Is Urine Egress into the Female Urethra a Risk Factor for UTI?
Abstract
1. Introduction
2. Risks for Urinary Tract Infections
3. Physiology of Urethral Closure and Urine Egress
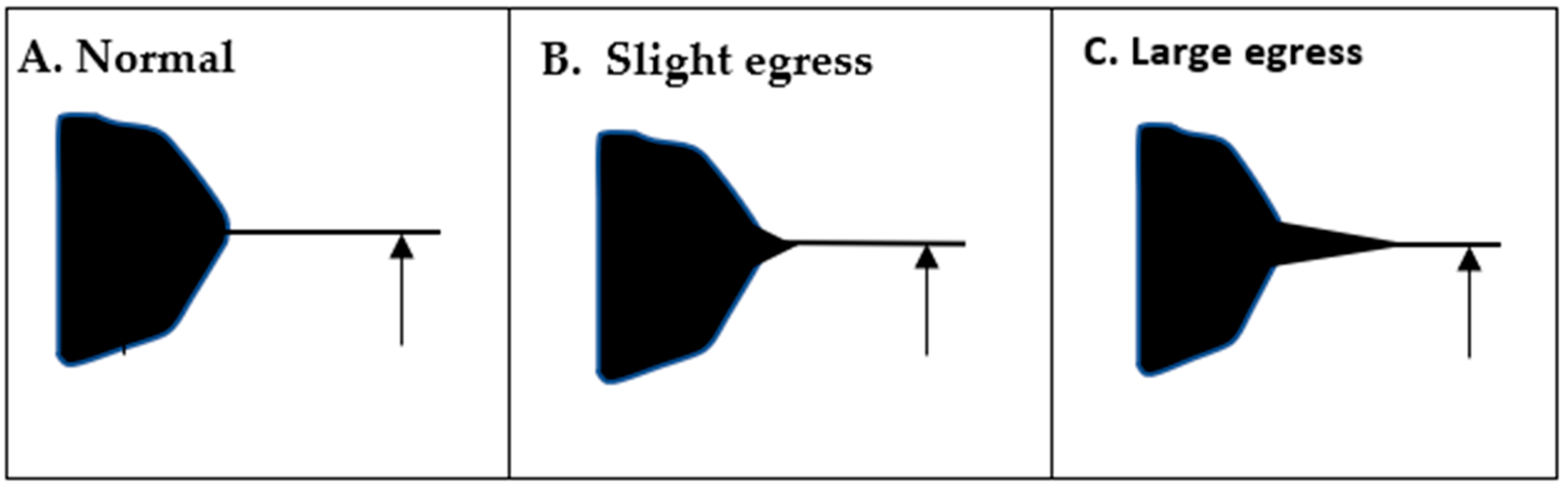
4. Diagnosis of Urine Egress
5. Possible Urine Egress in Clinical Practice
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fowler, C.J.; Griffiths, D.; de Groat, W.C. The neural control of micturition. Nat. Rev. Neurosci. 2008, 9, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Foxman, B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010, 7, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.V. Recurrent urinary tract infections. Best Pract. Clin. Obstet. Gynaecol. 2005, 19, 862–873. [Google Scholar] [CrossRef]
- Kodner, C.M.; Gupton, T.E.K. Recurrent urinary tract infections in women: Diagnosis and management. Am. Fam. Physician 2010, 82, 638–643. [Google Scholar] [PubMed]
- Musco, S.; Giammò, A.; Savoca, F.; Gemma, L.; Geretto, P.; Soligo, M.; Sacco, E.; Del Popolo, G.; Marzi, V.L. How to Prevent Catheter-Associated Urinary Tract Infections: A Reappraisal of Vico’s Theory—Is History Repeating Itself? J. Clin. Med. 2022, 11, 3415. [Google Scholar] [CrossRef] [PubMed]
- Czajkowski, K.; Broś-Konopielko, M.; Teliga-Czajkowska, J. Urinary tract infection in women. Menopause Rev. 2021, 20, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, F.; Tu, L.M.; Carroll, M.S.; Morin, M. Agreement between simple catheter method and 3D transperineal ultrasound for assessing urethral length measurement before stress urinary incontinence treatment. Neurourol. Urodyn. 2018, 37, 2875–2880. [Google Scholar] [CrossRef] [PubMed]
- Kirby, A.C.; Tan-Kim, J.; Nager, C.W. Measurement of dynamic urethral pressures with a high resolution manometry system in continent and incontinent women. Female Pelvic Med. Reconstr. Surg. 2015, 21, 106–110. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Aoki, Y.; Brown, H.W.; Brubaker, L.; Cornu, J.N.; Daly, J.O.; Cartwright, R. Urinary incontinence in women. Nat. Rev. Dis. Primers 2017, 3, 17042–17086. [Google Scholar] [CrossRef] [PubMed]
- Sand, P.K.; Bowen, L.W.; Ostergard, D.R. The prognostic significance of augmentation of urethral closure pressure and functional length. Int. J. Gynaecol. Obstet. 1990, 33, 135–139. [Google Scholar] [CrossRef]
- Herschorn, S. Female pelvic floor anatomy: The pelvic floor supporting structures, and pelvic organs. Rev. Urol. 2004, 6 (Suppl. 5), 2–10. [Google Scholar]
- Ghoniem, G.; Stanford, E.; Kenton, K.; Achtari, C.; Goldberg, R.; Mascarenhas, T.; Parekh, M.; Tamussino, K.; Tosson, S.; Lose, G.; et al. Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2008, 19, 5–33. [Google Scholar] [CrossRef] [PubMed]
- Khizer, Z.; Sadia, A.; Sharma, R.; Farhaj, S.; Nirwan, J.S.; Kakadia, P.G.; Hussain, T.; Yousaf, A.M.; Shahzad, Y.; Conway, B.R. Drug Delivery Approaches for Managing Overactive Bladder (OAB): A Systematic Review. Pharmaceuticals 2021, 14, 409. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walter, J.; Wheeler, J.; Khan, A. Is Urine Egress into the Female Urethra a Risk Factor for UTI? Uro 2022, 2, 199-203. https://doi.org/10.3390/uro2040024
Walter J, Wheeler J, Khan A. Is Urine Egress into the Female Urethra a Risk Factor for UTI? Uro. 2022; 2(4):199-203. https://doi.org/10.3390/uro2040024
Chicago/Turabian StyleWalter, James, John Wheeler, and Aasma Khan. 2022. "Is Urine Egress into the Female Urethra a Risk Factor for UTI?" Uro 2, no. 4: 199-203. https://doi.org/10.3390/uro2040024
APA StyleWalter, J., Wheeler, J., & Khan, A. (2022). Is Urine Egress into the Female Urethra a Risk Factor for UTI? Uro, 2(4), 199-203. https://doi.org/10.3390/uro2040024





