Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology?
Abstract
1. Introduction
2. What May Happen to People with LHs
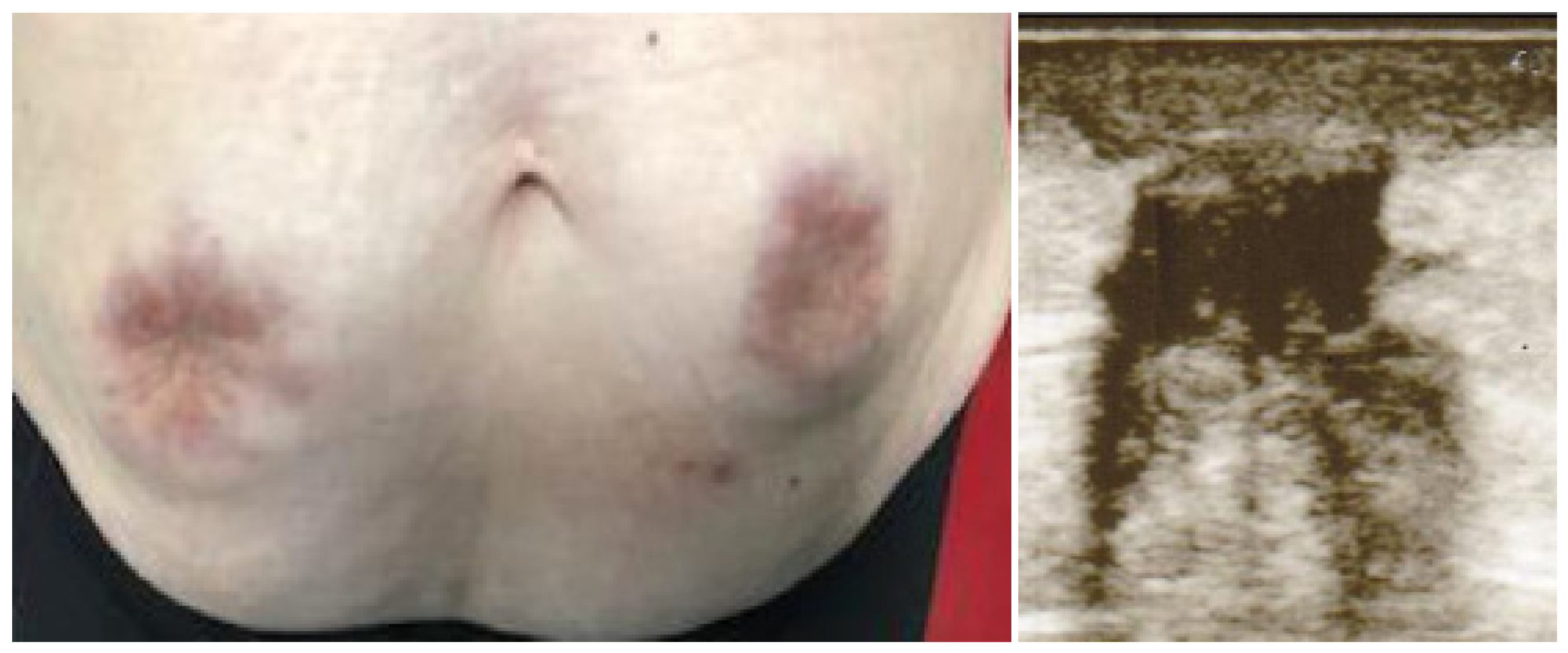
3. A Case of Monster LH
4. Practical Considerations
5. Why Do People with Diabetes Forget the Lessons over Time?
6. What Are the Consequences of Injection Technique Errors?
7. What Can We Do to Prevent Lipohypertrophies?
8. A Proposal for the Future
9. Key Summary Points
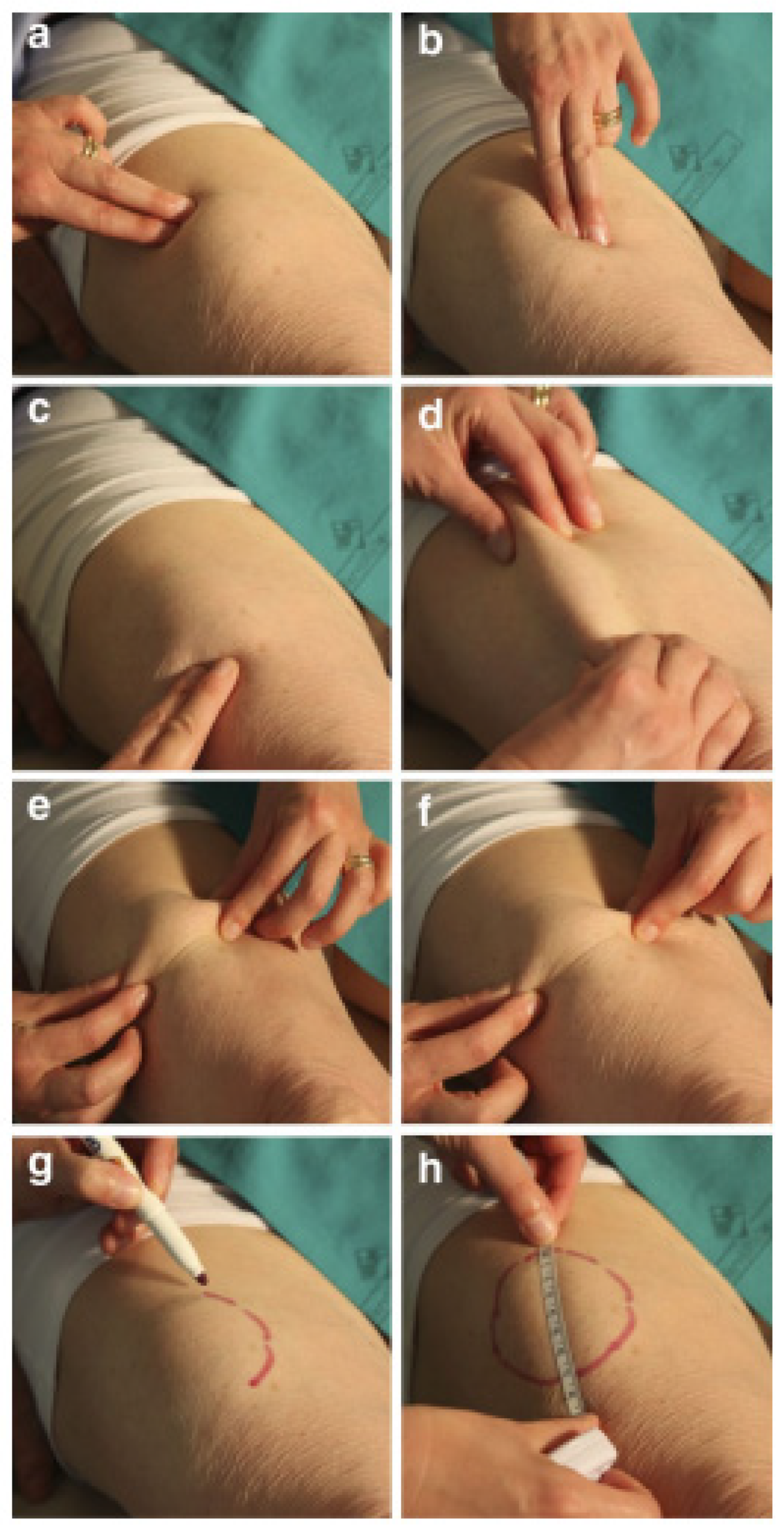
- Improper Insulin injection causes skin lipohypertrophic lesions (LHs), which are often flat and barely visible, thus requiring thorough deep palpation examination and ultrasonography (US) for identification;
- The detection of LHs is crucial to prevent poor diabetes control due to unpredictable insulin-release patterns;
- The skin undergoes fundamental structural changes with aging, potentially increasing the risk of developing LHs;
- Too many healthcare professionals (doctors and nurses) know little or nothing about lipohypertrophy and its associated metabolic consequences and, worse, they do not know how to avoid or counteract this type of complication;
- The data from the literature suggest the need (i) to take specific actions to prevent and control the high risk of acute hypoglycemia-related cardiovascular events, especially in older subjects, and (ii) to identify specific, better-targeted, practical, and structured educational programs suited to older patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Strollo, F. Role of Structured Education in Reducing Lypodistrophy and its Metabolic Complications in Insulin-Treated People with Type 2 Diabetes: A Randomized Multicenter Case–Control Study. Diabetes Ther. 2021, 12, 1379–1398. [Google Scholar] [CrossRef] [PubMed]
- Blanco, M.; Hernández, M.; Strauss, K.; Amaya, M. Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013, 39, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Guarino, G.; Giancaterini, A.; Guida, P.; Strollo, F.; AMD-OSDI Italian Injection Technique Study Group. A suitable palpation technique allows to identify skin lipohypertrophic lesions in insulin-treated people with diabetes. SpringerPlus 2016, 5, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Agrusta, M.; Guarino, G.; Carbone, L.; Cavallaro, V.; Carucci, I.; Strollo, F. Metabolic consequences of incorrect insulin administration techniques in aging subjects with diabetes. Geol. Rundsch. 2010, 48, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Famulla, S.; Hövelmann, U.; Fischer, A.; Coester, H.-V.; Hermanski, L.; Kaltheuner, M.; Kaltheuner, L.; Heinemann, L.; Heise, T.; Hirsch, L. Insulin Injection Into Lipohypertrophic Tissue: Blunted and More Variable Insulin Absorption and Action and Impaired Postprandial Glucose Control. Diabetes Care 2016, 39, 1486–1492. [Google Scholar] [CrossRef] [PubMed]
- Improta, M.; Strollo, F.; Gentile, S.; AMD-OSDI Study Group on Injection Technique. Lessons learned from an unusual case of severe hypoglycemia. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 1237–1239. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Guarino, G.; Strollo, F. How to treat improper insulin injection-related lipohypertrophy: A 3-year follow-up of a monster case and an update on treatment. Diabetes Res. Clin. Pract. 2020, 171, 108534. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Giordano, L.; Loiacono, F.; et al. The Durability of an Intensive, Structured Education-Based Rehabilitation Protocol for Best Insulin Injection Practice: The ISTERP-2 Study. Diabetes Ther. 2021, 12, 2557–2569. [Google Scholar] [CrossRef] [PubMed]
- Nusca, A.; Tuccinardi, D.; Albano, M.; Cavallaro, C.; Ricottini, E.; Manfrini, S.; Pozzilli, P.; Di Sciascio, G. Glycemic variability in the development of cardiovascular complications in diabetes. Diabetes/Metabolism Res. Rev. 2018, 34, e3047. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Strollo, F. Cost saving effects of a short-term educational intervention entailing lower hypoglycaemic event rates in people with type 1 diabetes and lipo-hypertrophy. Diabetes Res. Clin. Pr. 2018, 143, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Fusco, A.; Corigliano, G.; Colarusso, S.; Piscopo, M.; Improta, M.R.; Corigliano, M.; et al. Lipohypertrophy in Elderly Insulin-Treated Patients With Type 2 Diabetes. Diabetes Ther. 2020, 12, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhao, F.; Zhang, M.; Yuan, L.; Zheng, Y.; Huang, J.; Li, Y.; Li, C. Insulin Injection Knowledge, Attitudes, and Practices of Nurses in China: A Cross-Sectional Nationwide Study. Diabetes Ther. 2021, 12, 2451–2469. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, S.; Poudel, R.S.; Rajbanshi, L.; Shrestha, S. Assessment of Insulin Injection Practice of Nurses Working in a Tertiary Healthcare Center of Nepal. Nurs. Res. Pract. 2018, 2018, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Mushta, A.M. Study of insulin injection technique amongst the nursing staff. Pak. J. Med. Sci. 2006, 22, 310–312. [Google Scholar]
- Yacoub, M.; Demeh, W.; Darawad, M.; Barr, J.; Saleh, A.; Saleh, M. An assessment of diabetes-related knowledge among registered nurses working in hospitals in Jordan. Int. Nurs. Rev. 2014, 61, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Theofanidis, D. In-Hospital Administration of Insulin by Nurses in Northern Greece: An Observational Study. Diabetes Spectr. 2017, 30, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Robb, A.; Reid, B.; A Laird, E. Insulin knowledge and practice: A survey of district nurses in Northern Ireland. Br. J. Community Nurs. 2017, 22, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Derr, R.L.; Sivanandy, M.S.; Bronich-Hall, L.; Rodriguez, A. Insulin-related knowledge among health care professionals in inter-nal medicine. Diabetes Spectr. 2007, 20, 177–185. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strollo, F.; Satta, E.; Gentile, S. Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology? Diabetology 2022, 3, 615-619. https://doi.org/10.3390/diabetology3040047
Strollo F, Satta E, Gentile S. Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology? Diabetology. 2022; 3(4):615-619. https://doi.org/10.3390/diabetology3040047
Chicago/Turabian StyleStrollo, Felice, Ersilia Satta, and Sandro Gentile. 2022. "Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology?" Diabetology 3, no. 4: 615-619. https://doi.org/10.3390/diabetology3040047
APA StyleStrollo, F., Satta, E., & Gentile, S. (2022). Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology? Diabetology, 3(4), 615-619. https://doi.org/10.3390/diabetology3040047







