Factors Influencing USA Women to Receive the Human Papillomavirus Vaccine: A Systematic Literature Review
Abstract
1. Introduction
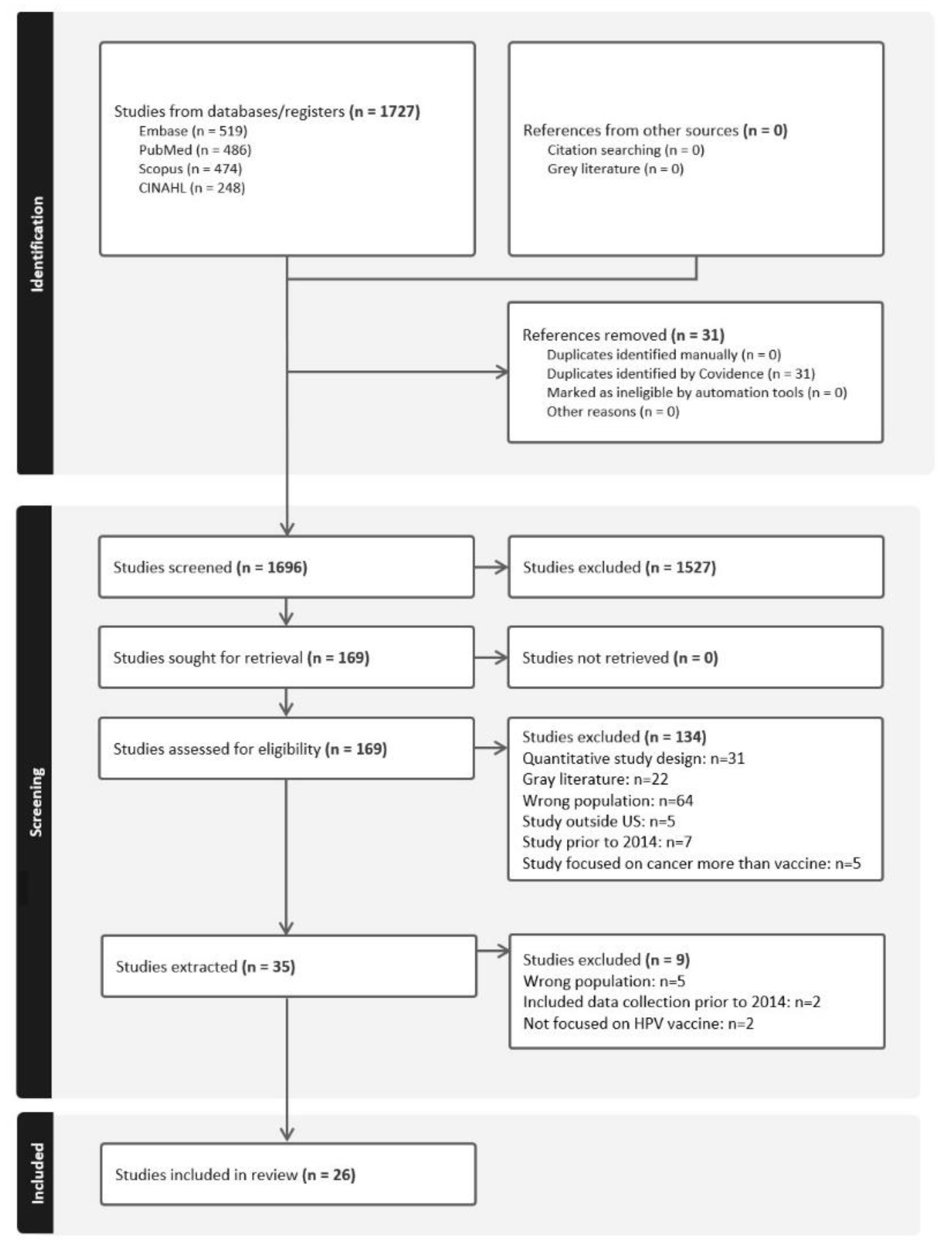
2. Methods
2.1. Selection Criteria: Inclusion and Exclusion
2.2. Search Sources
2.3. Study Selection
2.4. Data Collection and Extraction
3. Results
3.1. Theme 1: Facilitators Perceived by Women to Uptake the HPV Vaccine (4 Studies)
3.2. Theme 2: Barriers Perceived by Women to Uptake the HPV Vaccine (13 Studies Focused Only on Barriers)
3.3. Theme 3: Barriers and Facilitators Perceived by Women to Uptake the HPV Vaccine (9 Studies)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. PubMed/MEDLINE Search Strategy
- ((((((“Papillomavirus Infections”[Mesh]) OR “Papillomaviridae”[Mesh]) OR “Uterine Cervical Neoplasms”[Mesh]) OR “Alphapapillomavirus”[Mesh]) OR (human papilloma virus OR HPV OR papillomavirus infections OR papillomaviridae OR uterine cervial neoplasms OR cervical cancer OR alphapapillomavirus))
- AND
- ((((“Papillomavirus Vaccines”[Mesh]) OR “Immunization Programs”[Mesh]) OR (“Vaccination”[Mesh] OR “Vaccination Refusal”[Mesh] OR “Vaccination Hesitancy”[Mesh] OR “Anti-Vaccination Movement”[Mesh])) OR (papillomavirus vaccines OR immunization programs OR (vaccination AND (refusal OR hesitancy OR anti)) OR anti-vaccination movement OR anti-vax OR antivax OR HPV vaccine OR gardasil OR cervarix)))
- AND
- (((“Health Knowledge, Attitudes, Practice”[Mesh]) OR “Patient Acceptance of Health Care”[Mesh]) OR ((patient OR parent OR mother OR daughter OR female OR woman) AND (parent OR knowledge OR attitude OR practice OR acceptance OR perspective OR stigma OR communication OR education))
- AND
- ((((“Qualitative Research”[Mesh]) OR (“Interview” [Publication Type] OR “Interviews as Topic”[Mesh])) OR “Focus Groups”[Mesh]) OR (qualitative OR interview* OR focus group*)) AND
- (2009:2023[pdat])
References
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664. [Google Scholar] [CrossRef]
- Plummer, M.; Schiffman, M.; Castle Philip, E.; Maucort-Boulch, D.; Wheeler Cosette, M. A 2-Year Prospective Study of Human Papillomavirus Persistence among Women with a Cytological Diagnosis of Atypical Squamous Cells of Undetermined Significance or Low-Grade Squamous Intraepithelial Lesion. J. Infect. Dis. 2007, 195, 1582–1589. [Google Scholar] [CrossRef]
- Castle, P.E.; Fetterman, B.; Akhtar, I.; Husain, M.; Gold, M.A.; Guido, R.; Glass, A.G.; Kinney, W. Age-appropriate use of human papillomavirus vaccines in the U.S. Gynecol. Oncol. 2009, 114, 365–369. [Google Scholar] [CrossRef]
- Saraiya, M.; Unger, E.R.; Thompson, T.D.; Lynch, C.F.; Hernandez, B.Y.; Lyu, C.W.; Steinau, M.; Watson, M.; Wilkinson, E.J.; Hopenhayn, C.; et al. US assessment of HPV types in cancers: Implications for current and 9-valent HPV vaccines. J. Natl. Cancer Inst. 2015, 107, djv086. [Google Scholar] [CrossRef]
- American Cancer Society. Cancer Statistics Center. 2018. Available online: https://cancerstatisticscenter.cancer.org/ (accessed on 19 April 2024).
- de Sanjose, S.; Quint, W.G.V.; Alemany, L.; Geraets, D.T.; Klaustermeier, J.E.; Lloveras, B.; Tous, S.; Felix, A.; Bravo, L.E.; Shin, H.-R.; et al. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010, 11, 1048–1056. [Google Scholar] [CrossRef]
- Center for Disease Control. Cervical Cancer Statistics. Available online: https://www.cdc.gov/cancer/cervical/statistics/ (accessed on 26 March 2024).
- World Health Organization. Cervical Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed on 26 March 2024).
- Chesson, H.W.; Laprise, J.-F.; Brisson, M.; Martin, D.; Ekwueme, D.U.; Markowitz, L.E. The Estimated Lifetime Medical Cost of Diseases Attributable to Human Papillomavirus Infections Acquired in 2018. Sex. Transm. Dis. 2021, 48, 278–284. [Google Scholar] [CrossRef]
- Cervarix [Package Insert]; GlaxoSmithKline: Research Triangle Park, NC, USA, 2019.
- Gardasil [Package Insert]; Merck and Co., Inc.: Whitehouse Station, NJ, USA, 2015.
- Gardasil 9 [Package Insert]; Merck Sharp and Dohme LLC, Inc.: Rahway, NJ, USA, 2023.
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR. Recomm. Rep. 2021, 70, 1183–1190. [Google Scholar] [CrossRef]
- Pingali, C.; Yankey, D.; Elam-Evans, L.D.; Markowitz, L.E.; Williams, C.L.; Fredua, B.; McNamara, L.A.; Stokley, S.; Singleton, J.A. National, Regional, State, and Selected Local Area Vaccination Coverage among Adolescents Aged 13–17 Years—United States, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 1183–1190. [Google Scholar] [CrossRef]
- Hubbard, D.; Shrestha, S.; Levitan, E.B.; Yun, H. Human Papillomavirus Vaccination Schedule: Adherence Among Commercially Insured Adolescents and Young Adults in the United States, 2011–2017. Am. J. Public Health 2020, 110, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Boersma, P.; Black, L.I. Human Papillomavirus Vaccination among Adults Aged 18–26, 2013–2018. NCHS Data Brief 2020. Available online: https://www.cdc.gov/nchs/data/databriefs/db354-h.pdf (accessed on 27 March 2024).
- Beavis, A.L.; Meek, K.; Moran, M.B.; Fleszar, L.; Adler, S.; Rositch, A.F. Exploring HPV vaccine hesitant parents? perspectives on decision-making and motivators for vaccination. Vaccine X 2022, 12, 100231. [Google Scholar] [CrossRef] [PubMed]
- Bloom, J.C.; Kaufmann, N.; Koss, S.; Edwards, H.A.; Perkins, R.B.; Faden, D.L. Deciphering Knowledge and Opinions of Human Papillomavirus and Human Papillomavirus Vaccination for Facilitation of Point-of-Care Vaccination in Adults. JAMA Otolaryngol. Head Neck Surg. 2023, 149, 870–877. [Google Scholar] [CrossRef]
- Association for Cancer Research. Hesitancy over the HPV Vaccine Has Stabilized or Risen in Some Subgroups. Available online: https://www.aacr.org/about-the-aacr/newsroom/news-releases/hesitancy-over-the-hpv-vaccine-has-stabilized-or-risen-in-some-subgroups/ (accessed on 31 January 2024).
- Cella, P.; Voglino, G.; Barberis, I.; Alagna, E.; Alessandroni, C.; Cuda, A.; D’aloisio, F.; Dallagiacoma, G.; De Nitto, S.; Di Gaspare, F.; et al. Resources for assessing parents’ vaccine hesitancy: A systematic review of the literature. J. Prev. Med. Hyg. 2020, 61, E340–E373. [Google Scholar]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- Quadri-Sheriff, M.; Hendrix, K.S.; Downs, S.M.; Sturm, L.A.; Zimet, G.D.; Finnell, S.M.E. The Role of Herd Immunity in Parents’ Decision to Vaccinate Children: A Systematic Review. Pediatrics 2012, 130, 522–530. [Google Scholar] [CrossRef]
- Center for Disease Control. HPV Vaccination Recommendations. 2021. Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html (accessed on 15 April 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Bond, S.M.; Cartmell, K.B.; Lopez, C.M.; Ford, M.E.; Brandt, H.M.; Gore, E.I.; Zapka, J.G.; Alberg, A.J. Racial and Ethnic Group Knowledge, Perceptions and Behaviors about Human Papillomavirus, Human Papillomavirus Vaccination, and Cervical Cancer among Adolescent Females. J. Pediatr. Adolesc. Gynecol. 2016, 29, 429–435. [Google Scholar] [CrossRef]
- Lechuga, J.; Prieto, C.; Mata, H.; Belknap, R.A.; Varela, I. Culture and sexuality-related communication as sociocultural precursors of HPV vaccination among mother-daughter dyads of Mexican descent. Prev. Med. Rep. 2020, 19, 101105. [Google Scholar] [CrossRef]
- Allen, E.M.; Lee, H.Y.; Pratt, R.; Vang, H.; Desai, J.R.; Dube, A.; Lightfoot, E. Facilitators and Barriers of Cervical Cancer Screening and Human Papilloma Virus Vaccination among Somali Refugee Women in the United States: A Qualitative Analysis. J. Transcult. Nurs. 2018, 30, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Btoush, R.; Brown, D.R.; Tsui, J.; Toler, L.; Bucalo, J. Knowledge and Attitudes Toward Human Papillomavirus Vaccination Among Latina Mothers of South American and Caribbean Descent in the Eastern US. Health Equity 2019, 3, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Colón-López, V.; Fernández-Espada, N.; Vélez, C.; Gonzalez, V.J.; Diaz-Toro, E.C.; Calo, W.A.; Savas, L.S.; Pattatucci, A.; Fernández, M.E. Communication about sex and HPV among Puerto Rican mothers and daughters. Ethn. Health 2017, 22, 348–360. [Google Scholar] [CrossRef]
- Kim, M.; Lee, H.; Kiang, P.; Kim, D. Human Papillomavirus: A Qualitative Study of Korean American Female College Students’ Attitudes Toward Vaccination. Clin. J. Oncol. Nurs. 2017, 21, E239–E247. [Google Scholar] [CrossRef] [PubMed]
- Polonijo, A.N.; Mahapatra, D.; Brown, B. “I Thought It Was Just For Teenagers”: Knowledge, Attitudes, and Beliefs about HPV Vaccination among Women Aged 27 to 45. Women’s Health Issues 2022, 32, 301–308. [Google Scholar] [CrossRef]
- Albright, K.; Barnard, J.; O’Leary, S.T.; Lockhart, S.; Jimenez-Zambrano, A.; Stokley, S.; Dempsey, A.; Kempe, A. Noninitiation and Noncompletion of HPV Vaccine among English- and Spanish-Speaking Parents of Adolescent Girls: A Qualitative Study. Acad. Pediatr. 2017, 17, 778–784. [Google Scholar] [CrossRef]
- Hull, P.C.; Williams, E.A.; Khabele, D.; Dean, C.; Bond, B.; Sanderson, M. HPV vaccine use among African American girls: Qualitative formative research using a participatory social marketing approach. Gynecol. Oncol. 2014, 132 (Suppl. S1), S13–S20. [Google Scholar] [CrossRef] [PubMed]
- Avni-Singer, L.; Oliveira, C.R.; Torres, A.; Shapiro, E.D.; Niccolai, L.M.; Sheth, S.S. Inpatient Immunization with HPV Vaccine: A Qualitative Study with Postpartum Women. Women’s Health Issues 2021, 31, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Burke, N.J.; Do, H.H.; Talbot, J.; Sos, C.; Ros, S.; Taylor, V.M. Protecting our Khmer daughters: Ghosts of the past, uncertain futures, and the human papillomavirus vaccine. Ethn. Health 2015, 20, 376–390. [Google Scholar] [CrossRef] [PubMed]
- Fields, E.J.; Hopfer, S.; Warren, J.R.; BeLue, R.; Lebed, J.; Hecht, M.L. Motivators and Barriers to HPV Vaccination: A Qualitative Study of Underserved Women Attending Planned Parenthood. Vaccines 2022, 10, 1126. [Google Scholar] [CrossRef]
- Galbraith-Gyan, K.V.; Lechuga, J.; Jenerette, C.M.; Palmer, M.H.; Moore, A.D.; Hamilton, J.B. HPV vaccine acceptance among African-American mothers and their daughters: An inquiry grounded in culture. Ethn. Health 2019, 24, 323–340. [Google Scholar] [CrossRef] [PubMed]
- Garcia, S.; Hopfer, S.; Amaro, H.; Tanjasiri, S. HPV vaccine delay and refusal among unvaccinated Mexican American young adult women: A qualitative investigation of Mexican-born and US-born HPV vaccine decision narratives. J. Behav. Med. 2023, 46, 88–99. [Google Scholar] [CrossRef]
- Hopfer, S.; Duong, H.T.; Garcia, S.; Tanjasiri, S.P. Health Information Source Characteristics Matter: Adapting the Dissemination of an HPV Vaccine Intervention to Reach Latina and Vietnamese Women. J. Prim. Prev. 2021, 42, 511–529. [Google Scholar] [CrossRef] [PubMed]
- Hopfer, S.; Garcia, S.; Duong, H.T.; Russo, J.A.; Tanjasiri, S.P. A Narrative Engagement Framework to Understand HPV Vaccination Among Latina and Vietnamese Women in a Planned Parenthood Setting. Health Educ. Behav. 2017, 44, 738–747. [Google Scholar] [CrossRef]
- Pierre-Victor, D.; Stephens, D.; Gabbidon, K.; Jean-Baptiste, N.; Clarke, R.; Madhivanan, P. Conversations about sexual activity within Haitian families: Implications for HPV vaccine uptake. Ethn. Health 2021, 26, 571–584. [Google Scholar] [CrossRef]
- Pierre-Victor, D.; Stephens, D.P.; Omondi, A.; Clarke, R.; Jean-Baptiste, N.; Madhivanan, P. Barriers to HPV Vaccination Among Unvaccinated, Haitian American College Women. Health Equity 2018, 2, 90–97. [Google Scholar] [CrossRef]
- Pierre-Victor, D.; Stephens, D.P.; Clarke, R.; Gabbidon, K.; Madhivanan, P. Role of Healthcare Providers Recommendation Style in HPV Vaccine Decision-Making among Haitian Parents and Female Patients. Californian J. Health Promot. 2017, 15, 68–80. [Google Scholar] [CrossRef]
- Ramírez, M.; Jessop, A.B.; Leader, A.; Crespo, C.J. Acceptability of the human papillomavirus vaccine among diverse hispanic mothers and grandmothers. Hisp. Health Care Int. 2014, 12, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Roncancio, A.M.; Ward, K.K.; Carmack, C.C.; Muñoz, B.T.; Cribbs, F.L. Hispanic mothers’ beliefs regarding HPV vaccine series completion in their adolescent daughters. Health Educ. Res. 2017, 32, 96–106. [Google Scholar] [CrossRef]
- Stephens, D.P.; Tamir, H.; Thomas, T.L. Factors Motivating HPV Vaccine Uptake among Vaccinated and Nonvaccinated Hispanic Young Adult Women. Hisp. Health Care Int. 2016, 14, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Stephens, D.P.; Thomas, T.L. Social Networks Influence Hispanic College Women’s HPV Vaccine Uptake Decision-Making Processes. Women’s Reprod. Health 2014, 1, 120–137. [Google Scholar] [CrossRef]
- Thompson, E.L.; Vamos, C.A.; Straub, D.M.; Sappenfield, W.M.; Daley, E.M. “We’ve Been Together. We Don’t Have It. We’re Fine”. How Relationship Status Impacts Human Papillomavirus Vaccine Behavior among Young Adult Women. Women’s Health Issues 2017, 27, 228–236. [Google Scholar] [CrossRef]
- Thompson, E.L.; Vamos, C.A.; Straub, D.M.; Sappenfield, W.M.; Daley, E.M. Human papillomavirus vaccine information, motivation, and behavioral skills among young adult US women. J. Health Psychol. 2018, 23, 1832–1841. [Google Scholar] [CrossRef]
- Walker, K.K.; Owens, H.; Zimet, G. The role of the media on maternal confidence in provider HPV recommendation. BMC Public Health 2020, 20, 1765. [Google Scholar] [CrossRef]
- Santhanes, D.; Wong, C.P.; Yap, Y.Y.; San, S.P.; Chaiyakunapruk, N.; Khan, T.M. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): A scoping review. Hum. Vaccines Immunother. 2018, 14, 124–133. [Google Scholar] [CrossRef]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; De Angelis, S.; Takacs, J.; Ali, K.A.; Pastore Celentano, L.; et al. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccines Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef]
- National Alliance of State Pharmacy Associations. Pharmacist Administered Vaccines. Available online: https://naspa.us/wp-content/uploads/2021/01/Pharmacist-Immunization-Authority-April-2023.pdf (accessed on 26 March 2024).
- DiStefano, M.J.; Markell, J.M.; Doherty, C.C.; Alexander, G.C.; Anderson, G.F. Association between Drug Characteristics and Manufacturer Spending on Direct-to-Consumer Advertising. JAMA 2023, 329, 386–392. [Google Scholar] [CrossRef]
- Fierce Pharma. Gardasil Vaccine Maker Merck Appeals to Parents of 9-Year-Olds in Latest HPV Awareness Ad. Available online: https://www.fiercepharma.com/marketing/gardasil-vaccine-maker-merck-appeals-parents-9-year-olds-latest-hpv-awareness-ad (accessed on 26 March 2024).
- US Food and Drug Administration. Vaccines. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines (accessed on 26 March 2024).
| Primary Author Last Name, Publish Date | Study Design * Interview = (INT) * Focus Group = (FG) * Both: Interview and Focus Group = (BO) CERQual Assessment | Geographic Location | Ethnicity/Race/Age | Facilitators | Barriers | Facilitators and Barriers |
|---|---|---|---|---|---|---|
| BO/High | Southern | White Latina African American Parents of adolescents Ages 18–49 | * | ||
| FG/Moderate | Midwest | African American Parents of adolescents Ages 23–64 | * | ||
| INT/Moderate | East Coast | Latina African American Caucasian Other Ages 15–26 | * | ||
| FG/Moderate | East Coast | Adolescents African American Latina Caucasian Ages 13–19 | * | ||
| FG/High | East Coast | Latina Mothers of adolescents Ages 21–55 | * | ||
| INT/High | West Coast | Cambodia Mothers of adolescents Over 30 years old | * | ||
| FG/High | US territory (Puerto Rico) | Latina Puerto Rican Islanders Mothers: 42–54 years old Daughters: 16–24 years old | * | ||
| INT/High | East Coast | African American Latina Caucasian Mixed: Haitian; Hawaiian Ages 18–34 | * | ||
| INT/High | East Coast | African American Mothers: mean age of 42.6 years old (SD 6.2) Daughters: 12–17 years old | * | ||
| INT/High | West Coast | Latina (Mexico) Ages 18–26 | * | ||
| INT/High | West Coast | Vietnamese Latina Ages 18–24 | * | * | |
| INT/High | West Coast | Vietnamese Latina Ages 18–26 | * | * | |
| BO/Moderate | Southern | African American Mothers: 31–55 years old Daughters: 11–18 years old | * | ||
| FG/Moderate | East Coast | Korean American Ages 18–26 | * | ||
| INT/High | Southwest | Latina Mothers: age n/a Daughters: 9–15 years old | * | ||
| INT/Moderate | Southeast | Haitian American Age 17–26 | * | ||
| INT/Moderate | Southeast | Haitian American Age 17–26 | |||
| INT/Moderate | Southeast | Haitian American Age 17–26 | * | ||
| FG/Moderate | West Coast | Latina Black Asian Ages 27–45 | * | ||
| INT/High | Northeastern | Latina Mothers and grandmothers ages 26–76 | * | ||
| INT/High | Southeastern | Latina Mothers: mean age of 41.94 years old (SD = 6.02) | * | ||
| INT/High | Southeastern | White Latina Ages 18–24 | * | ||
| INT/High | Southeastern | White Latina Ages 18–24 | * | ||
| INT/High | Southeastern | White Latina Ages 18–26 | * | ||
| INT/High | Southeastern | White Latina Ages 18–26 | * | ||
| INT/High | Midwest | White Black Pacific Islander Mothers ages 36–58 | * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cernasev, A.; Barenie, R.E.; Jasmin, H.; Yatsko, A.; Stultz, J.S. Factors Influencing USA Women to Receive the Human Papillomavirus Vaccine: A Systematic Literature Review. Women 2024, 4, 157-171. https://doi.org/10.3390/women4020012
Cernasev A, Barenie RE, Jasmin H, Yatsko A, Stultz JS. Factors Influencing USA Women to Receive the Human Papillomavirus Vaccine: A Systematic Literature Review. Women. 2024; 4(2):157-171. https://doi.org/10.3390/women4020012
Chicago/Turabian StyleCernasev, Alina, Rachel E. Barenie, Hilary Jasmin, Ashley Yatsko, and Jeremy S. Stultz. 2024. "Factors Influencing USA Women to Receive the Human Papillomavirus Vaccine: A Systematic Literature Review" Women 4, no. 2: 157-171. https://doi.org/10.3390/women4020012
APA StyleCernasev, A., Barenie, R. E., Jasmin, H., Yatsko, A., & Stultz, J. S. (2024). Factors Influencing USA Women to Receive the Human Papillomavirus Vaccine: A Systematic Literature Review. Women, 4(2), 157-171. https://doi.org/10.3390/women4020012








