Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study †
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Design
2.3. Data Collection
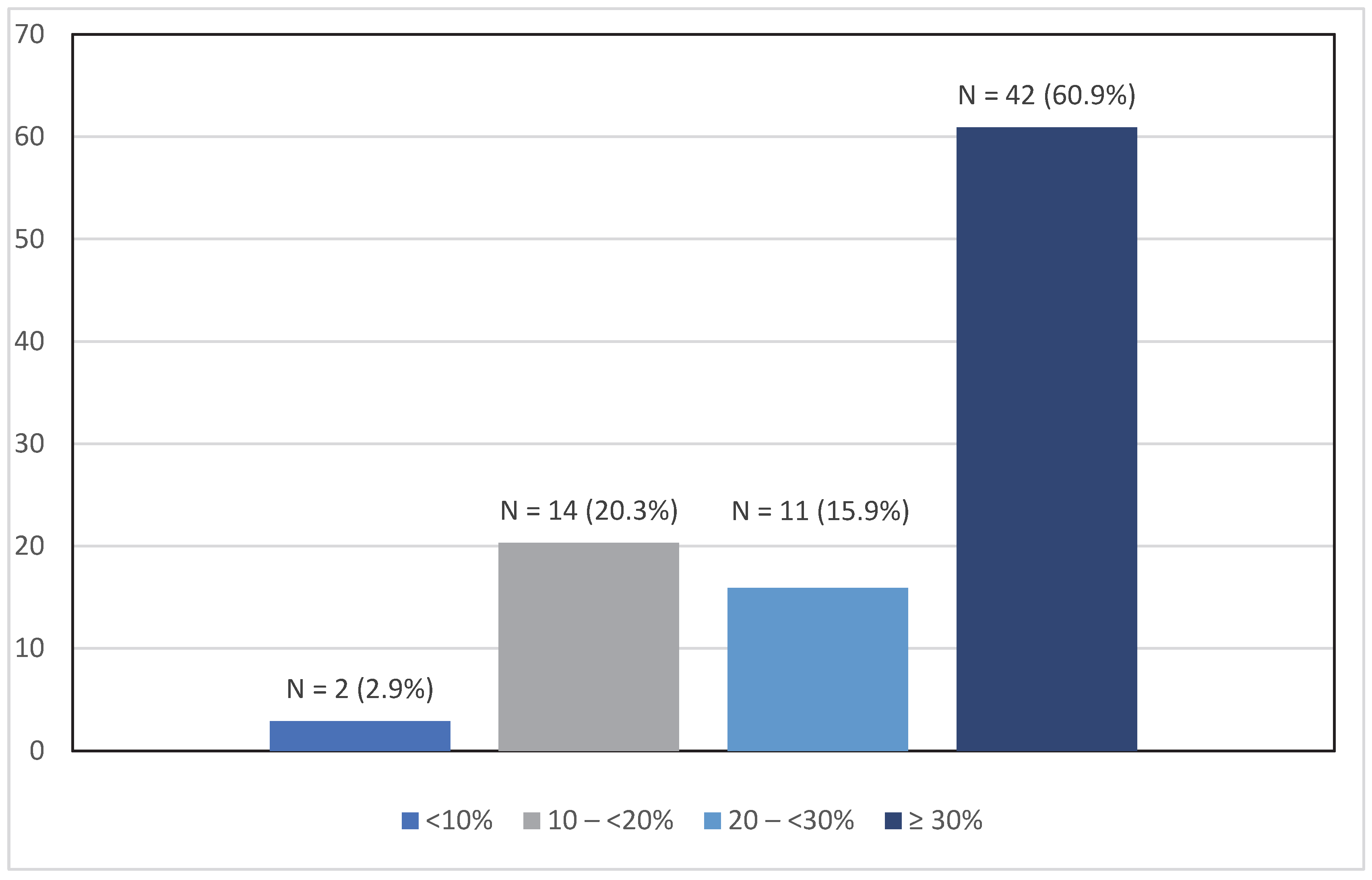
2.4. Framingham Cardiovascular Risk Estimation
2.5. Achievement of Hypertension Treatment Goal
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Health Service Executive. Diabetes National Clinical Programme. Available online: https://www.hse.ie/eng/about/who/cspd/ncps/diabetes/ (accessed on 9 August 2025).
- Pierse, T.; Barry, L.; Glynn, L.; Murphy, A.W.; Cruise, S.; O’Neill, C. A comparison, for older people with diabetes, of health and health care utilisation in two different health systems on the island of Ireland. BMC Public Health 2020, 20, 1446. [Google Scholar] [CrossRef]
- Al Hamarneh, Y.N.; Charrois, T.; Lewanczuk, R.; Tsuyuki, R.T. Pharmacist intervention for glycaemic control in the community (the RxING study). BMJ Open 2013, 3, e003154. [Google Scholar] [CrossRef]
- Al Hamarneh, Y.N.; Hemmelgarn, B.R.; Hassan, I.; Jones, C.A.; Tsuyuki, R.T. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk in Adult Patients with Type 2 Diabetes: The Multicentre Randomized Controlled R x EACH Trial. Can. J. Diabetes 2017, 41, 580–586. [Google Scholar] [CrossRef]
- Tsuyuki, R.T.; Al Hamarneh, Y.N.; Jones, C.A.; Hemmelgarn, B.R. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk. JACC 2016, 67, 2846–2854. [Google Scholar] [CrossRef] [PubMed]
- Krass, I.; Armour, C.L.; Mitchell, B.; Brillant, M.; Dienaar, R.; Hughes, J.; Lau, P.; Peterson, G.; Stewart, K.; Taylor, S.; et al. The Pharmacy Diabetes Care Program: Assessment of a community pharmacy diabetes service model in Australia. Diabet. Med. 2007, 24, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Schifano, F.; Robinson, P.; Phillips, G.; Doherty, L.; Melnick, P.; Laming, L.; Sinclair, A.; Dhillon, S. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: A randomized controlled study. Diabet. Med. 2012, 29, e326–e333. [Google Scholar] [CrossRef]
- Tsuyuki, R.T.; Beahm, N.P.; Okada, H.; Al Hamarneh, Y.N. Pharmacists as accessible primary health care providers: Review of the evidence. Can. Pharm. J. 2018, 151, 4–5. [Google Scholar] [CrossRef] [PubMed]
- IPSOS. Ipsos (Ireland) Veracity Index 2024—Who Do We Trust? 2024. Available online: https://www.ipsos.com/en-ie/ipsos-ba-veracity-index-2024-who-do-we-trust-ireland (accessed on 9 August 2025).
- Cooney, P.; Hanley, J.; Ryan-O’Brien, N.; Okada, H.; Bermingham, M. The views and experiences of people with type 2 diabetes being cared for by their community pharmacist: A cross-sectional patient survey. J. Diabetes Metab. Disord. 2022, 21, 1619–1624. [Google Scholar] [CrossRef]
- Henman, M.C. Primary Health Care and Community Pharmacy in Ireland: A lot of visions but little progress. Pharm. Pract. 2020, 18, 2224. [Google Scholar] [CrossRef]
- Irish Pharmaceutical Healthcare Association. Supply and Reimbursement. Available online: www.ipha.ie/supply-and-reimbursement (accessed on 9 August 2025).
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Government of Ireland. Healthy Ireland Survey 2022—Summary Report. 2022. Available online: https://www.gov.ie/pdf/?file=https://assets.gov.ie/241111/e31b2aaa-a8d7-411d-8b62-02cca079c741.pdf#page=null (accessed on 9 August 2025).
- HSE National Tobacco Control Office Health and Wellbeing Division. Smoking in Ireland 2014: Synopsis of Key Patterns. Available online: https://www.drugsandalcohol.ie/23450/1/smokinginireland2014.pdf (accessed on 9 August 2025).
- Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; Rosengren, A.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef]
- Brown, T.J.; Todd, A.; O’Malley, C.; Moore, H.J.; Husband, A.K.; Bambra, C.; Kasim, A.; Sniehotta, F.F.; Steed, L.; Smith, S.; et al. Community pharmacy-delivered interventions for public health priorities: A systematic review of interventions for alcohol reduction, smoking cessation and weight management, including meta-analysis for smoking cessation. BMJ Open 2016, 6, e009828. [Google Scholar] [CrossRef]
- Twigg, M.J.; Poland, F.; Bhattacharya, D.; Desborough, J.A.; Wright, D.J. The current and future roles of community pharmacists: Views and experiences of patients with type 2 diabetes. Res. Soc. Adm. Pharm. 2013, 9, 777–789. [Google Scholar] [CrossRef]
- Mittal, S.; Okada, H.; Bermingham, M.; Onda, M.; Farrelly, S.; Zaki, M.; Nakayama, T. Community Pharmacists’ Attitude, Practice and Confidence in Supporting People with Diabetes in Japan and Ireland: A Cross-sectional Survey. Yakugaku Zasshi 2023, 143, 871–879. [Google Scholar] [CrossRef]
- Elhiny, R.; O’Keeffe, L.M.; Bodunde, E.O.; Byrne, S.; Donovan, M.; Bermingham, M. Goal attainment, medication adherence and guideline adherence in the treatment of hypertension and dyslipidemia in Irish populations: A systematic review and meta-analysis. Int. J. Cardiol. Cardiovasc. Risk Prev. 2025, 24, 200364. [Google Scholar] [CrossRef] [PubMed]
- Buckley, B.; Shanahan, E.; Colwell, N.; Turgonyi, E.; Bramlage, P.; Perry, I.J. Blood pressure control in hypertensive patients in Irish primary care practices. J. Clin. Hypertens. 2009, 11, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.L.; Stevens, R.J.; Retnakaran, R.; Holman, R.R. Framingham, SCORE, and DECODE risk equations do not provide reliable cardiovascular risk estimates in type 2 diabetes. Diabetes Care 2007, 30, 1292–1293. [Google Scholar] [CrossRef]
- SCORE2 Working Group; ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Coupland, C.; Brindle, P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: Prospective cohort study. BMJ 2017, 357, j2099. [Google Scholar] [CrossRef]
- Stevens, R.J.; Kothari, V.; Adler, A.I.; Stratton, I.M.; Holman, R.R. The UKPDS risk engine: A model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clin. Sci. 2001, 101, 671–679. [Google Scholar] [CrossRef]
- Steed, L.; Sohanpal, R.; Todd, A.; Madurasinghe, V.W.; Rivas, C.; Edwards, E.A.; Summerbell, C.D.; Taylor, S.J.C.; Walton, R.T. Community pharmacy interventions for health promotion: Effects on professional practice and health outcomes. Cochrane Database Syst. Rev. 2019, 12, CD011207. [Google Scholar] [CrossRef]
- Collins, C.; Limone, B.L.; Scholle, J.M.; Coleman, C.I. Effect of pharmacist intervention on glycemic control in diabetes. Diabetes Res. Clin. Pract. 2011, 92, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Integrated Model of Care for People with Type 2 Diabetes Mellitus 2024. Available online: https://www.hse.ie/eng/about/who/cspd/ncps/diabetes/moc/hse-integrated-model-of-care-for-people-with-type-2-diabetes-mellitus.pdf (accessed on 9 August 2025).
- Okura, Y.; Urban, L.H.; Mahoney, D.W.; Jacobsen, S.J.; Rodeheffer, R.J. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J. Clin. Epidemiol. 2004, 57, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Number (%) or Mean (±SD)/Median (IQR) |
|---|---|
| Demographic | |
| Male/female | 70 (66.0)/36 (34.0) |
| Age (years) | 66.0 (56.5:72.0) |
| Duration of diabetes (years) | 9.5 (5.0:17.0) |
| Medical history | |
| Family history of premature heart disease | 40 (37.7) |
| Chronic kidney disease | 6 (5.7) |
| Atrial fibrillation | 9 (8.5) |
| Heart failure | 2 (1.9) |
| Dyslipidaemia | 59 (55.7) |
| Hypertension | 60 (56.6) |
| Peripheral arterial disease | 5 (4.7) |
| Stroke/transient ischaemic attack | 5 (4.7) |
| Angina/coronary artery disease/coronary revascularisation | 10 (9.4) |
| Myocardial infarction a | 7 (6.6) |
| Measures | |
| Body mass index (kg/m2) b | 28.9 ± 5.3 |
| Systolic blood pressure (mmHg) | 136.4 ± 19.0 |
| Diastolic blood pressure (mmHg) | 80.8 ± 10.1 |
| Home blood glucose measure (mmol/L) c | 7.15 ± 2.23 |
| Lifestyle Characteristic | Number (%) |
|---|---|
| Smoking status | |
| Current smoker | 21 (19.8) |
| Former smoker | 45 (42.5) |
| Non-smoker | 40 (37.7) |
| Alcohol consumption | |
| None | 38 (35.8) |
| Occasional | 53 (50.0) |
| 1–2 days/week | 13 (12.3) |
| >2 days per week | 2 (1.9) |
| Diet a | |
| No specific diet | 31 (29.2) |
| Low-sugar diet | 58 (54.7) |
| Low-salt diet | 33 (31.1) |
| Low-saturated fat diet | 20 (18.9) |
| Gluten-free diet | 3 (2.8) |
| High fruit and vegetable diet | 27 (25.5) |
| Other diet | 26 (24.5) |
| Exercise b | |
| No exercise | 44 (41.5) |
| Moderate exercise | 33 (31.1) |
| Very active | 28 (26.4) |
| Self-reported stress | |
| No stress | 36 (34.0) |
| Mild stress | 38 (35.8) |
| Moderate stress | 23 (21.7) |
| High stress | 9 (8.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaki, M.; O’Sullivan, C.; Barrett, E.; Mirzai, N.; Thornton, H.; Al Hamarneh, Y.N.; Bermingham, M. Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study. Diabetology 2025, 6, 107. https://doi.org/10.3390/diabetology6100107
Zaki M, O’Sullivan C, Barrett E, Mirzai N, Thornton H, Al Hamarneh YN, Bermingham M. Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study. Diabetology. 2025; 6(10):107. https://doi.org/10.3390/diabetology6100107
Chicago/Turabian StyleZaki, Marian, Claire O’Sullivan, Ellen Barrett, Nasim Mirzai, Hazel Thornton, Yazid N. Al Hamarneh, and Margaret Bermingham. 2025. "Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study" Diabetology 6, no. 10: 107. https://doi.org/10.3390/diabetology6100107
APA StyleZaki, M., O’Sullivan, C., Barrett, E., Mirzai, N., Thornton, H., Al Hamarneh, Y. N., & Bermingham, M. (2025). Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study. Diabetology, 6(10), 107. https://doi.org/10.3390/diabetology6100107





