Recreational Female Athletes’ Understanding of and Perceived Impact of the Menstrual Cycle on Physical Performance, Mood, and Sleeping Behaviour
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Statistical Analysis
3. Results
3.1. Menstrual Cycle and Knowledge
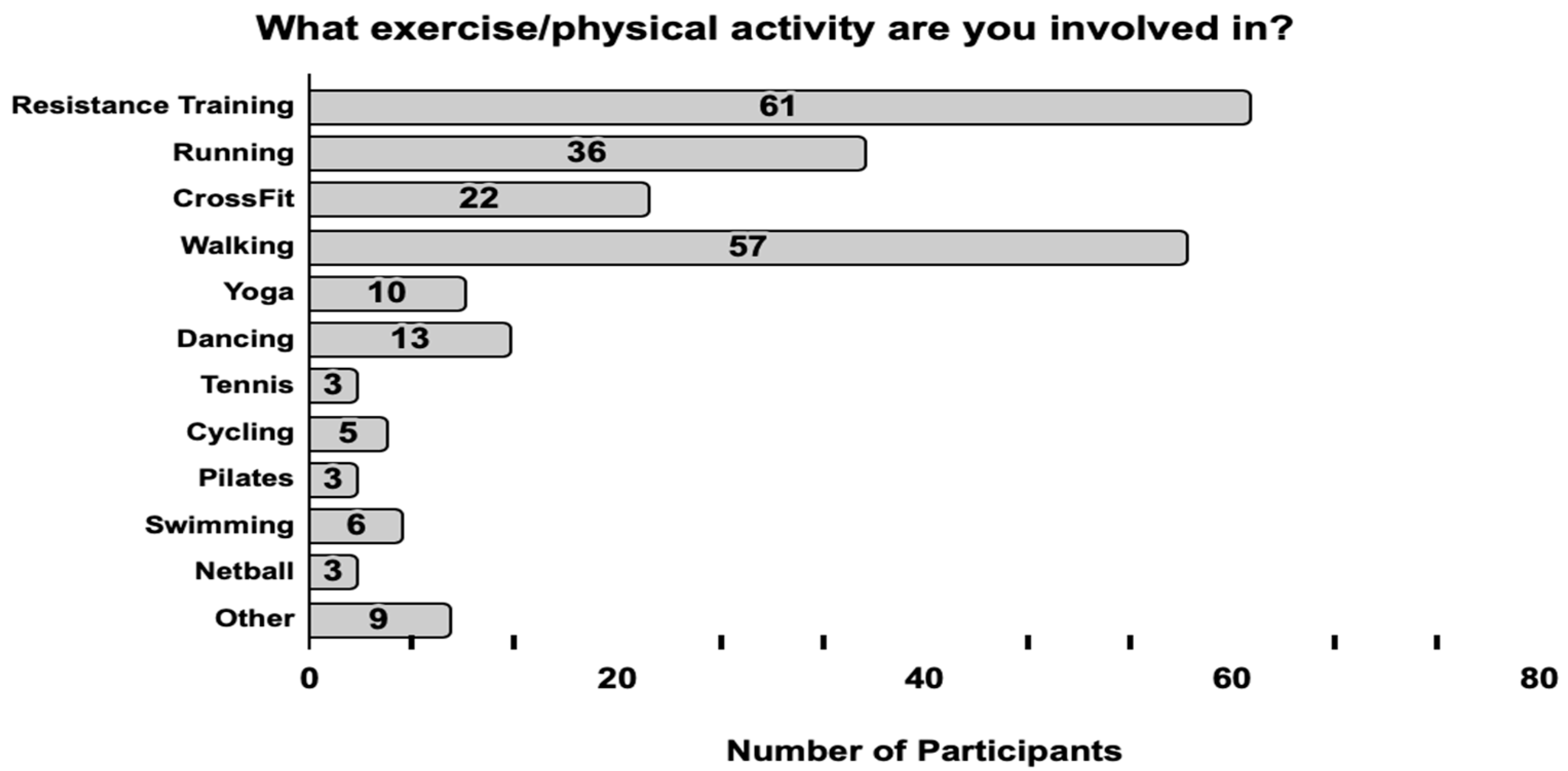
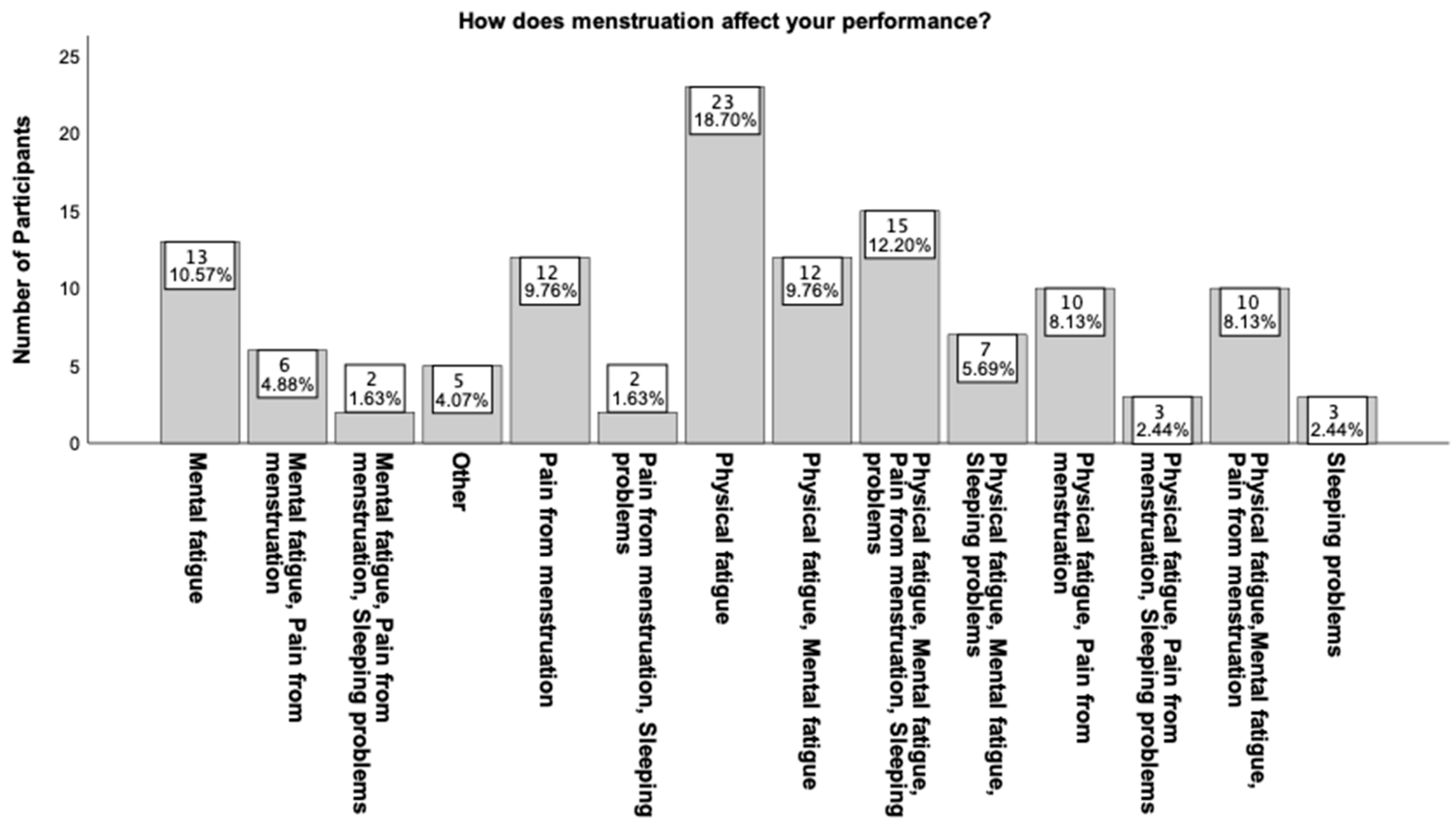
3.2. Menstrual Cycle and Performance
3.3. Menstrual Cycle and Symptoms
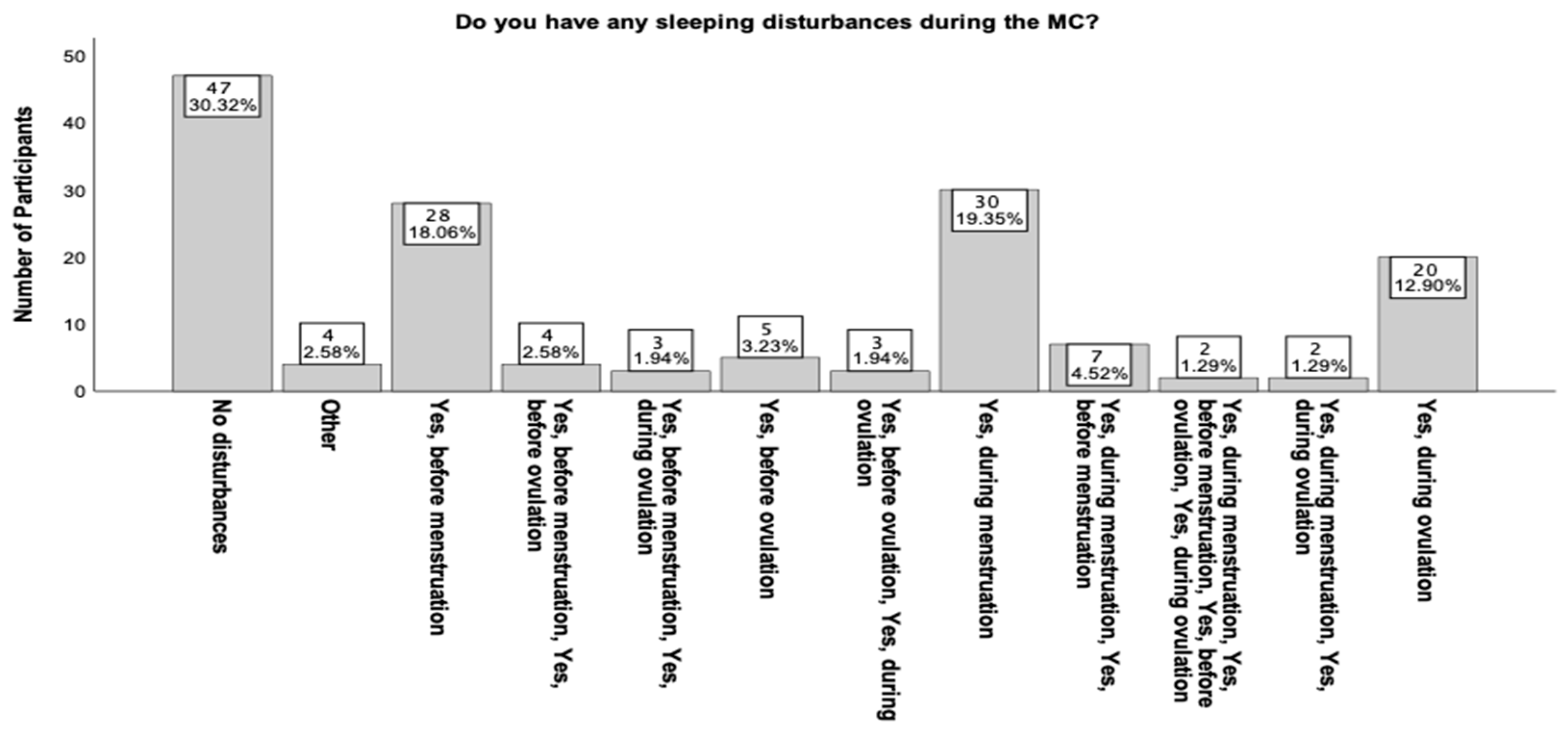
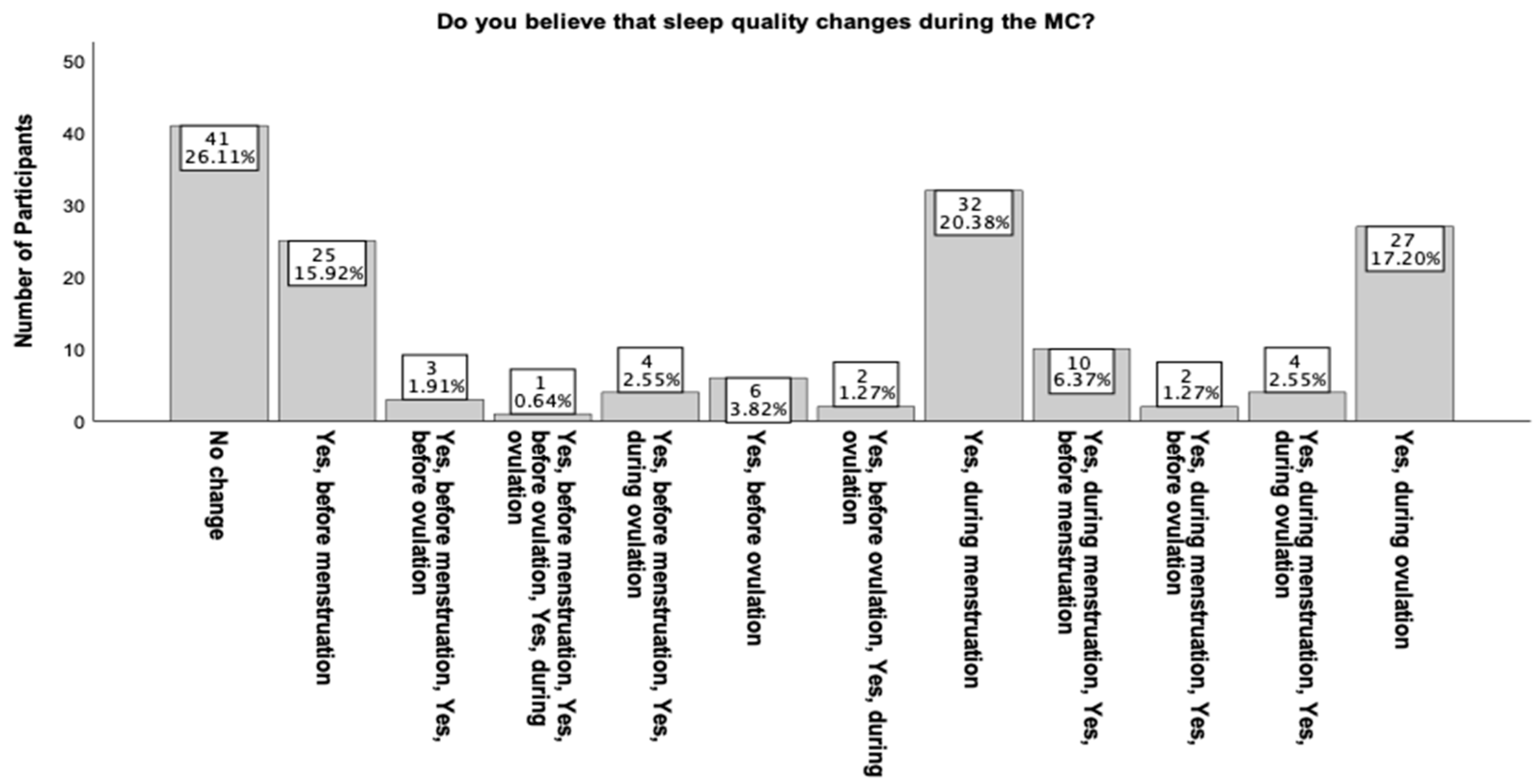
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pitchers, G.; Elliott-Sale, K. Considerations for Coaches Training Female Athletes. Prof. Strength Cond. 2019, 55, 19–30. [Google Scholar]
- Janse De Jonge, X.; Thomson, B.; Han, A. Methodological Recommendations for Menstrual Cycle Research in Sports, and Exercise. Med. Sci. Sports Exerc. 2019, 12, 2610–2617. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, M.A.; Thomson, R.L.; Moran, L.J.; Dunstan, J.R.; Nelson, M.J.; Mathai, M.L.; Wycherley, T.P. A Pilot Study on the Impact of Menstrual Cycle Phase on Elite Australian Football Athletes. Int. J. Environ. Res. Public Health 2021, 18, 9591. [Google Scholar] [CrossRef] [PubMed]
- Constantini, N.W.; Dubnov, G.; Lebrun, C.M. The Menstrual Cycle and Sport Performance. Clin. Sports Med. 2005, 2, e51–e82. [Google Scholar] [CrossRef]
- Hawkins, S.M.; Matzuk, M.M. The Menstrual Cycle. Ann. N. Y. Acad. Sci. 2008, 1, 10–18. [Google Scholar] [CrossRef]
- Loureiro, S.; Dias, I.; Sales, D.; Alessi, I.; Simão, R.; Fermino, R.C. Effect of Different Phases of the Menstrual Cycle on the Performance of Muscular Strength in 10RM. Rev. Bras. Med. Esporte 2011, 17, 22–25. [Google Scholar] [CrossRef]
- Baker, F.C.; Driver, H.S. Circadian Rhythms, Sleep, and the Menstrual Cycle. Sleep Med. 2007, 6, 613–622. [Google Scholar] [CrossRef]
- Rodrigues, P.; de Azevedo Correia, M.; Wharton, L. Effect of Menstrual Cycle on Muscle Strength. J. Exerc. Physiol. 2019, 5, 89–97. [Google Scholar]
- Oosthuyse, T.; Bosch, A.N. The Effect of the Menstrual Cycle on Exercise Metabolism. Sports Med. 2010, 3, 207–227. [Google Scholar] [CrossRef]
- Larsen, B.; Morris, K.; Quinn, K.; Osborne, M.; Minahan, C. Practice does not make perfect: A brief view of athletes’ knowledge on the menstrual cycle and oral contraceptives. J. Sci. Med. Sport 2020, 20, 690–694. [Google Scholar] [CrossRef]
- Tremback-Ball, A.; Fulton, K.; Giampietro, N.; Gibbons, M.; Kneller, A.; Zelinka, H. Effect of the Menstrual Cycle on Athletic Performance in NCAA Division III Collegiate Athletes. J. Women’s Health Phys. Ther. 2020, 45, 20–26. [Google Scholar] [CrossRef]
- Ojezele, M.O.; Eduviere, A.T.; Adedapo, E.A.; Wool, T.K. Mood Swing During Menstruation: Confounding Factors and Drug Use. Ethiop. J. Health Sci. 2022, 4, 681–688. [Google Scholar] [CrossRef]
- Pöllänen, E.; Sipilä, S.; Alen, M.; Ronkainen, P.H.A.; Ankarberg-Lindgren, C.; Puolakka, J.; Suominen, H.; Hämäläinen, E.; Turpeinen, U.; Konttinen, Y.T.; et al. Differential Influence of Peripheral and Systemic Sex Steroids on Skeletal Muscle Quality in Pre- and Postmenopausal Women. Aging Cell 2011, 10, 650–660. [Google Scholar] [CrossRef] [PubMed]
- McClung, J.M.; Davis, J.M.; Wilson, M.A.; Goldsmith, E.C.; Carson, J.A. Estrogen Status and Skeletal Muscle Recovery from Disuse Atrophy. J. Appl. Physiol. 2006, 100, 2012–2023. [Google Scholar] [CrossRef] [PubMed]
- Sitnick, M.; Foley, A.; Brown, M.; Spangenburg, E.E. Ovariectomy Prevents the Recovery of Atrophied Gastrocnemius Skeletal Muscle Mass. J. Appl. Physiol. 2006, 100, 286–293. [Google Scholar] [CrossRef]
- Diel, P. The Role of the Estrogen Receptor in Skeletal Muscle Mass Homeostasis and Regeneration. Acta Physiol. 2014, 212, 14–16. [Google Scholar] [CrossRef]
- Ekenros, L.; Papoutsi, Z.; Fridén, C.; Dahlman Wright, K.; Lindén Hirschberg, A. Expression of Sex Steroid Hormone Receptors in Human Skeletal Muscle during the Menstrual Cycle. Acta Physiol. 2016, 219, 486–493. [Google Scholar] [CrossRef]
- Paludo, A.C.; Paravlic, A.; Dvořáková, K.; Gimunová, M. The Effect of Menstrual Cycle on Perceptual Responses in Athletes: A Systematic Review with Meta-Analysis. Front. Psychol. 2022, 13, 926854. [Google Scholar] [CrossRef]
- Lochbaum, M. Understanding the meaningfulness and potential impact of sports psychology on performance. In Proceedings of the 8th International Scientific Conference on Kinesiology, Opatija, Croatia, 10–14 May 2017; Milanović, D., Sporiš, G., Šalaj, S., Škegro, D., Eds.; Faculty of Kinesiology, University of Zagreb: Zagreb, Croatia, 2017; pp. 486–489. [Google Scholar]
- Leong, R.L.F.; Cheng, G.H.L.; Chee, M.W.L.; Lo, J.C. The Effects of Sleep on Prospective Memory: A Systematic Review and Meta-analysis. Sleep Med. Rev. 2019, 47, 18–27. [Google Scholar] [CrossRef]
- Wallace, M.; Hashim, Y.Z.H.-Y.; Wingfield, M.; Culliton, M.; McAuliffe, F.; Gibney, M.J.; Brennan, L. Effects of Menstrual Cycle Phase on Metabolomic Profiles in Premenopausal Women. Hum. Reprod. 2010, 25, 949–956. [Google Scholar] [CrossRef]
- Fong, A.K.; Kretsch, M.J. Changes in Dietary Intake, Urinary Nitrogen, and Urinary Volume across the Menstrual Cycle. Am. J. Clin. Nutr. 1993, 57, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Yen, J.Y.; Chang, S.J.; Ko, C.H.; Yen, C.-F.; Chen, C.S.; Yeh, Y.C.; Chen, C.C. The High-Sweet-Fat Food Craving among Women with Premenstrual Dysphoric Disorder: Emotional response, Implicit Attitude and Rewards Sensitivity. Psychoneuroendocrinology 2010, 35, 1203–1212. [Google Scholar] [CrossRef] [PubMed]
- Reed, S.C.; Levin, F.R.; Evans, S.M. Changes in Mood, Cognitive Performance and Appetite in the Late Luteal and Follicular Phases of the Menstrual Cycle in Women with and Without PMDD (Premenstrual Dysphoric Disorder). Horm. Behav. 2008, 54, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Frackiewicz, E.J.; Shiovitz, T.M. Evaluation and Management of Premenstrual Syndrome and Premenstrual Dysphoric Disorder. J. Am. Pharm. Assoc. 2001, 41, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Dye, L.; Blundell, J.E. Menstrual Cycle and Appetite Control: Implications for Weight Regulation. Hum. Reprod. 1997, 12, 1142–1151. [Google Scholar] [CrossRef]
- Groeger, J.A.; Zijlstra, F.R.H.; Dijk, D.J. Sleep Quantity, Sleep Difficulties, and their Perceived Consequences in a Representative Sample of some 2000 British Adults. J. Sleep Res. 2014, 4, 359–371. [Google Scholar] [CrossRef]
- Lindberg, E.; Janson, C.; Gislason, T.; Björnsson, E.; Hetta, J.; Boman, G. Sleep Disturbances in a Young Adult Population: Can Gender Differences Be Explained by Differences in Psychological Status? Sleep 1997, 6, 381–387. [Google Scholar] [CrossRef]
- Woosley, J.A.; Lickstein, K.L. Dysmenorrhea, the Menstrual Cycle, and Sleep. Behav. Med. 2014, 1, 14–21. [Google Scholar] [CrossRef]
- Reilly, T.; Piercy, M. The Effect of Partial Sleep Deprivation on Weightlifting Performance. Ergonomics 1994, 1, 107–115. [Google Scholar] [CrossRef]
- Axelsson, J.; Ingre, M.; Kecklund, G.; Lekander, M.; Wright, K.P.; Sundelin, T. Sleepiness as Motivation: A Potential Mechanism for How Sleep Deprivation Affects Behavior. Sleep 2019, 43, p.zsz291. [Google Scholar] [CrossRef]
- Edwards, B.J.; Waterhouse, J. Effects of One Night of Partial Sleep Deprivation upon Diurnal Rhythms of Accuracy and Consistency in Throwing Darts. Chronobiol. Int. 2009, 4, 756–768. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, K.M.; Crawford, S.L.; Kim, S.; Joffe, H. Objective Sleep Interruption and Reproductive Hormone Dynamics in the Menstrual Cycle. Sleep Med. 2014, 6, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Farage, M.A.; Neill, S.; MacLean, A.B. Physiological Changes Associated with the Menstrual Cycle: A Review. Obstet. Gynecol. Surv. 2009, 1, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.C.; Hackney, A.C. The Hypothalamic–Pituitary–Ovarian Axis and Oral Contraceptives: Regulation and Function. In Sex Hormones, Exercise and Women; Springer: Cham, Switzerland, 2016; pp. 1–17. [Google Scholar] [CrossRef]
- Hennegan, J.; Nansubuga, A.; Akullo, A.; Smith, C.; Schwan, K.J. The menstrual practices Questionnaire (MPQ): Development, Elaboration, and Implications for Future Research. Glob. Health Action 2020, 1, 1829402. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.R. Knowledge and Attitudes Regarding the Menstrual Cycle, Oral Contraceptives and Sports Performance: The Conceptualization and Development of a Questionnaire for Athletic Coaches. Ph.D. Thesis, Florida State University, Tallahassee, FL, USA, 2008. [Google Scholar]
- Elliott-Sale, K.J.; McNulty, K.L.; Ansdell, P.; Goodall, S.; Hicks, K.M.; Thomas, K.; Swinton, P.A.; Dolan, E. The Effects of Oral Contraceptives on Exercise Performance in Women: A Systematic Review and Meta-analysis. Sports Med. 2020, 10, 1785–1812. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, A.G.; Andersen, M.L.; Pires, G.N.; Tufik, S.; Hachul, H. The Effects of Hormonal Contraceptive Use on Sleep in Women: A Systematic Review and Meta-Analysis. J. Sleep Res. 2022, 32, e13757. [Google Scholar] [CrossRef]
- Sarwar, R.; Nicols, M.; Huhtaniemi, I.; Adlercreutz, H. Measurement of sex steroids in serum by liquid chromatography–tandem mass spectrometry in the simultaneous presence of steroid sulfates. Clin. Chem. 2022, 40, 1773–1780. [Google Scholar]
- Prado, R.C.R.; Silveira, R.; Kilpatrick, M.W.; Pires, F.O.; Asano, R.Y. The Effect of Menstrual Cycle and Exercise Intensity on Psychological and Physiological Responses in Healthy Eumenorrheic Women. Physiol. Behav. 2021, 6, 113290. [Google Scholar] [CrossRef]
- Bruinvels, G.; Hackney, A.C.; Pedlar, C.R. Menstrual Cycle: The Importance of Both the Phases and the Transitions Between Phases on Training and Performance. Sports Med. 2022, 7, 1457–1460. [Google Scholar] [CrossRef]
- Czajkowska, M.; Drosdzol-Cop, A.; Naworska, B.; Galazka, I.; Gogola, C.; Rutkowska, M.; Skrzypulec-Plinta, V. The Impact of Competitive Sports on Menstrual Cycle and Menstrual Disorders, Including Premenstrual Syndrome, Premenstrual Dysphoric Disorder, and Hormonal Imbalances. Ginekol. Pol. 2020, 9, 503–512. [Google Scholar] [CrossRef]
- Halson, S.L. Sleep in Elite Athletes and Nutritional Interventions to Enhance Sleep. Sports Med. 2014, 44 (Suppl. 1), 13–23. [Google Scholar] [CrossRef]
- Bull, J.R.; Rowland, S.P.; Scherwitzl, E.B.; Scherwitzl, R.; Danielsson, K.G.; Harper, J. Real-world Menstrual Cycle Characteristics of More than 600,000 Menstrual Cycles. NPJ Digit. Med. 2019, 1, 83. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.; Knight, C.J.; Forrest née Whyte, L.J. Elite female athletes’ Experiences and Perceptions of the Menstrual Cycle on Training and Sport Performance. Scand. J. Med. Sci. 2020, 1, 52–69. [Google Scholar] [CrossRef] [PubMed]
- Findlay, R.J.; Macrae, E.H.R.; Whyte, I.Y.; Easton, C.; Whyte, L.J.F. How the Menstrual Cycle and Menstruation Affect Sporting Performance: Experiences and Perceptions of Elite Female Rugby Players. Br. J. Sports Med. 2020, 54, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Draper, C.F.; Duisters, K.; Weger, B.; Chakrabarti, A.; Harms, A.C.; Brennan, L.; Hankemeier, T.; Goulet, L.; Konz, T.; Martin, F.P.; et al. Menstrual Cycle Rhythmicity: Metabolic Patterns in Healthy Women. Sci. Rep. 2018, 8, 14568. [Google Scholar] [CrossRef]
- Hall, K.S.; Westhoff, C.L.; Castaño, P.M. The Impact of an Educational Text Message Intervention on Young Urban Women’s Knowledge of Oral Contraception. Contraception 2013, 87, 449–454. [Google Scholar] [CrossRef] [PubMed]
- De Souza, M.J.; Toombs, R.J.; Scheid, J.L.; O’Donell, E.; West, S.L.; Williams, N.I. High Prevalence of Subtle and Severe Menstrual Disturbances in Exercising Women: Confirmation Using Daily Hormone Measures. Hum. Reprod. 2009, 25, 491–503. [Google Scholar] [CrossRef]
- McGawley, K.; Sargent, D.; Noordhof, D.; Badenhorst, C.E.; Julian, R.; Govus, A.D. Improving Menstrual Health Literacy in Sport. J. Sci. Med. Sport 2023, 26, 351–357. [Google Scholar] [CrossRef]
- Minahan, C.; Joyce, S.; Bulmer, A.C.; Cronin, N.; Sabapathy, S. The Influence of Estradiol on Muscle Damage and Leg Strength after Intense Eccentric Exercise. Eur. J. Appl. Physiol. 2015, 115, 1493–1500. [Google Scholar] [CrossRef]
- Minahan, C.; Melnikoff, M.; Quinn, K.; Larsen, B. Response of Women using Oral Contraception to Exercise in the Heat. Eur. J. Appl. Physiol. 2017, 117, 1383–1391. [Google Scholar] [CrossRef]
- Lochbaum, M.; Stoner, E.; Hefner, T.; Cooper, S.; Lane, A.M.; Terry, P.C. Sport Psychology and Performance Meta-Analyses: A Systematic Review of Literature. PLoS ONE 2022, 17, e0263408. [Google Scholar] [CrossRef] [PubMed]
- Knowles, O.E.; Aisbett, B.; Main, L.C.; Drinkwater, E.J.; Orellana, L.; Lamon, S. Resistance Training and Skeletal Muscle Protein Metabolism in Eumenorrheic Females: Implications for Researchers and Practitioners. Sport Med. 2019, 49, 1637–1650. [Google Scholar] [CrossRef] [PubMed]
- Meignie, A.; Duclos, M.; Carling, C.; Orhant, E.; Provost, P.; Toussaint, J.F.; Antero, J. The Effects of Menstrual Cycle Phase on Elite Athlete Performance: A Critical and Systematic Review. Front. Physiol. 2021, 12, 654585. [Google Scholar] [CrossRef] [PubMed]
- Von Rosen, P.; Ekenros, L.; Solli, G.S.; Sandbakk, O.; Holmberg, H.C.; Hirschberg, A.L.; Friden, C. Offered Support and Knowledge about Menstrual Cycle in the Athletic Community: A Cross-Sectional Study of 1086 Female Athletes. Int. J. Environ. Res. Public Health 2022, 19, 11932. [Google Scholar] [CrossRef]

| Do You Know the Phases of the MC? | Participants (n) 164 | Percent (%) 100 |
|---|---|---|
| Yes | 49 | 29.9 |
| No | 115 | 70.1 |
| How many phases do you know? | Participants (n) 164 | Percent (%) 100 |
| 0 | 115 | 70.1 |
| 1 | 1 | 0.6 |
| 2 | 12 | 7.3 |
| 3 | 6 | 3.7 |
| 4 | 30 | 18.3 |
| Do you know the four basic hormones of the MC? | Participants (n) 164 | Percent (%) 100 |
| Yes | 18 | 11.2 |
| I know some of them | 55 | 33.5 |
| No | 91 | 55.5 |
| How many hormones do you know? | Participants (n) 164 | Percent (%) 100 |
| 0 | 91 | 56 |
| 1 | 12 | 7.3 |
| 2 | 38 | 23.2 |
| 3 | 6 | 3.7 |
| 4 | 16 | 9.8 |
| Do You Feel Comfortable Training during Your Period? | Participants (n) 143 | Percent (%) 100 |
|---|---|---|
| Yes | 58 | 40.6 |
| No | 34 | 23.8 |
| Sometimes | 51 | 35.7 |
| How would you describe your performance during ovulation? | Participants (n) 143 | Percent (%) 100 |
| I always feel strong, motivated, and ready to push myself | 20 | 14.0 |
| I usually feel strong, motivated, and ready to push myself | 42 | 29.4 |
| I sometimes feel strong, motivated, and ready to push myself | 54 | 37.8 |
| I rarely feel strong, motivated, and ready to push myself | 12 | 8.4 |
| I feel weak, unmotivated, and not ready to push myself | 15 | 10.5 |
| Do you believe your mood affects your performance? | Participants (n) 143 | Percent (%) 100 |
| Yes | 88 | 61.5 |
| Sometimes | 30 | 21.0 |
| Maybe | 22 | 15.4 |
| No | 3 | 2.1 |
| How Would You Describe Your Symptoms Prior to Menstruation? | Participants (n) 135 | Percent (%) 100 |
|---|---|---|
| Bloating/Stomach issues | 4 | 3.0 |
| Bloating/Stomach issues, Breast tenderness | 4 | 3.0 |
| Mood swings, Bloating/Stomach issues, Breast tenderness | 4 | 3.0 |
| Mood swings, Bloating/Stomach issues, Breast tenderness, Fatigue | 10 | 7.4 |
| Mood swings, Bloating/Stomach issues, Breast tenderness, Headaches, Fatigue | 12 | 8.9 |
| Mood swings, Bloating/Stomach issues, Fatigue | 8 | 5.9 |
| Mood swings, Bloating/Stomach issues, Headaches, Fatigue | 4 | 3.0 |
| Mood swings, Breast tenderness | 6 | 4.4 |
| Mood swings, Fatigue | 9 | 6.7 |
| Mood swings, Sleeping problems, Bloating/Stomach issues, Breast tenderness | 3 | 2.2 |
| Mood swings, Sleeping problems, Bloating/Stomach issues, Breast tenderness, Fatigue | 7 | 5.2 |
| Mood swings, Sleeping problems, Bloating/Stomach issues, Breast tenderness, Headaches, Fatigue | 16 | 11.9 |
| Mood swings, Sleeping problems, Bloating/Stomach issues, Fatigue | 5 | 3.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michelekaki, E.A.; Michaelides, M.; Govindasamy, K.; Parpa, K. Recreational Female Athletes’ Understanding of and Perceived Impact of the Menstrual Cycle on Physical Performance, Mood, and Sleeping Behaviour. Women 2023, 3, 445-456. https://doi.org/10.3390/women3030034
Michelekaki EA, Michaelides M, Govindasamy K, Parpa K. Recreational Female Athletes’ Understanding of and Perceived Impact of the Menstrual Cycle on Physical Performance, Mood, and Sleeping Behaviour. Women. 2023; 3(3):445-456. https://doi.org/10.3390/women3030034
Chicago/Turabian StyleMichelekaki, Eleni Anna, Marcos Michaelides, Karuppasamy Govindasamy, and Koulla Parpa. 2023. "Recreational Female Athletes’ Understanding of and Perceived Impact of the Menstrual Cycle on Physical Performance, Mood, and Sleeping Behaviour" Women 3, no. 3: 445-456. https://doi.org/10.3390/women3030034







