Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Variables and Data Collection
2.3. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- INE. Principales Enfermedades Crónicas o de Larga Evolución. 2020. Available online: https://www.ine.es/jaxi/Datos.htm?path=/t00/mujeres_hombres/tablas_1/&file=d03005.px#_tabs-grafico (accessed on 8 March 2025).
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Gaglia, J.L.; Hilliard, M.E.; Isaacs, D.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2022, 46 (Suppl. S1), S19–S40. [Google Scholar] [CrossRef]
- Informe Mundial Sobre la Diabetes. Available online: https://iris.who.int/bitstream/handle/10665/254649/9789243565255-spa.pdf?sequence=1&isAllowed=y (accessed on 14 January 2025).
- World Health Organitation. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003; Available online: https://apps.who.int/iris/bitstream/handle/10665/42682/9?sequence=1 (accessed on 1 May 2024).
- Kim, Y.Y.; Lee, J.S.; Kang, H.J.; Park, S.M. Effect of medication adherence on long-term all-cause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients. Sci. Rep. 2018, 8, 12190. [Google Scholar] [CrossRef] [PubMed]
- Domínguez Gallardo, L.A.; Ortega Filártiga, E.; Domínguez Gallardo, L.A.; Ortega Filártiga, E. Factores asociados a la falta de adherencia al tratamiento en pacientes con diabetes mellitus tipo 2. Rev. Virtual Soc. Paraguaya Med. Interna. 2019, 6, 63–74. [Google Scholar] [CrossRef]
- Saldaña, A.C.C. Diabetes mellitus y sus comorbilidades: Un enfoque integral para la atención del paciente. Rev. Interdiscip. Educ. Salud Act. Física Deporte 2024, 1, 231–240. [Google Scholar]
- Sosa, A.T.A.; Paucar, P.A.Z.; Vivas, N.M.S.; Troya, B.B.B.; Alaleo, A.E.J.; Rivera, S.Y.A. Comorbilidad, Adherencia y Calidad de Vida en Personas con Diabetes Tipo 2: Estudio Comparativo en Población Urbana y Rural. Estud. Perspect. Rev. Científica Académica 2025, 5, 1262–1283. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Świątoniowska-Lonc, N.; Karniej, P.; Polański, J.; Tański, W.; Grochans, E. Influential factors in adherence to the therapeutic regime in patients with type 2 diabetes and hypertension. Diabetes Res. Clin. Pract. 2021, 173, 108693. [Google Scholar] [CrossRef]
- Sendekie, A.K.; Netere, A.K.; Kasahun, A.E.; Belachew, E.A. Medication adherence and its impact on glycemic control in type 2 diabetes mellitus patients with comorbidity: A multicenter cross-sectional study in Northwest Ethiopia. PLoS ONE 2022, 17, e0274971. [Google Scholar] [CrossRef]
- Zulman, D.M.; Chee, C.P.; Wagner, T.H.; Yoon, J.; Cohen, D.M.; Holmes, T.H.; Ritchie, C.; Asch, S.M. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open 2015, 5, e007771. [Google Scholar] [CrossRef]
- Soley-Bori, M.; Ashworth, M.; Bisquera, A.; Dodhia, H.; Lynch, R.; Wang, Y.; Fox-Rushby, J. Impact of multimorbidity on healthcare costs and utilisation: A systematic review of the UK literature. Br. J. Gen. Pract. 2021, 71, e39–e46. [Google Scholar] [CrossRef]
- García Soidán, F.J.; Villoro, R.; Merino, M.; Hidalgo Vega, Á.; Hernando Martín, T.; González Martín Moro, B. Estado de salud, calidad de vida y utilización de recursos sanitarios de los pacientes con diabetes mellitus en España. Semer. Rev. Esp. Med. Fam. 2017, 43, 416–424. [Google Scholar] [CrossRef]
- Martinez-Perez, P.; Orozco-Beltrán, D.; Pomares-Gomez, F.; Hernández-Rizo, J.L.; Borras-Gallen, A.; Gil-Guillen, V.F.; Quesada, J.A.; Lopez-Pineda, A.; Carratala-Munuera, C. Validation and psychometric properties of the 8-item Morisky Medication Adherence Scale (MMAS-8) in type 2 diabetes patients in Spain. Aten Primaria 2021, 53, 101942. [Google Scholar] [CrossRef]
- Elhenawy, Y.I.; Abdelmageed, R.I.; Zaafar, D.K.; Abdelaziz, A.W. Adherence to Insulin Therapy Among Children with Type 1 Diabetes: Reliability and Validity of the Arabic Version of the 4-Item Morisky Medication Adherence Scale. Patient Prefer. Adherence 2022, 16, 1415–1421. [Google Scholar] [CrossRef]
- Pagès-Puigdemont, N.; Valverde-Merino, M.I. Métodos para medir la adherencia terapeútica. ARS Pharm. 2018, 59, 163–172. [Google Scholar] [CrossRef]
- Reyes-García, R.; Moreno-Pérez, Ó.; Bellido, V.; Botana-López, M.; Rodríguez-Hervada, A.D.; Fernández-García, D.; Fernández-García, J.C.; Gargallo-Fernández, M.; González-Clemente, J.M.; Jódar-Gimeno, E.; et al. Título: Abordaje Integral de las Personas con Diabetes tipo 2. Área Conoc. Diabetes Soc. Española Endocrinol. Nutr. 2023, 70, 95–102. [Google Scholar]
- Represas Carrera, F.J.; Carrera García, Á.; Clavería Fontán, A. Perfil clínico de los pacientes diagnosticados de Diabetes Mellitus tipo 2 en el Área Sanitaria de Vigo. Rev. Esp. Salud. Pública 2020, 92, e201803008. [Google Scholar]
- Fortin, F.; Vorilhon, P.; Laporte, C.; Boirie, Y.; Ruivard, M.; Riquelme, M.; Pereira, B.; Tanguy, G. Profile of patients with type 2 diabetes and glycated haemoglobin ≥ 10% followed in general practice. Fam. Pract. 2022, 39, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Elissen, A.M.J.; Hertroijs, D.F.L.; Schaper, N.C.; Bosma, H.; Dagnelie, P.C.; Henry, R.M.; van der Kallen, C.J.; Koster, A.; Schram, M.T.; Stehouwer, C.D.A.; et al. Differences in biopsychosocial profiles of diabetes patients by level of glycaemic control and health-related quality of life: The Maastricht Study. PLoS ONE 2017, 12, e0182053. [Google Scholar] [CrossRef] [PubMed]
- Nair, D.R.; Satheesh, K.; Raghavan, A.; Nanditha, A.; Vinitha, R.; Susairaj, P.; Snehalatha, C.; Ramachandran, A. Trend in the clinical profile of type 2 diabetes in India—Study from a diabetes care centre in South India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1851–1857. [Google Scholar] [CrossRef] [PubMed]
- Torres, E.; Arévalo, H.; Suarez, I.; Vega, N. Perfil clínico de pacientes atendidos con diabetes mellitus tipo 2 en un programa de reversión. Rev. Fac. Med. Humana 2021, 21, 145–150. [Google Scholar]
- Albuja Chaves, M.; Vera Alcívar, D.; Albuja Chaves, M.; Vera Alcívar, D. Perfil clínico de pacientes antes y después de un programa de reversión de diabetes en Ecuador. Rev. Fac. Med. Humana 2022, 22, 147–153. [Google Scholar]
- American Diabetes Association Professional Practice Committee. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2025. Diabetes Care 2025, 48 (Suppl. S1), S14–S26. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 3. Prevention or Delay of Diabetes and Associated Comorbidities: Standards of Care in Diabetes—2025. Diabetes Care 2024, 48 (Suppl. S1), S50–S58. [Google Scholar] [CrossRef]
- Dinca-Panaitescu, S.; Dinca-Panaitescu, M.; Bryant, T.; Daiski, I.; Pilkington, B.; Raphael, D. Diabetes prevalence and income: Results of the Canadian Community Health Survey. Health Policy 2011, 99, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Duan, M.-J.F.; Zhu, Y.; Dekker, L.H.; Mierau, J.O.; Corpeleijn, E.; Bakker, S.J.; Navis, G. Effects of Education and Income on Incident Type 2 Diabetes and Cardiovascular Diseases: A Dutch Prospective Study. J. Gen. Intern. Med. 2022, 37, 3907–3916. [Google Scholar] [CrossRef]
- Buichia Sombra, F.G.; Miranda Cota, G.A. Determinantes sociales de la salud y riesgo de Diabetes Tipo 2 en adultos de poblaciones originarias, aproximaciones desde la Teoría Social. J. Acad. 2021, 4, 227–251. [Google Scholar] [CrossRef]
- Hanson, R.L.; Van Hout, C.V.; Hsueh, W.-C.; Shuldiner, A.R.; Kobes, S.; Sinha, M.; Baier, L.J.; Knowler, W.C.; Center, R.G. Assessment of the potential role of natural selection in type 2 diabetes and related traits across human continental ancestry groups: Comparison of phenotypic with genotypic divergence. Diabetologia 2020, 63, 2616–2627. [Google Scholar] [CrossRef]
- Chuck, R.S.; Dunn, S.P.; Flaxel, C.J.; Gedde, S.J.; Mah, F.S.; Miller, K.M.; Wallace, D.K.; Musch, D.C. Comprehensive Adult Medical Eye Evaluation Preferred Practice Pattern®. Ophthalmology 2021, 128, P1–P29. [Google Scholar] [CrossRef]
- Flaxel, C.J.; Adelman, R.A.; Bailey, S.T.; Fawzi, A.; Lim, J.I.; Vemulakonda, G.A.; Ying, G.S. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology 2020, 127, P66–P145. [Google Scholar] [CrossRef]
- Caro-Bautista, J.; Morilla-Herrera, J.C.; Villa-Estrada, F.; Cuevas-Fernández-Gallego, M.; Lupiáñez-Pérez, I.; Morales-Asencio, J.M. Adaptación cultural al español y validación psicométrica del Summary of Diabetes Self-Care Activities measure (SDSCA) en personas con diabetes mellitus tipo 2. Aten Primaria 2015, 48, 458–467. [Google Scholar] [CrossRef]
- Afaya, R.A.; Bam, V.; Azongo, T.B.; Afaya, A.; Kusi-Amponsah, A.; Ajusiyine, J.M.; Hamid, T.A.; Laws, M.B. Medication adherence and self-care behaviours among patients with type 2 diabetes mellitus in Ghana. PLoS ONE 2020, 15, e0237710. [Google Scholar] [CrossRef] [PubMed]
- Strandberg, R.B.; Nilsen, R.M.; Pouwer, F.; Igland, J.; Forster, R.B.; Jenum, A.K.; Buhl, E.S.; Iversen, M.M. Lower education and immigrant background are associated with lower participation in a diabetes education program—Insights from adult patients in the Outcomes & Multi-morbidity In Type 2 diabetes cohort (OMIT). Patient Educ. Couns. 2023, 107, 107577. [Google Scholar] [PubMed]
- Chasens, E.R.; Dinardo, M.; Imes, C.C.; Morris, J.L.; Braxter, B.; Yang, K. Citizenship and health insurance status predict glycemic management: NHANES data 2007–2016. Prev. Med. 2020, 139, 106180. [Google Scholar] [CrossRef] [PubMed]
- Hunt, K.J.; Davis, M.; Pearce, J.; Bian, J.; Guagliardo, M.F.; Moy, E.; Axon, R.N.; Neelon, B. Geographic and Racial/Ethnic Variation in Glycemic Control and Treatment in a National Sample of Veterans with Diabetes. Diabetes Care 2020, 43, 2460–2468. [Google Scholar] [CrossRef]
- Nagrebetsky, A.; Griffin, S.; Kinmonth, A.L.; Sutton, S.; Craven, A.; Farmer, A. Predictors of suboptimal glycaemic control in type 2 diabetes patients: The role of medication adherence and body mass index in the relationship between glycaemia and age. Diabetes Res. Clin. Pract. 2012, 96, 119–128. [Google Scholar] [CrossRef]
- Cai, X.; Yang, W.; Gao, X.; Zhou, L.; Han, X.; Ji, L. Baseline Body Mass Index and the Efficacy of Hypoglycemic Treatment in Type 2 Diabetes: A Meta-Analysis. PLoS ONE 2016, 11, e0166625. [Google Scholar] [CrossRef]
| Variable | n | % | |||
|---|---|---|---|---|---|
| Sex | Male | 186 | 50.3 | ||
| Female | 184 | 49.7 | |||
| Age | 18–29 | Male | 5 | 1.35 | |
| Female | 3 | 0.85 | |||
| 30–39 | Male | 6 | 1.62 | ||
| Female | 8 | 2.16 | |||
| 40–49 | Male | 21 | 5.67 | ||
| Female | 14 | 3.78 | |||
| 50–59 | Male | 34 | 9.18 | ||
| Female | 39 | 10.54 | |||
| 60–69 | Male | 67 | 18.1 | ||
| Female | 58 | 15.67 | |||
| 70–79 | Male | 42 | 11.35 | ||
| Female | 33 | 8.91 | |||
| Over 80 | Male | 11 | 2.97 | ||
| Female | 29 | 7.83 | |||
| Marital status | Single | Male | 25 | 6.75 | |
| Female | 11 | 2.97 | |||
| Married | Male | 145 | 39.18 | ||
| Female | 108 | 29.18 | |||
| Widowed | Male | 10 | 2.7 | ||
| Female | 53 | 14.32 | |||
| Divorced | Male | 6 | 1.62 | ||
| Female | 12 | 3.24 | |||
| BMI | Normal weight | Male | 46 | 12.43 | |
| Female | 22 | 5.94 | |||
| Overweight | Male | 89 | 24.05 | ||
| Female | 81 | 21.89 | |||
| Obesity | Male | 51 | 13.78 | ||
| Female | 81 | 21.89 | |||
| Monthly income | 0–500 | Male | 26 | 7.02 | |
| Female | 62 | 16.75 | |||
| 501–1000 | Male | 42 | 11.35 | ||
| Female | 49 | 13.24 | |||
| 1001–1500 | Male | 43 | 11.62 | ||
| Female | 39 | 10.54 | |||
| 1501–2000 | Male | 33 | 8.91 | ||
| Female | 18 | 4.86 | |||
| Over 2000 | Male | 42 | 11.35 | ||
| Female | 16 | 4.32 | |||
| Cultural background | European | Male | 94 | 25.4 | |
| Female | 88 | 23.78 | |||
| Maghrebian | Male | 92 | 24.86 | ||
| Female | 96 | 25.94 | |||
| Family support | No | Male | 55 | 14.86 | |
| Female | 58 | 15.86 | |||
| Yes | Partner | Male | 105 | 28.37 | |
| Female | 73 | 19.73 | |||
| Children | Male | 12 | 3.24 | ||
| Female | 46 | 12.43 | |||
| Parents | Male | 8 | 2.16 | ||
| Female | 3 | 0.81 | |||
| Close relatives | Male | 6 | 1.62 | ||
| Female | 4 | 1.08 | |||
| Education level | No education | Male | 37 | 10 | |
| Female | 77 | 20.81 | |||
| Primary education | Male | 62 | 16.75 | ||
| Female | 50 | 13.51 | |||
| Secondary education | Male | 23 | 6.21 | ||
| Female | 26 | 7.02 | |||
| High School | Male | 39 | 10.54 | ||
| Female | 18 | 4.86 | |||
| University | Male | 25 | 6.75 | ||
| Female | 13 | 3.51 | |||
| Variable | n | % | ||
|---|---|---|---|---|
| MMSA-8 Score | Low adherence | Male | 38 | 10.27 |
| Female | 55 | 14.86 | ||
| Medium adherence | Male | 73 | 19.73 | |
| Female | 68 | 18.38 | ||
| High adherence | Male | 75 | 20.27 | |
| Female | 61 | 16.48 | ||
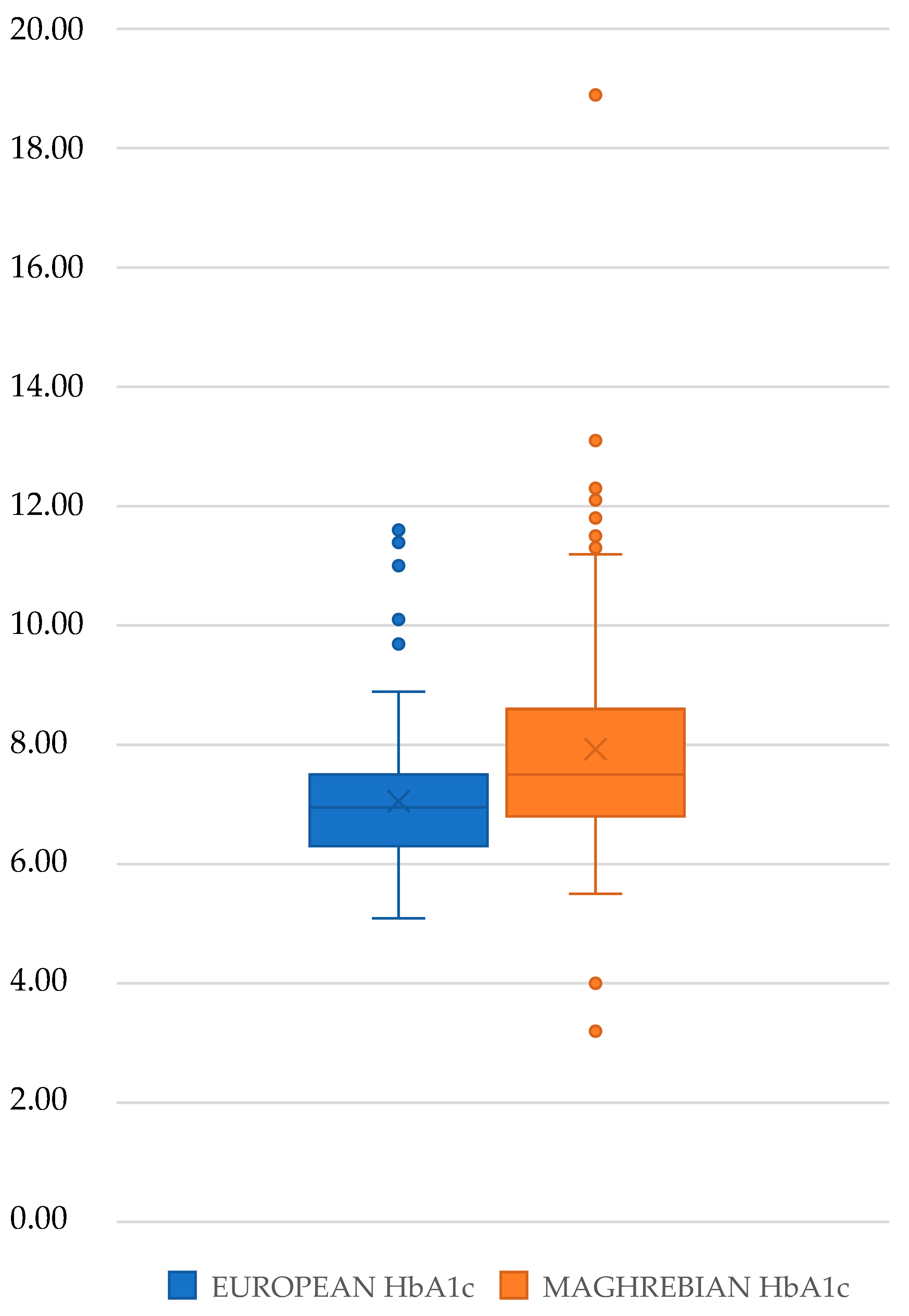
| HbA1c (mean) | 7.5 (SD 1.55) | Male | 7.46 (D.E. 1.57) | |
| Female | 7.54 (D.E. 1.53) | |||
| Years of evolution (median) | 12.02 (SD 6.94) | Male | 11.47 (D.E. 6.94) | |
| Female | 12.59 (D.E. 6.91) | |||
| Treatment | No pharmacological treatment | Male | 2 | 0.54 |
| Female | 11 | 2.97 | ||
| Oral anti-diabetic (OAD) | Male | 105 | 28.38 | |
| Female | 92 | 24.86 | ||
| Insulin | Male | 26 | 7.02 | |
| Female | 17 | 4.59 | ||
| OAD + insulin | Male | 53 | 14.32 | |
| Female | 64 | 17.3 | ||
| N | % | ||||
|---|---|---|---|---|---|
| Smoking | No | Male | 147 | 39.73 | |
| Female | 172 | 46.49 | |||
| Yes | Less than 5 | Male | 7 | 1.98 | |
| Female | 5 | 1.35 | |||
| Between 6 and 15 | Male | 19 | 5.13 | ||
| Female | 3 | 0.81 | |||
| More than 16 | Male | 13 | 3.51 | ||
| Female | 4 | 1.08 | |||
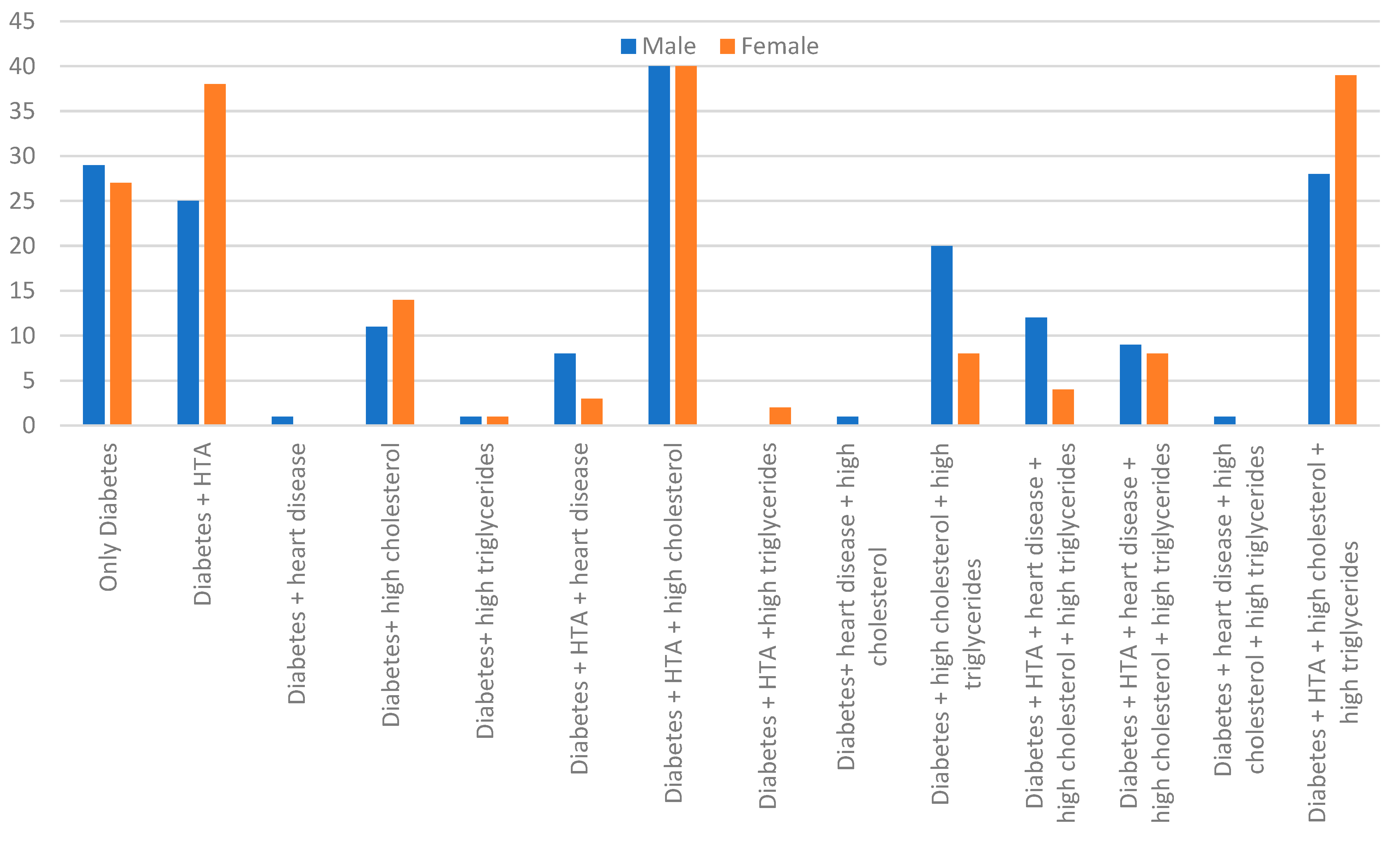
| Hypertension | Yes | Male | 122 | 32.97 | |
| Female | 134 | 36.22 | |||
| Heart disease | Yes | Male | 32 | 8.65 | |
| Female | 15 | 4.05 | |||
| Hypercholesterolemia | Yes | Male | 122 | 32.98 | |
| Female | 113 | 30.54 | |||
| Hypertriglyceridemia | Yes | Male | 62 | 16.76 | |
| Female | 54 | 14.59 | |||
| Age | Education Level | Smoking | Monthly Income | Family Support | Cultural Background | HbA1c | Adherence to Treatment | BMI | |
|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||
| Education level | −0.261 (<0.001) | ||||||||
| Smoking | −0.163 (0.002) | 0.232 (<0.001) | |||||||
| Monthly income | 0.033 (0.525) | 0.506 (<0.001) | 0.189 (<0.001) | ||||||
| Family support | 0.023 (0.663) | 0.020 (0.696) | 0.10 (0.851) | −0.004 (0.931) | |||||
| Cultural background | −0.259 (<0.001) | 0.366 (<0.001) | 0.124 (0.017) | 0.507 (<0.001) | 0.077 (0.138) | ||||
| HbA1c | −0.110 (0.035) | 0.177 (<0.001) | 0.049 (0.351) | −0.218 (<0.001) | 0.034 (0.516) | 0.288 (<0.001) | |||
| Adherence to treatment | −0.076 (0.147) | 0.198 (<0.001) | 0.319 (0.370) | 0.148 (0.004) | 0.121 (0.020) | 0.213 (<0.001) | −0.112 (0.031) | ||
| BMI | −0.087 (0.097) | 0.125 (0.16) | −0.138 (0.008) | −0.168 (0.001) | 0.002 (0.968) | 0.013 (0.796) | −0.054 (0.298) | 0.082 (0.116) |
| B | Standard Error | Wald | df | Sig | Exp(B) | |
|---|---|---|---|---|---|---|
| HbA1c–Education level | 0.005 | 0.098 | 0.003 | 1 | 0.959 | 1.005 |
| HbA1c–monthly income | −0.110 | 0.103 | 1.147 | 1 | 0.284 | 0.896 |
| HbA1c–cultural background | 0.988 | 0.221 | 19.974 | 1 | <0.001 | 2.686 |
| Adherence to treatment–education level | −0.181 | 0.097 | 3.473 | 1 | 0.062 | 0.834 |
| Adherence to treatment–monthly income | 0.089 | 0.103 | 0.736 | 1 | 0.391 | 1.093 |
| Adherence to treatment–cultural background | 0.895 | 0.222 | 16.504 | 1 | <0.001 | 2.448 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
del Río Pascual, B.; María, A.J.A.; María, V.L.J.; Azahara, R.N.; Dolores, V.L.M.; Rocio, P.G.; Alejandro, A.G.; Luciano, R.D.; Javier, F.C.F. Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study. Diabetology 2025, 6, 100. https://doi.org/10.3390/diabetology6090100
del Río Pascual B, María AJA, María VLJ, Azahara RN, Dolores VLM, Rocio PG, Alejandro AG, Luciano RD, Javier FCF. Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study. Diabetology. 2025; 6(9):100. https://doi.org/10.3390/diabetology6090100
Chicago/Turabian Styledel Río Pascual, Brieba, Antolí Jover Ana María, Vázquez Lara Juana María, Ruger Navarrete Azahara, Vázquez Lara María Dolores, Palomo Gómez Rocio, Artero García Alejandro, Rodríguez Díaz Luciano, and Fernández Carrasco Francisco Javier. 2025. "Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study" Diabetology 6, no. 9: 100. https://doi.org/10.3390/diabetology6090100
APA Styledel Río Pascual, B., María, A. J. A., María, V. L. J., Azahara, R. N., Dolores, V. L. M., Rocio, P. G., Alejandro, A. G., Luciano, R. D., & Javier, F. C. F. (2025). Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study. Diabetology, 6(9), 100. https://doi.org/10.3390/diabetology6090100






