scholar] [CrossRef]
- Collins, S.; Ŝabanović, S.; Fraune, M.; Randall, N.; Eldridge, L.; Piatt, J.A.; Bennett, C.C.; Nagata, S. Sensing Companions: Potential Clinical Uses of Robot Sensor Data for Home Care of Older Adults with Depression. In Companion of the 2018 ACM/IEEE International Conference on Human-Robot Interaction (HRI ’18); Association for Computing Machinery: Chicago, IL, USA, 2018; pp. 89–90. [Google Scholar] [CrossRef]
- Boumans, R.; van Meulen, F.; Hindriks, K.; Neerincx, M.; Olde Rikkert, M. A Feasibility Study of a Social Robot Collecting Patient Reported Outcome Measurements from Older Adults. Int. J. Soc. Robot. 2020, 12, 259–266. [Google Scholar] [CrossRef]
- Yusif, S.; Soar, J.; Hafeez-Baig, A. Older People, Assistive Technologies, and the Barriers to Adoption: A Systematic Review. Int. J. Med. Inform. 2016, 94, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Richert, A.; Schiffmann, M.; Yuan, C. A Nursing Robot for Social Interactions and Health Assessment. In Advances in Human Factors in Robots and Unmanned Systems; Chen, J., Ed.; Advances in Intelligent Systems and Computing; Springer International Publishing: Cham, Switzerland, 2020; pp. 83–91. [Google Scholar] [CrossRef]
- Ding, X.; Zhang, Y.T. Pulse Transit Time Technique for Cuffless Unobtrusive Blood Pressure Measurement: From Theory to Algorithm. Biomed. Eng. Lett. 2019, 9, 37–52. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neef, C.; Richert, A. Promoting Autonomy in Care: Combining Sensor Technology and Social Robotics for Health Monitoring. Eng. Proc. 2020, 2, 42. https://doi.org/10.3390/ecsa-7-08239
Neef C, Richert A. Promoting Autonomy in Care: Combining Sensor Technology and Social Robotics for Health Monitoring. Engineering Proceedings. 2020; 2(1):42. https://doi.org/10.3390/ecsa-7-08239
Chicago/Turabian StyleNeef, Caterina, and Anja Richert. 2020. "Promoting Autonomy in Care: Combining Sensor Technology and Social Robotics for Health Monitoring" Engineering Proceedings 2, no. 1: 42. https://doi.org/10.3390/ecsa-7-08239
APA StyleNeef, C., & Richert, A. (2020). Promoting Autonomy in Care: Combining Sensor Technology and Social Robotics for Health Monitoring. Engineering Proceedings, 2(1), 42. https://doi.org/10.3390/ecsa-7-08239





