Evaluation of Tribulus terrestris Extracts Relative to Metformin on Oxidative Stress and Histopathology of the Liver for Diabetic Male Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Preparation of Tribulus terrestris Aqueous Extract
2.3. Phytochemical Screening of the Extract
2.4. Preparation of Metformin Drug (MET)
2.5. Animals Care
2.6. Induction of Diabetes Mellitus by Streptozotocin
2.7. Experimental Design
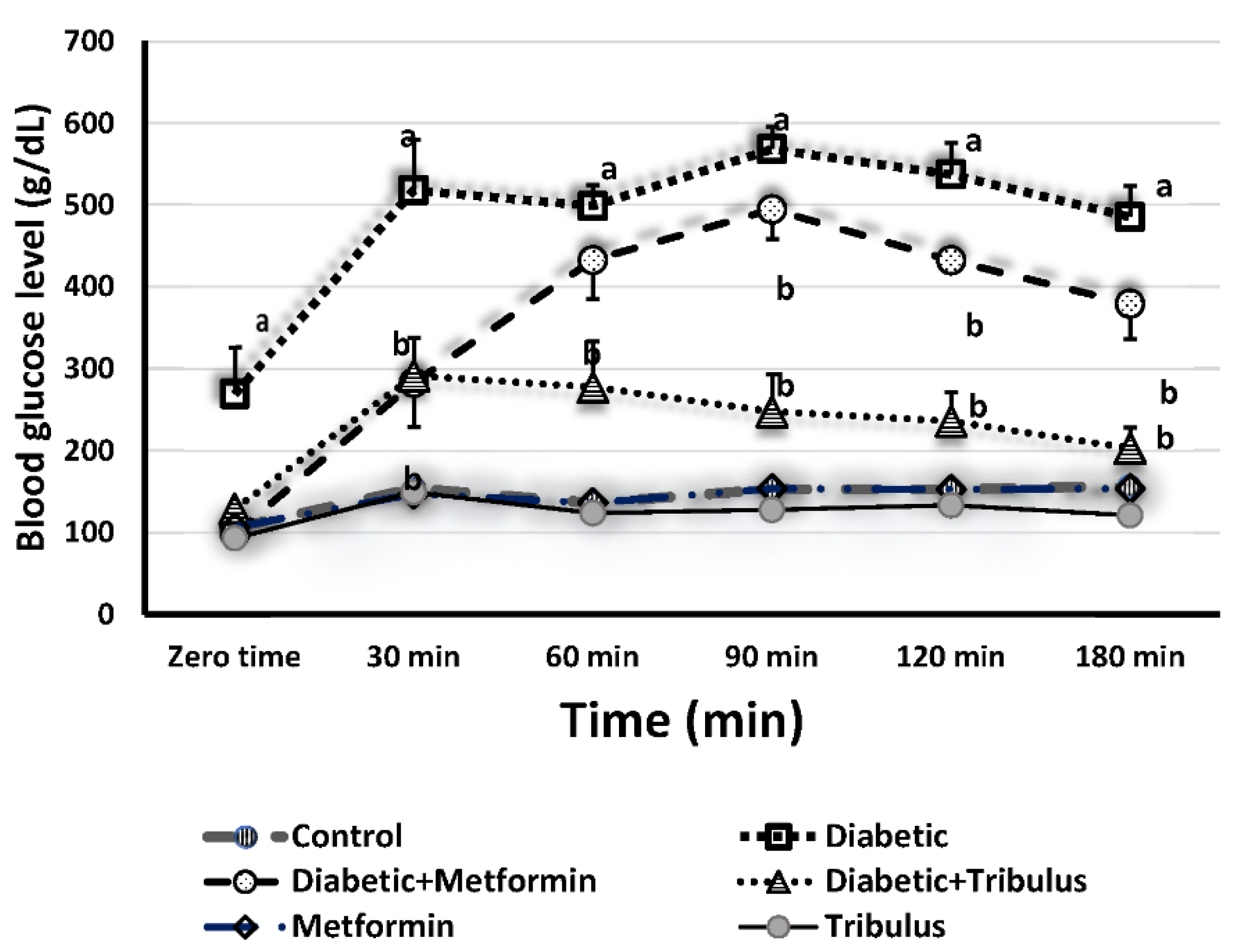
2.8. Glucose Tolerance Test
2.9. Preparation of Liver Homogenate for Measuring the Oxidative/Antioxidant Parameters
2.10. Determination of Oxidative/Antioxidant Parameters
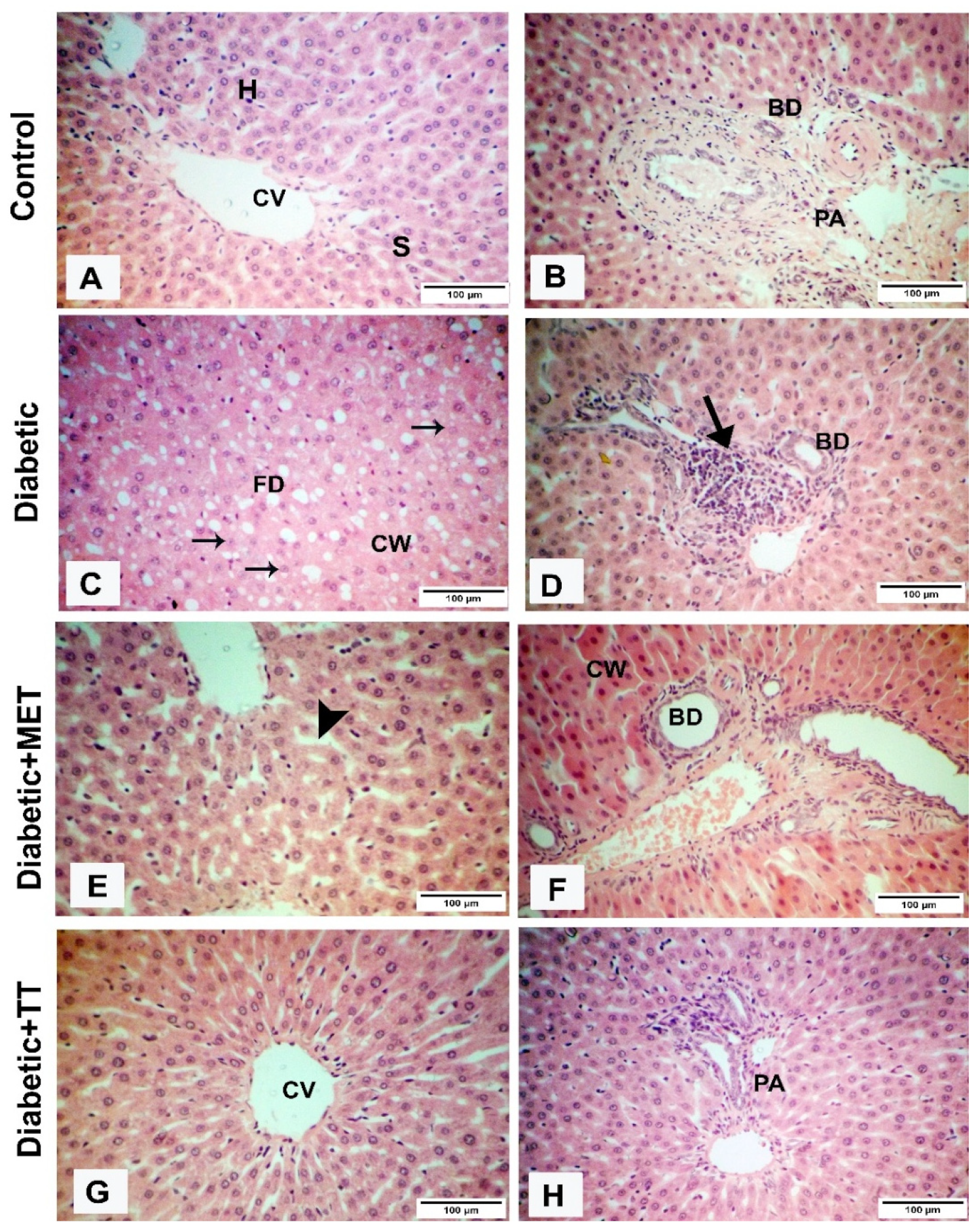
2.11. Histological Evaluation
2.12. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation (IDF). IDF Diabetes; International Diabetes Federation: Brussels, Belgium, 2013. [Google Scholar]
- Hunt, J.V.; Smith, C.C.; Wolff, S.P. Autoxidative glycosylation and possible involvement of peroxides and free radicals in LDL modification by glucose. Diabetes 1990, 39, 1420–1424. [Google Scholar] [CrossRef] [PubMed]
- Mansour, H.A.; Newairy, A.S.; Yousef, M.I.; Sheweita, S.A. Biochemical study on the effects of some Egyptian herbs in alloxan-induced diabetic rats. Toxicology 2002, 170, 221–228. [Google Scholar] [CrossRef]
- Maritim, A.C.; Sanders, A.; Watkins, J.B., III. Diabetes, oxidative stress, and antioxidants: A review. J. Biochem. Mol. Toxicol. 2003, 17, 24–38. [Google Scholar] [CrossRef]
- El-Shenawy, N.S.; Refat, M.S.; Fakihi, F.H. Decreasing the diabetic complication by vanadyl(VO)2+/vitamin B 6 complex in alloxan-induced diabetic mice. J. Mater. Sci. Mater. Med. 2013, 24, 911–930. [Google Scholar] [CrossRef]
- El-Said, S.M.; Al-Barak, A.S. Extraction of insulin like compounds from bitter melon plants. Am. J. Drug Discov. Dev. 2011, 1, 1–7. [Google Scholar] [CrossRef]
- Loizzo, M.R.; Rashed, K.; Said, A.; Bonesi, M.; Menichini, F.; Tundis, R. Antiproliferative and antioxidant properties of Alhagi maurorum Boiss (Leguminosae) aerial parts. Ind. Crops Prod. 2014, 53, 289–295. [Google Scholar] [CrossRef]
- Sheweita, S.A.; Mashaly, S.; Newairy, A.A.; Abdou, H.M.; Eweda, S.M. Changes in oxidative stress and antioxidant enzyme activities in streptozotocin-induced diabetes mellitus in rats: Role of Alhagi maurorum extracts. Oxidative Med. Cell. Longev. 2016, 2016, 5264064. [Google Scholar] [CrossRef] [PubMed]
- Chhatre, S.; Nesari, T.; Somani, G.; Kanchan, D.; Sathaye, S. Phytopharmacological overview of Tribulus terrestris. Pharmacogn. Rev. 2014, 8, 45–51. [Google Scholar] [CrossRef]
- Mohammed, M.M.; Shaddad, S.A.I.; Mudathir, A.E.; Elsharif, B.A.; Abu Algasem, A.A.E. Effects of Tribulus terrestris ethanolic extract in male rats and cocks fertility. J. Pharm. Biomed. Sci. 2013, 30 (Suppl. 1), S13–S18. [Google Scholar]
- Heidari, M.R.; Mehrabani, M.; Pardakhty, A.; Khazaeli, P.; Zahedi, M.J.; Yakhchali, M.; Vahedian, M. The analgesic effect of Tribulus terrestris extract and comparison of gastric ulcerogenicity of the extract with indomethacin in animal experiments. Ann. N. Y. Acad. Sci. 2007, 1095, 418–427. [Google Scholar] [CrossRef]
- Adaay, M.H.; Mosa, A.R. Evaluation of the effect of aqueous extract of Tribulus terrestris on some reproductive parameters in female mice. J. Mater. Environ. Sci. 2012, 3, 1153–1162. [Google Scholar]
- Tag, H.M.; Abdelazek, H.M.; Mahoud, Y.S.; EL-Shenawy, N.S. Efficacy of Tribulus terrestris extract and metformin on fertility indices and oxidative stress of testicular tissue in streptozotocin-induced diabetic male rats. Afr. J. Pharm. Pharmacol. 2015, 9, 1088–1098. [Google Scholar]
- Li, M.; Qu, W.; Wang, Y.; Wan, H.; Tian, C. Hypoglycemic effect of saponin from Tribulus terrestris. Zhong Yao cai = Zhongyaocai = J. Chin. Med. Mater. 2002, 25, 420–422. [Google Scholar]
- Amin, A.M.; Lotfy, M.; Shafiullah, M.; Adeghate, E. The protective effect of Tribulus terrestris in diabetes. Ann. N. Y. Acad. Sci. 2006, 1084, 391–401. [Google Scholar] [CrossRef]
- Kamboj, P.; Aggarwal, M.; Puri, S.; Singla, S.K. Effect of aqueous extract of Tribulus terrestris on oxalate-induced oxidative stress in rats. Indian J. Nephrol. 2011, 21, 154–159. [Google Scholar]
- Rahmathulla, S.M.; Maruthi, E.; Bheemewsaraiah, K.; Manjunatha, S.; Devi, K.L. Effect of Tribulus terrestris (L.) on liver in ISO-induced myocardial infarction. Int. J. Res. Biochem. Biophys. 2012, 2, 10–12. [Google Scholar]
- Yakubu, M.T.; Afolayan, A.J. Effect of aqueous extract of Bulbine natalensis (Baker) stem on the sexual behavior of male rats. Int. J. Androl. 2009, 32, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Linden, M.A.; Lopez, K.T.; Fletcher, J.A.; Morris, E.M.; Meers, G.M.; Siddique, S.; Laughlin, M.H.; Sowers, J.R.; Thyfault, J.P.; Ibdah, J.A.; et al. Combining metformin therapy with caloric restriction for the management of type 2 diabetes and nonalcoholic fatty liver disease in obese rats. Appl. Physiol. Nutr. Metab. 2015, 40, 1038–1047. [Google Scholar] [CrossRef] [PubMed]
- Brownlee, M. A radical explanation for glucose-induced β cell dysfunction. J. Clin. Investig. 2003, 112, 1788–1790. [Google Scholar] [CrossRef]
- Shao, J.; Qiao, L.; Janssen, R.C.; Pagliassotti, M.; Friedman, J.E. Chronic hyperglycemia enhances PEPCK gene expression and hepatocellular glucose production via elevated liver activating protein/liver inhibitory protein ratio. Diabetes 2005, 54, 976–984. [Google Scholar] [CrossRef]
- Raddatz, D.; Ramadori, G. Carbohydrate metabolism and the liver: Actual aspects from physiology and disease. Z. Gastroenterol. 2007, 45, 51–62. [Google Scholar] [CrossRef]
- Eagappan, K.; Sasikumar, S.; Brindha, D. Antioxidant capacity insolvent and cooked extracts of Tribulus Terrestris L Fruit. Int. J. Biol. Pharm. Res. 2015, 6, 63–67. [Google Scholar]
- Costa, A.F. Farmacognosia, 2nd ed.; Fundacao Calouste Gulbenkian: Lisbon, Portugal, 1977; Volume 1–2. [Google Scholar]
- Freireich, E.J.; Gehan, E.A.; Rall, D.; Schmidt, L.H.; Skipper, H.E. Quantitative comparison of toxicity of anticancer agents in mouse, rat, hamster, dog, monkey, and man. Cancer Chemother. Rep. 1966, 50, 219–224. [Google Scholar]
- European Communities (EC). Council Directive 86/609/EEC of 24 November 1986 on the approximation of laws, regulations, and administrative provisions of the Member States regarding the protection of animals used for experimental and other scientific purposes. Off. J. Eur. Communities 1986, L 358, 1–28. [Google Scholar]
- Akbarzadeh, A.; Norouzian, D.; Mehrabi, M.R.; Jamshidi, S.H.; Farhangi, A.; Verdi, A.A.; Mofidian, S.M.; Rad, B.L. Induction of diabetes by streptozotocin in rats. Indian J. Clin. Biochem. 2007, 22, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, O.J.; Omogbai, E.K. Effect of metformin on potassium-adapted and Nonadapted Diabetic Rats. Trop. J. Pharm. Res. 2012, 11, 747–752. [Google Scholar] [CrossRef][Green Version]
- Gauthaman, K.; Ganesan, A.P. The hormonal effects of Tribulus terrestris and its role in the management of male erectile dysfunction–an evaluation using primates, rabbit, and rat. Phytomedicine 2008, 15, 44–54. [Google Scholar] [CrossRef]
- Islam, M.A.; Akhtar, M.A.; Khan, M.R.; Hossain, M.S.; Alam, A.H.; Ibne-Wahed, M.I.; Amran, M.S.; Rahman, B.M.; Ahmed, M. Oral glucose tolerance test (OGTT) in normal control and glucose induced hyperglycemic rats with Coccinia cordifolia L. and Catharanthus roseus L. Pak. J. Pharm. Sci. 2009, 22, 402–404. [Google Scholar] [PubMed]
- Hamza, R.Z.; Ismail, H.A.; Khaled, H.E.; El-Shenawy, N.S. Antioxidant effect of L-cysteine on sodium-valproate-induced oxidative stress in rat liver: Biochemical and ultrastructural approaches. Toxicol. Environ. Chem. 2015, 97, 1041–1056. [Google Scholar] [CrossRef]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef]
- Aebi, M.; Furter, R.; Prand, F.; Niederberger, P.; Hütter, R. Structure and function of the TRP3 gene of Saccharomyces cerevisiae: Analysis of transcription, promoter sequence, and sequence coding for a glutamine amidotransferase. Curr. Genet. 1984, 8, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Ålin, P.; Danielson, U.H.; Mannervik, B. 4-Hydroxyalk-2-enals are substrates for glutathione transferase. FEBS Lett. 1985, 179, 267–270. [Google Scholar] [CrossRef]
- Beutler, E.; Duron, O.; Kelly, B.M. Improved method for the determination of blood glutathione. J. Lab. Clin. Med. 1963, 61, 882–888. [Google Scholar] [PubMed]
- Bancroft, J.D.; Gamble, M. (Eds.) Theory and Practice of Histological Techniques, 6th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Thoolen, B.; Maronpot, R.R.; Harada, T.; Nyska, A.; Rousseaux, C.; Nolte, T.; Malarkey, D.E.; Kaufmann, W.; Küttler, K.; Deschl, U.; et al. Proliferative and nonproliferative lesions of the rat and mouse hepatobiliary system. Toxicol. Pathol. 2010, 38 (Suppl. 7), S5–S81. [Google Scholar] [CrossRef] [PubMed]
- Filed, A.P. Discovering Statistics Using SPSS for Windows: Advanced Techniques for the Beginner; Sage publications: London, UK, 2000. [Google Scholar]
- Matough, F.A.; Budin, S.B.; Hamid, Z.A.; Alwahaibi, N.; Mohamed, J. The role of oxidative stress and antioxidants in diabetic complications. Sultan Qaboos Univ. Med. J. 2012, 12, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Rahman, K. Studies on free radicals, antioxidants, and co-factors. Clin. Interv. Aging 2007, 2, 219–236. [Google Scholar]
- Wolf, S.P. Diabetes mellitus and free radicals. Br. Med. Bull. 1993, 49, 642–652. [Google Scholar] [CrossRef]
- Afshari, A.T.; Shirpoor, A.; Farshid, A.; Saadatian, R.; Rasmi, Y.; Saboory, E.; Ilkhanizadeh, B.; Allameh, A. The effect of ginger on diabetic nephropathy, plasma antioxidant capacity, and lipid peroxidation in rats. Food Chem. 2007, 101, 148–153. [Google Scholar] [CrossRef]
- Takemoto, K.; Tanaka, M.; Iwata, H.; Nishihara, R.; Ishihara, K.; Wang, D.H.; Ogino, K.; Taniuchi, K.; Masuoka, N. Low catalase activity in blood is associated with the diabetes caused by alloxan. Clin. Chim. Acta 2009, 407, 43–46. [Google Scholar] [CrossRef]
- Lapshina, E.A.; Sudnikovich, E.J.; Maksimchik, J.Z.; Zabrodskaya, S.V.; Zavodnik, L.B.; Kubyshin, V.L.; Nocun, M.; Kazmierczak, P.; Dobaczewski, M.; Watala, C.; et al. Antioxidative enzyme and glutathione S-transferase activities in diabetic rats exposed to long-term ASA treatment. Life Sci. 2006, 79, 1804–1811. [Google Scholar] [CrossRef]
- Li, S.; Tan, H.Y.; Wang, N.; Zhang, Z.J.; Lao, L.; Wong, C.W.; Feng, Y. The role of oxidative stress and antioxidants in liver diseases. Int. J. Mol. Sci. 2015, 16, 26087–260124. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, B.K.; Pandey, K.B.; Abidi, A.B.; Rizvi, S.I. Markers of oxidative stress during diabetes mellitus. J. Biomark. 2013, 2013, 378790. [Google Scholar] [CrossRef] [PubMed]
- Shaker, E.; Mahmoud, H.; Mnaa, S. Anti-inflammatory and anti-ulcer activity of the extract from Alhagi maurorum (camelthorn). Food Chem. Toxicol. 2010, 48, 2785–2790. [Google Scholar] [CrossRef] [PubMed]
- Ștefănescu, R.; Farczadi, L.; Huțanu, A.; Ősz, B.E.; Mărușteri, M.; Negroiu, A.; Vari, C.E. Tribulus terrestris efficacy and safety concerns in diabetes and erectile dysfunction, assessed in an experimental model. Plants 2021, 10, 744. [Google Scholar] [CrossRef] [PubMed]

| Groups | MDA (µM/g) | CAT Activity (µM/min/g) | GST (µM/g) | GSH (mM/g) |
|---|---|---|---|---|
| Control | 87.40 ± 3.12 | 43.39 ± 5.81 | 34.98 ± 1.97 | 49.21 ± 4.89 |
| MET | 42.80 ± 10.23 a | 42.89 ± 5.55 | 33.88 ± 3.22 | 51.72 ± 3.28 |
| TT extract | 31.00 ± 7.18 a | 51.33 ± 2.53 | 32.61 ± 3.00 | 61.79 ± 3.39 |
| Diabetic | 184.20 ± 12.22 a | 12.80 ± 0.54 a | 22.03 ± 0.82 a | 29.26 ± 1.90 a |
| Diabetic and MET | 86.20 ± 2.65 b | 24.37 ± 1.23 b | 29.05 ± 0.57 b | 44.01 ± 1.23 b |
| Diabetic and TT | 61.20 ± 4.74 b,c | 32.53 ± 2.62 b,c | 29.85 ± 0.88 b | 50.50 ± 1.58 b,c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Eisa, R.A.; Tag, H.M.; ElNaggar, M.S.; Abdelrazek, H.M.A.; El-Shenawy, N.S. Evaluation of Tribulus terrestris Extracts Relative to Metformin on Oxidative Stress and Histopathology of the Liver for Diabetic Male Rats. Diabetology 2022, 3, 46-55. https://doi.org/10.3390/diabetology3010004
Al-Eisa RA, Tag HM, ElNaggar MS, Abdelrazek HMA, El-Shenawy NS. Evaluation of Tribulus terrestris Extracts Relative to Metformin on Oxidative Stress and Histopathology of the Liver for Diabetic Male Rats. Diabetology. 2022; 3(1):46-55. https://doi.org/10.3390/diabetology3010004
Chicago/Turabian StyleAl-Eisa, Rasha A., Hend M. Tag, Mohamed Salah ElNaggar, Heba M. A. Abdelrazek, and Nahla S. El-Shenawy. 2022. "Evaluation of Tribulus terrestris Extracts Relative to Metformin on Oxidative Stress and Histopathology of the Liver for Diabetic Male Rats" Diabetology 3, no. 1: 46-55. https://doi.org/10.3390/diabetology3010004
APA StyleAl-Eisa, R. A., Tag, H. M., ElNaggar, M. S., Abdelrazek, H. M. A., & El-Shenawy, N. S. (2022). Evaluation of Tribulus terrestris Extracts Relative to Metformin on Oxidative Stress and Histopathology of the Liver for Diabetic Male Rats. Diabetology, 3(1), 46-55. https://doi.org/10.3390/diabetology3010004







