Bio-Artificial Liver Support System: A Prospective Future Therapy
Abstract
1. Introduction
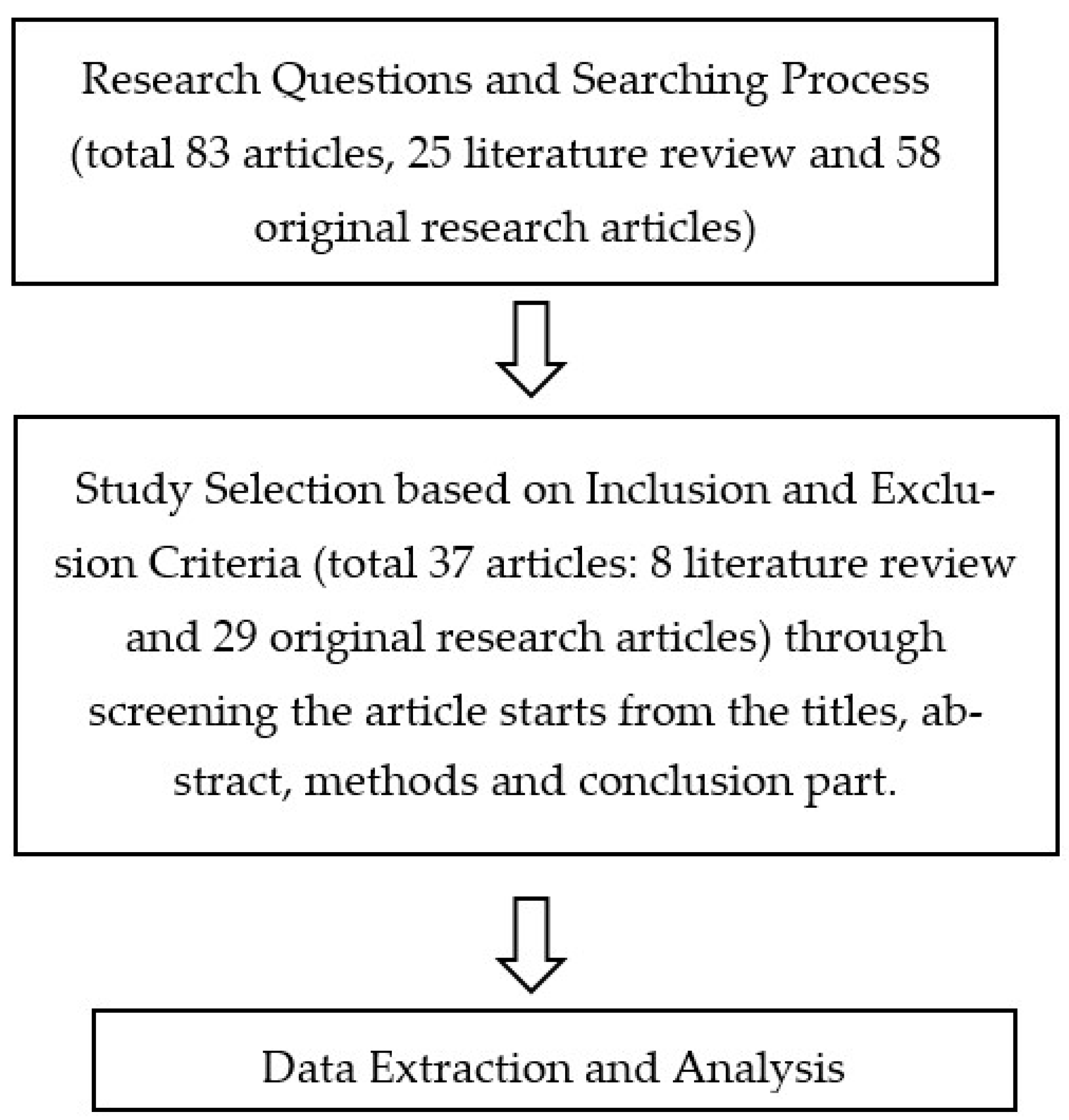
2. Materials and Methods
- What is the method of liver support system for treating chronic and acute liver failure?
- How do the advantages and disadvantages of each conventional liver support system provide liver failure treatment?
- What is the bio-artificial liver support system method, and how can it treat liver failure compared to the other systems?
- ScienceDirect (http://www.sciencedirect.com) (accessed on 15 June 2022)
- SpringerLink (http://www.springer.com/in/) (accessed on 25 June 2022)
- ProQuest (http://www.proquest.com) (accessed on 30 June 2022)
- PubMed (https://pubmed.ncbi.nlm.nih.gov/) (accessed on 25 June 2022)
- Elsevier (https://www.elsevier.com/en-xs) (accessed on 10 June 2022)
- Cochrane (https://www.cochrane.org/) (accessed on 15 June 2022)
3. Results
3.1. Liver Support System
3.1.1. Molecular Adsorbent Recirculation System (MARS)
3.1.2. Single-Pass Albumin Dialysis (SPAD)
3.2. Bio-Artificial Liver Support System
3.2.1. Animal Subject Study
3.2.2. Human Subject Study
3.3. Induced Pluripotent Stem Cells/iPSC
Animal Subject Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Angeli, P.; Bernardi, M.; Villanueva, C. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J. Hepatol. 2018, 69, 406–460. [Google Scholar] [CrossRef] [PubMed]
- Tandon, R.; Froghi, S. Systematic review of artificial liver support systems: Current clinical challenges. HPB 2020, 22, S377. [Google Scholar] [CrossRef]
- Bernal, W.; Lee, W.M.; Wendon, J. Acute liver failure: A curable disease by 2024? J. Hepatol. 2015, 62, S112–S120. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.J.; Royer, A.; John, S. Acute Liver Failure. StatPearls 2018, 30, 12–17. [Google Scholar]
- García Martínez, J.J.; Bendjelid, K. Artificial liver support systems: What is new over the last decade? Ann. Intensive Care 2018, 8, 109. [Google Scholar] [CrossRef]
- Iansante, V.; Mitry, R.R.; Filippi, C. Human hepatocyte transplantation for liver disease: Current status and future perspectives. Pediatr. Res. 2018, 83, 232–240. [Google Scholar] [CrossRef]
- Cardoso, F.S.; Marcelino, P.; Bagulho, L. Acute liver failure: An up-to-date approach. J. Crit. Care 2017, 39, 25–30. [Google Scholar] [CrossRef]
- MacDonald, A.J.; Karvellas, C.J. Emerging Role of Extracorporeal Support in Acute and Acute-on-Chronic Liver Failure: Recent Developments. Semin. Respir. Crit. Care Med. 2018, 39, 625–634. [Google Scholar] [CrossRef]
- Schmuck, R.B.; Nawrot, G.H.; Fikatas, P. Single Pass Albumin Dialysis-A Dose-Finding Study to Define Optimal Albumin Concentration and Dialysate Flow. Artif. Organs 2017, 41, 153–161. [Google Scholar] [CrossRef]
- Matar, A.J.; Subramanian, R. Extracorporeal Liver Support: A Bridge to Somewhere. Clin. Liver Dis. 2021, 18, 274–279. [Google Scholar] [CrossRef]
- Karvellas, C.J.; Subramanian, R.M. Current Evidence for Extracorporeal Liver Support Systems in Acute Liver Failure and Acute-on-Chronic Liver Failure. Crit. Care Clin. 2016, 32, 439–451. [Google Scholar] [CrossRef]
- Wiesmann, T.; Hoenl, D.; Wulf, H. Extracorporeal liver support: Trending epidemiology and mortality—A nationwide database analysis 2007–2015. BMC Gastroenterol. 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Alshamsi, F.; Alshammari, K.; Belly-Cote, E. Extracorporeal Liver Support in Patients With Acute or Acute on Chronic Liver Failure: A Systematic Review and Meta-Analysis of Randomized Trials. Chest 2019, 155, 116A. [Google Scholar] [CrossRef]
- Pocze, B.; Fazakas, J.; Zádori, G. MARS therapy, the bridging to liver retransplantation—Three cases from the Hungarian liver transplant program. Interv. Med. Appl. Sci. 2013, 5, 70. [Google Scholar] [CrossRef]
- Bañares, R.; Catalina, M.V.; Vaquero, J. Molecular adsorbent recirculating system and bioartificial devices for liver failure. Clin. Liver Dis. 2014, 18, 945–956. [Google Scholar] [CrossRef]
- Cisneros-Garza, L.E.; del Rosario Muñoz-Ramírez, M.; Muñoz-Espinoza, L.E. The molecular adsorbent recirculating system as a liver support system. Summary of Mexican experience. Ann. Hepatol. 2014, 13, 240–247. [Google Scholar] [CrossRef]
- Kanjo, A.; Ocskay, K.; Gede, N. Efficacy and safety of liver support devices in acute and hyperacute liver failure: A systematic review and network meta-analysis. Sci. Rep. 2021, 11, 1–10. [Google Scholar] [CrossRef]
- Hanish, S.I.; Stein, D.M.; Scalea, J.R. Molecular Adsorbent Recirculating System Effectively Replaces Hepatic Function in Severe Acute Liver Failure. Ann. Surg. 2017, 266, 677–684. [Google Scholar] [CrossRef]
- A case report therapeutic plasma exchange and singlepass albumin dialysis in a 10-month-old girl with dengue shock syndrome in Thailand | The Southeast Asian Journal of Tropical Medicine and Public Health. Available online: https://journal.seameotropmednetwork.org/index.php/jtropmed/article/view/235 (accessed on 10 April 2022).
- Sparrelid, E.; Gilg, S.; van Gulik, T.M. Systematic review of MARS treatment in post-hepatectomy liver failure. HPB 2020, 22, 950–960. [Google Scholar] [CrossRef]
- He, Y.T.; Qi, Y.N.; Zhang, B.Q. Bioartificial liver support systems for acute liver failure: A systematic review and meta-analysis of the clinical and preclinical literature. World J. Gastroenterol. 2019, 25, 3634–3648. [Google Scholar] [CrossRef]
- Gerth, H.U.; Pohlen, M.; Thölking, G. Molecular adsorbent recirculating system (MARS) in acute liver injury and graft dysfunction: Results from a case-control study. PLoS ONE 2017, 12, e0175529. [Google Scholar] [CrossRef] [PubMed]
- Kaps, L.; Ahlbrand, C.J.; Gadban, R. Applicability and safety of discontinuous ADVanced Organ Support (ADVOS) in the treatment of patients with acute-on-chronic liver failure (ACLF) outside of intensive care. PLoS ONE 2021, 16, e0249342. [Google Scholar] [CrossRef] [PubMed]
- Bañares, R.; Nevens, F.; Larsen, F.S. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: The RELIEF trial. Hepatology 2013, 57, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.F.; Tseng, C.Y.; Wang, H.W. Rapid generation of mature hepatocyte-like cells from human induced pluripotent stem cells by an efficient three-step protocol. Hepatology 2012, 55, 1193–1203. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.N.; Underhill, G.H.; Zaret, K.S. Cell and Tissue Engineering for Liver Disease. Sci. Transl. Med. 2014, 6, 245sr2. [Google Scholar] [CrossRef]
- Selden, C.; Bundy, J.; Erro, E. A clinical-scale BioArtificial Liver, developed for GMP, improved clinical parameters of liver function in porcine liver failure. Sci. Rep. 2017, 7, 14518. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, D.H.; Lee, S. Functional Evaluation of a Bioartificial Liver Support System Using Immobilized Hepatocyte Spheroids in a Porcine Model of Acute Liver Failure. Sci. Rep. 2017, 7, 3804. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, S.; He, X. A breakthrough trial of an artificial liver without systemic heparinization in hyperbilirubinemia beagle models. Bioact. Mater. 2023, 20, 651–662. [Google Scholar] [CrossRef]
- Wu, G.; Wu, D.; Lo, J. A bioartificial liver support system integrated with a DLM/GelMA-based bioengineered whole liver for prevention of hepatic encephalopathy: Via enhanced ammonia reduction. Biomater. Sci. 2020, 8, 2814–2824. [Google Scholar] [CrossRef]
- Pourcher, G.; El-Kehdy, H.; Kanso, F. Volumetric Portal Embolization: A New Concept to Improve Liver Regeneration and Hepatocyte Engraftment. Transplantation 2016, 100, 344–354. [Google Scholar] [CrossRef]
- Du, Y.; Wang, J.; Jia, J. Human hepatocytes with drug metabolic function induced from fibroblasts by lineage reprogramming. Cell Stem Cell 2014, 14, 394–403. [Google Scholar] [CrossRef]
- Guha, P.; Morgan, J.W.; Mostoslavsky, G. lack of immune response to differentiated cells derived from syngeneic induced pluripotent stem cells. Cell Stem Cell 2013, 12, 407–412. [Google Scholar] [CrossRef]
- Fitzpatrick, E.; Wu, Y.; Dhadda, P. Coculture with mesenchymal stem cells results in improved viability and function of human hepatocytes. Cell Transplant. 2015, 24, 73–83. [Google Scholar] [CrossRef]
- Yagi, H.; Fukumitsu, K.; Fukuda, K. Human-scale whole-organ bioengineering for liver transplantation: A regenerative medicine approach. Cell Transplant. 2013, 22, 231–242. [Google Scholar] [CrossRef]
- Wang, A.; Kuriata, O.; Xu, F. A Survival Model of In Vivo Partial Liver Lobe Decellularization Towards In Vivo Liver Engineering. Tissue Eng. Part C Methods 2020, 26, 402–417. [Google Scholar] [CrossRef]
- Hussein, K.H.; Park, K.M.; Kang, K.S. Heparin-gelatin mixture improves vascular reconstruction efficiency and hepatic function in bioengineered livers. Acta Biomater. 2016, 38, 82–93. [Google Scholar] [CrossRef]
- Li, Y.; Wu, Q.; Wang, Y. Construction of bioengineered hepatic tissue derived from human umbilical cord mesenchymal stem cells via aggregation culture in porcine decellularized liver scaffolds. Xenotransplantation 2017, 24, e12285. [Google Scholar] [CrossRef]
- Balasiddaiah, A.; Moreno, D.; Guembe, L. Hepatic differentiation of mouse iPS cells and analysis of liver engraftment potential of multistage iPS progeny. J. Physiol. Biochem. 2013, 69, 835–845. [Google Scholar] [CrossRef]
- Shi, X.L.; Gao, Y.; Yan, Y. Improved survival of porcine acute liver failure by a bioartificial liver device implanted with induced human functional hepatocytes. Cell Res. 2016, 26, 206–216. [Google Scholar] [CrossRef]
- Huang, P.; Zhang, L.; Gao, Y. Direct reprogramming of human fibroblasts to functional and expandable hepatocytes. Cell Stem Cell 2014, 14, 370–384. [Google Scholar] [CrossRef]
- Zhu, S.; Rezvani, M.; Harbell, J. Mouse liver repopulation with hepatocytes generated from human fibroblasts. Nature 2014, 508, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Iwamuro, M.; Shiraha, H.; Nakaji, S. A preliminary study for constructing a bioartificial liver device with induced pluripotent stem cell-derived hepatocytes. Biomed. Eng. Online 2012, 11, 93. [Google Scholar] [CrossRef] [PubMed]
- Hou, P.; Li, Y.; Zhang, X. Pluripotent stem cells induced from mouse somatic cells by small-molecule compounds. Science 2013, 341, 651–654. [Google Scholar] [CrossRef] [PubMed]
- Asgari, S.; Moslem, M.; Bagheri-Lankarani, K. Differentiation and transplantation of human induced pluripotent stem cell-derived hepatocyte-like cells. Stem Cell Rev. Rep. 2013, 9, 493–504. [Google Scholar] [CrossRef]
- Pareja, E.; Gómez-Lechón, M.J.; Tolosa, L. Induced pluripotent stem cells for the treatment of liver diseases: Challenges and perspectives from a clinical viewpoint. Ann. Transl. Med. 2020, 8, 566. [Google Scholar] [CrossRef]
- Fiorotto, R.; Amenduni, M.; Mariotti, V. Liver diseases in the dish: iPSC and organoids as a new approach to modeling liver diseases. Biochim. Biophys. Acta (BBA)—Mol. Basis Dis. 2019, 1865, 920–928. [Google Scholar] [CrossRef]
- Nevens, F.; Laleman, W. Artificial liver support devices as treatment option for liver failure. Best Pract. Res. Clin. Gastroenterol. 2012, 26, 17–26. [Google Scholar] [CrossRef]

| No. | Liver Support Method | Advantages | Disadvantages |
|---|---|---|---|
| 1. | Single-Pass Albumin Dialysis (SPAD) | Significant reduction (>50%) in total plasma bilirubin, conjugated bilirubin, blood urea nitrogen, and creatinine | Clinical studies about effectiveness in toxin removal are still limited (only 1–2 studies from the last five years). |
| 3. | Molecular Adsorbent Recirculation System (MARS) | Eliminate toxins, and repair liver failure symptoms (toxin blood level 0%) Reduction in bilirubin, bile acid, ammonia, urea, lactate, and creatinine levels (>50% compared to previous levels) MARS can stabilize the anhepatic condition in ALF and ACLF for 96 h before transplantation. Effective in clearing bile acid compared to SPAD (bile acid clear 100%) A significant increase (50%) in mean arterial pressure and systemic blood circulation resistance without a change in heart index. Plasma renin activity reduction (up to 50%). | The survival rate has not been reported (no studies). The mortality percentage did not significantly reduce (compared to the previous study, 0% reduction). Thrombocytopenia, coagulopathy, and bleeding risks up to 20–30%. MARS is relatively more expensive (cost >1000 USD in Europe) |
| 4. | Bio-artificial Liver Support System (BALSS) | Improve neurological state and liver and kidney functions to bridge transplantation (the function status is usually based on assessment score). | BALSS might not reduce ALF deaths, but the survival rate is still controversial. It can either reduce or increase ALF deaths (the percentages are 50%) The delivery of bioreactors is expensive and impractical (it costs USD >500) Limited study and case reports (there have only been 1–2 studies in the last five years.) The risk of zoonosis disease transmission is up to 30%. |
| 5. | Induced-Pluripotent Stem Cells/iPSC | Increase the viability and function of human hepatocytes (from 20 to >40%) Improve the regeneration of liver function and facilitate a speedy recovery (up to 100%). | There is no study with human subjects reported. Therefore, the method should be produced on a larger scale of up to <100 subjects. |
| No. | Liver Support Method | Human Subject | Animal Subject |
|---|---|---|---|
| 1. | Hepatocyte-based Bio-Artificial Liver (BAL) | Not yet used in clinical trials. RCT meta-analysis results showed that BAL might not reduce ALF deaths. | Pre-clinically modified and applied to large animals. As a result, six out of seven patients with liver failure bridged to transplantations, and one recovered without transplantation. |
| 2. | Single-Pass Albumin Dialysis | Twelve patients with ALF and CLF were treated, and there was a reduction in total bilirubin levels. However, clinical experience in toxic removal is still limited. [48] | One of the simplest methods for eliminating toxins and water-soluble compounds from albumin has been proven to be single-pass albumin dialysis (SPAD), which was tested on five pigs. |
| 3. | Molecular Adsorbent Recirculation System (MARS) | A random clinical trial in 23 patients with ALF and CLF showed a reduction in bilirubin level. MARS has been proven to eliminate toxins and stabilize the anhepatic condition in humans. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jasirwan, C.O.M.; Muradi, A.; Antarianto, R.D. Bio-Artificial Liver Support System: A Prospective Future Therapy. Livers 2023, 3, 65-75. https://doi.org/10.3390/livers3010006
Jasirwan COM, Muradi A, Antarianto RD. Bio-Artificial Liver Support System: A Prospective Future Therapy. Livers. 2023; 3(1):65-75. https://doi.org/10.3390/livers3010006
Chicago/Turabian StyleJasirwan, Chyntia Olivia Maurine, Akhmadu Muradi, and Radiana Dhewayani Antarianto. 2023. "Bio-Artificial Liver Support System: A Prospective Future Therapy" Livers 3, no. 1: 65-75. https://doi.org/10.3390/livers3010006
APA StyleJasirwan, C. O. M., Muradi, A., & Antarianto, R. D. (2023). Bio-Artificial Liver Support System: A Prospective Future Therapy. Livers, 3(1), 65-75. https://doi.org/10.3390/livers3010006






