Abstract
Men of all ages frequently experience erectile dysfunction (ED) or impotence, and it is a difficult health issue that adversely affects the quality of life of those who experience it. There are multiple types of treatment strategies for ED available, depending on the origin and severity of ED, as well as any underlying medical issues. However, these therapeutics are known to have a number of negative health effects. In contrast, plant-based treatments are more effective for managing diseases due to their ability to modulate biological processes like inflammation, oxidative stress, and cell signaling molecules. Many medicinal plants have been reported to be quite helpful in the improvement of ED. In this review, ED and its causes, diagnostic methods, treatment strategies, and some of the most potent plant-based interventions against ED are discussed in greater detail, along with a description of their mechanisms of action and a brief discussion of approaches to increase their efficacy, with a focus on the management of ED using herbal interventions as complementary and alternative medicines. While there is hope that medicinal plants could provide lead substances for erectile dysfunction medications, additional investigation is necessary to ascertain the efficacy and security of these prospective treatments.
1. Introduction
Erectile dysfunction (ED) is defined as the consistent inability to attain or maintain sufficient penile erection for satisfactory sexual intercourse. This can negatively impact the quality of life (QoL) [1] of those who suffer from it, encompassing areas such as social and family life, mental health and confidence, and overall health [2]. In addition, ED has a detrimental effect on the female partners of ED-afflicted men as well, leading to relationship problems and lower relationship satisfaction [3]. QoL is measured by aspects of social interactions and contacts, mobility, self-care, physical activity level, social role functioning in relation to work and family, mental health and well-being, psychological distress, and psychiatric disorders [4].
Men of all ages (range 21–75 years) experience erectile dysfunction or impotence, and it is a difficult condition [1,5]. An erection is the result of the release of nitric oxide (NO) from non-adrenergic, noncholinergic (NANC) nerve fibers during sexual stimulation. The release of NO facilitates the production of 3’,5’-cyclic guamosine monophosphate (cGMP), leading to the activation of protein kinase. Simultaneously, intracellular Ca2+ levels decrease, and relaxation of smooth muscle cells occurs. Blood can fill the lacunar spaces in the corpora cavernosa as the smooth muscle relaxes, compressing the subtunical venules and obstructing the venous outflow (veno-occlusion). Phosphodiesterase type 5 (PDE5) hydrolyzes cGMP and reverses the process. Thus, any disruption to any of these processes may disturb penile erection and result in erectile dysfunction [1]. It has been reported that phosphodiesterase type 5 (PDE-5) is able to activate guanylate cyclase. In turn, guanylate cyclase catalyses the conversion of guanosine triphosphate (GTP) into cyclic guanosine monophosphate (cGMP) and enhances the flow of blood across the penis. However, phosphodiesterase-5 breaks down cGMP to 5′-GMP. PDE-5 inhibitors competitively bind to PDE-5 and inhibit the hydrolysis of cGMP, amplifying the effects of NO [6].
Various PDE-5 inhibitors have been developed for the treatment of erectile dysfunction by diminishing the degradation of cGMP [7]. Many medical conditions have been found to be reliable indicators of major adverse cardiovascular events (MACE) linked with ED [8].
The International Index of Erectile Function (IIEF-5) questionnaire, which consists of five items, is commonly used to categorize erectile dysfunction severity. A score of 1–7 indicates severe, 8–11 moderate, 12–16 mild–moderate, 17–21 mild, and 22–25 no erectile dysfunction [1]. There are notable variations between men with ED and those without it in terms of age, nationality, occupation, education level, number of children, and income satisfaction. Exercise has a substantial correlation with erectile dysfunction. The prevalence of erectile dysfunction was lower in smokers than in non-smokers. An increased incidence of erectile dysfunction has been noticed among men consuming liquor. Individuals with obesity and specific chronic disorders, such as diabetes mellitus, hypertension, hypercholesterolemia, and coronary artery disease, had a much higher prevalence of erectile dysfunction than healthy males [9].
It is clear that an increasing proportion of men suffer from erectile dysfunction, which severely lowers their quality of life. Addressing ED risk factors through lifestyle change, diagnosis of ED in conjunction with medical and surgical therapy, and management by herbal plants may lessen the physical and psychological effects of ED. The current review aims to briefly discuss ED, summarize the causes and risk factors of ED based on in vivo or clinical studies, and elucidate the underlying mechanisms of this disease. In addition, this review briefly outlines the diagnosis and treatment approaches, detailing plants that are conventionally advised for male ED. This review is divided into different sections, including introduction, causes and risk factors of ED, diagnosis of ED, and brief highlights of treatment strategies for ED, with a detailed list of plants used for ED management. Additionally, the mechanisms of plants against ED, along with a few approaches to increase the efficacy of these plants, are provided. Moreover, optimal patient selection, dosage regimen, formulation, and future research for plant-based therapy, along with the perspectives and novelty of the current study are also discussed.
2. Causes of Erectile Dysfunction
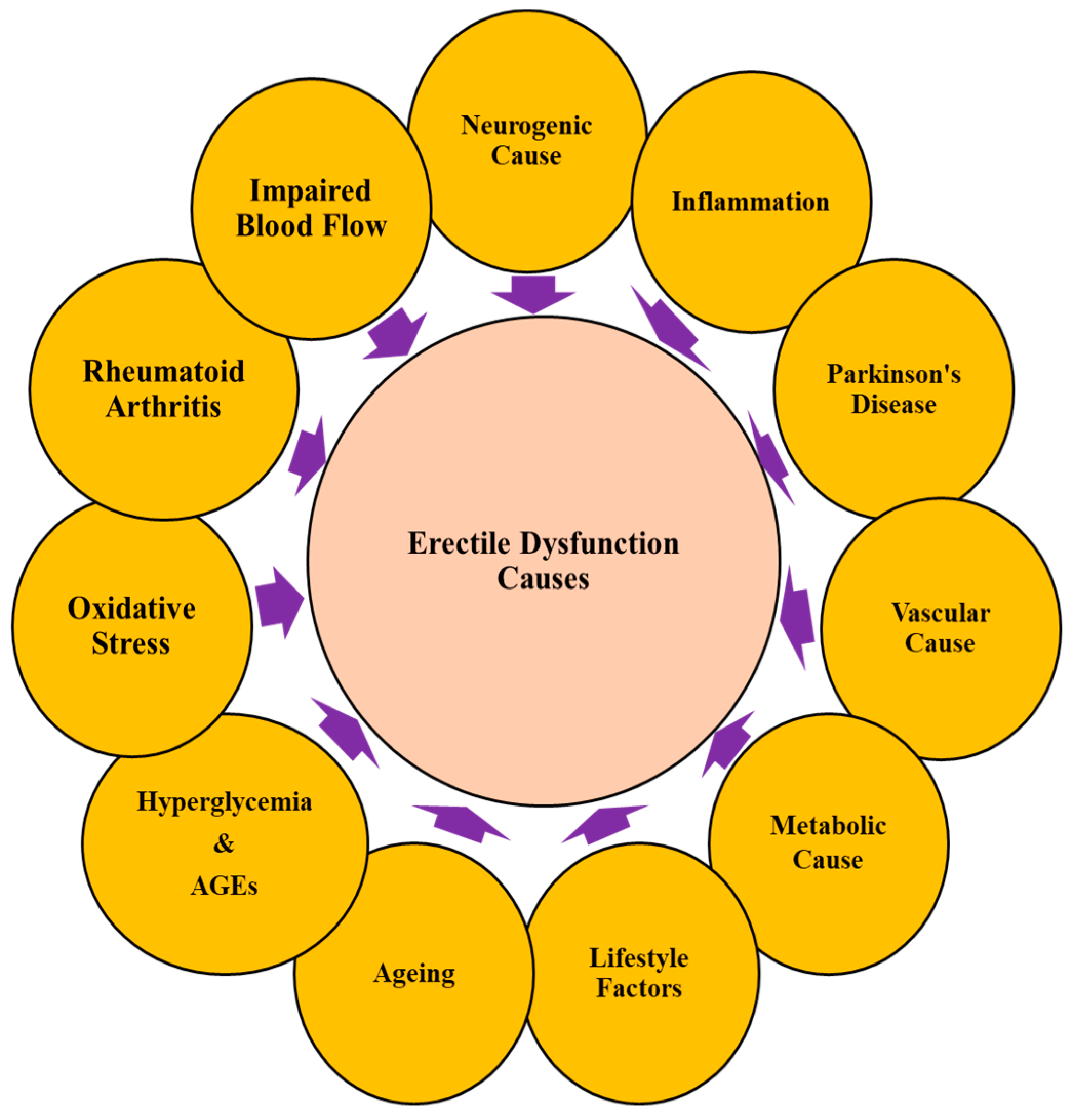
Numerous psychogenic, neurogenic, vascular, and drug-induced factors, or a combination of these factors, can affect erection in males. In addition, alcohol abuse, fatherhood, decreased partner sexual interest, severe impairment in erection during intercourse or during masturbation, decreased penile blood flow, insufficient fasting glucose, elevated triglycerides, and obesity have been reported to be associated with ED [1]. In older men, anomalies of the penile arteries, veins, or both can cause ED. Arteriosclerosis, obesity, inactivity, elevated blood pressure, high cholesterol, smoking, and arteriosclerosis are some modifiable risk factors for erectile dysfunction [10]. The causes of ED could be multifactorial; the sexual performance of males is affected by several factors, as shown in Figure 1.
Figure 1.
Risk factors causing erectile dysfunction. Multiple causes are responsible for the sexual performance of a man.
2.1. Ageing
Age is one of the main risk factors for ED. ED has been reported to be linked to obesity, hypertension, diabetes mellitus (DM), and hyperlipidemia. These conditions are known to be common in older people. Therefore, ED is commonly observed in the elderly [11]. The prevalence and severity of ED have been reported to be obviously rising with age in all epidemiologic research. The Massachusetts Male Ageing Study reported that the overall chance of full ED tripled from 5% in men aged 40 to 15% in men aged 70 [12]. The European Male Ageing Study (EMAS) confirmed that the prevalence of ED increases in older people [13].
2.2. Psychological Causes
Various physiological events, including the emotions involved in sexual excitation, are largely initiated by the brain. Further, anxiety, depression, several mental illnesses, stress, relationship issues, inadequate communication, and other issues can significantly affect sexual performance [14,15]. Depression and performance anxiety are among the most common psychogenic ED factors because they can alter erectile processes by raising cortisol levels and activating the nervous system. Furthermore, depression can decrease energy, interest, and libido or desire. Conscious and unconscious factors, such as performance anxiety, work stress, and strained personal relationships, can also affect ED. One of the underlying reasons for erectile dysfunction is performance anxiety, which can interfere with the brain signals that generate and sustain erections [14].
In a study focussing on the urological setting, the diagnosis and treatment of psychogenic erectile dysfunction were studied for 18 consecutive days. The longest sleep erectile episodes were found to last for 11.2 min on average, with an average penile stiffness of 572 g [16].
Recently, the frequency of mental health issues among erectile dysfunction (ED) sufferers was investigated. According to the findings of the study, the psychological condition of patients with ED seemed to be significantly influenced by partner support. Further, over 50% of the ED patients had experienced psychiatric issues throughout their lives [17].
Additionally, a cross-sectional study investigated the prevalence of anxiety and depression in a particular Chinese population. It was found that anxiety and depression were prevalent in ED patients at 38.16% and 64.97%, respectively [18].
2.3. Neurogenic Causes and Parkinson’s Disease (PD)
The inability to establish or maintain a penile erection as a result of neurologic impairment (central or peripheral) is considered to be neurogenic erectile dysfunction [19]. Any damage to the neurological system involved in erections may result in ED. Long-term diabetes affecting nerves, PD, Alzheimer’s disease, strokes, and head injuries can all impact the libido or nerve impulses necessary for erections [1]. Therefore, they can contribute to ED. In addition, patients with spinal cord injuries often face ED [20]. Patients who have had pelvic surgeries, such as radical prostatectomy, cystectomy, or colectomy, may also have ED due to damage to the cavernous nerves responsible for the regulation of erection [21]. The prevalence of neurogenic sexual dysfunction (NSD) among erectile dysfunction (ED) causes ranges from 10% to 19% [22].
An investigation found that men with neurological disabilities are much more likely to experience erectile dysfunction than men without neurological disabilities [19]. Multiple sclerosis [MS] is a common inflammatory autoimmune illness of the CNS, characterized by the demyelination of nerve cells in the brain and spinal cord. The capacity to transmit signals and, hence, sexual performance, capacity for ejaculation, the expression of libido, and orgasmic reactions are interfered with by this damage [23].
The most common mobility disorder is PD. It is a long-lasting neurodegenerative condition with both motor and non-motor symptoms. Patients with PD have altered dopaminergic pathways that control erection and arousal [24]. A multicenter Italian observational study conducted on 200 Parkinson’s disease patients revealed a decrease in libido in 68% of men and 53% of women with PD, leading to diminished sexual life and desire [25].
Parkinsonism and various combinations of cerebellar, autonomic, urinary, and pyramidal dysfunction are linked with multiple system atrophy (MSA), which is a neurodegenerative condition. In addition, MSA affects the brain’s dopaminergic circuits, which control erection. Hence, the majority of individuals with MSA frequently experience ED. Spinal cord injury (SCI) in individuals leads to reflexogenic, psychogenic, and mixed erections. Early erectile dysfunction was observed to be more prevalent in MSA cases than in matched controls [26].
2.4. Vascular Causes
The risk factors for both CVD and ED include age, hypertension, dyslipidemia, smoking, obesity, and diabetes. ED patients are more likely to experience coronary heart disease and stroke than non-ED patients. Additionally, the severity of ED has been considered a predictor of morbidity and mortality for cardiovascular disease. Vascular ED and cardiovascular disease both share the etiology of endothelial dysfunction, and they also have similar risk factors, such as obesity, cigarette use, inactivity, diabetes, hypertension, and hyperlipidemia [27]. In a 14-year prospective analysis, obesity was reported to be a separate risk factor for ED. According to Fillo et al., males with abdominal obesity had an increased risk of developing ED, and this risk increased proportionally to the degree of obesity [28].
The interplay of androgens, chronic inflammation, and cardiovascular risk factors determines endothelial dysfunction and atherosclerosis and contributes to problems with penile and coronary circulation. The size of the penile artery is less than that of the coronary artery. Hence, there is less blood flow to the erectile tissues than to the coronary circulation. The complicated link between endothelial dysfunction and autonomic hyperactivity could also verify the relationship between ED and the development of CVD [29]. The results of a meta-analysis of prospective cohort studies indicated that ED considerably raises the risk of CVD, coronary heart disease, stroke, and all-cause mortality, and that this rise is likely unrelated to traditional cardiovascular risk factors [30].
In a study conducted between 1994 and 2003, men 55 years of age or older were randomly assigned to a placebo group (n = 9457). 47% of these men reported having erectile dysfunction to some extent at the study entrance. After 5 years, 57% of the males who experienced ED who had no erectile dysfunction at the study entrance reported experiencing an episode, and 65% of enrolled males were reported to have ED at 7 years [31].
In a cohort study of the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation) trial participants, 6304 type 2 diabetic males (aged 55 to 88 years) with baseline medical exams were questioned about ED. In this study, baseline ED was reported to be linked with a higher incidence of all CVD events [32].
2.5. Lifestyle Factors
The prevalence of ED is rising globally due to lifestyle disturbances. Smoking, inactivity, poor diets, being overweight or obese, metabolic syndrome, and excessive consumption of alcohol are among the modifiable risk factors for ED.
2.5.1. Smoking
Both direct tobacco use and passive exposure are significant risk factors for ED [33]. A Spanish study indicated that smoking males had 2.5 times more ED as compared with non-smokers [34]. An Italian study showed that smokers had 1.7 times more ED in comparison with non-smokers [35]. According to a recent meta-analysis of four prospective cohort studies and four case-control studies, the overall odds ratio of ED in prospective cohort studies was 1.29 for former smokers. In contrast, it was 1.51 for current smokers when compared to non-smokers [36].
2.5.2. Alcohol Consumption
Prolonged and chronic alcohol consumption is reported to be linked with sexual dysfunction. Heavy drinking is one of the most significant factors in ED. In a study, one hundred male patients with an alcohol dependence syndrome diagnosis were questioned regarding sexual dysfunction. The findings suggested that 72% of this population had experienced erectile dysfunction, low sexual desire, and premature ejaculation [37].
2.5.3. Dietary Factors
A limited intake of red meat, full-fat dairy products, and beverages with high sugars can lower the risk of ED. Whole grains, legumes, vegetables, and fruits can protect against ED [33]. A cohort study showed that the consumption of fruits, vegetables, nuts, legumes, fish, and sources of long-chain (n-3) fats, as well as avoiding red and processed meats, reduced the risk of ED [38].
2.6. Hormonal Disorders and Hypogonadism
The physiology of the erectile organ is significantly impacted by the level of androgens. It has been reported that functional hypogonadism (FH) and erectile dysfunction (ED) are connected to low levels of testosterone. Men with both testosterone (T) insufficiency and erectile dysfunction (ED) are difficult to treat [39]. In a study, the effects of TTh (testosterone therapy) on anthropometric and metabolic parameters were examined in patients with a history of CVD, functional hypogonadism, and erectile dysfunction. It was found that IIEF was increased by 5.4 in hypogonadal men receiving TTh [40].
In a placebo-controlled study, patients with late-onset hypogonadism were treated with Tribulus terrestris vs. a placebo for erectile dysfunction and symptoms of the lower urinary tract. This study confirmed the results of other studies relating to the potent impact of this herbal remedy on boosting testosterone levels and enhancing sexual performance in patients with erectile dysfunction and partial androgen insufficiency [41].
2.7. Metabolic Causes and Hyperglycemia
Numerous theories have been put forth to explain the connection between ED and metabolic causes. ED, as a diagnostic signal for metabolic and cardiovascular diseases, has gained great significance in this research area. Diabetes mellitus (DM) and cardiovascular disease (CVD) are the main indicators of metabolic syndrome (MetS). Further, MetS comprises dyslipidemia, poor glucose tolerance, hypertension (HTN), and central obesity. A cross-sectional study in an Indian population has shown the correlation between ED and metabolic syndrome. The findings showed that MetS or one of its components was implicated in 56.25% of ED patients [42].
For males with diabetes mellitus (DM), erectile dysfunction (ED) is thought to be the most significant type of sexual dysfunction. In addition, those with DM have an approximately 3.5-fold higher prevalence of ED than those without DM [43]. Increased blood glucose levels are linked to vascular problems and endothelial dysfunction. In addition, chronic hyperglycemia increases the level of reactive oxygen species (ROS) and advanced glycation end products (AGEs), which can hasten endothelial dysfunction by reducing NO production and endothelial NO synthase (eNOS) activity. Endothelial integrity is compromised as a result of an imbalance between vasoactive mediators and vasoconstrictors, which alters vascular permeability. This results in reduced vascular and smooth muscle relaxation, which gives rise to clinical ED. Endothelial walls also become more sensitive to vasoconstrictor stimuli and lose their sensitivity to mediators of vasodilation [44]. High-dose tadalafil, a drug used to treat erectile dysfunction, was found to dramatically reduced long-term blood sugar levels in a small group of type 2 diabetic patients [45].
2.8. Advanced Glycation End-Products
Advanced glycation end-products (AGEs) are formed in an irreversible reaction between glucose and proteins, lipids, and nucleic acids via a non-enzymatic glycation pathway [46,47]. AGEs formation contributes to the pathologic cross-linking of collagen, leading to endothelial dysfunction, vascular thickening, and eventually atherosclerosis [48,49,50].
An international five-item erectile function questionnaire was used to identify ED patients using a cross-sectional survey. By assessing skin autofluorescence, the buildup of AGEs on the skin was evaluated noninvasively. Severe ED was reported to be substantially correlated with higher skin AGEs levels and lower levels of antioxidant vitamins. The study further indicated that zeaxanthin might have an influence on ED by lowering tissue AGE levels [51].
2.9. Oxidative Stress
Oxidative stress occurs as a result of an imbalance between prooxidants and antioxidants [52,53]. Previous studies have shown a significant association between levels of reactive oxygen species (ROS) and ED, especially in diabetic animal models [54]. L-carnitine, an antioxidant, and sildenafil have been found to decrease monocyte oxidative activity and the levels of endothelial dysfunction indicators in diabetic individuals with ED [55]. It has also been discovered that Vitamin E improves the therapeutic effect of the PDE-5 inhibitor, supporting the potential use of ROS scavengers in saving erectile function in diabetic patients [56].
It is believed that lipid peroxidation, protein oxidation, DNA oxidation, decreased synthesis, and the bioavailability of nitric oxide (NO) are the main mechanisms of oxidative stress for ED [57]. Exogenous antioxidants, including the vitamins E and C, as well as endogenous antioxidants, such as superoxide dismutase, catalase, glutathione peroxidase, bilirubin, and uric acid, can limit free radical damage and oxidative stress. When increases in oxidants and losses in antioxidants cannot be reversed, the oxidative/antioxidative balance may shift towards oxidative stress [58].
2.10. Inflammation
A cross-sectional study was conducted to evaluate the link between dietary inflammatory potential (DII) and ED using multivariable-adjusted logistic regression models. The results showed a positive correlation between ED and DII, as measured by the DII score [59]. Due to vascular endothelial damage, systemic inflammation and oxidative stress raise the risk of erectile dysfunction (ED). In a prospective, cross-sectional, single-center study, the state of oxidative stress and systemic inflammation in ED was assessed. While multi-inflammatory index-1 (MII-1) and multi-inflammatory index-2 (MII-2) showed effectiveness, the oxidative stress index (OSI) demonstrated diagnostic potential for ED as a sign of oxidative stress [60].
Increases in peripheral blood inflammatory indicators, specifically the neutrophil-to-lymphocyte ratio (NLR), have been demonstrated to cause a reduction in erectile performance. In patients with localized prostate cancer, the NLR does seem to represent a substitute marker for the persistent inflammation that leads to baseline ED [61].
A recent study showed that inflammation-related erectile dysfunction was a result of an altered NO-cGMP-dependent PKG signaling cascade through the upregulation of important cytokines and chemokines (MCP-1). Overall, the downregulation of inflammatory erectile dysfunction was reported to be mediated through the NO-cGMP-PKG-dependent NF-kB signaling cascade, and it was further activated by a mixture of salt intake [62]. In a hypertensive rat model exposed to bisphenol-A, naringin was suggested to control erectile dysfunction by blocking the NOS/cGMP/PKG signaling pathway, apoptosis, and inflammation [63].
2.11. Rheumatic Arthritis
Sexual functioning in people with rheumatoid arthritis (RA) is a neglected area of QoL that is rarely addressed by medical professionals or other healthcare professionals. Various studies have found that between 31% and 76% of arthritic individuals have sexual problems. Sexual dysfunction can be caused by a variety of circumstances, including those connected to diseases and treatments [64]. Men with RA are more likely than men without RA to develop sexual dysfunction, including ED. For instance, research that appeared in the Journal of Rheumatology discovered that more than half of males with RA reported experiencing some sort of sexual dysfunction. Men with RA exhibited a higher prevalence of ED than men without RA (55% vs. 30%), according to a different study published in The Journal of Sexual Medicine [41].
RA is characterized by the progressive deterioration of joints, brought on by persistent synovial inflammation. It has a significant impact on the patient’s social, economic, psychological, and sexual facets of life. It was demonstrated in a study by Gordon et al. that RA can lead to hypogonadism and sexual dysfunction, including impotence and a decline in desire [65]. A cross-sectional study using a computerized questionnaire at a Danish university hospital reported that patients with RA frequently had sexual dysfunction [66].
2.12. Other Causes
Impaired blood flow and penile fractures can also contribute to ED.
2.12.1. Impaired Neuronal Blood Flow
The inability to establish or maintain a penile erection as a result of neurologic impairment is a broad definition of neurogenic erectile dysfunction. Any injury to the central or peripheral nervous system can cause sexual dysfunction. Using the International Index of Erectile Function questionnaire, 326 male patients were assessed for ED. The patients who reported having ED underwent vascular, neurophysiological, and hormonal testing. Men with neurological disabilities are much more likely to experience erectile dysfunction than men without neurological disabilities, especially those with lesions below the S2-S4 region. Since erectile dysfunction is common in males with neurological disorders, it is advised to frequently check sexual performance during both short- and long-term rehabilitation. If sexual dysfunction is detected, it should be addressed in the treatment plan [19].
2.12.2. Penile Fracture
The penis is not a bone; hence, a penile fracture is not really a fracture. However, if the penis becomes twisted or struck when it is erect, it could break. Two columns, or cylinders, that resemble sponges and fill with blood to harden the penis are found in the penis. The tunica albuginea serves as a protective coating over these columns. When the tunica albuginea is ruptured, a penis is deemed fractured or broken. While the majority of patients were able to retain their erectile function and overall sexual function over time, some penile fracture patients may have underlying psychological or vascular issues that could act as predisposing factors for long-term ED development [67].
3. Diagnosis
Treatment selection can become more specific when the root cause of a patient’s ED is known. The following techniques are commonly performed to investigate the cause of erectile dysfunction.
3.1. Psychological Counseling
Psychologic counseling potentially investigates the symptoms or disorders that contribute to dysfunction. In addition, it tries to find out about problems relating to erectile dysfunction, ejaculation, orgasm, or sexual desire. Further, this procedure is performed in order to recognize probable psychological consequences affecting sexual performance. To determine the demands and panoramas observed across a sexual relationship, a sexual partner of the patient can be separately interviewed [68].
3.2. Physical Examination
Physical examination involves the investigation of symptoms associated with systemic disorders, such as neurological dysfunction. Physical examinations can be accomplished in multiple ways. Hairstyle textures, along with additional secondary characteristics of sex, are linked to endocrine system-associated hormonal disorders. An enlargement of the vessels could represent a warning sign of circulatory issues. Any abnormal behaviors associated with the penis can actually point to the root cause of ED [69].
Physical examination includes measuring the size and consistency of the testicles and examining the genitalia for lesions, scars, plaques, and meatal position. In addition, examining abdominal masses, peripheral pulses and feelings, secondary sex features, and the existence of gynecomastia are all important physical investigations. Waist and hip circumference can provide information about obesity. Therefore, the waist-to-hip ratio could be an useful metric for assessing weight loss and the response to hypogonadal medications. It is recommended that men who are considering hormone replacement therapy should have a digital rectal examination [70].
3.3. Laboratory Examinations
A clinical evaluation is necessary for the diagnosis of ED. Blood testing for diabetes, atherosclerosis, chronic renal disease, and hormone issues is one of the basic requirements for ED investigations. Further, evaluations of lipid profiles, hepatic enzyme levels, blood counts, urine tests, and measurements of creatinine are recommended. The fasting lipid profile, fasting glucose level, and, in certain situations, the total testosterone level are among the laboratory tests performed on men with ED. In selected high-risk individuals, screening for prostate cancer is advocated for. A digital rectal examination and a prostate-specific antigen test are other tests required for men with ED [70,71].
3.4. Blood Test for Measurement of Testosterone
Men suffering from ED must check their levels of testosterone, along with other male reproductive hormones, especially when they are suffering from hyperglycemia or reduced sexual desire. Between 12.5% and 35% of men with ED have low total testosterone levels. It is rare to have a testosterone shortage if total testosterone is ≥12 nmol/L (346 ng/dL). Total testosterone below 12 nmol/L (346 ng/dL) necessitates the investigation of serum luteinizing hormone and prolactin levels. This must be done at least one week apart. Serum luteinizing hormone, which is either raised in primary hypogonadism or decreased in secondary hypogonadism, must be measured in order to determine the subtype of testosterone shortage [71].
3.5. Blood Sugar Evaluation
Chronically elevated blood sugar levels may contribute to neurological damage and the destruction of blood vessels, which may cause difficulties in achieving an adequate erection during sex [72].
3.6. Imaging
While there are a number of imaging modalities, including ultrasound, angiography, cavernosography, MRI, etc., that may be used to look into the physical causes of ED, penile Doppler sonography (PDS) is the most informative method and should be used in individuals who do not react to oral pharmaceuticals (such as phosphodiesterase type 5 inhibitors). The Doppler ultrasonography technique is used for observing the flow of blood in the penis [73].
3.7. Nocturnal Penile Tumescence (NPT)
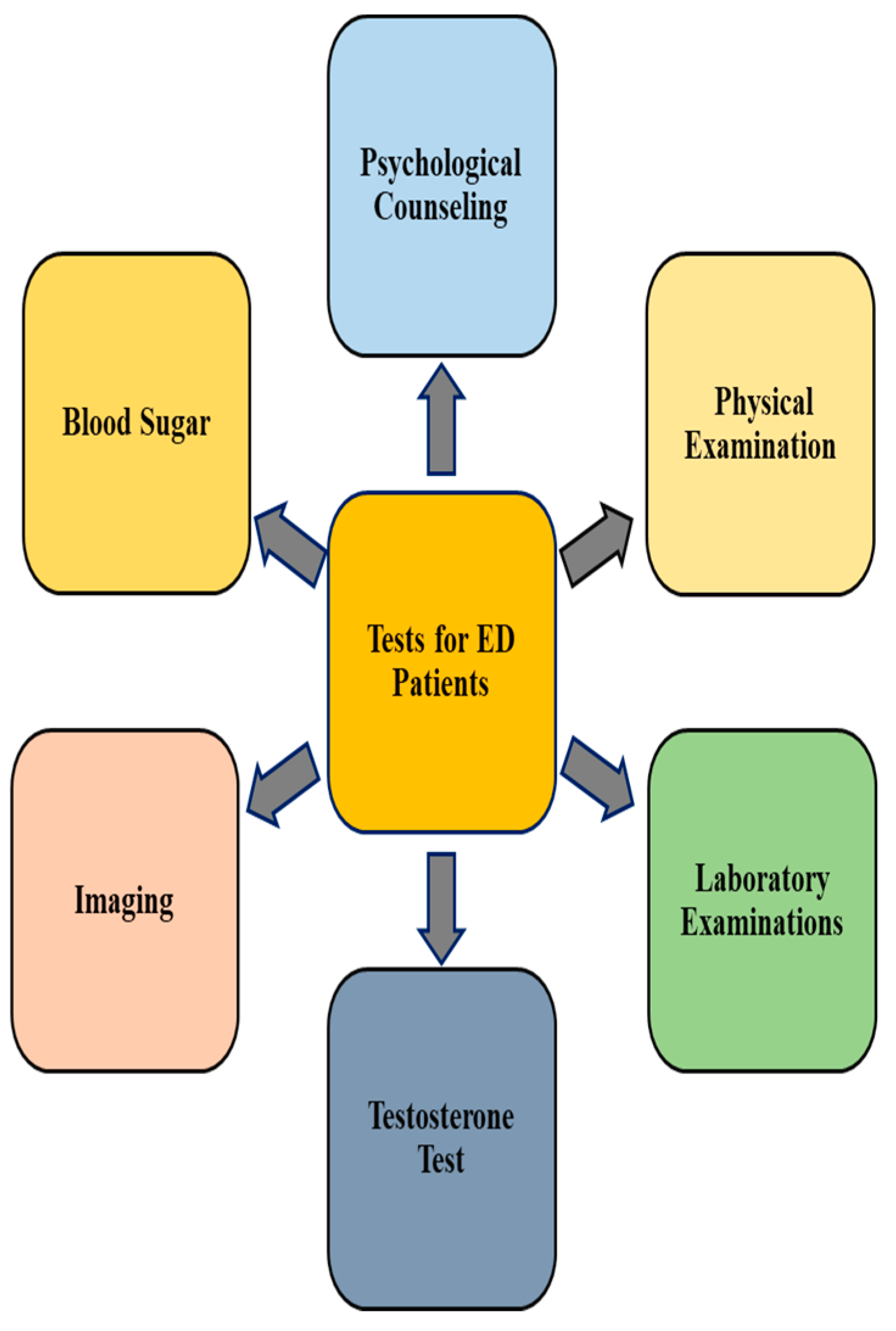
Nocturnal penile tumescence (NPT) is conducted to find out if an erection occurred while sleeping. The patient can typically apply NPT monitoring at home, because it is a straightforward process. Before going to bed, the penis is either treated with an electronic monitor or a single-use snap-gauge device for this test. Normal nocturnal erections are regarded as evidence that the mechanical components of penile erection are operating as intended. Other data, such as the quantity and length of erections, can be evaluated using a more advanced electronic monitor [74]. Figure 2 represents a graphical representation of various kinds of diagnosis strategies.
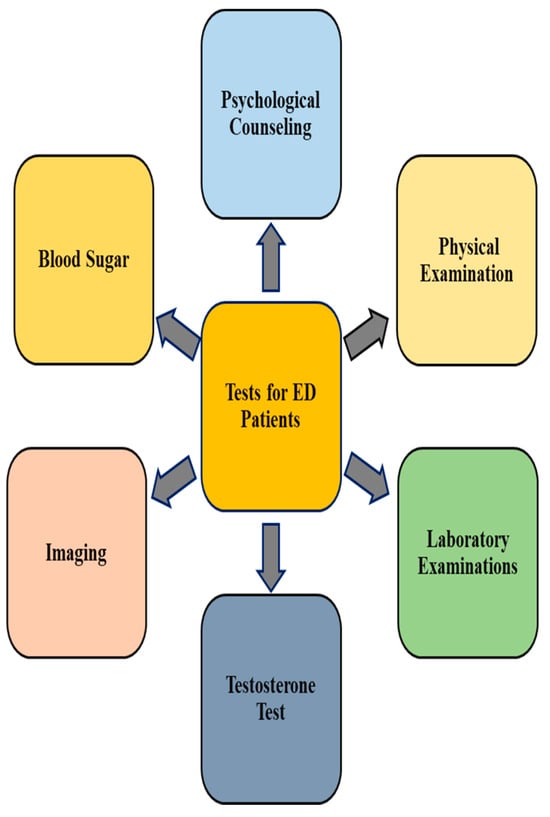
Figure 2.
Screening tests for erectile dysfunction. The diagnosis of erectile dysfunction can be accomplished using numerous strategies.
4. Treatment of ED
ED has been established in prior research to have a detrimental effect on quality of life (QoL) and to be substantially linked to poor social functioning, psychological health, emotional domain, and general health quality in ED patients [2]. A state of whole physical, mental, and social well-being, rather than just the lack of disease or impairment, is referred to as health. Thus, treatment and management of ED patients could improve their general health [75].
Even though a number of off-label medications have demonstrated promising outcomes in the treatment of various common diseases, these illnesses and disorders are not currently treated by fully licensed therapies. This makes the use of off-label medications or other potential medical treatments extremely necessary. In order to avoid using conventional methods for treating diabetes and other related conditions, it is crucial to look into alternative medicine, such as folk medicine [58].
There are multiple types of treatment for ED available, depending on the origin and severity of ED, as well as any underlying medical issues [70]. In addition to taking preferences into consideration, a therapist can go over the advantages and disadvantages of each treatment. Medical and surgical management, lifestyle changes, and psychosexual therapy are the components of ED treatment. In this review, interventions using natural products are discussed in greater detail as alternative and complementary medicines for improving ED.
4.1. Allopathic Treatment
Physicians treat erectile dysfunction with respect to the health status, age, history of health conditions, and level of severity of the disease specific to the patient, along with considering their susceptibility to specific medicines, medications, or techniques. Nowadays, the most commonly used ED medications are vardenafil, tadalafil, and sildenafil. For the treatment of ED, sildenafil was the first PDE5 inhibitor to be licensed. In healthy men, sildenafil, vardenafil, and tadalafil have all demonstrated effectiveness when used as needed and over an extended period of time, with high first-dose response rates [70]. An explanation for this is that metals attached to conserved metal-binding motifs in PDEs aid in the production of attacking OH-. The kinetics of the process are consistent with a random-order mechanism with respect to the cyclic nucleotide and the divalent cation(s) required for catalysis [76].
The above-mentioned treatment has also been found to be effective in ED patients with diabetes mellitus (DM), neurological conditions such as multiple sclerosis and spinal cord injury, hypertension, CAD, renal insufficiency, kidney transplantation, or nerve-sparing radical prostatectomy [70]. In hypogonadal males with ED, testosterone supplementation may reduce cardiovascular risk in addition to ED symptoms. According to a meta-analysis, men with ED respond to testosterone monotherapy and show improvement in their erectile function due to it [77]. Several studies have explored the role of human chorionic gonadotropin (hCG) and clomiphene citrate on sexual function in hypogonadal men, which is particularly significant in hypogonadal men with ED who wish to achieve fatherhood [78].
4.2. Surgery
The primary surgical technique for correcting erectile dysfunction includes the installation of a penile implant, also referred to as a penile prosthesis. Implants are the next step for elderly men who have not responded to oral PDE5 inhibitors, ICIs, or IU treatments, as penile vascular surgery is not advised in these cases. Penile implant implantation is the most successful and well-received therapeutic option for erectile dysfunction, despite being a surgical procedure with attendant risks [70].
4.3. Treatment Based on Plants and Other Natural Products
Because of the widespread distribution of the phosphodiesterase type 5 gene at multiple places throughout the body, PDE5-Is can cause headaches, myalgia, face flushing, heartburn, nasal congestion, and visual issues. Furthermore, illnesses and disorders impacting the upstream nitric oxide pathways have been linked to an effective decrease in efficacy. As a result, it is critical to seek out and identify optional agents capable of overcoming these constraints. With fewer negative effects, natural products and their bioactive components are important in managing disease. Many medicinal plants have been found to be quite helpful in the treatment and prevention of a wide range of illnesses [79]. Plants have been used as remedies to heal a variety of human ailments since time immemorial. This is due to the fact that plants have a wealth of bioactive substances that can be used to treat a variety of diseases [46,49,52,80,81].
Many factors might contribute to an individual’s symptoms of ED, and there are numerous causes of this disorder. Therapeutic interventions using natural products for ED are mainly based on the root causes of sexual dysfunction. The signs and symptoms of erectile dysfunction may be attributed to a broad spectrum of circumstances. Therapeutic natural product techniques focus on the particular causes as well as parameters of each patient, comparable to conventional practitioners. In ddition, a combination of techniques, including plant-based remedies, nutrition, physical treatment, techniques for breathing, the practice of meditation, and physical activity, is advised.
As a whole, developing novel medications to treat ED is imperative, and herbal remedies can be a valuable source of these medications. Herbal remedies for ED have been employed as aphrodisiacs. Numerous plants are still utilized to boost libido, treat ED, and improve sexual dysfunction. Many phytochemicals are found in plants, including steroids, polyphenols, terpenoids, alkaloids, and steroids. Polyphenols such as tannins, phenolic acids, stilbenoids, catechins, procyanidins, and flavonoids are thought to possess anti-inflammatory, anti-cancer, antibacterial, antiviral, anti-tumor, and anti-mutagenic qualities. These polyphenols have the potential to shield the vascular endothelium from ROS damage [82]. Sebastiani and colleagues (2023) studied the therapeutic qualities and modes of action of plant-based supplementations in treating infertility and verified their beneficial effects on infertility and general human health [83].
Table 1 displays some medicinal plants used for ED improvement.

Table 1.
Medicinal plants used for the treatment of ED.
4.3.1. Ashwagandha
Withania somnifera (WS), often known as ashwagandha, is a herb that has recently acquired popularity in the United States as a cure for anxiety and stress. Despite being used as a broad-spectrum medicine in India for centuries, WS has only lately been studied in a laboratory context. WS is classified as an anti-inflammatory herbal supplement with antioxidant properties [103].
Furthermore, the herb has been suggested for use as an adaptogen and energy booster, as a result of its recognized antioxidant and free radical-scavenging properties [104].
In one study, muscular strength and muscular mass in the arms and chest was found to have increased significantly in WS-treated patients. The level of exercise-induced muscle myocyte damage was much lower in the Ashwagandha-supplemented patients than in the placebo group, as seen by the stabilization of plasma creatine kinase levels. Furthermore, a large increase in testosterone levels and a significant decrease in body fat were observed in the WS-treated group [90].
Ashwagandha, as well as its extract, is believed to provide a potent sexually stimulating effect due to the fact that it is composed of numerous bioactive chemical compounds, which include withanolides. A study conducted on both humans and animals has proven the sexual stimulant and testosterone-boosting benefits associated with ashwagandha [105].
A previous study evaluated the aphrodisiac properties of an ashwagandha root extract in adult males in an 8-week randomized, double-blind, placebo-controlled trial. When compared to a placebo, ashwagandha root extract consumption was related to a statistically significant rise in total DISFM scores. It was also linked to a statistically significant increase in serum testosterone levels [106].
The effects of Ashwagandha on weariness, vigor, and steroid hormones in aging males were explored in randomized, double-blind, placebo-controlled crossover research. For 8 weeks, using a standardized ashwagandha extract (Shoden beads) was related to increased levels of DHEA-S and testosterone, but no significant between-group variations in cortisol, estradiol, weariness, vigor, or sexual well-being were detected [89].
4.3.2. Kaunch (Mucuna pruriens)
Mucuna pruriens (Fabaceae) is a well-known herbal remedy used as an aphrodisiac and to treat mental problems and male infertility. Research has demonstrated that the seeds of this plant may have significant medical value. M. pruriens may exhibit antioxidant actions, because it has been demonstrated to have neuroprotective and anti-Parkinson’s properties. Furthermore, M. pruriens has been shown to possess antioxidant activity in vitro through its capacity to scavenge reactive oxygen species and DPPH radicals [107].
Due to the fact that kaunch seeds carry aphrodisiac characteristics, they improve enthusiasm for sexual activities. In addition, this stimulates the supply of blood through the male reproductive organs, so it helps stimulate the sensation of sexual interest for both women and men. The powder of seeds from kaunch provides a naturally occurring source of testosterone. The reason for this is the fact that it provides L-dopamine, and so it boosts the gonadotropic hormone (GnRH) synthesis process [108].
It promotes the mobility of sperm as well as the count. Furthermore, it contributes to enhancing semen output and amount. In addition, kaunch seeds strengthen the quality of semen and minimize stress on the body via their antioxidative properties. Based on a number of studies, kaunch seed can be suggested as a means to promote sexual performance by prolonging ejaculation [109].
4.3.3. Dates
The date palm is being widely used for its pharmacological activity. Date palm pollen (DPP) has been shown in earlier research to boost sperm count and quality. Age-old medications for erectile dysfunction and impotence have involved the consumption of Phoenix dactylifera, commonly known as date palm pollen, which constitutes the male reproductive powder of palm flowers. A randomized, double-blind, and placebo-controlled clinical trial was conducted involving 60 Iranian men who underwent coronary artery bypass graft (30 were in the DPP group, and 30 were in the control group) and were treated with DPP daily. These patients showed improvement in their complaints of male sexual dysfunction after consuming 6 g of DPP daily for two months [97].
A double-blind, placebo-controlled clinical experiment was conducted that took place in 2019 among Iranian infertile couples who were referred to infertility clinics by their spouses. The control group received a placebo, whereas the intervention group received a date palm pill. An attempt was made to treat erectile dysfunction as well as sexual dysfunction by consuming seven dates every day in combination with an appropriate diet. According to the study, the sexual function of infertile couples was improved after consuming date palms for one month [110].
Date palm pollen (DPP) may enhance semen parameters and stimulate antioxidant activity in male rats, according to mounting data. The effects of DPP on male fertility in humans are, nevertheless, supported by a small body of scientific data. Therefore, a previous study assessed infertile men’s sperm characteristics and the expression pattern of the genes encoding peroxiredoxin-1 (PRDX1) and peroxiredoxin-6 (PRDX6) in relation to the oral ingestion of DPP. DPP consumption was found to significantly improve sperm morphology and semen volume. The DPP group’s 8-isoprostane levels sharply decreased after intervention. Consuming DPP considerably raised the expression of the PRDX1 and PRDX6 genes. Increased expression of the PRDX6 and PRDX1 genes was positively correlated with improved metrics of sperm, including count, volume, motility, and shape [111].
4.3.4. Musli
Known by its common name, Shweta musli, Chlorophytum borivilianum L. is a medicinal plant that grows in large quantities over the Indian subcontinent. It has been determined that pre-treatment with 50 mg/kg body weight of CRE might shield sperm from oxidative stress during the maturation of the epididym [98].
With no negative side effects, safed musli (Chlorophytum) is a highly-liked aphrodisiac. It is frequently recommended for the purpose of increasing male potency and reducing fatigue symptoms. The aphrodisiac potential and reproductive system safety profile of the standardized extract of saved musli root were assessed in vivo. Male rats were dosed with extract for 54 days at 125 and 250 mg kg−1 p.o. The animals were watched for sexual activity from the cage side on days 14 and 28. Up to the 28th day, safed musli at both dosage levels increased libido and sexual energy, suggesting potential benefits for treating male sexual dysfunction. After using it for 54 days, the safety profile was also evaluated. Both doses increased the number and motility of sperm. Given that both doses have the capacity to proliferate, it can be concluded that treatment using safed musli would be extremely helpful in treating sexual dysfunction [112]. By lowering oxidative stress, apoptosis, and free radical levels in the sperm of diabetics, C. borivilianum root extract prevents deterioration in sperm characteristics and morphology [99].
4.3.5. Watermelon
Citrullus lanatus, a member of the Cucurbitaceae family, is high in citrulline and arginine. These amino acids are crucial for the synthesis of nitric oxide (NO), a powerful vasodilator [113]. Watermelon is a special source of easily accessible cis-isomeric lycopene. Medium- and short-chain fatty acids, neral, ß-ionone, and geranial all contribute to the unique scent of watermelon. Its strong nutritional profile and associated health advantages have led to an increase in its consumption. It has been found to be efficacious in mitigating the degree of cancer recurrence, cardiovascular ailments, diabetes, and corneal problems [114].
Twenty Wistar male rats were divided into two groups, including the control group and the Citrullus vulgaris (C.V.) group. The C.V. group received 55 mg kg−1.day−1 C.V. via gavage technique for four weeks. The control group, on the other hand, received an equal volume of distilled water every day. Testicular tissues were taken on the 28th day and processed for sperm examination. Significant increases in sperm population, motility, and viability were observed at 55 mg kg−1 of C.V. [100].
Men with mild ED (erection hardness score of three) were given a placebo for one month and 1.5 g/d of L-citrulline for an additional month in a single-blind research study. Records were kept on the number of intercourse events each month, treatment satisfaction, erection hardness score, and adverse events. Supplementing with L-citrulline has been shown to be safe and well-received by patients mentally. It is used as a substitute therapy for mild to moderate ED, especially in individuals who have a phobia of phosphodiesterase type 5 enzyme inhibitors on a psychological level [115].
4.3.6. Yohimbine
The bark of the African yohimbe tree, Pausinystalia johimbe, yields yohimbine, an indole alkaloid [116]. Diabetes, depression, weariness, and sexual dysfunction have all been reported to be treated with yohimbine. When treating ED with infrequent adverse effects, yohimbine was found to be more effective than a placebo in a meta-analysis of seven studies [101].
Instead of a true increase in sexual excitement at first, researchers thought that the extract’s aphrodisiac effects were only a placebo or caused by an increase in peripheral vascular congestion. According to the suggested mechanism of action, increased NO is produced by inhibiting central alpha-2-adrenergic receptors, reducing central inhibition of arousal, and boosting penile nerve stimulation. Headache, perspiration, agitation, hypertension, and sleeplessness are typical adverse effects. In addition, patients on tricyclic antidepressants, antihypertensives, or central nervous system stimulants are contraindicated [117].
4.3.7. Ginseng
Among the most significant therapeutic herbs in Asia is ginseng (Panax ginseng Meyer). Ginseng-containing dietary supplements, or ginseng supplements alone, have been commonly used to treat a variety of ailments, including erectile dysfunction. Asia is home to a large population of ginseng users. Among the most popular ingredients found in sexual health supplements for men, ginseng is the most prevalent. Ginseng has long been utilized to support and restore the body’s natural state of well-being. Ginseng’s benefits derive from its interactions with the immune system, metabolism, cardiovascular system, and central nervous system. Ginsenosides, a class of triterpene saponins, are the main active ingredients. Certain ginsenosides may be responsible for the ginseng-mediated effects on copulatory behavior, according to research on animals. Ginsenoside hyperpolarizes the smooth muscle membrane by activating large-conductance KCa channels, which causes smooth muscle relaxation [117].
Individual studies evaluating its effects are few, have inconsistent methodological quality, and have produced ambiguous results. Due to ginseng’s safety profile and associated notable improvement in International Index of Erectile Function (IIEF)-5 scores, it is a viable option for presently recommended treatments for ED [118].
4.3.8. Ginkgo biloba
It is recommended to use Ginkgo biloba to cure a variety of ailments, from high blood pressure to Alzheimer’s disease. There is evidence that it improves memory in elderly populations [119], claudication distance and cutaneous ulcers in patients with peripheral vascular disease [120], and overall cognitive performance [121].
It is suggested that extract from Ginkgo biloba stimulates NO production in endothelial cells, which relaxes vascular smooth muscles. According to research on animals, Ginkgo biloba was responsible for the relaxation of the smooth muscle cells of the rabbit corpus cavernosus [122]. Images showing the different plants with proven potential to treat erectile dysfunction are provided in Figure 3.

Figure 3.
Plants with proven potential for improving erectile dysfunction. (A) W. somnifera; (B) kauch; (C) safed musli; (D) ginseng; (E) Ginkgo biloba; (F) watermelon.
4.3.9. Arctium lappa
Arctium lappa L. is a member of the family Compositae. It is commonly referred to as “burdock” in English and has been used to cure a variety of illnesses, including dermatitis and sore throats. The phytochemical characteristics of the plant, including anti-inflammatory, antiviral, anti-cancer, and anti-diabetic effects, have been documented [123]. In addition to being used to treat ED and infertility, A. lappa has also been utilized as a sexual stimulant. JianFeng et al. (2012) examined the aphrodisiac effects of A. lappa aqueous root extracts (300, 600, and 1200 mg/kg) given orally to adult male Sprague-Dawley rats for a period of seven days. The extract treatment dramatically raised the rates of mounting, intromission, and ejaculation [124].
In another study, only diabetic mice showed increased sperm vitality after consuming 300 mg/kg of the hydroalcoholic extract of A. lappa. Furthermore, as compared to the control group, this extract dose enhanced testosterone, FSH, LH, and sperm count in non-diabetic mice. The findings show that applying burdock root extract to non-diabetic mice has anti-infertility benefits [125].
4.3.10. Euphorbia hirta L.
The family Euphorbiaceae includes Euphorbia hirta L.’s extracts, which are utilized in East and West Africa to treat respiratory tract inflammation and asthma [126]. In Madagascar, it is also used to treat respiratory conditions, such as chronic bronchitis and coughs. Angola also uses the plant extensively to treat diarrhea and dysentery, particularly amoebic dysentery. Plant extracts or exudates are used as ear drops, to treat boils, to relieve sore throats, and to encourage the healing of wounds in Nigeria [127]. Additionally, Nigerian traditional healers use Euphorbia hirta to treat male sexual dysfunction [128].
4.3.11. Crocus sativus L. (Saffron)
This plant is a member of the family Iridaceae. There have been three clinical studies that have shown that this plant considerably raised patient IIEF scores [129,130,131]. Moreover, a study discovered that C. sativus considerably enhanced base tumescence, tip tumescence, tip rigidity, and base rigidity (p < 0.0001). However, there was no placebo group in this open-label investigation, and the entire intervention lasted for just ten days. Furthermore, only 20 individuals between the ages of 26 and 62 were enrolled [129].
Saffron was tested in a double-blind, randomized, placebo-controlled trial to evaluate how it affected men’s fluoxetine-induced sexual dysfunction. By week 4, the saffron group outperformed the placebo group in terms of improvement in overall scores (p < 0.001), intercourse pleasure domains (p = 0.001), and erectile function (p < 0.001).
A double-blind, placebo-controlled, randomized, parallel-group trial was carried out to examine the impact of topical saffron (C. sativus L) gel on ED in diabetics. The produced saffron gel was shown to considerably improve erectile dysfunction in diabetic individuals when compared to placebo (p < 0.001) [131].
4.3.12. Rosa damascena (Damask Rose)
Damask rose belongs to the Rosaceae family. Rosa damascena (R. damascena) has been studied in two double-blind, randomized, placebo-controlled clinical trials [132]. In one study, patients with methadone-induced sexual dysfunction were treated with the essential oils of R. damascena (drops) containing 17 mg of citronellol for two months each. Considerable improvements in methadone-induced sexual dysfunction and a considerable rise in blood testosterone levels were observed with R. damascena [133].
Another study concentrated on patients with SSRI-induced sexual dysfunction. In this investigation, 68 patients were included with 8 dropouts and were provided essential oil of R. damascena (drops) containing 17 mg of citronellol for two months each. Significant improvements were seen in major depressive disorder (MDD) symptoms and SSRI-induced sexual dysfunction, with improvements in MDD symptoms coinciding with improvements in sexual dysfunction [134].
4.4. Treatment of ED Using Vitamin B12 and Vitamin E
4.4.1. Vitamin B12
Vitamin B12 (cobalamin) is necessary for the synthesis of DNA and its methylation, folate metabolism, the formation of red blood cells, neurological development, the proper functioning of the central nervous system, as well as for controlling and producing fatty acids. Additionally, it plays a significant role in the synthesis of energy as well as the degradation of proteins, phospholipids, and neurotransmitters [135].
A vitamin B12 deficiency may lead to complications with sexual performance, especially an inability to induce and maintain a good erection. The association between folic acid, homocysteine, vitamin B12, and erectile dysfunction was studied in a cross-sectional study. The purpose of this study was to investigate the relationship between ED, homocysteine (HCY), vitamin B12 (B12), and folic acid (FA). Out of all of the participants, 1381 completed the questionnaires, and the males with ED had higher B12 levels [136].
B12 is crucial for the breakdown of homocysteine and may also be the primary cause of erectile dysfunction. In a study, 691 males (47.4%) with ED showed several factors associated with ED, including age, Hcy, and B12, as revealed by a logistic regression analysis. This research showed a correlation between elevated homocysteine levels and B12 deficiency [137].
4.4.2. Vitamin E
Patients aged 18 to 60 who had erectile dysfunction as defined by the IIEF questionnaire were randomized equally to receive a daily supplement of 100 IU of vitamin E, 67 mg of Korean ginseng, 40 mg of Siberian ginseng, or a placebo in a placebo-controlled trial. It was suggested that a vitamin E and ginseng supplement might help erectile function management while preserving a safe and tolerable adverse event profile. Vitamin E is a potent antioxidant and vascular stimulant that can improve and prolong erections as well as protect penis blood circulation. Since damage caused by oxidative stress causes diminished circulation within the pelvic tissues, reduced elasticity of arteries and veins, decreased stimulation of nerves and sensations, and lowered penile adaptability, vitamin E supplementation improves the symptoms patients with ED. Vitamin E-rich foods include broccoli, spinach, nuts, and seeds, as well as vegetable oils. Vitamin E’s capacity to destroy harmful free radicals has been suggested to be beneficial for individuals who struggle with problems with ED. In vitro and in vivo data have confirmed the significance of vitamin E as an antioxidant and a lipid-soluble peroxyl radical scavenger [138]. In hypertensive rats, antioxidant therapy with alpha-tocopherol was shown to improve ED [139].
5. Herb-Based Treatment Mechanisms for Improvement of ED
Because herbal medicines mimic hormones, nitric oxide, and neurons, they have a number of impacts on improving ED. NO is an unusual regulating molecule that functions as both a neurotransmitter and a secondary messenger. It has been demonstrated that a variety of medicinal herbs and medications prepared from these herbs affect the NO signaling pathway. For instance, it has been shown that ginsenosides relax blood vessels and the corpus cavernosum, which may help explain ginseng’s anti-fatigue and blood pressure-lowering properties [96]. Androgens are essential for the development of secondary male sexual organs like the penis, seminal vesicle, vas deferens, and epididymis. In addition, male sexual function, male fertility, and puberty all depend on androgens. After crossing the nuclear membrane and attaching to DNA, the testosterone- or dihydrotestosterone-receptor complex promotes the production of new mRNA and, consequently, new proteins. The hypothalamus’s conversion of testosterone to estradiol may be necessary for the impact of testosterone on libido. Men’s testosterone concentrations can be positively impacted by certain herbs, including fenugreek seed and ashwagandha extracts [140].
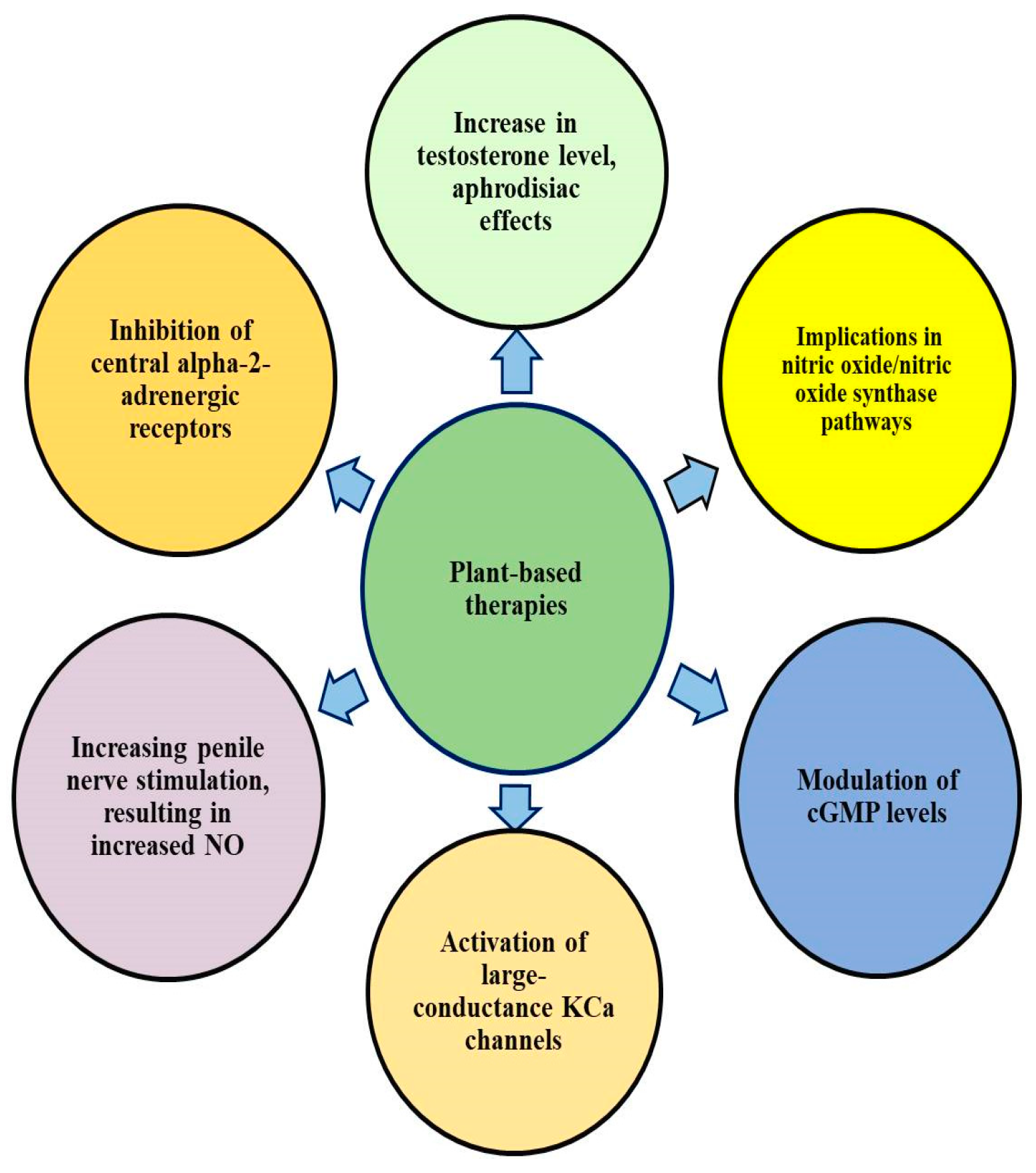
Penile erection can be effectively improved by B. superba ethanol extract. According to a study by Cherdshewasart and Nimsakul (2003), ethanol extract raised intracavernous pressure (ICP) in vivo [141]. Moreover, a study has demonstrated how C. orchioides helps people recover from sexual dysfunction brought on by physical testicular injury [142]. In addition, a study confirmed that sperm count increased significantly, the motility and the percentage of living sperm were enhanced, and the number of aberrant sperm was reduced by using an aqueous extract of Cynomorium coccineum. As compared to the untreated controls, testicular histology from the treated group revealed higher spermatogenesis and seminiferous tubules filled with sperm with this treatment [143]. The plant Icariin, which is derived from Epimedium koreanum, has been shown to imitate the actions of testosterone and increase the generation of bioactive nitric oxide and cyclic guanosine monophosphate in cavernous smooth muscle cells treated with sodium nitroprusside [144]. Plant-based treatments have multiple mechanisms, as exhibited in Figure 4. A list of medicinal plants used for ED treatment, with causes of ED, their mechanisms of action and diagnosis methods in various investigations, is provided in Table 2.
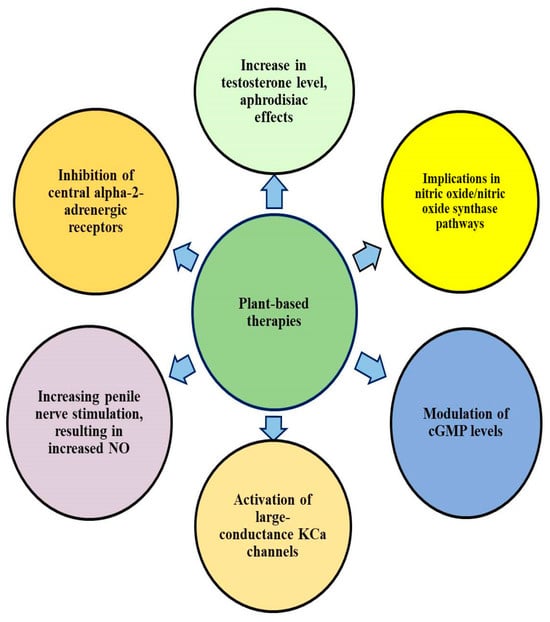
Figure 4.
Plant-based therapy for erectile dysfunction has multiple mechanisms of action.

Table 2.
A list of medicinal plants used in investigations against ED, inducers and causes of ED in investigations, mechanisms of action, and diagnosis strategies.
6. Approach to Increase the Efficiency of Natural Products
Herbal remedies have a long history of use in ancient medical systems and are now widely accepted as safe and natural substitutes for pharmaceutical treatments for diseases. Nonetheless, strict quality control procedures have been utilized to guarantee uniformity and safety in the creation, production, and distribution of herbal products for the effective treatment of ED. Further, standardization, contaminant detection and prevention, herbal ingredient authentication, and regulatory standard conformance are some methodologies used in original research to evaluate the efficacy, onset of action, and safety of herbal therapies over time. The combination of ancient knowledge and contemporary scientific methods can be used to achieve the best possible quality control results [150].
Significant properties of natural products include their remarkable diversity, chemical and biological potential with macromolecular accuracy, and fewer side effects. Therefore, they are considered among the most efficient options for finding new medications. However, natural products contain a broad spectrum of chemical ingredients. Moreover, there are a number of issues linked with natural products, such as poor in vivo solubility, stability, and bioavailability, low absorption in the body, issues with tonic efficacy and target-specific delivery, and potentially harmful pharmacological adverse effects. As a result of these issues, numerous natural compounds have not yet passed the stage of clinical trials. As a result, significant work is advised for this purpose. Thus, utilizing novel drug delivery techniques to tailor medications to certain body areas may be a solution to these pressing problems [144].
Because of associated isolation processes, pure constituents are more expensive to manufacture, but easier to work with. These efforts, as in many situations, were not sufficient. The development of semisynthetic substances or synthetic analogues, or the synthesis of prodrugs, represents a further attempt to optimize the performance of natural products. An additional and more sophisticated method for maximizing the bioavailability and/or stability of separated constituents and extracts is provided by the design and manufacture of suitable drug delivery devices, particularly those at the nanoscale [151].
The development of THM delivery systems, such as liposomes, microcapsules, emulsions, solid dispersions, magnetic nanocarriers, and nanocomposites, is made possible by the use of nanotechnological materials, which have been shown to have a greater curative impact or novel efficacy, improved medication stability, flexible dosage forms, enhanced drug delivery pathways, etc. One of the main benefits of using nanocarriers is that they can distribute medications in a regulated and sustained manner, increasing their biological half-lives and prolonging their in vivo cycle durations [152].
7. Optimal Patient Selection, Dosage Regimen, Formulation and Future Research
One of the most difficult problems in drug development is still choosing the right dose for confirmatory studies. Furthermore, the majority of patients included in pivotal trials are often very young or elderly, malnourished or morbidly obese, pregnant, or have many features that could affect dose. These individuals are also not included in the majority of the present labeled guidelines. Physicians may therefore have to make informed decisions on the appropriate dosage and plan for these individuals. Providing recommendations for dosage and regimen for these individuals is now possible through the integration of existing scientific knowledge and the use of or modification of established regulatory agency–industry methods. Therefore, it is advised to investigate a number of variables that need to be taken into account while developing a procedure that would offer more accurate, secure, and appropriate medication dosing recommendations for the majority of patients [153,154].
8. Perspectives and Novelity of Current Study
If appropriate action is not taken to stop the rising incidence of erectile dysfunction (ED), it is projected that 322 million men worldwide will be affected by the condition by 2025 [155]. Currently, there are various standard therapies for ED available, including oral allopathic medicines, vacuum erectile devices (VEDs), intraurethral suppositories or penile injections, and penile prostheses. However, satisfactory ED treatment still remains a clinically demanding phenomenon, despite recent progress [156]. Hyperestrogenism has been reported to be one of the significant causative factors of ED [157]. Aromatase inhibitors (AI) and selective estrogen receptor modulators (SERM) have been used to treat hyperestrogenism symptoms [158]. Coronary heart disease (CHD) severity may be predicted by the severity of ED and the interval between the development of ED and CHD. Therefore, it is recommended that ED patients cut back on alcohol and tobacco use, keep a healthy weight, and engage in regular physical activity to prevent CHD [159]. PDE5 inhibitors have been used for the improvement of ED. However, the use of phosphodiesterase type 5 inhibitors has many side effects, like malignant melanoma [160,161]. Food deficits brought on by a poor diet will almost definitely exacerbate chronic diseases [162]. It is suggested that maintaining the health of erections may be aided by following a balanced food regimen [39].
It has been previously reported that medicinal plants can be used to treat diseases related to men more effectively and with the fewest side effects [49]. Medicinal plants and their bioactive compounds have been reported as excellent therapeutic choices due to their important roles in disease prevention. In addition, their use as complementary medicines with existing treatments for various diseases has already been recommended by previous research. Moreover, many in vivo studies, preliminary clinical studies, and clinical trials have shown significant improvements in ED (references are provided). These studies look very promising. While it is possible that medicinal plants could supply the lead ingredients for erectile dysfunction medications, further research is necessary to determine the dosage, toxicity, and effectiveness of these potential remedies. Polyphenolic compounds present in plants are suggested to contribute to ED improvement activity. Due to their capacity to inhibit arginase, acetylcholinesterase, angiotensin converting enzyme, rho-kinase II, and their potential to activate endothelial and neuronal NO synthase to reduce the synthesis of luteinizing hormone and testosterone, as well as inhibit free radical and reactive oxygen species, natural polyphenols are suggested as being involved in the improvement of ED [155]. Therefore, it is likely that combination therapy of current modes of therapy with herbal interventions will become widely accepted for more difficult and refractory instances of ED in the future.
This manuscript reviewed previous studies, including in vitro, in vivo, and clinical investigations, to ascertain whether a plant-based diet was associated with a reduction in ED symptoms. In addition, the risk factors and linked variables, along with diagnostic strategies for ED, have also been outlined. Herb-based treatment mechanisms for improving ED, approaches to increasing the efficiency of natural products, optimal patient selection, dosage regimen, and formulation in context with future research have been discussed. In addition, the roles of vitamin E and B12 have been discussed under separate headings. To the best of our knowledge, all of these topics have not been covered together in a single previous study before now. Further, the most recent studies in this field were reviewed, and they added new realms to the existing knowledge in a new and innovative way. All of these are compiled in the present study, making it novel and significant compared to previous investigations.
9. GRADE or Oxford CEBM Levels of Evidence: A Grading System for Leveling Evidences for Herbal Therapy
The goal of evidence-based medicine (EBM) is to locate evidence and apply it to clinical decision-making. EBM’s hierarchical evidence classification method is one of its main tenets, and the levels of evidence refer to this structure. The essential parts of EBM are the evidence levels. Knowing the levels and the rationale behind their assignment to articles and abstracts facilitates the reader’s information prioritization. There is a ranking criteria used to determine the quality of evidence and suggestions. In addition, there are recognized, well-established standards that are also followed by other firms. These criteria include evidence levels from Oxford’s Centre for Evidence-Based Medicine (CEBM), recommendation grade (per CEBM), and evidence quality rating according to GRADE standards [163]. Table 3 shows the criteria and grading system for leveling evidence for herbal therapy. This was adopted from https://www.ebmconsult.com/articles/levels-of-evidence-and-recommendations, accessed on 3 April 2024 with some modifications.

Table 3.
The criteria for therapy, prevention, etiology, and harm for herbal products.
10. Conclusions
People who suffer from overweight, Type 2 diabetes, cigarette smoking, depressive disorders, alcohol dependence, as well as hormonal dysfunction must pay considerable attention to optimizing their dietary habits as well as their physical activity. The causes of ED across different populations are many and include organic, psychogenic, and mixed variables. Moreover, comorbid conditions like diabetes, heart disease, and neurological illnesses are frequently linked to the etiology of ED. Therefore, it is necessary to take into account every facet of the patient’s health when managing ED. For the treatment of ED, there are a few therapeutic alternatives available, including surgery and medicine, and these treatment choices seem promising. Nevertheless, not every patient responds to the existing treatments, and pharmacological intervention may be further limited by side effects and costs. Many people with ED have been documented to use herbal and alternative medicines, especially dietary supplements that are sold in stores. The current review offers a summary of herbal treatments for ED and how they work in relation to earlier studies that suggested they could help with ED. However, not much research is currently being conducted concerning specific dosages as well as periods of treatment for ED. Since the effects of some plants on ED have been proven, these plants may be used as a starting point to find novel chemical compounds that treat erectile dysfunction and sexual dysfunction. While there is hope that medicinal plants could provide lead chemicals for ED drugs, even more research is crucial to explore the dosage, toxicity, and efficacy of these prospective treatments.
Author Contributions
Conceptualization, S.A., V.K. and F.A.; writing—original draft preparation, S.A., E.A.Y. and F.A.; writing—review and editing, S.A., F.A. and R.R.; visualization, S.A.; supervision, F.A. and S.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors extend their appreciation to the Chairman, Mohan Institute of Nursing and Paramedical Sciences, India, Faculty of Nursing, Cairo University, Egypt, and College of Applied Medical Sciences, and Qassim University, Saudi Arabia, for their support.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yafi, F.A.; Jenkins, L.; Albersen, M.; Corona, G.; Isidori, A.M.; Goldfarb, S.; Maggi, M.; Nelson, C.J.; Parish, S.; Salonia, A.; et al. Erectile dysfunction. Nat. Rev. Dis. Primers 2016, 2, 16003. [Google Scholar] [CrossRef] [PubMed]
- Agaba, P.A.; Ocheke, A.N.; Akanbi, M.O.; Gimba, Z.M.; Ukeagbu, J.; Mallum, B.D.; Agaba, E.I. Sexual Functioning and Health-related Quality of Life in Men. Niger. Med. J. 2017, 58, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Elterman, D.S.; Bhattacharyya, S.K.; Mafilios, M.; Woodward, E.; Nitschelm, K.; Burnett, A.L. The Quality of Life and Economic Burden of Erectile Dysfunction. Res. Rep. Urol. 2021, 13, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Cai, T.; Verze, P.; Bjerklund Johansen, T.E. The Quality of Life Definition: Where Are We Going? Uro 2021, 1, 14–22. [Google Scholar] [CrossRef]
- Anderson, D.; Laforge, J.; Ross, M.M.; Vanlangendonck, R.; Hasoon, J.; Viswanath, O.; Kaye, A.D.; Urits, I. Male Sexual Dysfunction. Health Psychol. Res. 2022, 10, 37533. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.A.; Lie, J.D. Phosphodiesterase-5 (PDE5) Inhibitors In the Management of Erectile Dysfunction. Pharm. Ther. 2013, 38, 407–419. [Google Scholar]
- Sheweita, S.; Salama, B.; Hassan, M. Erectile dysfunction drugs and oxidative stress in the liver of male rats. Toxicol. Rep. 2015, 2, 933–938. [Google Scholar] [CrossRef]
- Yannas, D.; Frizza, F.; Vignozzi, L.; Corona, G.; Maggi, M.; Rastrelli, G. Erectile Dysfunction Is a Hallmark of Cardiovascular Disease: Unavoidable Matter of Fact or Opportunity to Improve Men’s Health? J. Clin. Med. 2021, 10, 2221. [Google Scholar] [CrossRef]
- Ahmed, A.; Alnaama, A.; Shams, K.; Salem, M. Prevalence and risk factors of erectile dysfunction among patients attending primary health care centres in Qatar. East. Mediterr. Health J. 2011, 17, 587–592. [Google Scholar] [CrossRef]
- Available online: https://www.hopkinsmedicine.org/health/conditions-and-diseases/erectile-dysfunction#:~:text=Organic%20Erectile%20Dysfunction,arteries%20may%20be%20the%20cause (accessed on 3 April 2024).
- Gareri, P.; Castagna, A.; Francomano, D.; Cerminara, G.; De Fazio, P. Erectile Dysfunction in the Elderly: An Old Widespread Issue with Novel Treatment Perspectives. Int. J. Endocrinol. 2014, 2014, 878670. [Google Scholar] [CrossRef]
- Feldman, H.A.; Goldstein, I.; Hatzichristou, D.G.; Krane, R.J.; McKinlay, J.B. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J. Urol. 1994, 151, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Lee, D.M.; Forti, G.; O’connor, D.B.; Maggi, M.; O’neill, T.W.; Pendleton, N.; Bartfai, G.; Boonen, S.; Casanueva, F.F.; et al. Age-Related Changes in General and Sexual Health in Middle-Aged and Older Men: Results from the European Male Ageing Study (EMAS). J. Sex. Med. 2010, 7 Pt 1, 1362–1380. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.S.; Wood, A.M.; Sheffield, D. The Psychology of Erectile Dysfunction. Curr. Dir. Psychol. Sci. 2023, 32, 487–493. [Google Scholar] [CrossRef]
- Ciaccio, V.; Di Giacomo, D. Psychological Factors Related to Impotence as a Sexual Dysfunction in Young Men: A Literature Scan for Noteworthy Research Frameworks. Clin. Pract. 2022, 12, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Vickers, M.A.; De Nobrega, A.M.; Dluhy, R.G. Diagnosis and Treatment of Psychogenic Erectile Dysfunction in a Urological Setting: Outcomes of 18 Consecutive Patients. J. Urol. 1993, 149 Pt 2, 1258–1261. [Google Scholar] [CrossRef] [PubMed]
- Mallis, D.; Moysidis, K.; Nakopoulou, E.; Papaharitou, S.; Hatzimouratidis, K.; Hatzichristou, D. Psychiatric morbidity is frequently undetected in patients with erectile dysfunction. J. Urol. 2005, 174, 1913–1916. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Xie, T.; Peng, J.; Zhou, X.; Long, J.; Yang, M.; Zhu, H.; Yang, J. Factors associated with anxiety and depression in patients with erectile dysfunction: A cross-sectional study. BMC Psychol. 2023, 11, 36. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, R.; Gervasi, G.; Naro, A.; de Luca, R.; Marullo, M.; Bramanti, P. Erectile Dysfunction in Individuals with Neurologic Disability: A Hospital-based Cross-sectional Study. Innov. Clin. Neurosci. 2016, 13, 10–14. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4896824/ (accessed on 10 December 2023). [PubMed]
- Available online: https://www.ucsfhealth.org/conditions/erectile-dysfunction#:~:text=Neurological%20conditions&text=Parkinson’s%20disease%2C%20Alzheimer’s%20disease%2C%20stroke,the%20extent%20of%20the%20injury (accessed on 3 April 2024).
- Villegas, G.; Tar, M.T.; Davies, K.P. Erectile dysfunction resulting from pelvic surgery is associated with changes in cavernosal gene expression indicative of cavernous nerve injury. Andrologia 2022, 54, e14247. [Google Scholar] [CrossRef]
- Shridharani, A.N.; Brant, W.O. The treatment of erectile dysfunction in patients with neurogenic disease. Transl. Androl. Urol. 2016, 5, 88–101. [Google Scholar] [CrossRef]
- Thomas, C.; Konstantinidis, C. Neurogenic Erectile Dysfunction. Where Do We Stand? Med. Basel Switz. 2021, 8, 3. [Google Scholar] [CrossRef] [PubMed]
- Bronner, G.; Vodušek, D.B. Management of sexual dysfunction in Parkinson’s disease. Ther. Adv. Neurol. Disord. 2011, 4, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Javaroni, V. Editorial Comment: Sexual Dysfunction in Parkinson Disease: A Multicenter Italian Cross-sectional Study on a Still Overlooked Problem. Int. Braz. J. Urol. Off. J. Braz. Soc. Urol. 2021, 47, 1057–1060. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.; Mielke, M.M.; Ahlskog, J.E.; Bower, J.; Turcano, P.; Savica, R. Erectile Dysfunction Preceding Clinically Diagnosed α-Synucleinopathies: A Case-Control Study in Olmsted County. Park. Dis. 2019, 2019, 6303945. [Google Scholar] [CrossRef]
- Ma, M.; Yu, B.; Qin, F.; Yuan, J. Current approaches to the diagnosis of vascular erectile dysfunction. Transl. Androl. Urol. 2020, 9, 709–721. [Google Scholar] [CrossRef] [PubMed]
- Fillo, J.; Levcikova, M.; Ondrusova, M.; Breza, J.; Labas, P. Importance of Different Grades of Abdominal Obesity on Testosterone Level, Erectile Dysfunction, and Clinical Coincidence. Am. J. Mens. Health 2017, 11, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Gandaglia, G.; Briganti, A.; Jackson, G.; Kloner, R.A.; Montorsi, F.; Montorsi, P.; Vlachopoulos, C. A Systematic Review of the Association between Erectile Dysfunction and Cardiovascular Disease. Eur. Urol. 2014, 65, 968–978. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.-Y.; Zhang, Y.-H.; Qin, L.-Q. Erectile Dysfunction and Risk of Cardiovascular Disease: Meta-Analysis of Prospective Cohort Studies. J. Am. Coll. Cardiol. 2011, 58, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Thompson, I.M.; Tangen, C.M.; Goodman, P.J.; Probstfield, J.L.; Moinpour, C.M.; Coltman, C.A. Erectile Dysfunction and Subsequent Cardiovascular Disease. JAMA 2005, 294, 2996–3002. [Google Scholar] [CrossRef]
- Batty, G.D.; Li, Q.; Czernichow, S.; Neal, B.; Zoungas, S.; Huxley, R.; Patel, A.; de Galan, B.E.; Woodward, M.; Hamet, P.; et al. Erectile dysfunction and later cardiovascular disease in men with type 2 diabetes: Prospective cohort study based on the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation) trial. J. Am. Coll. Cardiol. 2010, 56, 1908–1913. [Google Scholar] [CrossRef]
- Maiorino, M.I.; Bellastella, G.; Esposito, K. Lifestyle modifications and erectile dysfunction: What can be expected? Asian J. Androl. 2015, 17, 5–10. [Google Scholar] [CrossRef]
- Nicolosi, A.; Moreira, E.D.; Shirai, M.; Tambi, M.I.B.M.; Glasser, D.B. Epidemiology of erectile dysfunction in four countries: Cross-national study of the prevalence and correlates of erectile dysfunction. Urology 2003, 61, 201–206. [Google Scholar] [CrossRef]
- Parazzini, F.; Fabris, F.M.; Bortolotti, A.; CalabrÒ, A.; Chatenoud, L.; Colli, E.; Landoni, M.; Lavezzari, M.; Turchi, P.; Sessa, A.; et al. Frequency and determinants of erectile dysfunction in Italy. Eur. Urol. 2000, 37, 43–49. [Google Scholar] [CrossRef]
- Cao, S.; Yin, X.; Wang, Y.; Zhou, H.; Song, F.; Lu, Z. Smoking and Risk of Erectile Dysfunction: Systematic Review of Observational Studies with Meta-Analysis. PLoS ONE 2013, 8, e60443. [Google Scholar] [CrossRef]
- Arackal, B.S.; Benegal, V. Prevalence of sexual dysfunction in male subjects with alcohol dependence. Indian J. Psychiatry 2007, 49, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Bauer, S.R.; Breyer, B.N.; Stampfer, M.J.; Rimm, E.B.; Giovannucci, E.L.; Kenfield, S.A. Association of Diet with Erectile Dysfunction Among Men in the Health Professionals Follow-up Study. JAMA Netw. Open 2020, 3, e2021701. [Google Scholar] [CrossRef]
- Onyeji, I.C.; Clavijo, R.I. Testosterone replacement therapy and erectile dysfunction. Int. J. Impot. Res. 2022, 34, 698–703. [Google Scholar] [CrossRef]
- Alwani, M.; Yassin, A.; Talib, R.; Al-Qudimat, A.; Aboumarzouk, O.; Al-Zoubi, R.M.; Saad, F.; Haider, K.S.; Al Ansari, A. Cardiovascular Disease, Hypogonadism and Erectile Dysfunction: Early Detection, Prevention and the Positive Effects of Long-Term Testosterone Treatment: Prospective Observational, Real-Life Data. Vasc. Health Risk Manag. 2021, 17, 497–508. [Google Scholar] [CrossRef] [PubMed]
- GamalEl Din, S.F.; Salam, M.A.A.; Mohamed, M.S.; Ahmed, A.R.; Motawaa, A.T.; Saadeldin, O.A.; Elnabarway, R.R. Tribulus terrestris versus placebo in the treatment of erectile dysfunction and lower urinary tract symptoms in patients with late-onset hypogonadism: A placebo-controlled study. Urol. J. 2019, 86, 74–78. [Google Scholar] [CrossRef]
- Sood, R.; Sharma, D.; Goel, H.; Khattar, N.; Kulshreshtha, B.; Singh, K.K. The correlation between erectile dysfunction and metabolic syndrome in an Indian population: A cross-sectional observational study. Arab. J. Urol. 2019, 17, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Defeudis, G.; Mazzilli, R.; Tenuta, M.; Rossini, G.; Zamponi, V.; Olana, S.; Faggiano, A.; Pozzilli, P.; Isidori, A.M.; Gianfrilli, D. Erectile dysfunction and diabetes: A melting pot of circumstances and treatments. Diabetes Metab. Res. Rev. 2022, 38, e3494. [Google Scholar] [CrossRef]
- An, Y.; Xu, B.-T.; Wan, S.-R.; Ma, X.-M.; Long, Y.; Xu, Y.; Jiang, Z.-Z. The role of oxidative stress in diabetes mellitus-induced vascular endothelial dysfunction. Cardiovasc. Diabetol. 2023, 22, 237. [Google Scholar] [CrossRef] [PubMed]
- Fryk, E.; Silva, V.R.R.; Bauzá-Thorbrügge, M.; Schmelz, M.; Gan, L.-M.; Strindberg, L.; Jansson, P.-A. Feasibility of high-dose tadalafil and effects on insulin resistance in well-controlled patients with type 2 diabetes (MAKROTAD): A single-centre, double-blind, randomised, placebo-controlled, cross-over phase 2 trial. eClinicalMedicine 2023, 59, 101985. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Khan, M.A.; Sadaf, A.; Younus, H. A structural study on the protection of glycation of superoxide dismutase by thymoquinone. Int. J. Biol. Macromol. 2014, 69, 476–481. [Google Scholar] [CrossRef]
- Khan, M.A.; Anwar, S.; Aljarbou, A.N.; Al-Orainy, M.; Aldebasi, Y.H.; Islam, S.; Younus, H. Protective effect of thymoquinone on glucose or methylglyoxal-induced glycation of superoxide dismutase. Int. J. Biol. Macromol. 2014, 65, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Younus, H.; Anwar, S. Antiglycating activity of aloe vera gel extract and its active component aloin. J. Proteins Proteom. 2018. Available online: https://www.semanticscholar.org/paper/Antiglycating-activity-of-aloe-vera-gel-extract-and-Younus-Anwar/3afba14f74f47b1b1f2dd784af889cff5dae6cb1 (accessed on 10 December 2023).
- Younus, H.; Anwar, S. Prevention of non-enzymatic glycosylation (glycation): Implication in the treatment of diabetic complication. Int. J. Health Sci. 2016, 10, 261–277. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4825899/ (accessed on 10 December 2023). [CrossRef]
- Singh, V.P.; Bali, A.; Singh, N.; Jaggi, A.S. Advanced glycation end products and diabetic complications. Korean J. Physiol. Pharmacol. Off. J. Korean Physiol. Soc. Korean Soc. Pharmacol. 2014, 18, 1–14. [Google Scholar] [CrossRef]
- Fujita, N.; Ishida, M.; Iwane, T.; Suganuma, H.; Matsumoto, M.; Hatakeyama, S.; Yoneyama, T.; Hashimoto, Y.; Mikami, T.; Itoh, K.; et al. Association between Advanced Glycation End-Products, Carotenoids, and Severe Erectile Dysfunction. World J. Mens. Health 2023, 41, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Almatroudi, A.; Allemailem, K.S.; Joseph, R.J.; Khan, A.A.; Rahmani, A.H. Protective Effects of Ginger Extract against Glycation and Oxidative Stress-Induced Health Complications: An In Vitro Study. Processes 2020, 8, 468. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Almatroudi, A.; Anwar, S.; Babiker, A.Y.; Khan, A.A.; Alsahli, M.A.; Rahmani, A.H. Antioxidant, anti-inflammatory and hepatoprotective effects of olive fruit pulp extract: In vivo and in vitro study. J. Taibah Univ. Sci. 2020, 14, 1660–1670. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, H.; Kim, Y.H.; Chung, W.-S.; Suh, J.K.; Kim, S.J. Antioxidant Effect of Captopril and Enalapril on Reactive Oxygen Species-Induced Endothelial Dysfunction in the Rabbit Abdominal Aorta. Korean J. Thorac. Cardiovasc. Surg. 2013, 46, 14–21. [Google Scholar] [CrossRef]
- Morano, S.; Mandosi, E.; Fallarino, M.; Gatti, A.; Tiberti, C.; Sensi, M.; Gandini, L.; Buchetti, B.; Lenti, L.; Jannini, E.A.; et al. Antioxidant Treatment Associated with Sildenafil Reduces Monocyte Activation and Markers of Endothelial Damage in Patients with Diabetic Erectile Dysfunction: A Double-Blind, Placebo-Controlled Study. Eur. Urol. 2007, 52, 1768–1776. [Google Scholar] [CrossRef]
- Sheweita, S.A.; Meftah, A.A.; Sheweita, M.S.; Balbaa, M.E. Erectile dysfunction drugs altered the activities of antioxidant enzymes, oxidative stress and the protein expressions of some cytochrome P450 isozymes involved in the steroidogenesis of steroid hormones. PLoS ONE 2020, 15, e0241509. [Google Scholar] [CrossRef]
- Lubos, E.; Handy, D.E.; Loscalzo, J. Role of oxidative stress and nitric oxide in atherothrombosis. Front. Biosci. J. Virtual Libr. 2008, 13, 5323–5344. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2617738/ (accessed on 10 December 2023). [CrossRef]
- Anwar, S.; Raut, R.; Alsahli, M.A.; Almatroudi, A.; Alfheeaid, H.; Alzahrani, F.M.; Khan, A.A.; Allemailem, K.S.; Almatroodi, S.A.; Rahmani, A.H. Role of Ajwa Date Fruit Pulp and Seed in the Management of Diseases through In Vitro and In Silico Analysis. Biology 2022, 11, 78. [Google Scholar] [CrossRef]
- Ruan, Z.; Xie, X.; Yu, H.; Liu, R.; Jing, W.; Lu, T. Association between dietary inflammation and erectile dysfunction among US adults: A cross-sectional analysis of the National Health and Nutrition Examination Survey 2001–2004. Front. Nutr. 2022, 9, 930272. [Google Scholar] [CrossRef]
- Taskiran, M.; Dogan, K. The efficacy of systemic inflammatory response and oxidative stress in erectile dysfunction through multi-inflammatory index: A prospective cross-sectional analysis. J. Sex. Med. 2023, 20, 591–596. [Google Scholar] [CrossRef]
- Alcaidinho, A.; Nguyen, D.; Delouya, G.; Zorn, K.C.; Saad, F.; Taussky, D.; Liberman, D. The interaction between inflammation, urinary symptoms and erectile dysfunction in early-stage prostate cancer treated with brachytherapy. Andrologia 2021, 53, e14070. [Google Scholar] [CrossRef]
- Akintunde, J.K.; Olayinka, M.; Ugbaja, V.; Akinfenwa, C.; Akintola, T.; Akamo, A.; Bello, I. Downregulation of inflammatory erectile dysfunction by Mantisa religiosa egg-cake through NO-cGMP-PKG dependent NF-kB signaling cascade activated by mixture of salt intake. Toxicol. Rep. 2023, 10, 633–646. [Google Scholar] [CrossRef] [PubMed]
- Akintunde, J.K.; Akintola, T.E.; Aliu, F.H.; Fajoye, M.O.; Adimchi, S.O. Naringin regulates erectile dysfunction by abolition of apoptosis and inflammation through NOS/cGMP/PKG signalling pathway on exposure to Bisphenol-A in hypertensive rat model. Reprod. Toxicol. 2020, 95, 123–136. [Google Scholar] [CrossRef]
- Tristano, A.G. Impact of rheumatoid arthritis on sexual function. World J. Orthop. 2014, 5, 107–111. [Google Scholar] [CrossRef]
- Gordon, D.; Beastall, G.H.; Thomson, J.A.; Sturrock, R.D. Androgenic status and sexual function in males with rheumatoid arthritis and ankylosing spondylitis. Q. J. Med. 1986, 60, 671–679. [Google Scholar]
- Bay, L.T.; Graugaard, C.; Nielsen, D.S.; Möller, S.; Ellingsen, T.; Giraldi, A. Sexual Health and Dysfunction in Patients With Rheumatoid Arthritis: A Cross-sectional Single-Center Study. Sex. Med. 2020, 8, 615–630. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Mandal, S.; Bhowmik, P.; Gupta, P.; Bahal, B.; Sharma, P.K. Sexual function outcomes and risk factors of erectile dysfunction after surgical repair of penile fracture. Turk. J. Urol. 2021, 47, 106–112. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’Donoghue, F. Psychological management of erectile dysfunction and related disorders. Int. J. STD AIDS 1996, 7 (Suppl. S3), 9–12. [Google Scholar] [CrossRef]
- Ghanem, H.M.; Salonia, A.; Martin-Morales, A. SOP: Physical Examination and Laboratory Testing for Men with Erectile Dysfunction. J. Sex. Med. 2013, 10, 108–110. [Google Scholar] [CrossRef]
- Pastuszak, A.W. Current Diagnosis and Management of Erectile Dysfunction. Curr. Sex. Health Rep. 2014, 6, 164–176. [Google Scholar] [CrossRef]
- McMahon, C.G. Current diagnosis and management of erectile dysfunction. Med. J. Aust. 2019, 210, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Dean, R.C.; Lue, T.F. Physiology of Penile Erection and Pathophysiology of Erectile Dysfunction. Urol. Clin. N. Am. 2005, 32, 379–395. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.V.; Halls, J.; Patel, U. Investigation of erectile dysfunction. Br. J. Radiol. 2012, 85, S69–S78. [Google Scholar] [CrossRef] [PubMed]
- Fink, G. Encyclopedia of Stress; Academic Press: San Diego, CA, USA, 2007. [Google Scholar]
- Svalastog, A.L.; Donev, D.; Jahren Kristoffersen, N.; Gajović, S. Concepts and definitions of health and health-related values in the knowledge landscapes of the digital society. Croat. Med. J. 2017, 58, 431–435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Corbin, J.D.; Francis, S.H. Cyclic GMP phosphodiesterase-5: Target of sildenafil. J. Biol. Chem. 1999, 274, 13729–13732. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.; Rademaker, A.W.; McVary, K.T. Testosterone supplementation for erectile dysfunction: Results of a meta-analysis. J. Urol. 2000, 164, 371–375. [Google Scholar] [CrossRef]
- Buvat, J.; Lemaire, A.; Buvat-Herbaut, M. Human chorionic gonadotropin treatment of nonorganic erectile failure and lack of sexual desire: A double-blind study. Urology 1987, 30, 216–219. [Google Scholar] [CrossRef]
- Rahmani, A.H.; Babiker, A.Y.; Anwar, S. Hesperidin, a Bioflavonoid in Cancer Therapy: A Review for a Mechanism of Action through the Modulation of Cell Signaling Pathways. Molecules 2023, 28, 5152. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Alam, M.; Khatoon, F.; Fatima, U.; Elasbali, A.M.; Adnan, M.; Islam, A.; Hassan, M.I.; Snoussi, M.; De Feo, V. Natural products can be used in therapeutic management of COVID-19: Probable mechanistic insights. Biomed. Pharmacother. 2022, 147, 112658. [Google Scholar] [CrossRef]
- Clark, A.M. Natural products as a resource for new drugs. Pharm. Res. 1996, 13, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Masuku, N.P.; Unuofin, J.O.; Lebelo, S.L. Promising role of medicinal plants in the regulation and management of male erectile dysfunction. Biomed. Pharmacother. 2020, 130, 110555. [Google Scholar] [CrossRef]
- Sebastiani, F.; D’Alterio, C.; Vocca, C.; Gallelli, L.; Palumbo, F.; Cai, T.; Palmieri, A. Effectiveness of Silymarin, Sulforaphane, Lycopene, Green Tea, Tryptophan, Glutathione, and Escin on Human Health: A Narrative Review. Uro 2023, 3, 208–228. [Google Scholar] [CrossRef]
- Kamtchouing, P.; Mbongue, G.Y.F.; Dimo, T.; Watcho, P.; Jatsa, H.B.; Sokeng, S.D. Effects of Aframomum melegueta and Piper guineense on sexual behaviour of male rats. Behav. Pharmacol. 2002, 13, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Thakur, M.; Bhargava, S.; Dixit, V.K. Effect of Asparagus racemosus on sexual dysfunction in hyperglycemic male rats. Pharm. Biol. 2009, 47, 390–395. [Google Scholar] [CrossRef]
- Guohua, H.; Yanhua, L.; Rengang, M.; Dongzhi, W.; Zhengzhi, M.; Hua, Z. Aphrodisiac properties of Allium tuberosum seeds extract. J. Ethnopharmacol. 2009, 122, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Ratnasooriya, W.D.; Jayakody, J.R.A.C. Effects of aqueous extract of Alpinia calcarata rhizomes on reproductive competence of male rats. Acta Biol. Hung. 2006, 57, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Subramoniam, A.; Madhavachandran, V.; Ravi, K.; Anuja, V.S. Aphrodisiac Property of the Elephant Creeper Argyreia nervosa. J. Endocrinol. Reprod. 2007. Available online: https://www.semanticscholar.org/paper/Aphrodisiac-Property-of-the-Elephant-Creeper-Subramoniam-Madhavachandran/73e3d3795e48903bff6d32ad8d6e88ce66ce42f3 (accessed on 19 December 2023).
- Lopresti, A.L.; Drummond, P.D.; Smith, S.J. A Randomized, Double-Blind, Placebo-Controlled, Crossover Study Examining the Hormonal and Vitality Effects of Ashwagandha (Withania somnifera) in Aging, Overweight Males. Am. J. Mens. Health 2019, 13, 155798831983598. [Google Scholar] [CrossRef] [PubMed]
- Wankhede, S.; Langade, D.; Joshi, K.; Sinha, S.R.; Bhattacharyya, S. Examining the effect of Withania somnifera supplementation on muscle strength and recovery: A randomized controlled trial. J. Int. Soc. Sports Nutr. 2015, 12, 43. [Google Scholar] [CrossRef] [PubMed]
- Choowong-in, P.; Sattayasai, J.; Boonchoong, P.; Poodendaen, C.; Wu, A.T.; Tangsrisakda, N.; Sawatpanich, T.; Arun, S.; Uabundit, N.; Iamsaard, S. Protective effects of Thai Mucuna pruriens (L.) DC. var. pruriens seeds on sexual behaviors and essential reproductive markers in chronic unpredictable mild stress mice. J. Tradit. Complement. Med. 2022, 12, 402–413. [Google Scholar] [CrossRef] [PubMed]
- Suresh, S.; Prakash, S. Effect of Mucuna pruriens (Linn.) on Sexual Behavior and Sperm Parameters in Streptozotocin-Induced Diabetic Male Rat. J. Sex. Med. 2012, 9, 3066–3078. [Google Scholar] [CrossRef]
- Duangnin, N.; Phitak, T.; Pothacharoen, P.; Kongtawelert, P. In vitro and in vivo investigation of natural compounds from seed extract of Mucuna pruriens lacking l -DOPA for the treatment of erectile dysfunction. Asian Pac. J. Trop. Med. 2017, 10, 238–252. [Google Scholar] [CrossRef]
- Campos, A.R.; Lima, R.C.P.; Uchoa, D.E.A.; Silveira, E.R.; Santos, F.A.; Rao, V.S.N. Pro-erectile effects of an alkaloidal rich fraction from Aspidosperma ulei root bark in mice. J. Ethnopharmacol. 2006, 104, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-N.; Liao, C.-H.; Chen, K.-C.; Liu, S.-P.; Chiang, H.-S. Effect of Ginkgo biloba Extract (EGb-761) on Recovery of Erectile Dysfunction in Bilateral Cavernous Nerve Injury Rat Model. Urology 2015, 85, 1214.e7–1214.e15. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, N.S.; Sharma, V.; Dixit, V.K. Effect of Asteracantha longifolia seeds on the sexual behaviour of male rats. Nat. Prod. Res. 2011, 25, 1423–1431. [Google Scholar] [CrossRef]
- Hooshang, H.; Farahani, A.V.; Rezaeizadeh, H.; Forouzannia, S.K.; Alaeddini, F.; Ashraf, H.; Karimi, M. Efficacy of Date Palm Pollen in the Male Sexual Dysfunction after Coronary Artery Bypass Graft: A Randomized, Double-Blind, Clinical Trial. Evid.-Based Complement. Altern. Med. ECAM 2022, 2022, 5032681. [Google Scholar] [CrossRef]
- Vyas, R.; Kesari, K.K.; Lukac, N.; Slama, P.; Roychoudhury, S.; Sisodia, R. Radical scavenging activity of Chlorophytum borivilianum L. root extract and its protective role in cauda epididymal sperm integrity in Mus musculus after gamma irradiation. Front. Cell Dev. Biol. 2023, 11, 1064574. Available online: https://www.frontiersin.org/articles/10.3389/fcell.2023.1064574 (accessed on 14 December 2023). [CrossRef] [PubMed]
- Giribabu, N.; Kumar, K.E.; Rekha, S.S.; Muniandy, S.; Salleh, N. Chlorophytum borivilianum (Safed Musli) root extract prevents impairment in characteristics and elevation of oxidative stress in sperm of streptozotocin-induced adult male diabetic Wistar rats. BMC Complement. Altern. Med. 2014, 14, 291. [Google Scholar] [CrossRef]
- Khaki, A.; Fathiazad, F.; Nouri, M. Effects of Watermelon Seed Extract (Citrullus vulgaris) onSpermatogenesis in Rat. Int. J. Womens Health Reprod. Sci. 2013, 1, 99–104. [Google Scholar] [CrossRef]
- Ernst, E.; Pittler, M.H. Yohimbine for erectile dysfunction: A systematic review and meta-analysis of randomized clinical trials. J. Urol. 1998, 159, 433–436. [Google Scholar] [CrossRef]
- De Andrade, E.; de Mesquita, A.A.; Claro, J.d.A.; de Andrade, P.M.; Ortiz, V.; Paranhos, M.; Srougi, M.; Erdogrun, T. Study of the efficacy of Korean Red Ginseng in the treatment of erectile dysfunction. Asian J. Androl. 2007, 9, 241–244. [Google Scholar] [CrossRef]
- Pratte, M.A.; Nanavati, K.B.; Young, V.; Morley, C.P. An Alternative Treatment for Anxiety: A Systematic Review of Human Trial Results Reported for the Ayurvedic Herb Ashwagandha (Withania somnifera). J. Altern. Complement. Med. 2014, 20, 901–908. [Google Scholar] [CrossRef]
- Singh, N.; Bhalla, M.; de Jager, P.; Gilca, M. An Overview on Ashwagandha: A Rasayana (Rejuvenator) of Ayurveda. Afr. J. Tradit. Complement. Altern. Med. 2011, 8 (Suppl. S5), 208–213. [Google Scholar] [CrossRef] [PubMed]
- Mikulska, P.; Malinowska, M.; Ignacyk, M.; Szustowski, P.; Nowak, J.; Pesta, K.; Szeląg, M.; Szklanny, D.; Judasz, E.; Kaczmarek, G.; et al. Ashwagandha (Withania somnifera)-Current Research on the Health-Promoting Activities: A Narrative Review. Pharmaceutics 2023, 15, 1057. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.; Srivastava, M.K.; Pathak, A.K. Effect of standardized root extract of ashwagandha (Withania somnifera) on well-being and sexual performance in adult males: A randomized controlled trial. Health Sci. Rep. 2022, 5, e741. [Google Scholar] [CrossRef] [PubMed]
- Lampariello, L.R.; Cortelazzo, A.; Guerranti, R.; Sticozzi, C.; Valacchi, G. The Magic Velvet Bean of Mucuna pruriens. J. Tradit. Complement. Med. 2012, 2, 331–339. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942911/ (accessed on 14 December 2023). [CrossRef] [PubMed]
- Chauhan, N.S.; Sharma, V.; Dixit, V.K.; Thakur, M. A Review on Plants Used for Improvement of Sexual Performance and Virility. BioMed Res. Int. 2014, 2014, 868062. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Saha, S. An updated review on Taxonomy, Phytochemistry, Pharmacology and Toxicology of Macuna Pruriens. J. Pharmacogn. Phytochem. 2013, 2, 306–314. Available online: https://www.phytojournal.com/archives/2013.v2.i1.636/an-updated-review-on-taxonomy-phytochemistry-pharmacology-and-toxicology-of-macuna-pruriens (accessed on 14 December 2023).
- Jahromi, A.R.; Mosallanezhad, Z.; Hosini, F.S.; Jamali, S.; Sharifi, N. The effect of date palm on sexual function in infertile couples: A double-blind controlled clinical trial. BMC Res. Notes 2022, 15, 55. [Google Scholar] [CrossRef]
- Falahati, A.M.; Fallahi, S.; Allamehzadeh, Z.; Raieni, M.I.; Malekzadeh, K. Effects of Date Palm Pollen Supplementations on The Expression of PRDX1 and PRDX6 Genes in Infertile Men: A Controlled Clinical Trial. Int. J. Fertil. Steril. 2023, 17, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Singhal, S.; Kumar, N.; Rao, C.M.; Sumalatha, S.; Dave, J.; Dave, R.; Nandakumar, K. Standardised extract of safed musli (Chlorophytum borivilianum) increases aphrodisiac potential besides being safe in male Wistar rats. Andrologia 2016, 48, 1236–1243. [Google Scholar] [CrossRef]
- Munglue, P.; Kupittayanant, S.; Kupittayanant, P. Effect of Watermelon (Citrullus lanatus) Flesh Extract on Sexual Behavior of Male Rats. Chiang Mai Univ. J. Nat. Sci. 2014, 13, 519–527. [Google Scholar] [CrossRef]
- Naz, A.; Butt, M.S.; Sultan, M.T.; Qayyum, M.M.N.; Niaz, R.S. Watermelon lycopene and allied health claims. EXCLI J. 2014, 13, 650–660. [Google Scholar] [PubMed]
- Cormio, L.; De Siati, M.; Lorusso, F.; Selvaggio, O.; Mirabella, L.; Sanguedolce, F.; Carrieri, G. Oral L-citrulline supplementation improves erection hardness in men with mild erectile dysfunction. Urology 2011, 77, 119–122. [Google Scholar] [CrossRef]
- Tamler, R.; Mechanick, J.I. Dietary supplements and nutraceuticals in the management of andrologic disorders. Endocrinol. Metab. Clin. N. Am. 2007, 36, 533–552. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.C.; Tan, R.B.W.; Chung, E. Erectile dysfunction treatment and traditional medicine—Can East and West medicine coexist? Transl. Androl. Urol. 2017, 6, 91–100. [Google Scholar] [CrossRef]
- Yee, A.T.S.; Chan, L.T. Effectiveness of Ginseng in Treating Erectile Dysfunction: A Review Paper. OALib 2021, 8, e8043. [Google Scholar] [CrossRef]
- Cohen, A.J.; Bartlik, B. Ginkgo biloba for antidepressant-induced sexual dysfunction. J. Sex Marital. Ther. 1998, 24, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.F.; Maclennan, K.; Darlington, C.L. The neuroprotective properties of the Ginkgo biloba leaf: A review of the possible relationship to platelet-activating factor (PAF). J. Ethnopharmacol. 1996, 50, 131–139. [Google Scholar] [CrossRef]
- Rowland, D.L.; Tai, W. A review of plant-derived and herbal approaches to the treatment of sexual dysfunctions. J. Sex. Marital. Ther. 2003, 29, 185–205. [Google Scholar] [CrossRef] [PubMed]
- Paick, J.S.; Lee, J.H. An experimental study of the effect of ginkgo biloba extract on the human and rabbit corpus cavernosum tissue. J. Urol. 1996, 156, 1876–1880. [Google Scholar] [CrossRef]
- Chan, Y.S.; Cheng, L.N.; Wu, J.H.; Chan, E.; Kwan, Y.W.; Lee, S.M.; Leung, G.P.; Yu, P.H.; Chan, S.W. A review of the pharmacological effects of Arctium lappa (burdock). Inflammopharmacology 2011, 19, 245–254. [Google Scholar] [CrossRef]
- Cao, J.F.; Zhang, P.Y.; Xu, C.W.; Huang, T.T.; Bai, Y.G.; Chen, K.S. Effect of aqueous extract of Arctium lappa L. (burdock) roots on the sexual behavior of male rats. BMC Complement. Altern. Med. 2012, 12, 8. [Google Scholar] [CrossRef]
- Ahangarpour, A.; Oroojan, A.A.; Heidari, H.; Ghaedi, E.; Taherkhani, R. Effects of Hydro-alcoholic Extract from Arctium lappa L. (Burdock) Root on Gonadotropins, Testosterone, and Sperm Count and Viability in Male Mice with Nicotinamide/Streptozotocin-Induced Type 2 Diabetes. Malays. J. Med. Sci. 2015, 22, 25–32. [Google Scholar]
- Bhagwat, G.G. Pharmacognostic Study of Plant Euphorbia hirta L. J. Pharm. Res. 2008, 1, 39–43. [Google Scholar]
- Ogueke, C.C.; Ogbulie, J.N.; Okoli, I.C.; Anyanwu, B.N. Antibacterial Activities And Toxicological Potentials of Crude Ethanolic Extracts of Euphorbia hirta. J. Am. Sci. 2007, 3, 11–16. [Google Scholar]
- Yakubu, M.T.; Akanji, M.A.; Oladiji, A.T. Male sexual dysfunction and methods used in assessing medicinal plants with aphrodisiac potentials. Phcog Rev. 2007, 1, 49–56. [Google Scholar]
- Shamsa, A.; Hosseinzadeh, H.; Molaei, M.; Shakeri, M.T.; Rajabi, O. Evaluation of Crocus sativus L. (saffron) on male erectile dysfunction: A pilot study. Phytomedicine 2009, 16, 690–693. [Google Scholar] [CrossRef]
- Modabbernia, A.; Sohrabi, H.; Nasehi, A.A.; Raisi, F.; Saroukhani, S.; Jamshidi, A.; Tabrizi, M.; Ashrafi, M.; Akhondzadeh, S. Effect of saffron on fluoxetine-induced sexual impairment in men: Randomized double-blind placebo-controlled trial. Psychopharmacology 2012, 223, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh-Moghadam, H.; Nazari, S.M.; Shamsa, A.; Kamalinejad, M.; Esmaeeli, H.; Asadpour, A.A.; Khajavi, A. Effects of a Topical Saffron (Crocus sativus L) Gel on Erectile Dysfunction in Diabetics: A Randomized, Parallel-Group, Double-Blind, Placebo-Controlled Trial. J. Evid.-Based Complement. Altern. Med. 2015, 20, 283–286. [Google Scholar] [CrossRef]
- Xu, D.; Zhang, Y.; Bai, J.; Yuan, H.; Wang, T.; Liu, J.; Song, W.; Ma, D. Botanical drugs for treating erectile dysfunction: Clinical evidence. Front. Pharmacol. 2023, 14, 1232774. [Google Scholar] [CrossRef] [PubMed]
- Farnia, V.; Tatari, F.; Alikhani, M.; Shakeri, J.; Taghizadeh, M.; Karbasizadeh, H.; Sadeghi Bahmani, D.; Holsboer-Trachsler, E.; Brand, S. Rosa Damascena oil improved sexual function and testosterone in male patients with opium use disorder under methadone maintenance therapy-results from a double-blind, randomized, placebo-controlled clinical trial. Drug Alcohol Depend. 2017, 176, 117–125. [Google Scholar] [CrossRef]
- Farnia, V.; Shirzadifar, M.; Shakeri, J.; Rezaei, M.; Bajoghli, H.; Holsboer-Trachsler, E.; Brand, S. Rosa damascena oil improves SSRI-induced sexual dysfunction in male patients suffering from major depressive disorders: Results from a double-blind, randomized, and placebo-controlled clinical trial. Neuropsychiatr. Dis. Treat. 2015, 11, 625–635. [Google Scholar] [CrossRef]
- Anwar, S.; Kumar, V.; Raut, R. A review on factors causing vitamin b12 deficiency in pregnant women and infants. IJCRT 2024, 12, 1–13. [Google Scholar]
- Cheng, J.Y.W.; Ng, E.M.L.; Ko, J.S.N.; Chen, R.Y.L. Physical activity and erectile dysfunction: Meta-analysis of population-based studies. Int. J. Impot. Res. 2007, 19, 245–252. [Google Scholar] [CrossRef]
- Lu, Z.; Mo, Z. AB156. Homocysteine and vitamin B12: Risk factors for erectile dysfunction. Transl. Androl. Urol. 2014, 3 (Suppl. S1), AB156. [Google Scholar] [CrossRef]
- Niki, E. Role of vitamin E as a lipid-soluble peroxyl radical scavenger: In vitro and in vivo evidence. Free Radic. Biol. Med. 2014, 66, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-C.; Chin, C.-C.; Chen, C.-S.; Shindel, A.W.; Ho, D.-R.; Lin, C.-S.; Shi, C.-S. Chronic Cigarette Smoking Impairs Erectile Function through Increased Oxidative Stress and Apoptosis, Decreased nNOS, Endothelial and Smooth Muscle Contents in a Rat Model. PLoS ONE 2015, 10, e0140728. [Google Scholar] [CrossRef]
- Smith, S.J.; Lopresti, A.L.; Teo, S.Y.M.; Fairchild, T.J. Examining the Effects of Herbs on Testosterone Concentrations in Men: A Systematic Review. Adv. Nutr. 2021, 12, 744–765. [Google Scholar] [CrossRef] [PubMed]
- Cherdshewasart, W.; Nimsakul, N. Clinical trial of Buten superba, an alternative herbal treatment for erectile dysfunction. Asian J. Androl. 2003, 5, 243–246. [Google Scholar]
- Thakur, M.; Loeppert, R.; Praznik, W.; Dixit, V.K. Effect of some ayurvedic vajikarana rasayana herbs on heat induced testicular damage in male rats. J. Complement. Integr. Med. 2008, 5, 1–14. [Google Scholar] [CrossRef]
- Abd El-Rahman, H.A.; El-Badry, A.A.; Mahmoud, O.M.; Harraz, F.A. The effect of the aqueous extract of Cynomorium coccineum on the epididymal sperm pattern of the rat. Phytother. Res. 1999, 13, 248–250. [Google Scholar] [CrossRef]
- Thomford, N.E.; Senthebane, D.A.; Rowe, A.; Munro, D.; Seele, P.; Maroyi, A.; Dzobo, K. Natural Products for Drug Discovery in the 21st Century: Innovations for Novel Drug Discovery. Int. J. Mol. Sci. 2018, 19, 1578. [Google Scholar] [CrossRef]
- Simonsen, U.; Prieto, D.; Hernández, M.; Sáenz de Tejada, I.; García-Sacristán, A. Prejunctional alpha 2-adrenoceptors inhibit nitrergic neurotransmission in horse penile resistance arteries. J. Urol. 1997, 157, 2356–2360. [Google Scholar] [CrossRef]
- Sung, H.H.; Chae, M.R.; So, I.; Jeon, J.H.; Park, J.K.; Lee, S.W. Effects of ginsenoside on large-conductance K(Ca) channels in human corporal smooth muscle cells. Int. J. Impot. Res. 2011, 23, 193–199. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, S.D.; Kim, Y.J.; Huh, J.S.; Kim, S.W.; Sohn, D.W. Improvement of erectile function by Korean red ginseng (Panax ginseng) in a male rat model of metabolic syndrome. Asian J. Androl. 2013, 15, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Do, J.; Choi, S.; Choi, J.; Hyun, J.S. Effects and Mechanism of Action of a Tribulus terrestris Extract on Penile Erection. Korean J. Urol. 2013, 54, 183–188. [Google Scholar] [CrossRef]
- Partin, J.F.; Pushkin, Y.R. Tachyarrhythmia and hypomania with horny goat weed. Psychosomatics 2004, 45, 536–537. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chen, Y.; Wang, L.; Liu, Q.; Yang, S.; Wang, C. Advancing herbal medicine: Enhancing product quality and safety through robust quality control practices. Front. Pharmacol. 2023, 14, 1265178. [Google Scholar] [CrossRef] [PubMed]
- Bilia, A.R.; Piazzini, V.; Guccione, C.; Risaliti, L.; Asprea, M.; Capecchi, G.; Bergonzi, M.C. Improving on Nature: The Role of Nanomedicine in the Development of Clinical Natural Drugs. Planta Med. 2017, 83, 366–381. [Google Scholar] [CrossRef] [PubMed]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; del Pilar Rodriguez-Torres, M.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Musuamba, F.T.; Manolis, E.; Holford, N.; Cheung, S.; Friberg, L.E.; Ogungbenro, K.; Posch, M.; Yates, J.; Berry, S.; Thomas, N.; et al. Advanced Methods for Dose and Regimen Finding During Drug Development: Summary of the EMA/EFPIA Workshop on Dose Finding (London 4-5 December 2014). CPT Pharmacomet. Syst. Pharmacol. 2017, 6, 418–429. [Google Scholar] [CrossRef]
- Sander, O.; Magnusson, B.; Ludwig, I.; Jullion, A.; Meille, C.; Lorand, D.; Bornkamp, B.; Hinder, M.; Kovacs, S.J.; Looby, M. A framework to guide dose & regimen strategy for clinical drug development. CPT Pharmacomet. Syst. Pharmacol. 2021, 10, 1276–1280. [Google Scholar] [CrossRef] [PubMed]
- Eleazu, C.; Obianuju, N.; Eleazu, K.; Kalu, W. The role of dietary polyphenols in the management of erectile dysfunction-Mechanisms of action. Biomed. Pharmacother. 2017, 88, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.J.; Lin, H.; Wang, R. New advances in erectile technology. Ther. Adv. Urol. 2014, 6, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Belladelli, F.; Boeri, L.; Fallara, G.; Pozzi, E.; Corsini, C.; Cilio, S.; Capogrosso, P.; D’Arma, A.; Eisenberg, M.L.; Montorsi, F.; et al. Hyperestrogenism is associated with sexual function impairment in men-findings from a cross-sectional, real-life study. Andrology 2024, 12, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.S.; Cook, K.R.; Reilly, W.G. High estrogen in men after injectable testosterone therapy: The low T experience. Am. J. Mens Health 2015, 9, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, Y.; Ma, M.; Liu, F.; Shang, Y.; Yuan, Q.; Li, X.; Ju, B. Does erectile dysfunction predict cardiovascular risk? A cross-sectional study of clinical characteristics in patients with erectile dysfunction combined with coronary heart disease. Front. Cardiovasc. Med. 2024, 11, 1341819. [Google Scholar] [CrossRef]
- Lui, J.L.; Shaw, N.M.; Abbasi, B.; Hakam, N.; Breyer, B.N. Adverse reactions of PDE5 inhibitors: An analysis of the World Health Organization pharmacovigilance database. Andrology 2023, 11, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.E.; Rojanasarot, S.; Hincapie, A.L.; Guo, J.J. Safety profile and signal detection of phosphodiesterase type 5 inhibitors for erectile dysfunction: A Food and Drug Administration Adverse Event Reporting System analysis. Sex. Med. 2023, 11, qfad059. [Google Scholar] [CrossRef]
- Anwar, S.; Raut, R.; Kanwal, B.; Yahia, E.A. Vitamin B 12 deficiency and increased susceptibility and severity of COVID-19: A review. Int. J. Creat. Res. Thoughts 2022, 10, 623–651. [Google Scholar]
- Available online: https://www.ebmconsult.com/articles/levels-of-evidence-and-recommendations (accessed on 3 April 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).