Abstract
Diabetes is a leading non-communicable disease with a huge and predictably increasing burden on individuals, societies and governments. Interprofessional education (IPE) aims to enhance healthcare providers’ competence and patient care by providing well-organised, coordinated interprofessional care (IPC) within teams of healthcare professionals of different disciplines. Interprofessional practices are crucial in diabetes care. However, evidence on the effect of diabetes-specific IPE on diabetes outcomes is limited. This study aims to survey and report recent findings on the impact of interprofessional approaches on the outcomes of diabetes management. A systematic search of PubMed and Google Scholar from 2008 was adopted to identify relevant studies. After screening for relevance, the studies used in this review were thematically analysed, and two main categories of the findings were isolated: the impact of IPE and IPC on enhanced care provision and on improved diabetes self-management. The results indicate that healthcare professionals and students and people with diabetes benefit from IPE/IPC to improve diabetes outcomes and quality of care. However, improving diabetes care is achieved when inhibitors are addressed to incorporate IPE in health professions curricula and to support IPC in clinical settings.
1. Introduction
Diabetes is one of the most prevalent non-communicable diseases in the world [1]. It is an arguably familiar disease as it has been thoroughly researched over the years [2]. Furthermore, notable advancements in its treatment have been achieved [2]. Despite these facts, diabetes remains a substantial and remarkably worsening health and economic burden that policymakers and governments strive to control and mitigate [1,2]. The International Diabetes Federation (IDF) stated in its 2021 report that diabetes is “spiralling out of control” [1]. Accordingly, every effort leading to the prevention and treatment of diabetes and avoidance or delay of diabetes complications must be considered. Amongst those efforts, techniques like interprofessional education (IPE) and interprofessional collaboration (IPC) have been beneficial to patients with complex, chronic diseases [3]. However, the literature can benefit from an evaluation of the evidence base for the efficacy and effectiveness of interprofessional approaches on diabetes management practices and the outcomes of patients with diabetes.
IPE occurs when professionals from two or more disciplines learn with, from and about each other to optimise healthcare delivery by enhancing teamwork and communication skills, thus strengthening health systems and improving health outcomes [3,4].
IPE can be integrated into health profession curricula and introduced to existing practices via professional development and continued medical education. It is a combination of knowledge, skills, values, attitudes and behaviours that constitute collaborative practice [5,6]. Interprofessional collaboration (IPC) refers to the joint efforts of HCPs from different disciplines to work together with the common goal of providing high-quality patient care [6]. Health workers are ready for collaborative practice when they have learnt and are competent in interprofessional teamwork. Optimal care is provided when a team of HCPs works together and at equal measure, each member being aware of their own role and knowledgeable, supportive and appreciative of the other members’ roles in the care provision [3,4]. This is when IPE emerges as an essential aspect of care and when collaboration results in a synergistic effect that benefits the patients and refines HCPs’ skills, attitudes and knowledge [4]. Interprofessional strategies can effectively equip HCPs to provide enhanced care both individually and as a team, thus empowering people with diabetes to manage the multi-faceted challenges associated with their condition more effectively [7,8,9].
Despite being identified as approaches to care provision that enhance care services, IPE and IPC arguably have some overlapping features, which makes drawing conclusions on their distinct effects on improving aspects of health a bit challenging [10]. For example, the definitions for IPE and IPC partially overlap, which makes the conceptual demarcation of the two processes hard to identify and hinders the establishment of a profound evidence base on interprofessional strategies that are most effective in healthcare [10]. Additionally, the close-knit nature of IPE and IPC makes many researchers use the terms interchangeably as they report on their effects on improving care provision, and IPE is often used as an umbrella term to encompass any interprofessional activity [11].
The use of IPE in healthcare reportedly provides the highest quality of patient care, improving patient safety, healthcare services and the individual skills of every HCP team member [12,13]. In a meta-analysis aimed at determining the effectiveness of IPE on improving students’ knowledge, skills and attitudes, the positive impact and effectiveness of IPE programmes have been shown in multiple healthcare disciplines [12]. The health professions in which IPE has been assessed include emergency department nurses and physicians, primary health care practitioners, pharmacists, medical and allied health students and social care professionals, among others [12,13,14]. Diabetes care is also one of the many disciplines in which IPE has been proven beneficial as it improves confidence, knowledge and quality of diabetes care [3,4]. The improvement in the quality of diabetes care was reflected through specific parameters, including significantly reduced management errors, enhanced blood glucose monitoring, increased foot assessment and improved practice efficiency (number of patients seen per hour) [4,7]. A systematic review and meta-analysis by Nurchis et al. (2022) reported a significant association between collaborative practice and patient satisfaction and mental well-being, with promising evidence to support an association with increased self-care and quality of life [15].
While evidence suggests that IPE positively impacts healthcare practices in general and diabetes management in clinical practice, the efficacy and effectiveness of IPE on patient outcomes can benefit from additional scrutiny. This review aims to collect evidence related to the importance of IPE in diabetes management, potentially guiding cost-effective treatment options that can improve the quality of life for individuals with diabetes. The review will make two main contributions to the literature: (A) the personal benefit from IPE programmes for healthcare professionals and students and how this reflects on improved practice and quality of patient care; (B) measurable changes in disease outcomes for patients with diabetes. Additionally, the review will identify barriers to applying IPE in practice and highlight ways to overcome those barriers.
2. Methods
2.1. Objective
This review aims to answer the following question: What are the established results of implementing diabetes-specific IPE on diabetes management and outcomes?
2.2. Research Design
We utilised an integrative review approach because it is helpful in exploring the literature within a specific field [16]. It also allows the investigation of an extensive sample base and the inclusion of results from studies with various designs and methodologies [16].
2.3. Searching the Literature
The literature searches for this integrated review were conducted using PubMed and Google Scholar for recent studies/reviews investigating interprofessional interventions on diabetes management and outcomes. We looked for studies published within the past 15 years (2008–2023), and the vast majority of studies were concentrated within the past ten years, roughly following the issuance of the IPE core competencies in 2011 [6]. Search keywords were as follows: interprofessional, interprofessional education, interprofessional collaboration, collaborative teamwork, diabetes management and diabetes outcomes and combinations using Boolean operators. We included studies that reported on (1) health professions students and/or (2) healthcare professionals receiving IPE and/or engaging in IPC for the management of diabetes and (3) patients with diabetes receiving diabetes education by an IPC team. We excluded studies written in languages other than English, study protocols and studies that only reported the impact of IPE/IPC on oral health in people with diabetes. PubMed search returned 270 results, and Google Scholar returned 17,700 results. After screening to remove duplicates, full-text articles were appraised for relevance, and 19 studies were selected. Studies were analysed to generate themes for research findings (Figure 1: Searching the literature).
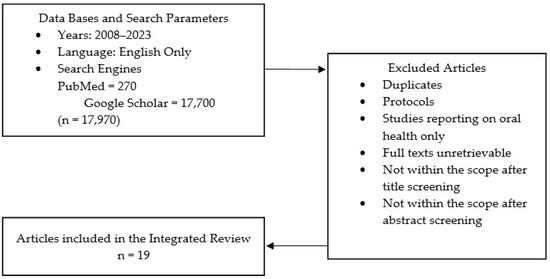
Figure 1.
Flow diagram of article selection for further review.
The nature of this research approach allows for broad sampling and the inclusion of studies with different methodologies [16]. Hence, the selected studies were conducted in different settings (clinical, primary and secondary care or educational; university campuses), had different research methodologies (quasi-experimental, systematic reviews, meta-analyses, randomised controlled trials and case studies), included different subjects (students of health professions, HCPs and people with diabetes receiving diabetes education or care from an IPC team) and had different interventions (different types of IPE/IPC encounters through on-site or virtual events). This allowed for greater opportunities to explore the topic more comprehensively.
3. Results
Nineteen studies were included in this review. The analysis of the included studies resulted in two main categories of the findings, both of which can positively influence patient outcomes: the impact of IPE/IPC on enhancing diabetes care provision by HCPs and students in healthcare professions and the effect of IPE/IPC on diabetes management.
3.1. Study Characteristics
The characteristics of the included studies are summarised in Table 1. Study designs and approaches were different, including mixed methods studies (n = 4), systematic reviews and meta-analyses (n = 3), systematic reviews (n = 3), meta-analyses (n = 2), quasi-experimental studies (n = 2), an integrative systematic review (n = 1), a narrative review (n = 1), qualitative/descriptive study (n = 1), a cross-sectional study (n = 1) and a non-randomised parallel-group clinical trial (n = 1).

Table 1.
Summary of the selected studies.
Table 1.
Summary of the selected studies.
| Citation | Title | Setting | Study Aim | Study Design | Study Participants | Data Collection Method | Sample Size | Study Results |
|---|---|---|---|---|---|---|---|---|
| Study 1 Nurchis et al. (2022) [15] | Interprofessional Collaboration and Diabetes Management in Primary Care: A Systematic Review and Meta-Analysis of Patient-Reported Outcomes | Primary Care | Evaluate the impact of IPC interventions for the management of type 2 diabetes in primary care settings via patient-reported outcomes. | Systematic review and meta-analysis | Patients with type 2 diabetes mellitus in primary care | Literature Search | 19 RCTs, each with different sample size | IPC is significantly associated with an increase in both patient satisfaction and mental well-being. There was also promising evidence supporting the association between an interprofessional approach and an increase in self-care and in generic and specific quality of life. |
| Study 2 Kangas et al. (2021) [17] | Students’ perceptions of interprofessional collaboration on the care of diabetes: A qualitative study | University, a course was given to med and pharmacy students | Explore changes in medical and nursing students’ perceptions of IPC on diabetes management after an experimental, voluntary course of IPE with practical content. | Qualitative study | Pharmacy and medical students | Focus-group interviews before and after a novel IPE course | 30 15 medical students 15 nursing students | The course improved the students’ self-perceived competence and confidence in IPC in the care of patients with diabetes, and their understanding of IPC changed towards a more patient-centred and holistic perspective. |
| Study 3 Pascucci et al. (2021) [18] | Impact of interprofessional collaboration on chronic disease management: Findings from a systematic review of clinical trial and meta-analysis | Pre-dominantly outpatient clinics. A few studies were conducted in hospitals or pharmacies. | Study the impact of IPC vs. usual care on clinical outcomes, clinical process measures and patient-reported outcomes for patients with chronic diseases. | Systematic review and meta-analysis | Patients with at least one chronic disease | Literature search: data extraction and synthesis from selected studies | 23 RCTs, each with different sample size | Significant reduction in the levels of systolic blood pressure, diastolic blood pressure, HbA1c and LDL. |
| Study 4 Lee et al. (2021) [19] | Assessment of Interprofessional Collaborative Practices and Outcomes in Adults with Diabetes and Hypertension in Primary Care A Systematic Review and Meta-analysis | Primary care | Study the association of interprofessional collaborative practice (3+ health professions) with HbA1c, systolic and diastolic blood pressure levels. | Systematic review and meta-analysis | Adults with diabetes and/or hypertension receiving primary care | Literature search: data extraction and synthesis from selected studies | 50 studies for the SR 39 studies in the meta-analyses, each with different sample size | ICP was associated with: Improved HbA1c, systolic and diastolic blood pressure levels. Reductions in HbA1c were irrespective of baseline value. |
| Study 5 Pisano et al. (2020) [20] | An interprofessional experience in diabetes management for pharmacy and medical students | University, a course was given to med and pharmacy students | Examine attitudes towards interprofessional learning before and after an IPE experience | Quasi-experimental | Pharmacy and medical students | Surveys comparing pre- and post-IPE experience | 168 participants 138 med students 30 pharmacy students | Learner attitudes were positive overall and improved from pre-test to post-test, suggesting more favourable attitudes to IPE after completing the class. Pharmacy students had more positive attitudes to IP learning before and after. Their understanding of the roles and responsibilities of the other learner groups was enhanced. |
| Study 6 Atsalos et al. (2019) [21] | Meeting the challenges posed by an escalating diabetes healthcare burden: A mixed methods study | Hospital | Identify new strategies to maintain optimal care for patients with diabetes while in hospital | Mixed methods | Nurses and midwives Recently discharged hospital patients | Surveys Focus group interviews Individual interviews | 173 surveys 40 focus group interviews 6 individual interviews | Knowledge and confidence in diabetes management among HCPs should be enhanced via the introduction of focused education strategies, improved communication and teamwork to avoid delays in treatment requirements. |
| Study 7 Levengood et al. (2019) [22] | Team-Based Care to Improve Diabetes Management: A Community Guide Meta-analysis | Mostly clinics or hospitals in an urban setting | Study the effectiveness of team-based care (TBC) in improving health outcomes of people with diabetes. Does TBC work? How should it be implemented to be effective? | Meta-analysis | Mostly patients with type 2 diabetes | Literature search: data extraction and synthesis from selected studies | 35 RCTs, each with different sample size | Team-based care improves blood glucose, blood pressure and lipid levels for patients with type 2 diabetes. |
| Study 8 Kangas et al. (2018) [9] | An integrative systematic review of interprofessional education on diabetes | University, online courses or the clinical workplace. | Assess the outcomes of IPE on diabetes management. | Integrative systematic review | Groups of healthcare or social care students or professionals. | Literature search: data extraction and synthesis from selected studies | 14 studies, each with different sample size | Diabetes-specific IPE results in benefits for the learners and potentially contributes to better care provision for patients with diabetes. |
| Study 9 Riskiyana et al. (2018) [23] | Objectively measured interprofessional education outcome and factors that enhance program effectiveness: A systematic review | University or clinical or community practices. | Generalise IPE learning outcomes in a global context. | Systematic Review | Healthcare professionals or students who experienced IPE or training. | Literature search: data extraction and synthesis from selected studies | 16 studies, each with different sample size | IPE improved interprofessional collaborative knowledge, skills, behaviour and quality of care. |
| Study 10 Nagelkerk et al. (2018) [7] | Improving outcomes in adults with diabetes via an interprofessional collaborative practice program | Universities, family practice clinics. | Assess the effectiveness of interprofessional collaborative practice (IPCP) intervention on HCPs efficiencies, student learning and clinical outcomes of patients with diabetes. | Sequential mixed methods design | HCPs and students and patients with diabetes. | Staff and student teams received core modules on IPCP, implemented IPCP practices and completed pre and post knowledge tests and evaluation surveys. Forms, questionnaires, assessment tools and surveys were used. Focus group discussions were also held periodically. | HCPs practice team (n = 20), an interprofessional team of students (n = 22) and patients (n = 250) | IPCP interventions improved communication, team care, provider productivity and improved diabetes outcomes (A1c, triglyceride, lipid ratio, blood glucose) for a subgroup of higher-risk patients with diabetes. |
| Study 11 Račić et al. (2017) [24] | The effects of interprofessional diabetes education on the knowledge of medical, dentistry and nursing students | University. | Assess the effects of interprofessional learning on diabetes knowledge. | Cross-sectional Study | Students of medicine, dentistry and nursing. | Group 1 received an interprofessional diabetes course. Group 2 received a diabetes course within groups of single professions. Both groups completed pre- and post-intervention knowledge assessments | 66 students. Medicine students (n = 29) Dentistry students (n = 21) Nursing students (n = 16). | IPE activities may improve health profession students’ specific clinical knowledge, skills, confidence and attitude toward IPC. |
| Study 12 Khan et al. (2017) [25] | Diabetes foot complication: assessing primary and secondary outcomes of multidisciplinary team versus standard care (a systematic review) | Healthcare setting (podiatry clinics, general hospitals and general practice) | Evaluate the effectiveness of multidisciplinary teamwork compared to standard care in reducing diabetes-related foot complications and cost and improving quality of life. | Systematic Review | Patients of 25 years of age or older with type 1 or type 2 diabetes with risk for foot ulceration or amputation. | Literature search: data extraction and synthesis from selected studies | 9 studies | Multidisciplinary team approaches to diabetic foot care cause a significant reduction in complications compared to the standard approach. |
| Study 13 Ching et al. (2015) [26] | Is an inter-professional education programme effective in promoting collaboration and improving diabetes care? | General practice setting (n = 26) | Assess the impact of an IPE program on the knowledge, attitudes and behaviours of HCPs and how it may relate to disease outcomes. | Mixed-method Study | General practitioners and practice nurses Patients with diabetes | Interviews and data extraction from diabetes registers. Comparison between pre- and post-IPE program data. (24 months) | 26 primary care practices 4167 people with diabetes | the IPE program resulted in improving the quality of care, patient outcomes (cholesterol and blood pressure levels), professional behaviours and clinical practices (lower referrals and more patients receiving foot care and being screened for microalbuminuria). |
| Study 14 Yamani et al. (2014) [27] | The effect of interprofessional education on interprofessional performance and diabetes care knowledge of health care teams at level one of health service provision | Educational. | Study the effect of IPE on diabetes care knowledge and performance of healthcare teams. | Quasi-experimental Study | Healthcare teams | Pre- and post-intervention (IPE workshop) team performance evaluations and knowledge assessments (3 months) | 6 teams (n = 34) 12 physicians 10 healthcare associates 12 Behvarz (rural healthcare providers) | IPE can increase diabetes care knowledge and collaborative performance of teams of HCPs |
| Study 15 Pittenger et al. (2013) [28] | An Interprofessional Diabetes Experience to Improve Pharmacy and Nursing Students’ Competency in Collaborative Practice | University campuses. | Improve pharmacy and nursing students’ competency in collaborative practice via an interprofessional diabetes experience. | Mixed-method Study | Pharmacy and nursing students. | An IPE diabetes course was given. Pre- and post-intervention surveys. | 9 groups. Pharmacy students (n = 34) Nursing students (n = 17) | Interprofessional approaches increase students’ knowledge of the roles of other professions and understanding of communication strategies. |
| Study 16 Reeves et al. (2013) [29] | Interprofessional education: effects on professional practice and healthcare outcomes | Different areas of clinical practice | Evaluate the effectiveness of IPE interventions as opposed to profession-specific or no-education interventions. | Narrative Review | Professionals or patients involved in IPE intervention | Comparison between outcomes following an IPE intervention, outcomes with a non-IPE intervention and outcomes with no intervention. | 15 studies (RCTs, controlled before and after studies and interrupted time series studies). | A range of positive results on diabetes clinical outcomes and improving diabetes care was reported. |
| Study 17 Pimouguet et al. (2011) [30] | Effectiveness of disease-management programs for improving diabetes care: a meta-analysis | Different healthcare settings. | Study the effectiveness of disease-management programs for improving glycemic control in adults with diabetes. | Meta-analysis | Adults with type 1 or 2 diabetes whose HbA1c levels were measured to evaluate the effects of disease management programs. | Literature search: data extraction and synthesis from selected studies | 41 RCTs | Disease management programs significantly impact HbA1c in adults with diabetes, |
| Study 18 Hammick et al. (2009) [31] | A best evidence systematic review of interprofessional education: BEME Guide no. 9 | Educational settings | Review best evidence on IPE evaluations, classify outcomes and identify mechanisms guiding IPE outcomes. | Systematic Review | Professional groups from health and social care. | Literature search: data extraction and synthesis from selected studies | 21 studies | IPE is used as a mechanism to develop clinical practice and improve services |
| Study 19 Janson et al. (2009) [32] | Improving Chronic Care of Type 2 Diabetes Using Teams of Interprofessional Learners | Internal medicine clinics. | Enhance the care and outcomes of patients with type 2 diabetes by introducing a care model to interprofessional teams. | Non-randomised parallel-group clinical trial (18 months) | Adults with type 2 diabetes | Interprofessional team care was provided by groups of HCPs and compared with usual care by internal medicine residents only. Pre- and post-intervention data collection. | Team care professionals: Primary care internal medicine residents, nurse practitioner students and pharmacy students. 384 adult patients with type 2 diabetes | The quality of care provided to adult patients with type 2 diabetes improved with interprofessional team care. |
3.2. Study Participants
Study participants were either of the following:
- Healthcare professionals (general practitioners, practice nurses and healthcare associates, n = 8);
- Students of healthcare professions (medicine, pharmacy, nursing, midwifery, dentistry, podiatry, dietetics and social care, n = 7);
- Adult patients with type 1 or type 2 diabetes (n = 11).
3.3. IPE Interventions and Settings
The IPE interventions used in the selected studies are diverse, particularly because many studies are reviews and analyses that included various additional studies. However, when study participants were students of health professions, the IPE intervention mostly consisted of an in-person or online IPE university course, either in respective university or health practice settings. The course was primarily mandatory for students but sometimes voluntary. Upon the completion of the course, students either received credit hours toward their programs or certificates of completion. For HCPs, the IPE intervention was predominantly a shift in practice toward a team-based interprofessional diabetes management approach following IPE learning and/or training sessions within primary or secondary care clinics.
3.4. Findings from Content Analysis
The findings are discussed in two main categories. First, personal benefit from IPE programmes for healthcare professionals and students and how it reflects on improved practice and quality of patient care will be highlighted. Second, the actual measurable changes in disease outcomes for patients with diabetes will be highlighted. Additional findings include identifying barriers/inhibitors to implementing IPE in practice and suggesting approaches to overcome such barriers.
3.5. Impact on Provider/Student Approaches and Enhancement of Care Provision
Of the 19 studies analysed, 13 studies reported on the (1) effects of IPE/IPC on provider or student characteristics in diabetes care provision and (2) on aspects of healthcare provision for patients with diabetes that were impacted. For provider/student characteristics, the studies mention advancements in self-perceived competence in diabetes care [17], improved confidence [17,21,24], knowledge [21,23,24,27], skills [23,24], behaviour [23,26] and attitudes [20,24] toward IPE and collaborative practice. For modified aspects of healthcare, the studies report improved clinical practice [9,17,26,31], quality of care [23,26,29,32], understanding of roles and responsibilities of other HCPs or students [20,28], communication [7,21,28], collaboration and interprofessional team care [7,21,27] and provider productivity [7]. Table 2 summarises those findings.
As far as healthcare provision in practice centres is concerned, the bulk of evidence points toward some form of added value for interprofessional approaches in diabetes care, while only a few studies suggest a neutral effect. A systematic review of 16 articles that used standardised, objective measurements to evaluate the outcomes of IPE programmes regarding IPC competencies concluded that IPE enhances IPC knowledge, skills and behaviour [23]. The major strength of the methodology of this systematic review is the use of objective assessment tools to draw conclusions as opposed to subjective assessments conducted in other studies, such as those with self-report assessments [23]. Those findings conform with, or even lend higher credibility to, previously described reports on the importance of IPE in increasing knowledge, skills and attitudes toward IPC in general [31,33] and toward IPC in diabetes care in particular [29].
Perhaps the most substantial evidence supporting IPE’s effectiveness on diabetes comes from the integrative systematic review by Kangas et al., published in 2018 [9]. This integrative review aimed at surveying all the available, recent literature on diabetes-specific IPE and analysing its effects on diabetes management [9]. With reference to a total of 14 studies that satisfied the inclusion criteria, this study concluded that IPE in diabetes care had both “individual gains” for the HCPs, such as an increase in knowledge and skills, confidence, motivation and team competency to treat patients with diabetes and “external benefits”, such as improved patient outcomes and optimised practice approaches [9]. The review also identifies some strengths and challenges of applying IPE in diabetes care. Strengths include acquiring better knowledge about diabetes management in interprofessional teams as opposed to individual, discipline-specific knowledge, while challenges include the novelty of IPE and the need for additional financial, organisational (scheduling, room allocations, etc.) and possibly human resources for its successful incorporation in healthcare [9].
The introduction of IPE as a mandatory learning module in undergraduate programmes has been on the rise in different countries, such as the USA, the UK, Finland and Germany. In some countries, it has been integrated in response to government reforms of the health sector concerning diabetes care in an attempt to increase treatment efficiency and avoid delays [7,32,34]. The aim was to increase treatment efficiency by providing care for more people with diabetes, particularly the easier-to-manage cases, in the primary care setting. Improved primary care treatment will avoid delays in care provision resulting from referring each patient to secondary care and free secondary and tertiary care for treating the most urgent cases first [32]. Positive outcomes have been observed when healthcare professionals are involved as partners in learning and teaching IPE modules and IPE implementation in practice. IPE modules have been successful in preparing HCPs with better knowledge of IPC care and practice [7,17,24,27,28], a more positive attitude to interprofessional learning [20] and improved self-perceived confidence and ability to perform IPC in diabetes care [17], team dynamics, such as communication [7,24,28], and behaviour change knowledge [7].
In addition to the relatively well-established importance of providing collaborative learning opportunities on diabetes management to current and future HCPs involved in diabetes management, it seems that the effect of this collaborative learning on students can be long-lasting [26]. Reeves et al. reported in a systematic review of 46 “high-quality” IPE studies that remarkably more positive than neutral outcomes of IPE are being reported [35]. The authors also communicated that learners have a good, sustained response to IPE, marked by improved attitudes and perceptions of each other and an increase in their collaborative skills and knowledge [35].

Table 2.
Reported impact on health provider/student approaches and enhancement of care provision.
Table 2.
Reported impact on health provider/student approaches and enhancement of care provision.
| Reported Parameter | Selected Studies |
|---|---|
| Impact on health provider/student | |
| Better self-perceived competence in diabetes care | [17] |
| Improved confidence | [17,21,24] |
| Improved knowledge | [21,23,24,27] |
| Improved skills | [23,24] |
| Improved behaviour | [23,26] |
| Improved attitudes toward IPE and IPC | [35] |
| Impact on aspects of healthcare provision | |
| Improved clinical practice | [9,17,26,31] |
| Improved quality of care | [23,26,29,32] |
| Improved understanding of roles and responsibilities of other HCPs or students | [20,28] |
| Improved communication | [7,21,28] |
| Improved IPC and team care | [7,21,27] |
| Improved provider productivity | [7] |
3.6. Effect on Diabetes Self-Management and Disease Outcomes
Nine studies reported findings on diabetes management, including subjective and objective measurements of patients’ outcomes. Findings included a significant association between IPE/IPC and an increase in patient satisfaction [15] and well-being [15] and promising evidence of improvements in diabetes self-management tasks [15] and quality of life [15]. Objectively reported patient outcomes include the following levels of clinical indicators that have also been positively impacted by IPE/IPC interventions: HbA1c [7,18,19,29,30], blood glucose [7,22], systolic blood pressure [18,19,22,26], diastolic blood pressure [18,19,22,26], LDL [18,19], cholesterol [26], triglyceride [7], lipid ratio [7] and diabetic foot complications [25]. Table 3 summarises those findings.
Patients treated in practice settings that provide care in interprofessionally influenced approaches have been described as more competent and efficient in their diabetes self-management in a way that significantly improves their disease outcomes [18,30]. This is true when patients contact their health providers more frequently and take the initiatives to make changes to their own diabetes management regimen [31]. This is also true when patients are aware and capable of using the available support system and when they receive integrated care from an interprofessional team, which improves care processes, lowers the use of urgent care and increases the number of scheduled visits for care follow-up [32]. This favourable patient outcome seems to be the result of the joint efforts of empowered patients and the IPC approach to managing those patients.
A recent systematic review and meta-analysis evaluating the impact of IPC interventions on chronic disease management revealed that five out of the eight studies that reported the effect on the blood levels of glycated haemoglobin found significantly lower HbA1c levels in the intervention groups [18]. There was also strong evidence indicating a decrease in smoking and moderate evidence documenting an improved clinical process outcome of performing diabetic foot examinations more frequently in the intervention groups [18]. The same effect on HbA1c levels has been described in a meta-analysis of 35 studies that aimed to assess the effectiveness of team-based care in managing diabetes, which additionally reported more significant improvements in blood lipid levels and blood pressure compared to controls [22]. Patient safety has also been reported as optimised by providing timely care and intervention and enhancing coordination and communication in the multidisciplinary, integrated team [21], as has the management of diabetic foot ulcers [36].

Table 3.
Reported effects on diabetes self-management and disease outcomes.
Table 3.
Reported effects on diabetes self-management and disease outcomes.
| Reported Parameter | Selected Studies |
|---|---|
| Indicators of Diabetes Management | |
| Increased patient satisfaction | [15] |
| Improved patient wellbeing | [15] |
| Improved DSM skills | [15] |
| Improved generic and diabetes-specific quality of life | [15] |
| Disease outcomes | |
| Reduced HbA1c | [7,18,19,29,30] |
| Reduced blood glucose | [7,22] |
| Reduced SBP | [18,19,22,26] |
| Reduced DBP | [18,19,22,26] |
| Reduced Cholesterol | [26] |
| Reduced LDL | [18,19] |
| Reduced Triglyceride | [7] |
| Reduced Lipid Ratio | [7] |
| Reduced diabetic foot complications | [25] |
DSM: diabetes self-management, SBP: systolic blood pressure, DBP: diastolic blood pressure, LDL: low-density lipoprotein.
3.7. Inhibitors and Enablers of IPE and IPC in Practice
For IPE to be successfully implemented in clinical practice settings, challenges associated with its learning and application must be addressed and enablers established. Incorporating IPE into the curricula of health professions is challenging as it entails drastic changes to the existing state of affairs, such as necessitating additional costs and having uncertain outcomes, and redefines the roles of individual stakeholders, resulting in a high degree of resistance [37]. A literature review by Lawlis et al., published in 2014, identified three primary stakeholders when the barriers to embedding IPE in higher education health curricula are reported: government and professional, institution and individual [37]. Being resource-intensive, additional funding is essential to ensure this implementation. At the government and professional level, funding is scarce, and the same is true at the level of higher educational institutions that are mostly already financially stretched [37]. Additionally, stakeholder relationships are impacted by the change in the organisation at the government and professional level associated with the implementation of IPE in higher education health curricula [37]. At the institutional level, additional barriers include the ability to develop and deliver IPE within the pre-existing curricula, especially when accounting for differences in scheduling and assessment criteria and time constraints of the diverse streams of health curricula [37]. At the individual level, barriers include the lack of adequate faculty support, understanding and perceived need for IPE, limited IPE professional development opportunities and lack of staff rewards for their involvement in IPE initiatives [37].
Likewise, some of the identified challenges for IPC is novelty [9]. It is increasingly being introduced to healthcare institutions with pre-existing operational systems, and the many changes that need to be undertaken for its initiation and implementation are often met with resistance in established practices. Additionally, the lack of adequate resources poses a great challenge, which also requires planning and sourcing [9]. Table 4 summarises the inhibitors of IPE/IPC in practice and suggests possible solutions to overcome them.

Table 4.
Barriers to applying IPE/IPC in practice and possible approaches to overcome those barriers.
Table 4.
Barriers to applying IPE/IPC in practice and possible approaches to overcome those barriers.
| General Barriers | ||
|---|---|---|
| General barriers | Barriers | Possible approaches to overcome barriers |
| Changes in existing state of affairs are often met with resistance due to the need for redefining the roles of individual stakeholders [37] | Identify the causes of resistance. Allow HCPs to influence the change, feel prepared for the change and recognise its value [38]. | |
| Novelty- resource-intensive programme with uncertain outcomes [9] | Awareness raising of the impact of IPE/IPC on patient outcomes [39]. | |
| Inadequate evaluation and research [40] | Develop standardised IPE assessment tools, establish research priorities and promote rigorous evaluation for IPE initiatives [40]. | |
| Stakeholder-Specific Barriers | ||
| Stakeholder | Barriers | Possible approaches to overcome barriers |
| Government and Professional | Scarce resources [37] | Allocating resources to support IPE research and initiatives, develop sustainable funding models, apply for grants and advocate for IPE at institutional and policy levels [39,41]. |
| Strained stakeholder relationships due to the change in the organisation following IPE implementation in higher education [37] | Having open communication, mutual respect and increasing awareness of the value of interprofessional initiatives on disease management [41]. | |
| Institution | Hierarchical culture [41] | Ensuring equal representation of the relevant disciplines and fostering a culture of respect to navigating professional hierarchy and empowering collaborative decision making [41]. |
| Time constraints [37] | Being flexible in scheduling and incorporating an online aspect to facilitate self-paced learning [41]. | |
| Limited resources [37] | Empowering clinical teams to advocate to obtain resources that can advance practice and improve care [42]. | |
| Ability to develop and deliver IPE within pre-existing curricula considering the different assessment criteria for individual healthcare programmes [37] | Creating clear, specific and measurable objectives and using adult learning theories to incorporate interprofessional knowledge and competencies in problem-based learning opportunities, most of which being pre-existing learning tools and opportunities in different health professions’ curricula [41]. | |
| Individual | Professional silos | Ensuring equal representation of the relevant disciplines and empowering collaborative decision making [41]. |
| Communication challenges | Fostering a culture of respect, advising on lines of communication providers can resort to for support and highlighting ongoing practice challenges to the appropriate channels [42]. | |
| Lack of adequate faculty support and understanding of the need for IPE [37] | Offering educational programmes to collaborating teams, highlighting the expected standards of care and publicising professional and technical support [42]. | |
| Limited professional development opportunities [37] | Providing interprofessional faculty-led training sessions and learning materials [41]. | |
| Lack of reward for staff involved in interprofessional activities [37] | Establish a reward system, such as a percentage increase in basic salary, and assign interprofessional service heroes to advocate for and represent interprofessional initiatives [43]. | |
Enablers for IPE clinical placements in diabetes teams include the presence of preceptors and students from at least two different domains of healthcare, a well-established curriculum on the provision of collaborative care, integration of students from multiple disciplines in diabetes teams, sufficient IPE resources and strong support from healthcare institutions [44].
4. Discussion
Interprofessional Education and Diabetes Management: The Impact
For chronic diseases to be managed more effectively, operative collaborative relationships must be established between healthcare practitioners from different disciplines, which can be achieved through teamwork. This is equally true for the management of diabetes as a disease of complex nature and multisystem involvement, of which prevalence continues to rise [1]. Due to this increasing prevalence, people with diabetes are more often being treated, whether in the inpatient or outpatient settings, by HCPs who are not always adequately trained to provide optimal diabetes care, which causes delays in care provision and suboptimal patient outcomes [21]. Additionally, quality-improvement collaboratives that are well integrated and patient centred are cost effective for large groups of people with diabetes [45]. This calls for developing an effective and efficient collaborative workforce equipped with the skills and knowledge to confidently manage diabetes in a timely manner [21]. At the core of providing effective, efficient healthcare services is IPE as a didactic program adopted to teach HCPs from different disciplines and its practical application, interprofessional collaboration, which describes how service to patients is provided within the multidisciplinary team of HCPs [14,18]. Two main features of IPE and IPC are the subject of recent research. Firstly, the effect of IPE and IPC has been evaluated on different aspects of the providers’ treatments of people with diabetes and other chronic diseases, while the other research parameter is the impact of IPC interventions on patient outcomes. While most studies ascertain an overall positive effect on HCPs’ practice [9,18,23], the extent to which IPE and IPC improve chronic disease outcomes in patients is a question with an answer that is not yet as conclusive but has been studied in many systematic reviews and meta-analyses [7,21]. This review attempts to survey the impact of IPE and IPC on clinical processes and patient outcomes in diabetes treatment and management.
Diabetes self-management (DSM) is a vital aspect of non-pharmacologic diabetes care that, when adequately applied, dramatically impacts the development and progression of diabetes by achieving good glycaemic control, reducing diabetes complications and improving the quality of life in a cost-effective manner [46,47]. Accordingly, the near normalisation of blood glucose is essential to the treatment plan, and extreme fluctuations in it should, ideally, be minimised [47,48]. The face-to-face interaction between diabetes patients and clinicians does not often exceed two hours in a year, while for the rest of the time, patients and/or families are left to care for this complex disease on their own [46]. Despite being effective, engagement and compliance to self-care behaviours are generally low [46]. The way IPE and IPC may positively impact diabetes outcomes could either be through patients becoming more empowered to improve their DSM after being taught the basics of DSM and the available support by IPC teams or by being cared for in centres where IPC is common practice [25,26,32], which, in turn, influences specific patient behaviours that impact diabetes outcomes.
5. Limitations and Future Research Potential
This review is not without limitations. Firstly, the quality of the studies included was not evaluated using a validated evaluation tool. This is mainly due to the different designs of the included studies, which a review of this kind allows to be included. Additionally, the impact of the introduction of an IPE/IPC programme was evaluated for a range of diabetes outcomes, and there are not many studies that corroborate the effect on each particular outcome. Accordingly, generalisations regarding the impact of IPE/IPC on diabetes outcomes should be made within those parameters. Future research should focus on studies with solid designs that evaluate the impact of IPE/IPC on specific diabetes outcomes, which will enable more rigid comparisons and generalisations.
6. IPE and Diabetes Care–Conclusions
The aim of this study is to evaluate the impact of IPE on diabetes management and outcomes. The findings unveil overwhelming evidence indicating that interprofessional approaches advance diabetes care. Interprofessional approaches increase the skills, attitudes and knowledge of healthcare professionals and students and enable them to adopt a better interdependent, collaborative approach to diabetes care that potentially improves patient outcomes. Furthermore, people with diabetes who receive care and education from interprofessional care teams improve their commitment, knowledge and ability to perform diabetes self-management, which also improves outcomes. Measurable effects on patient outcomes, including better HbA1c and glucose levels, have been recorded when IPE is taught and IPC is implemented. With adequate endorsement, funding, multi-level support and thoughtful facilitation, IPE/IPC can positively impact diabetes care in a cost-effective and life-changing manner.
Author Contributions
Writing—original draft preparation, S.S.; Writing—review and editing, K.D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethics approval is not required for this type of publication.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article. No new data is created for this review.
Acknowledgments
The authors would like to acknowledge Niall Winters for his insightful comments and suggestions on the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; Brussels, Belgium. 2021. Available online: https://www.diabetesatlas.org (accessed on 18 June 2022).
- Bommer, C.; Sagalova, V.; Heesemann, E.; Manne-Goehler, J.; Atun, R.; Bärnighausen, T.; Davies, J.; Vollmer, S. Global Economic Burden of Diabetes in Adults: Projections from 2015 to 2030. Diabetes Care 2018, 41, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Health Professions Networks Nursing & Midwifery Human Resources for Health Framework for Action on Interprofessional Education & Collaborative Practice. 2010. Available online: http://www.who.int/hrh/nursing_midwifery/en/ (accessed on 16 December 2020).
- Herring, R.; Pengilley, C.; Hopkins, H.; Tuthill, B.; Patel, N.; Nelson, C.; Currie, A.; Russell-Jones, D.L. Can an interprofessional education tool improve healthcare professional confidence, knowledge and quality of inpatient diabetes care: A pilot study? Diabet. Med. 2013, 30, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Witt Sherman, D.; Flowers, M.; Rodriguez Alfano, A.; Alfonso, F.; De Los Santos, M.; Evans, H.; Gonzalez, A.; Hannan, J.; Harris, N.; Munecas, T.; et al. An Integrative Review of Interprofessional Collaboration in Health Care: Building the Case for University Support and Resources and Faculty Engagement. Healthcare 2020, 8, 418. [Google Scholar] [CrossRef]
- IPEC (Interprofessional Education Collaborative). Core Competencies for Interprofessional Collaborative Practice: 2016 Update. 2016. Available online: https://ipec.memberclicks.net/assets/2016-Update.pdf (accessed on 25 June 2022).
- Nagelkerk, J.; Thompson, M.E.; Bouthillier, M.; Tompkins, A.; Baer, L.J.; Trytko, J.; Booth, A.; Stevens, A.; Groeneveld, K. Improving outcomes in adults with diabetes through an interprofessional collaborative practice program. J. Interprof. Care 2018, 32, 4–13. [Google Scholar] [CrossRef]
- De La Rosa, M.; Pitts, S.; Chen, P.H. An interprofessional collaboration of care to improve clinical outcomes for patients with diabetes. J. Interprof. Care 2020, 34, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Kangas, S.; Rintala, T.M.; Jaatinen, P. An integrative systematic review of interprofessional education on diabetes. J. Interprof. Care 2018, 32, 706–718. [Google Scholar] [CrossRef]
- Reeves, S.; Goldman, J.; Gilbert, J.; Tepper, J.; Silver, I.; Suter, E.; Zwarenstein, M. A scoping review to improve conceptual clarity of interprofessional interventions. J. Interprof. Care 2011, 25, 167–174. [Google Scholar] [CrossRef]
- Reeves, S. An overview of continuing interprofessional education. J. Contin. Educ. Health Prof. 2009, 29, 142–146. [Google Scholar] [CrossRef]
- Guraya, S.Y.; Barr, H. The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis. Kaohsiung J. Med. Sci. 2018, 34, 160–165. [Google Scholar] [CrossRef]
- Zanotti, R.; Sartor, G.; Canova, C. Effectiveness of interprofessional education by on-field training for medical students, with a pre-post design. BMC Med. Educ. 2015, 15, 121. [Google Scholar] [CrossRef]
- Bridges, D.R.; Davidson, R.A.; Odegard, P.S.; Maki, I.V.; Tomkowiak, J. Interprofessional collaboration: Three best practice models of interprofessional education. Med. Educ. Online 2011, 16, 6035. [Google Scholar] [CrossRef] [PubMed]
- Nurchis, M.C.; Sessa, G.; Pascucci, D.; Sassano, M.; Lombi, L.; Damiani, G. Interprofessional Collaboration and Diabetes Management in Primary Care: A Systematic Review and Meta-Analysis of Patient-Reported Outcomes. J. Pers. Med. 2022, 12, 643. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Kangas, S.; Jaatinen, P.; Metso, S.; Paavilainen, E.; Rintala, T.M. Students’ perceptions of interprofessional collaboration on the care of diabetes: A qualitative study. Nurse Educ. Pract. 2021, 53, 103023. [Google Scholar] [CrossRef]
- Pascucci, D.; Sassano, M.; Nurchis, M.C.; Cicconi, M.; Acampora, A.; Park, D.; Morano, C.; Damiani, G. Impact of interprofessional collaboration on chronic disease management: Findings from a systematic review of clinical trial and meta-analysis. Health Policy 2021, 125, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; McCutcheon, L.R.M.; Fazel, M.T.; Cooley, J.H.; Slack, M.K. Assessment of Interprofessional Collaborative Practices and Outcomes in Adults with Diabetes and Hypertension in Primary Care: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2036725. [Google Scholar] [CrossRef] [PubMed]
- Pisano, M.; Mazzola, N.; Block, L.; Ezzo, D.; Lu, C.; Coletti, D.J. An interprofessional experience in diabetes management for pharmacy and medical students. Curr. Pharm. Teach. Learn. 2020, 12, 459–464. [Google Scholar] [CrossRef]
- Atsalos, C.; Payk, M.; O’Neill, A.; Inglis, S.; Cheung, N.W.; Jackson, D. Meeting the challenges posed by an escalating diabetes healthcare burden: A mixed methods study. Contemp. Nurse 2019, 55, 469–485. [Google Scholar] [CrossRef]
- Levengood, T.W.; Peng, Y.; Xiong, K.Z.; Song, Z.; Elder, R.; Ali, M.K.; Chin, M.H.; Allweiss, P.; Hunter, C.M.; Becenti, A.; et al. Team-Based Care to Improve Diabetes Management: A Community Guide Meta-analysis. Am. J. Prev. Med. 2019, 57, e17–e26. [Google Scholar] [CrossRef]
- Riskiyana, R.; Claramita, M.; Rahayu, G.R. Objectively measured interprofessional education outcome and factors that enhance program effectiveness: A systematic review. Nurse Educ. Today 2018, 66, 73–78. [Google Scholar] [CrossRef]
- Račić, M.; Joksimović, B.N.; Cicmil, S.; Kusmuk, S.; Ivković, N.; Hadživuković, N.; Kulić, M.; Mijović, B.; Mirić, M.; Joksimović, V.R.; et al. The effects of interprofessional diabetes education on the knowledge of medical, dentistry and nursing students. Acta Med. Acad 2017, 46, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Sapsed, S. Diabetes foot complication: Assessing primary and secondary outcomes of multidisciplinary team versus standard care (a systematic review). Int. J. Diabetes Dev. Ctries. 2017, 37, 129–136. [Google Scholar] [CrossRef]
- Ching, D.L.; Forte, D.; Aitchison, L.; Earle, K. Is An Inter-Professional Education Programme Effective in Promoting Collaboration and Improving Diabetes Care? Article Points. Diabetes Prim. Care 2015, 17, 132–137. Available online: https://www.pcdsociety.org/resources/details/is-an-inter-professional-education-programme-effective-in-promoting-collaboration-and-improving-diabetes-care (accessed on 28 June 2022).
- Yamani, N.; Asgarimoqadam, M.; Haghani, F.; Alavijeh, A.Q. The effect of interprofessional education on interprofessional performance and diabetes care knowledge of health care teams at the level one of health service providing. Adv. Biomed. Res. 2014, 3, 153. [Google Scholar] [CrossRef]
- Pittenger, A.L.; Westberg, S.; Rowan, M.; Schweiss, S. An Interprofessional Diabetes Experience to Improve Pharmacy and Nursing Students’ Competency in Collaborative Practice. Am. J. Pharm. Educ. 2013, 77, 197. [Google Scholar] [CrossRef]
- Reeves, S.; Perrier, L.; Goldman, J.; Freeth, D.; Zwarenstein, M. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Pimouguet, C.; Le Goff, M.; Thiebaut, R.; Dartigues, J.F.; Helmer, C. Effectiveness of disease-management programs for improving diabetes care: A meta-analysis. Can. Med. Assoc. J. 2011, 183, E115–E127. [Google Scholar] [CrossRef]
- Hammick, M.; Freeth, D.; Koppel, I.; Reeves, S.; Barr, H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med. Teach. 2009, 29, 735–751. [Google Scholar] [CrossRef]
- Janson, S.L.; Cooke, M.; McGrath, K.W.; Kroon, L.; Robinson, S.; Baron, R.B. Improving Chronic Care of Type 2 Diabetes Using Teams of Interprofessional Learners. Acad. Med. 2009, 84, 1540–1548. [Google Scholar] [CrossRef]
- Lapkin, S.; Levett-Jones, T.; Gilligan, C. The effectiveness of interprofessional education in university-based health professional programs: A systematic review. JBI Libr. Syst. Rev. 2011, 9, 1917–1970. [Google Scholar] [CrossRef]
- CAIPE. Interprofessional Education—Today, Yesterday and Tomorrow (Barr, H.) Higher Education Academy, Learning & Teaching Support Network for Health Sciences & Practice, Occasional Paper 1—CAIPE. 2002. Available online: https://www.caipe.org/resources/publications/caipe-publications/caipe-2002-interprofessional-education-today-yesterday-tomorrow-barr-h (accessed on 20 June 2022).
- Reeves, S.; Fletcher, S.; Barr, H.; Birch, I.; Boet, S.; Davies, N.; McFadyen, A.; Rivera, J.; Kitto, S. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Med. Teach. 2016, 38, 656–668. [Google Scholar] [CrossRef]
- Andrews, K.L.; Houdek, M.T.; Kiemele, L.J. Wound management of chronic diabetic foot ulcers: From the basics to regenerative medicine. Prosthet. Orthot. Int. 2015, 39, 29–39. [Google Scholar] [CrossRef]
- Lawlis, T.R.; Anson, J.; Greenfield, D. Barriers and enablers that influence sustainable interprofessional education: A literature review. J. Interprof. Care 2014, 28, 305–310. [Google Scholar] [CrossRef]
- Nilsen, P.; Seing, I.; Ericsson, C.; Birken, S.A.; Schildmeijer, K. Characteristics of successful changes in health care organizations: An interview study with physicians, registered nurses and assistant nurses. BMC Health Serv. Res. 2020, 20, 147. [Google Scholar] [CrossRef]
- Drejeris, R.; Drejeriene, E. Novel Approach to the Actions for Causes Elimination of Staff Resistance to Innovative Change. J. Multidiscip. Healthc. 2022, 15, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Zwarenstein, M.; Reeves, S. Knowledge translation and interprofessional collaboration: Where the rubber of evidence-based care hits the road of teamwork. J. Contin. Educ. Health Prof. 2006, 26, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Schapmire, T.J.; Head, B.A.; Nash, W.A.; Yankeelov, P.A.; Furman, C.D.; Wright, R.B.; Gopalraj, R.; Gordon, B.; Black, K.P.; Jones, C.; et al. Overcoming barriers to interprofessional education in gerontology: The Interprofessional Curriculum for the Care of Older Adults. Adv. Med. Educ. Pract. 2018, 9, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Pichardo-Lowden, A.; Farbaniec, M.; Haidet, P. Overcoming barriers to diabetes care in the hospital: The power of qualitative observations to promote positive change. J. Eval. Clin. Pract. 2019, 25, 448. [Google Scholar] [CrossRef] [PubMed]
- Mladenovic, J.; Tilden, V.P. Strategies for overcoming barriers to IPE at a health sciences university. J. Interprof. Educ. Pract. 2017, 8, 10–13. [Google Scholar] [CrossRef]
- Dean, H.J.; MacDonald, L.; Alessi-Severini, S.; Halipchuk, J.A.C.; Sellers, E.A.C.; Grymonpre, R.E. Elements and Enablers for Interprofessional Education Clinical Placements in Diabetes Teams. Can. J. Diabetes 2014, 38, 273–278. [Google Scholar] [CrossRef]
- Schouten, L.M.T.; Niessen, L.W.; van de Pas, J.W.A.M.; Grol, R.P.T.M.; Hulscher, M.E.J.L. Cost-effectiveness of a quality improvement collaborative focusing on patients with diabetes. Med. Care 2010, 48, 884–891. [Google Scholar] [CrossRef]
- American Diabetes Association. 4. Lifestyle Management: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018, 41 (Suppl. 1), S38–S50. [Google Scholar] [CrossRef]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Role of self-care in management of diabetes mellitus. J. Diabetes Metab. Disord. 2013, 12, 14. [Google Scholar] [CrossRef]
- Choudhary, P.; Genovese, S.; Reach, G. Blood Glucose Pattern Management in Diabetes: Creating Order from Disorder. J. Diabetes Sci. Technol. 2013, 7, 1575–1584. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).