Abstract
Women with schizophrenia require health interventions that differ, in many ways, from those of men. The aim of this paper is to review male and female care needs and describe a newly established care unit for the treatment of women with schizophrenia. After reviewing the literature on the differentiated needs of men and women with schizophrenia, we describe the new unit’s assessment, intervention, and evaluation measures. The program consists of (1) individual/group patient/family therapy, (2) therapeutic drug monitoring and adherence checks, (3) perinatal mental health, (4) medical liaison, (5) suicide prevention/intervention, (6) social services with special focus on parenting, domestic abuse, and sexual exploitation, (7) home-based services, (8) peer support, (9) occupational therapies (physical activity and leisure programs), and (10) psychoeducation for both patients and families. Still in the planning stage are quality evaluation of diagnostic assessment, personalized care, drug optimization, health screening (reproductive health, metabolic syndrome, cardiovascular health, cancer, menopausal status), and patient and family satisfaction with services provided. Woman-specific care represents an important resource that promises to deliver state-of-the-art treatment to women and, ideally, prevent mental illness in their offspring.
1. Introduction
With growing appreciation of the differences in the clinical needs of men and women with schizophrenia, our hospital system decided to provide a specialized community service for this disorder for women only, built on a previous successful model [1].
This paper reviews the literature on male/female differences in schizophrenia and the specific needs of women at various stages of life. It is well known but worth repeating that many differences in the onset, expression, treatment response, and prognosis of schizophrenia exist, although they are sometimes under-appreciated. Schizophrenia is considered to be a neurodevelopmental disorder, so subtle manifestations can appear in infancy and childhood [2]. This is much more frequent in boys than in girls in that obstetric difficulties are more common in boys, as are autism attention deficit disorder, stuttering, and tics, all of which can act as precursors to later psychotic illness [3]. Puberty arrives earlier in girls than boys and is accompanied by social awareness at an age when boys may start showing premorbid signs of difficulty, such as social isolation, inability to step into others’ shoes (theory of mind), and preoccupation with esoteric or philosophical thought [4]. Boys are also more prone than girls to engage in substance abuse during adolescence, which further impairs thought processes. Young men develop schizophrenia on average two or three years before young women [5]. This often means that education remains incomplete and social skill is never attained. Once psychosis emerges, symptom differences between the two sexes become noticeable—women responding more emotionally, men with schizophrenia showing a flattened affect and increases in idiosyncratic thinking. When treatment is started, women respond more quickly and more robustly [6]. Women often maintain their social support after the onset of illness; men do not. Over the course of the disorder, men more often are incarcerated, commit suicide, and remain unemployed and unattached [6]. Women, in many cases, find intimate partners and become parents [7]. The difficulty is that treatment guidelines for schizophrenia are generally written with men in mind.
Accordingly, this paper, therefore, describes the rationale, objectives, programs, and implementation phases of a new service based on the clinical care needs of women. It is an amalgamation of two previously separate clinics. The paper also identifies the quality evaluation measures that are requisites for such a unit, measures that are currently awaiting implementation.
2. Results
2.1. Mental Health Problems of Women with Schizophrenia
Men and women with schizophrenia have different symptom profiles, which is usually attributed to hormonal differences [8,9,10,11,12,13]. Difficult-to-treat negative and cognitive symptoms are more prevalent among men, and affective and positive psychotic symptoms are more often seen in women [9,12]. Poor clinical outcomes are usually attributed to social causes. These include multiple hospitalizations, substance abuse, homelessness, perpetration of violence, and completed suicide, which are associated more closely with men than with women [13,14,15,16,17,18,19]. Men and women with schizophrenia also differ in antipsychotic treatment response, with women requiring relatively lower doses until the age of menopause [15,20,21]. With loss of estrogen, after menopause, women show a worsening of antipsychotic response and require raised antipsychotic doses, which leads to more severe adverse effects.
Sex selection bias in schizophrenia antipsychotic trials (more men recruited than women) may have obscured clinically important sex differences [15]. Another limitation of the available literature is that information about hormonal status (pre/post-menopause) in women participating in trials is rarely reported. Most trial outcomes do not distinguish between men and women, and most countries’ schizophrenia treatment guidelines fail to do so as well [22,23].
It has been frequently reported that women are at a higher risk than men for adverse secondary effects of antipsychotics [23,24], particularly for metabolic and prolactin-induced side effects [16]. As women age, notably after menopause, the risk of tardive dyskinesia increases [17]. To study this phenomenon, Turrone and collaborators conducted a selective review of the epidemiology, etiology, and treatment of tardive dyskinesia (TD), with a special focus on the influence of estrogen [23,25]. Their conclusion was that estrogen modulates dopamine-mediated behaviors and is likely to be protective against cell damage related to TD, a protection that disappears during menopause [26,27].
Women with schizophrenia and related disorders are reported to have mental health care needs that differ from those of men [28,29]. For instance, women may require intervention for symptom fluctuation over the course of the menstrual cycle [30,31,32,33]. They often need contraceptive advice to protect against unwanted pregnancy [34]; they may also need abortion/adoption support. During pregnancy, the postpartum period, and pre- and post-menopause, pharmacotherapy in women is reported as requiring careful adjustment because of changes in estrogen levels [35]. The progression of the effects of excessive substance use is known to differ in men and women [36]. Screening for potentially overlapping conditions, such as eating disorders or affective disorders, is often required in women with schizophrenia [37,38].
2.2. Medical Issues
Besides overlapping psychiatric conditions, women with schizophrenia require physical health interventions that are different from those of men [28,29]. There may also be difficult access to medical care for women in some parts of the world [39]. In most cultures, men and women with schizophrenia are exposed to different medical risk factors (trauma, toxins, childbirth) and need different preventive screening procedures because of inherently different anatomy and endocrine, metabolic, immune, and cardiovascular physiology [28]. This means that males and females are differentially affected by medical comorbidities [40].
Obstetrics and gynecology services are uniquely important to women, but women with schizophrenia have been reported to receive inadequate gynecological services, be less likely than other women to receive mammograms or cervical cancer screening, or breast and pelvic examinations, or to be prescribed hormone replacement therapies at menopause [41].
Death from breast cancer is disturbingly high in this population, attributable to lifestyle factors, symptoms, insufficient screening, and fewer physical examinations than other women (despite more hospital admissions), diagnostic overshadowing, and poor access to new chemotherapy trials [42,43,44].
Diabetes and metabolic syndrome are frequent in the schizophrenia female population, related to inactivity, poor diet, overuse of substances, and side effects of antipsychotics (AP) [45]. Obstructive sleep apnea (OSA) can result from medication-induced obesity, and because OSA is usually associated with males, it often passes unrecognized in women [46,47]. Certain infections not usually associated with women, such as HIV, may also be missed and remain untreated in this population [48,49].
AP-induced hyperprolactinemia produces a variety of symptoms in women, including infertility [50,51]; it also heightens the risk of osteoporosis [52]. All of this is preventable by a judicial choice of AP type and dosage [32,53,54].
2.3. Parental and Social Issues
The vast majority of the literature indicates that more than 50% of women with schizophrenia are mothers, and nearly 50% of these mothers suffer from a loss of custody of their children, at least temporarily [32,33,55,56]. Women with schizophrenia are often single, impoverished mothers living in inadequate housing in unsafe neighborhoods, which renders ’good enough’ parenting extremely difficult to achieve [55]. The children of mothers with schizophrenia are at a disadvantage from the time of conception. During their mothers’ pregnancies, they are exposed to subpar prenatal care, maternal alcohol, drugs, and nicotine excess, as well as to the adverse effects of maternal antipsychotic medication use. During pregnancy, their mothers may be homeless; they may be physically abused and may not receive adequate nutrition. Mothers of these children suffer a high rate of gestational diabetes [57]. The infants come into the world with low birth weights; they are often not breastfed for fear of antipsychotic drug transmission; nutrition and shelter and stimulation are often inadequate. The infant death rate is relatively high, and slow cognitive development and noxious exposures are more frequent than in the general population [58,59].
A recent review of psychopharmacology and pregnancy in women with schizophrenia [57] emphasized that the use of antipsychotics in pregnancy has increased. The authors recommended drug-level monitoring across the three trimesters of pregnancy. There is much uncertainty about the effect of pregnancy stages on AP metabolism, and much that is unknown about optimal pregnancy care for women with schizophrenia.
Vigod and collaborators carried out a retrospective study investigating maternal and newborn health outcomes in women with schizophrenia in Ontario, Canada [60]. Schizophrenia was associated with a high risk of pre-eclampsia, preterm birth, and venous thromboembolism, all requiring intensive care. The participating women suffered an elevated risk of adverse pregnancy outcomes, and neonatal morbidity was high [60]. More recently, Heinonen and collaborators also reported that fetal exposure to antipsychotics is associated with an increased risk of neonatal morbidity [61].
One important but neglected issue is that many AP induce somnolence and fatigue in women with schizophrenia, which can lead to perceived maternal negligence in the postpartum period, leading to loss of child custody [62].
There are other female-specific social risks that require prevention—sexual exploitation is one. Another is legal risk. In cases of separation and divorce, women with schizophrenia are in danger of losing maternal and financial rights because of their illness and the stigma that the illness elicits [63,64,65].
In summary, women with schizophrenia have psychiatric, medical, and social needs different from those of men, in our opinion, they require a specialized women-centered clinic.
3. Currently Offered Women-Centered Programs and Discussion of Findings
Currently, the Community Mental Health Services for Adults of Mutua Terrassa University Hospital serves a population of approximately 220,000 inhabitants in a well-defined area of the Terrassa and Sant Cugat regions in Barcelona (Spain). The two community mental health outpatient units, CMHU Rambla Terrassa and CMHU Sant Cugat, promote mental health and offer mental health care for people suffering from mental disorders. Approximately 40% of the population attending the two centers suffer from a severe mental illness, schizophrenia being the most common diagnosis. Nearly 58% of the population are women. The unit for women with schizophrenia is responsible for the clinical care of women with schizophrenia and related disorders (delusional disorder and schizoaffective disorder) who attend the two CMHUs. The staff of the two units are in constant communication; they provide similar services, and the plan is for staff to begin moving between the two centers and to hold joint weekly meetings.
Table 1 shows the main programs currently offered. Some, as marked, are still in the planning phase.

Table 1.
Currently offered and projected programs in the unit for women with schizophrenia.
3.1. Therapeutic Drug Monitoring/Adherence Program
Both CMHUs currently offer individual patient assessment that addresses symptom frequency and severity. Medications are chosen taking family and personal history into account. All psychotropic medications are regularly monitored for response, adherence, and adverse effects. Proven techniques [66] are used to improve adherence—motivational interviewing, eliciting self-reports, family confirmation, smart electronic reminders, blister packs, and determination of drug levels (TDM) [67].
We offer therapeutic drug monitoring (TDM) to patients experiencing adverse events, pregnant women, and women during the postpartum period [68]. TDM refers to the determination of the relationship between (1) drug dose and plasma levels, (2) plasma levels and therapeutic effects, and (3) plasma levels and adverse effects.
In the near future, we are planning the integration of therapeutic drug monitoring with pharmacogenetic testing [68]. This will allow useful correlations between drug serum concentrations, drug efficacy, and safety.
3.2. Individual/Group Patient and Family Sessions
Individual assessments and follow-up care are currently provided at both sites. Women-specific pharmacotherapy is stressed since the vast majority of scientific literature points to the fact that the efficacy, safety, and tolerability of AP medication differs in men and women [69]. This is based on sex differences in drug absorption, metabolism, and elimination. There are also differences in protein binding, because women tend to take more drugs, which also results in more drug interactions in women. Because current treatment guidelines are based predominantly on studies of men, this frequently results in women being overmedicated, which contributes to their greater risk of adverse effects [69]. There are differences in the effects of AP drugs according to their metabolic enzymes’ dependence on estrogen [69]. For these reasons, in our service, female-specific medications are carefully supervised and geared toward changing estrogen levels during menses, pregnancy, postpartum, and pre- and post-menopause.
Family sessions and family psychoeducation, as well as group therapies, are also provided [70]. Issues of safety in response to substance use, command hallucinations, persecutory delusions, tense family situations, forensic history, abuse, and exploitation, and suicidal urges are carefully monitored. Emergency hospitalization is organized when needed.
Over time, we have gained experience in addressing delusions in schizophrenia, and our teams specialize in addressing delusions common to women (denial of pregnancy, delusion of pregnancy, erotomania, delusional jealousy, dysmorphophobia, delusional parasitosis, and other somatic delusions). Our staff listen empathically, comment on the emotion that fuels the delusion, establish a therapeutic alliance, gradually suggest alternative explanations for troubling events, and remain always alert to safety risks [70].
3.3. Collaborative Programs (Primary Care)
Collaboration with primary care is vital in this population [71]. Multidisciplinary meetings that include general practitioners are held weekly with the aim of improving health risks such as hypertension, dyslipidemia, diabetes, and metabolic syndrome. Primary care is also crucial in the treatment of substance use disorders [72], smoking cessation, diet and exercise programming, and cancer screening [73,74].
3.4. Collaborative Programs (Other Medical Specialties)
The symptoms of psychiatric and neurologic disease often overlap, which makes collaboration with neurology essential for psychiatry. Sensory impairments are known to trigger delusions, which calls for close ties with ophthalmology and otolaryngology. Certain specifically female disorders (Turner syndrome, polycystic ovaries) increase the risk for schizophrenia [75,76], as do disorders more common in women than in men, such as systemic lupus erythematosus and other autoimmune disorders [77,78]. This requires liaisons with internal medicine and immunology.
We are currently organizing new collaborations [79] with gynecological services to increase screening for breast cancer and other gynecological cancers, because studies indicate that mortality from such cancers is increased in women with severe mental illness [80] compared, for instance, with women suffering from depression. Collaboration with oncology, dermatology, cardiology, and endocrinology is also being planned to reduce risks and improve the health of this population [81,82]. Health promotion interventions in collaboration with other medical specialties are in the planning phase based on life expectancy life expectancy data in women suffering from psychosis.
3.5. Suicide Risk—Prevention and Intervention
Suicide risk is high in this population, but suicidal behaviors are possible to prevent by early intervention.
Our service is part of the Catalonia Suicide Risk Code (CSRC), a secondary suicide prevention program, and the Epidemiology (CSRC-Epi) study, a registry-based study aiming to identify and document cases of attempted suicide [83].
Whenever there is suspicion of suicide risk (a bereavement, a break-up, a job loss, a friendship rupture, a child taken into care, depressive symptoms), a clinical appointment is scheduled within 7 days. The family is alerted, and patients are asked to call in daily to their case manager as a part of the Catalonia Suicide Risk Code [84]. Because women report significantly higher rates of stressful life events than men, and suicide methods differ between men and women, prevention and intervention need to be gender-specific.
3.6. Perinatal Mental Health
Women with schizophrenia show specific health needs according to age and reproductive stage. As stated earlier, careful monitoring of the efficacy and side effects of pharmacological treatment is critical during periods of hormonal transition [85].
Our community mental health team provides contraceptive and preconception advice, clinical assessment, and specialized intervention for women with psychotic illness during pregnancy and the postpartum period [85,86].
Psychiatrists, psychologists, and mental health nurses are members of the perinatal mental health team. Assessment of psychotropic drug efficacy and tolerability form part of our program, as does assessment of the quality of mother-infant interaction after delivery [87,88]. Several studies have noted impairment in mother-infant bonding in women with schizophrenia, which calls for support, education, and supervision of new mothers. As mentioned, close collaborations with gynecologists, obstetricians, and pediatricians are currently offered, and the plan is to expand this service.
3.7. Social Services
The social workers in our program provide a broad range of psychosocial interventions and supportive lifestyle interventions [89]. Once the two units are more closely amalgamated, social work plans to implement parent training and support groups for new mothers and for mothers who are at risk for losing custody of their children.
Our social workers find and help maintain appropriate supportive housing for this population of women [90,91]. A New York City study exploring risk factors for homelessness in severe mental illness investigated a cohort of 100 women with schizophrenia who fulfilled criteria for homelessness and 100 women without such a history [92]. Homeless women had higher rates of alcohol use and other substance use disorders as well as antisocial personality disorders. Overall, homeless women were less likely to benefit from family support. A recent systematic review and meta-analysis emphasized that female sex, a diagnosis of psychotic disorder, and substance use disorders are individual-level predictors for homelessness [92]. Housing First is an intervention widely implemented for homeless people suffering from mental illness in urban centers [93,94]. It has been demonstrated to have a positive effect on social stability [95] and is an approach that we are planning to emulate.
3.8. Home-Based Services
Community mental health outpatient services currently include home visits to postpartum women, domestically abused women, those suffering from difficulties in initial access to mental health outpatient services, and those who show poor engagement, suffer physical disabilities, or show poor adherence to psychiatric appointments [96]. Our plan is to expand this service.
Home-based treatment provides an alternative to inpatient care by offering multidisciplinary short-term intensive community support with the goal of assertively engaging patients in mental health care [97].
3.9. Peer and Family Support
Peer support is the ability of experts by experience to share what they have learned in a supportive and therapeutic way [98]. We are in the planning stage of hiring female peer support workers to help women, especially during the difficult postpartum period when many women with schizophrenia relapse. A recent study examined women’s experiences with peer support for mental health problems during the perinatal period and found them to be effective [99]. We also plan to involve family members in the comprehensive care of our patients [100].
3.10. Occupational Therapies
Women with schizophrenia tend to show better social and occupational functioning than men [101]. In Catalonia, a recent study investigated gender differences in social functioning in psychosocial rehabilitation services and concluded that gender-specific approaches to the rehabilitation process help both sexes improve their social skills [102]. The effects of occupational therapy on symptoms in schizophrenia have shown promise [103,104]. Occupational therapists and perinatal nurses, working together, are judged invaluable in addressing the needs of postpartum women with psychosis [105]. We are at the planning stage in recruiting an occupational therapist to engage women in art, crafts, preparation for employment, and other rehabilitative occupations.
3.11. Physical Activity and Leisure Programs
Because of low levels of aerobic and multiple medical comorbidities in this population, we found physical activity to be an essential part of comprehensive care [106]. It requires motivation because symptoms, side effects, and a lack of resources make physical activity difficult [107]. Both exercise and nutritional education strategies reduce weight gain and improve the health and well-being of our patients [108].
Exercise therapy has been found to also improve positive and negative symptoms, quality of life, and cognitive defects [109]. Using a biopsychological perspective [110], physical activities in our unit are adapted to the health needs and stages of women’s reproductive life-span: youth, pregnancy, postpartum, menopause, post-menopause, and old age.
3.12. Psychoeducation for Families and Patients
Psychoeducation in the setting of multi-family groups has been recommended in the treatment of schizophrenia [111]. Families of persons with schizophrenia almost always suffer from the burden of caring, each family situation remaining, nonetheless, somewhat unique [112]. We will offer psychoeducation via individual and group sessions for women and their families. A recent study explored the efficacy of programs designed for families to manage behavioral and prognostic uncertainty [113]. This is an interesting avenue to pursue, since symptom fluctuation and unexpected development in the course of schizophrenia can make living with someone with this diagnosis very challenging [114].
4. Future Directions
4.1. Phase I: Identification
The first step will be the identification of women with schizophrenia who are presently attending the two community mental health outpatient services (CMHU Rambla and CMHU Sant Cugat). Electronic searches through medical records will identify women suffering from schizophrenia, schizoaffective disorder, and delusional disorders as our special focus. All our attendees have already been assigned a general practitioner, with medical diagnoses and interventions currently documented in our computerized health system. We expect that approximately 400 women will be eligible for referral to the combined unit.
4.2. Phase II: Collaboration
The second step will be re-screening each of the women for potentially necessary referral within our collaborative multidisciplinary and multispecialty network.
4.3. Phase III: Planned Improvements
The third step will be the implementation of therapies that have been identified in the literature as effective, but that are not yet part of our program. In this third phase, we will hire more staff, and develop training programs and evaluation routines to assess the effectiveness of our offerings.
Table 2 presents the main phases of implementation.

Table 2.
Phases of implementation of the unit for women with schizophrenia.
Evaluations are planned at every stage of implementation of the transformation of the two existing services into the amalgamated unit for women with schizophrenia spectrum disorders.
The following scales are proposed (previously shown to be reliable and valid) at baseline, at the end of each phase of implementation, and annually thereafter: (1) the Positive and Negative Syndrome Scale (PANSS), Spanish Version for the assessment of psychotic symptoms [115,116], (2) the Personal and Social Performance Scale (PSP) to evaluate functionality [117,118], (3) the Clinical Global Impression Scale- Schizophrenia (CGI-SCH) [119,120], (4) the Health of the Nation Outcomes Scale (HoNos) [121,122] for the evaluation of health in psychiatric patients in the community, and (5) the Spanish Version of the Client Satisfaction Questionnaire (CSQ-8) [123] to evaluate clients satisfaction [124].
5. Methods
Screening and Selection of Evidence of Women-Specific Care Needs in Schizophrenia
We performed electronic searches through Medline via the PubMed database from 2000 to 2022, using the following search terms: women AND schizophrenia AND care. In order to access information on the paramedical (occupational, social, relational) needs of our intended population that were unavailable on PubMed, we also searched Google Scholar and the reference lists of systematic reviews by experts in the field of psychosocial care in the context of psychosis. These review papers were also included in our review and served as potential sources of additional papers. Several early classic papers were included if they were relevant to an all-women’s service.
Papers were included if they met the following inclusion criteria: (1) study participants were women with schizophrenia and/or other related psychoses, (2) the paper included a report on the medical, mental health, or psychosocial care of women with schizophrenia, (3) the paper included recommendations or suggestions for specific care, (4) the paper was published in a peer-reviewed journal, and (5) the language of the paper was English, Spanish, French, or German. Papers not fulfilling these criteria were excluded.
One thousand and twelve records were initially screened. Figure 1 shows the flow chart of the screened, excluded, and included papers. In the end, a total of 108 papers were included.
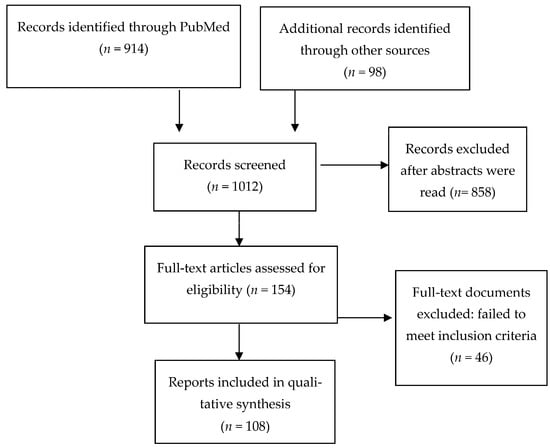
Figure 1.
Flow diagram of the included studies.
We grouped the included studies into three categories: (1) mental health issues, (2) non-psychiatric medical issues, and (3) parental and occupational/social issues.
6. Conclusions
Women with schizophrenia have sex-specific health needs that differ from those of men and also differ according to life stages.
A specific unit for women with schizophrenia and related disorders represents an important resource that can, in several ways, improve clinical care for this population.
Our hope is that the new unit will evolve to become a hub for exemplary clinical care.
Author Contributions
A.G.-R. wrote the first draft of the manuscript. M.V.S. collaborated with A.G.-R. on subsequent versions and revised the paper. M.N., P.B., E.R., A.B. and J.P.P. collaborated on writing the paper and building tables. J.A.M. supervised and critically reviewed the content. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this review are available on request from the corresponding author.
Conflicts of Interest
A.G.-R. has received free registration or travel funds for congresses from Janssen, Lundbeck-Otsuka, and Angelini. J.A.-M. has received consultancy and/or lecture honoraria from Sanofi, Pfizer, Servier, Janssen, and Lundbeck-Otsuka.
References
- Seeman, M.V.; Cohen, R. A service for women with schizophrenia. Psychiatr. Serv. 1998, 49, 674–677. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.J.; O'Donovan, M.C. Schizophrenia and the neurodevelopmental continuum: Evidence from genomics. World Psychiatry 2017, 16, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Suvisaari, J.M.; Taxell-Lassas, V.; Pankakoski, M.; Haukka, J.K.; Lönnqvist, J.K.; Häkkinen, L.T. Obstetric complications as risk factors for schizophrenia spectrum psychoses in offspring of mothers with psychotic disorder. Schizophr. Bull. 2013, 39, 1056–1066. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pence, A.Y.; Pries, L.K.; Ferrara, M.; Rutten, B.P.F.; van Os, J.; Guloksuz, S. Gender differences in the association between environment and psychosis. Schizophr. Res. 2022, 243, 120–137. [Google Scholar] [CrossRef] [PubMed]
- Brzezinski-Sinai, N.A.; Brzezinski, A. Schizophrenia and Sex Hormones: What Is the Link? Front. Psychiatry 2020, 11, 693. [Google Scholar] [CrossRef]
- Abel, K.M.; Drake, R.; Goldstein, J.M. Sex differences in schizophrenia. Int. Rev. Psychiatry 2010, 22, 417–428. [Google Scholar] [CrossRef]
- Posada Correa, A.M.; Andrade Carrillo, R.A.; Suarez Vega, D.C.; Gómez Cano, S.; Agudelo Arango, L.G.; Tabares Builes, L.F.; Agudelo García, Á.M.; Uribe Villa, E.; Aguirre-Acevedo, D.C.; López-Jaramillo, C. Sexual and Reproductive Health in Patients with Schizophrenia and Bipolar Disorder. Rev. Colomb. Psiquiatr. 2020, 49, 15–22. [Google Scholar] [CrossRef]
- Thomas, N.; Gurvich, C.; Hudaib, A.R.; Gavrilidis, E.; de Castella, R.A.; Thomas, E.H.; Kulkarni, J. Serum estradiol as a blood-based biomarker predicting hormonal treatment outcomes in women with schizophrenia. Psychoneuroendocrinology 2021, 126, 105165. [Google Scholar] [CrossRef] [PubMed]
- Heitz, U.; Studerus, E.; Menghini-Müller, S.; Papmeyer, M.; Egloff, L.; Ittig, S.; Navarra, A.; Andreou, C.; Riecher-Rössler, A. Gender differences in first self-perceived signs and symptoms in patients with an at-risk mental state and first-episode psychosis. Early Interv. Psychiatry 2019, 13, 582–588. [Google Scholar] [CrossRef]
- Spitz, A.; Studerus, E.; Koranyi, S.; Rapp, C.; Ramyead, A.; Ittig, S.; Heitz, U.; Uttinger, M.; Riecher-Rössler, A. Correlations between self-rating and observer-rating of psychopathology in at-risk mental state and first-episode psychosis patients: Influence of disease stage and gender. Early Interv. Psychiatry 2017, 11, 461–470. [Google Scholar] [CrossRef]
- Riecher-Rössler, A.; Butler, S.; Kulkarni, J. Sex and gender differences in schizophrenic psychoses-a critical review. Arch. Women’s Ment. Health 2018, 21, 627–648. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Seeman, M.V.; Díaz-Pons, A.; Ayesa-Arriola, R.; Natividad, M.; Calvo, E.; Monreal, J.A. Do sex/gender and menopause influence the psychopathology and comorbidity observed in delusional disorders? J. Clin. Med. 2022, 11, 4550. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Ma, X.; Wang, G.; Yang, J.; Wang, C. Why sex differences in schizophrenia? J. Transl. Neurosci. 2016, 1, 37–42. [Google Scholar]
- Seeman, M.V. Sex differences in schizophrenia relevant to clinical care. Expert. Rev. Neurother. 2021, 21, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Seeman, M.V.; González-Rodríguez, A. Stratification by sex and hormone level when contrasting men and women in schizophrenia trials will improve personalized treatment. J. Pers. Med. 2021, 11, 929. [Google Scholar] [CrossRef]
- Mazza, M.; Caroppo, E.; De Berardis, D.; Marano, G.; Avallone, C.; Kotzalidis, G.D.; Janiri, D.; Moccia, L.; Simonetti, A.; Conte, E.; et al. Psychosis in women: Time for personalized treatment. J. Pers. Med. 2021, 11, 1279. [Google Scholar] [CrossRef] [PubMed]
- Turrone, P.; Seeman, M.V.; Silvestri, S. Estrogen receptor activation and tardive dyskinesia. Can. J. Psychiatry 2000, 45, 288–290. [Google Scholar] [CrossRef]
- Álvarez, A.; Guàrdia, A.; González-Rodríguez, A.; Betriu, M.; Palao, D.; Monreal, J.A.; Soria, V.; Labad, J. A systematic review and meta-analysis of suicidality in psychotic disorders: Stratified analyses by psychotic subtypes, clinical setting and geographical region. Neurosci. Biobehav. Rev. 2022, 143, 104964. [Google Scholar] [CrossRef]
- Seeman, M.V. Suicide among women with schizophrenia spectrum disorders. J. Psychiatr. Pract. 2009, 15, 235–242. [Google Scholar] [CrossRef]
- Sommer, I.E.; Brand, B.A.; Gangadin, S.; Tanskanen, A.; Tiihonen, J.; Taipale, H. Women with schizophrenia-spectrum disorders after menopause: A vulnerable group for relapse. Schizophr. Bull. 2022, 49, 136–143. [Google Scholar] [CrossRef]
- Goldstein, J.M.; Cohen, L.S.; Horton, N.J.; Lee, H.; Andersen, S.; Tohen, M.; Crawford, A.; Tollefson, G. Sex differences in clinical response to olanzapine compared with haloperidol. Psychiatry Res. 2002, 110, 27–37. [Google Scholar] [CrossRef]
- Kulkarni, J. Estrogen—A key neurosteroid in the understanding and treatment of mental illness in women. Psychiatry Res. 2022, 319, 114991. [Google Scholar] [CrossRef] [PubMed]
- Paderina, D.Z.; Boiko, A.S.; Pozhidaev, I.V.; Mednova, I.A.; Goncharova, A.A.; Bocharova, A.V.; Fedorenko, O.Y.; Kornetova, E.G.; Semke, A.V.; Bokhan, N.A.; et al. The gender-specific association of drd2 polymorphism with metabolic syndrome in patients with schizophrenia. Genes 2022, 13, 1312. [Google Scholar] [CrossRef]
- Pu, C.; Huang, B.; Zhou, T.; Cheng, Z.; Wang, Y.; Shi, C.; Yu, X. Gender differences in the first-year antipsychotic treatment for Chinese first-episode schizophrenia. Neuropsychiatr. Dis. Treat. 2020, 16, 3145–3152. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.; Wang, D.; Zhou, H.; Chen, D.; Xiu, M.; Cui, L.; Zhang, X. Tardive dyskinesia in Chinese patients with schizophrenia: Prevalence, clinical correlates and relationship with cognitive impairment. J. Psychiatr. Res. 2022, 151, 181–187. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Catalán, R.; Penadés, R.; Ruiz Cortés, V.; Torra, M.; Seeman, M.V.; Bernardo, M. Antipsychotic response worsens with postmenopausal duration in women with schizophrenia. J. Clin. Psychopharmacol. 2016, 36, 580–587. [Google Scholar] [CrossRef]
- Brzezinski, A.; Brzezinski-Sinai, N.A.; Seeman, M.V. Treating schizophrenia during menopause. Menopause 2017, 24, 582–588. [Google Scholar] [CrossRef]
- Kulkarni, J.; Fitzgerald, P.; Seeman, M.V. Clinical needs of women with schizophrenia. In Pharmacological and Psychosocial Treatments in Schizophrenia, 3rd ed.; Castle, D.J., Copolov, D.L., Wykes, T., Mueser, K.T., Eds.; Informa Healthcare, Ltd.: London, UK, 2012; pp. 183–201. [Google Scholar]
- González-Rodríguez, A.; Seeman, M.V.; Álvarez, A.; Guàrdia, A.; Sanz, N.; Fucho, G.F.; Palao, D.J.; Labad, J. Care for women with delusional disorder: Towards a specialized approach. Women 2021, 1, 46–59. [Google Scholar] [CrossRef]
- Bergemann, N.; Parzer, P.; Runnebaum, B.; Resch, F.; Mundt, C. Estrogen, menstrual cycle phases, and psychopathology in women suffering from schizophrenia. Psychol. Med. 2007, 37, 1427–1436. [Google Scholar] [CrossRef]
- Reilly, T.J.; Sagnay de la Bastida, V.C.; Joyce, D.W.; Cullen, A.E.; McGuire, P. Exacerbation of psychosis during the perimenstrual phase of the menstrual cycle: Systematic review and meta-analysis. Schizophr. Bull. 2020, 46, 78–90. [Google Scholar] [CrossRef]
- Kiliçaslan, E.E.; Erol, A.; Zengin, B.; Çetinay Aydin, P.; Mete, L. Association between age at onset of schizophrenia and age at menarche. Noro. Psikiyatr. Ars. 2014, 51, 211–215. [Google Scholar] [CrossRef]
- Riecher-Rössler, A.; Häfner, H.; Stumbaum, M.; Schmidt, R. Do estrogens have an antipsychotic action? Fortschr. Neurol. Psychiatr. 1994, 62, 22–28. [Google Scholar] [CrossRef]
- Zerihun, T.; Sorsdahl, K.; Hanlon, C. Family planning for women with severe mental illness in rural Ethiopia: A qualitative study. Reprod. Health 2021, 18, 191. [Google Scholar] [CrossRef]
- Taylor, C.; Stewart, R.; Gibson, R.; Pasupathy, D.; Shetty, H.; Howard, L. Birth without intervention in women with severe mental illness: Cohort study. Br. J. Psych. Open 2022, 8, e50. [Google Scholar] [CrossRef]
- Chang, S.; Jeyagurunathan, A.; Lau, J.H.; Shafie, S.; Samari, E.; Cetty, L.; Mok, Y.M.; Verma, S.; Subramaniam, M. Problematic drug use among outpatients with schizophrenia and related psychoses. Front. Psychiatry 2021, 12, 762988. [Google Scholar] [CrossRef]
- Kouidrat, Y.; Amad, A.; Lalau, J.D.; Loas, G. Eating disorders in schizophrenia: Implications for research and management. Schizophr. Res. Treatment 2014, 2014, 791573. [Google Scholar] [CrossRef]
- Thara, R.; Kamath, S. Women and schizophrenia. Indian J. Psychiatry 2015, 57 (Suppl. 2), S246–S251. [Google Scholar] [CrossRef]
- Zhang, X.; Dupre, M.E.; Qiu, L.; Zhou, W.; Zhao, Y.; Gu, D. Age and sex differences in the association between access to medical care and health outcomes among older Chinese. BMC Health Serv. Res. 2018, 18, 1004. [Google Scholar] [CrossRef]
- Seeman, M.V. Psychosis and Physical Comorbidity. In Mental Health and Illness of Women. Mental Health and Illness Worldwide; Chandra, P., Herrman, H., Fisher, J., Riecher-Rössler, A., Eds.; Springer: Singapore, 2019; pp. 1–28. [Google Scholar] [CrossRef]
- Lindamer, L.A.; Buse, D.C.; Auslander, L.; Unützer, J.; Bartels, S.J.; Jeste, D.V. A comparison of gynecological variables and service use among older women with and without schizophrenia. Psychiatr. Serv. 2003, 54, 902–904. [Google Scholar] [CrossRef]
- Irwin, K.E.; Callaway, C.A.; Corveleyn, A.E.; Pappano, C.R.; Barry, M.J.; Tiersma, K.M.; Nelson, Z.E.; Fields, L.E.; Pirl, W.F.; Greer, J.A.; et al. Study protocol for a randomized trial of bridge: Person-centered collaborative care for serious mental illness and cancer. Contemp. Clin. Trials 2022, 123, 106975. [Google Scholar] [CrossRef]
- Seeman, M.V. Preventing breast cancer in women with schizophrenia. Acta Psychiatr. Scand. 2011, 123, 107–117. [Google Scholar] [CrossRef]
- Wootten, J.C.; Wiener, J.C.; Blanchette, P.S.; Anderson, K.K. Cancer incidence and stage at diagnosis among people with psychotic disorders: Systematic review and meta-analysis. Cancer Epidemiol. 2022, 80, 102233. [Google Scholar] [CrossRef]
- Kalucy, M.J.; Grunstein, R.; Lambert, T.; Glozier, N. Obstructive sleep apnoea and schizophrenia--a research agenda. Sleep Med. Rev. 2013, 17, 357–365. [Google Scholar] [CrossRef]
- Seeman, M.V. Diagnosis and treatment of sleep apnoea in women with schizophrenia. J. Ment. Health 2014, 23, 191–196. [Google Scholar] [CrossRef]
- Szaulińska, K.; Wichniak, A. BMI-NECK: A simple assessment of risk of obstructive sleep apnea in schizophrenia. J. Psychiatr. Res. 2020, 125, 33–37. [Google Scholar] [CrossRef]
- Seeman, M.V. The role of mental health services in addressing HIV infection among women with serious mental illness. Psychiatr. Serv. 2015, 66, 966–974. [Google Scholar] [CrossRef]
- Velligan, D.I.; Weiden, P.J.; Sajatovic, M.; Scott, J.; Carpenter, D.; Ross, R.; Docherty, J.P. Strategies for addressing adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. J. Psychiatr. Pract. 2010, 16, 306–324. [Google Scholar] [CrossRef]
- Druschky, K.; Bleich, S.; Grohmann, R.; Burda, K.; Frieling, H.; Hillemacher, T.; Neyazi, A.; Stübner, S.; Toto, S. Severe hair loss associated with psychotropic drugs in psychiatric inpatients-Data from an observational pharmacovigilance program in German-speaking countries. Eur. Psychiatry 2018, 54, 117–123. [Google Scholar] [CrossRef]
- Edinoff, A.N.; Silverblatt, N.S.; Vervaeke, H.E.; Horton, C.C.; Girma, E.; Kaye, A.D.; Kaye, A.; Kaye, J.S.; Garcia, A.J.; Neuchat, E.E.; et al. Hyperprolactinemia, clinical considerations, and infertility in women on antipsychotic medications. Psychopharmacol. Bull. 2021, 51, 131–148. [Google Scholar]
- Crews, M.P.; Howes, O.D. Is antipsychotic treatment linked to low bone mineral density and osteoporosis? A review of the evidence and the clinical implications. Hum. Psychopharmacol. 2012, 27, 15–23. [Google Scholar] [CrossRef]
- Rodolico, A.; Siafis, S.; Bighelli, I.; Samara, M.T.; Hansen, W.P.; Salomone, S.; Aguglia, E.; Cutrufelli, P.; Bauer, I.; Baeckers, L.; et al. Antipsychotic dose reduction compared to dose continuation for people with schizophrenia. Cochrane Database Syst. Rev. 2022, 11, CD014384. [Google Scholar]
- Chen, C.Y.; Lane, H.Y.; Lin, C.H. Effects of antipsychotics on bone mineral density in patients with schizophrenia: Gender differences. Clin. Psychopharmacol. Neurosci. 2016, 14, 238–249. [Google Scholar] [CrossRef]
- Teodorescu, A.; Ifteni, P.; Moga, M.A.; Burtea, V.; Bigiu, N. Dilemma of treating schizophrenia during pregnancy: A case series and a review of literature. BMC Psychiatry 2017, 17, 311. [Google Scholar] [CrossRef]
- Gentile, S.; Fusco, M.L. Schizophrenia and motherhood. Psychiatry Clin. Neurosci. 2019, 73, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Dazzan, P. Schizophrenia during pregnancy. Curr. Opin. Psychiatry 2021, 34, 238–244. [Google Scholar] [CrossRef]
- Lin, H.C.; Chen, I.J.; Chen, Y.H.; Lee, H.C.; Wu, F.J. Maternal schizophrenia and pregnancy outcome: Does the use of antipsychotics make a difference? Schizophr. Res. 2010, 116, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Patrick, P.M.; Reupert, A.E.; McLean, L.A. Relational trajectories in families with parental mental illness: A grounded theory approach. BMC Psychol. 2020, 8, 68. [Google Scholar] [CrossRef]
- Vigod, S.N.; Kurdyak, P.A.; Dennis, C.L.; Gruneir, A.; Newman, A.; Seeman, M.V.; Rochon, P.A.; Anderson, G.M.; Grigoriadis, S.; Ray, J.G. Maternal and newborn outcomes among women with schizophrenia: A retrospective population-based cohort study. BJOG 2014, 121, 566–574. [Google Scholar] [CrossRef]
- Heinonen, E.; Forsberg, L.; Nörby, U.; Wide, K.; Källén, K. Neonatal morbidity after fetal exposure to antipsychotics: A national register-based study. BMJ Open. 2022, 12, e061328. [Google Scholar] [CrossRef] [PubMed]
- Seeman, M.V. Antipsychotic-induced somnolence in mothers with schizophrenia. Psychiatr. Q. 2012, 83, 83–89. [Google Scholar] [CrossRef]
- Thara, R.; Kamath, S.; Kumar, S. Women with schizophrenia and broken marriages—doubly disadvantaged? Part I: Patient perspective. Int. J. Soc. Psychiatry 2003, 49, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Thara, R.; Kamath, S.; Kumar, S. Women with schizophrenia and broken marriages—doubly disadvantaged? Part II: Family perspective. Int. J. Soc. Psychiatry 2003, 49, 233–240. [Google Scholar] [CrossRef]
- Seeman, M.V. Intervention to prevent child custody loss in mothers with schizophrenia. Schizophr. Res. Treatment 2012, 2012, 796763. [Google Scholar] [CrossRef]
- Mercolini, L. Editorial: Advances in therapeutic drug monitoring of psychiatric subjects: Analytical strategies and clinical approaches. Front. Psychiatry 2022, 13, 1056380. [Google Scholar] [CrossRef]
- Cahaya, N.; Kristina, S.A.; Widayanti, A.W.; Green, J. Interventions to improve medication adherence in people with schizophrenia: A systematic review. Patient Prefer. Adherence 2022, 16, 2431–2449. [Google Scholar] [CrossRef]
- Pennazio, F.; Brasso, C.; Villari, V.; Rocca, P. Current status of therapeutic drug monitoring in mental health treatment: A review. Pharmaceutics 2022, 14, 2674. [Google Scholar] [CrossRef] [PubMed]
- Brand, B.A.; Haveman, Y.R.A.; de Beer, F.; de Boer, J.N.; Dazzan, P.; Sommer, I.E.C. Antipsychotic medication for women with schizophrenia spectrum disorders. Psychol. Med. 2021, 52, 1–15. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Seeman, M.V. Addressing delusions in women and men with delusional disorder: Key points for clinical management. Int. J. Environ. Res. Public. Health 2020, 17, 4583. [Google Scholar] [CrossRef] [PubMed]
- Aragonès, E.; López-Cortacans, G.; Cardoner, N.; Tomé-Pires, C.; Porta-Casteràs, D.; Palao, D.; INDIIResearch Team. Barriers, facilitators, and proposals for improvement in the implementation of a collaborative care program for depression: A qualitative study of primary care physicians and nurses. BMC Health Serv. Res. 2022, 22, 446. [Google Scholar] [CrossRef]
- Andreu, M.; Alcaraz, N.; Gual, A.; Segura, L.; Barrio, P. Primary care provider expectations of addiction services and patients in Spain. Fam. Pract. 2022, 39, 269–274. [Google Scholar] [CrossRef]
- Hwong, A.; Wang, K.; Bent, S.; Mangurian, C. Breast cancer screening in women with schizophrenia: A systematic review and meta-analysis. Psychiatr. Serv. 2020, 71, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Cather, C.; Pachas, G.N.; Cieslak, K.M.; Evins, A.E. Achieving smoking cessation in individuals with schizophrenia: Special considerations. C.N.S. Drugs. 2017, 31, 471–481. [Google Scholar] [CrossRef]
- Kamitaki, N.; Sekar, A.; Handsaker, R.E.; de Rivera, H.; Tooley, K.; Morris, D.L.; Taylor, K.E.; Whelan, C.W.; Tombleson, P.; Loohuis, L.M.O.; et al. Complement genes contribute sex-biased vulnerability in diverse disorders. Nature 2020, 582, 577–581. [Google Scholar] [CrossRef]
- Björlin Avdic, H.; Butwicka, A.; Nordenström, A.; Almqvist, C.; Nordenskjöld, A.; Engberg, H.; Frisén, L. Neurodevelopmental and psychiatric disorders in females with Turner syndrome: A population-based study. J. Neurodev. Disord. 2021, 13, 51. [Google Scholar] [CrossRef] [PubMed]
- Gui, Y.; Bai, W.; Xu, J.; Duan, X.; Zhan, F.; Zhao, C.; Jiang, Z.; Li, Z.; Wu, L.; Liu, S.; et al. Sex differences in systemic lupus erythematosus (SLE): An inception cohort of the Chinese SLE Treatment and Research Group (CSTAR) registry XVII. Chin. Med. J. 2022, 135, 2191–2199. [Google Scholar] [CrossRef] [PubMed]
- Ngo, S.T.; Steyn, F.J.; McCombe, P.A. Gender differences in autoimmune disease. Front. Neuroendocrinol. 2014, 35, 347–369. [Google Scholar] [CrossRef]
- Sporinova, B.; Manns, B.; Tonelli, M.; Hemmelgarn, B.; MacMaster, F.; Mitchell, N.; Au, F.; Ma, Z.; Weaver, R.; Quinn, A. Association of mental health disorders with health care utilization and costs among adults with chronic disease. JAMA Netw. Open 2019, 2, e199910. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.R.; Kuliszewski, M.G.; Hosler, A.S.; Leinung, M.C.; Zhang, X.; Zhang, W.; Du, Z.; Schymura, M.J.; Boscoe, F.P. Association between preexisting mental illnesses and mortality among medicaid-insured women diagnosed with breast cancer. Soc. Sci. Med. 2021, 270, 113643. [Google Scholar] [CrossRef]
- Nemani, K.L.; Greene, M.C.; Ulloa, M.; Vincenzi, B.; Copeland, P.M.; Al-Khadari, S.; Henderson, D.C. Clozapine, diabetes mellitus, cardiovascular risk and mortality: Results of a 21-year naturalistic study in patients with schizophrenia and schizoaffective disorder. Clin. Schizophr. Relat. Psychoses. 2019, 12, 168–176. [Google Scholar] [CrossRef]
- Westman, J.; Eberhard, J.; Gaughran, F.P.; Lundin, L.; Stenmark, R.; Edman, G.; Eriksson, S.V.; Jedenius, E.; Rydell, P.; Overgaard, K.; et al. Outcome of a psychosocial health promotion intervention aimed at improving physical health and reducing alcohol use in patients with schizophrenia and psychotic disorders (MINT). Schizophr. Res. 2019, 208, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Mortier, P.; Vilagut, G.; Puértolas Gracia, B.; De Inés Trujillo, A.; Alayo Bueno, I.; Ballester Coma, L.; Blasco Cubedo, M.J.; Cardoner, N.; Colls, C.; Elices, M.; et al. Catalonia Suicide Risk Code Epidemiology (CSRC-Epi) study: Protocol for a population-representative nested case-control study of suicide attempts in Catalonia, Spain. BMJ Open 2020, 10, e037365. [Google Scholar] [CrossRef] [PubMed]
- Pérez, V.; Elices, M.; Prat, B.; Vieta, E.; Blanch, J.; Alonso, J.; Pifarré, J.; Mortier, P.; Cebrià, A.I.; Campillo, M.T.; et al. The Catalonia Suicide Risk Code: A secondary prevention program for individuals at risk of suicide. J. Affect. Disord. 2020, 268, 201–205. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Guàrdia, A.; Álvarez-Pedrero, A.; Betriu, M.; Cobo, J.; Acebillo, S.; Monreal, J.A.; Seeman, M.V.; Palao, D.; Labad, J. Women with schizophrenia over the life span: Health promotion, treatment and outcomes. Int. J. Environ. Res. Public. Health 2020, 17, 5594. [Google Scholar] [CrossRef] [PubMed]
- Alves, S.P.; Costa, T.; Ribeiro, I.; Néné, M.; Sequeira, C. Perinatal mental health counselling programme: A scoping review. Patient. Educ. Couns. 2023, 106, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Healy, S.J.; Lewin, J.; Butler, S.; Vaillancourt, K.; Seth-Smith, F. Affect recognition and the quality of mother-infant interaction: Understanding parenting difficulties in mothers with schizophrenia. Arch. Womens Ment. Health 2016, 19, 113–124. [Google Scholar] [CrossRef]
- Layton, H.; Owais, S.; Savoy, C.D.; Van Lieshout, R.J. Depression, Anxiety, and mother-infant bonding in women seeking treatment for postpartum depression before and during the Covid-19 pandemic. J. Clin. Psychiatry 2021, 82, 21m13874. [Google Scholar] [CrossRef]
- Cesar, P.; King, R. Social workers' beliefs about the interventions for schizophrenia and depression: A comparison with the public and other health professionals—An Australian analysis. Br. J. Soc. Work. 2015, 45, 1750–1770. [Google Scholar] [CrossRef]
- Caton, C.L.; Shrout, P.E.; Dominguez, B.; Eagle, P.F.; Opler, L.A.; Cournos, F. Risk factors for homelessness among women with schizophrenia. Am. J. Public Health 1995, 85 Pt 1, 1153–1156. [Google Scholar] [CrossRef]
- Li, K.Y.; Wu, Y.H.; Chen, H.Y. Predictors of personal recovery for individuals with schizophrenia spectrum disorders living in the community. Clin. Psychol. Psychother. 2022, 30, 179–187. [Google Scholar] [CrossRef]
- Nilsson, S.F.; Nordentoft, M.; Hjorthøj, C. Individual-level predictors for becoming homeless and exiting homelessness: A systematic review and meta-analysis. J. Urban Health 2019, 96, 741–750. [Google Scholar] [CrossRef]
- Stergiopoulos, V.; Mejia-Lancheros, C.; Nisenbaum, R.; Wang, R.; Lachaud, J.; O'Campo, P.; Hwang, S.W. Long-term effects of rent supplements and mental health support services on housing and health outcomes of homeless adults with mental illness: Extension study of the At Home/Chez Soi randomised controlled trial. Lancet Psychiatry 2019, 6, 915–925. [Google Scholar] [CrossRef] [PubMed]
- O'Campo, P.; Stergiopoulos, V.; Nir, P.; Levy, M.; Misir, V.; Chum, A.; Arbach, B.; Nisenbaum, R.; To, M.J.; Hwang, S.W. How did a Housing First intervention improve health and social outcomes among homeless adults with mental illness in Toronto? Two-year outcomes from a randomised trial. BMJ Open 2016, 6, 010581. [Google Scholar] [CrossRef]
- Lanham, J.S.; White, P.; Gaffney, B. Care of people experiencing homelessness. Am. Fam. Physician 2022, 106, 684–693. [Google Scholar] [PubMed]
- Reifler, B.V.; Bruce, M.L. Home-based mental health services for older adults: A review of ten model programs. Am. J. Geriatr. Psychiatry 2014, 22, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, V.; Tehranidoost, M.; Yunesian, M.; Amini, H.; Mohammadi, M.; Jalali Roudsari, M. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: A 12-month randomized controlled study. Community Ment. Health J. 2012, 48, 766–770. [Google Scholar] [CrossRef]
- Shalaby, R.A.H.; Agyapong, V.I.O. Peer support in mental health: Literature review. JMIR Ment. Health 2020, 7, e15572. [Google Scholar] [CrossRef]
- Rice, C.; Ingram, E.; O'Mahen, H. A qualitative study of the impact of peer support on women’s mental health treatment experiences during the perinatal period. BMC Pregnancy Childbirth. 2022, 22, 689. [Google Scholar] [CrossRef]
- Taylor, B.L.; Billings, J.; Morant, N.; Bick, D.; Johnson, S. Experiences of how services supporting women with perinatal mental health difficulties work with their families: A qualitative study in England. BMJ Open 2019, 9, e030208. [Google Scholar] [CrossRef]
- Ochoa, S.; Usall, J.; Cobo, J.; Labad, X.; Kulkarni, J. Gender differences in schizophrenia and first-episode psychosis: A comprehensive literature review. Schizophr. Res. Treatment. 2012, 2012, 916198. [Google Scholar] [CrossRef]
- Prat, G.; Escandell, M.J.; Garcia-Franco, M.; Martín-Martínez, J.R.; Tortades, I.; Vilamala, S.; Calderón, M.; Torras, R.; Ochoa, S.; Casas-Anguera, E. Gender differences in social functioning in people with schizophrenia in psychosocial rehabilitation services using one-dimensional and multidimensional instruments. Compr. Psychiatry 2018, 87, 120–122. [Google Scholar] [CrossRef]
- Ercan Doğu, S.; Örsel, S. The relationship between psychopathology, occupational balance, and quality of life among people with schizophrenia. Aust. Occup. Ther. J. 2022; in press. [Google Scholar]
- Foruzandeh, N.; Parvin, N. Occupational therapy for inpatients with chronic schizophrenia: A pilot randomized controlled trial. Jpn. J. Nurs. Sci. 2013, 10, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Froehlich, J.; Donovan, A.; Ravlin, E.; Fortier, A.; North, J.; Bloch, M.K. Daily routines of breastfeeding mothers. Work 2015, 50, 433–442. [Google Scholar] [CrossRef]
- Curcic, D.; Stojmenovic, T.; Djukic-Dejanovic, S.; Dikic, N.; Vesic-Vukasinovic, M.; Radivojevic, N.; Andjelkovic, M.; Borovcanin, M.; Djokic, G. Positive impact of prescribed physical activity on symptoms of schizophrenia: Randomized clinical trial. Psychiatr. Danub. 2017, 29, 459–465. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, G.; Kim, C.E.; Ryu, S. Physical activity of patients with chronic schizophrenia and related clinical factors. Psychiatry Investig. 2018, 15, 811–817. [Google Scholar] [CrossRef]
- Sevillano-Jiménez, A.; Romero-Saldaña, M.; García-Rodríguez, M.; Molina-Luque, R.; Molina-Recio, G. Nutritional impact and eating pattern changes in schizophrenic spectrum disorders after health education program on symbiotic dietary modulation offered by specialised psychiatric nursing-two-arm randomised clinical trial. Nutrients 2022, 14, 5388. [Google Scholar] [CrossRef] [PubMed]
- Girdler, S.J.; Confino, J.E.; Woesner, M.E. Exercise as a treatment for schizophrenia: A review. Psychopharmacol. Bull. 2019, 49, 56–69. [Google Scholar]
- Arnautovska, U.; Kesby, J.P.; Korman, N.; Rebar, A.L.; Chapman, J.; Warren, N.; Rossell, S.L.; Dark, F.L.; Siskind, D. Biopsychology of physical activity in people with schizophrenia: An integrative perspective on barriers and intervention strategies. Neuropsychiatr. Dis. Treat. 2022, 18, 2917–2926. [Google Scholar] [CrossRef] [PubMed]
- Sari, A.; Duman, Z.Ç. Effects of the family support and psychoeducation program based on the Calgary Family Intervention Model on the coping, psychological distress and psychological resilience levels of the family caregivers of chronic psychiatric patients. Arch. Psychiatr. Nurs. 2022, 41, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G. Schizophrenia in a member of the family: Burden, expressed emotion and addressing the needs of the whole family. S. Afr. J. Psychiatr. 2016, 22, 922. [Google Scholar] [CrossRef]
- Bora, S.T.; Buldukoğlu, K.; Bailey, D.E., Jr. Effectiveness of an uncertainty management psychoeducation program for schizophrenia caregivers: A randomized controlled trial. J. Am. Psychiatr. Nurses. Assoc. 2022; in press. [Google Scholar]
- Amsalem, D.; Jankowski, S.E.; Pagdon, S.; Valeri, L.; Smith, S.; Yang, L.H.; Markowitz, J.C.; Lewis-Fernández, R.; Dixon, L.B. “It is hard to be a woman with schizophrenia”: Randomized controlled trial of a brief video intervention to reduce public stigma in young adults. J. Clin. Psychiatry 2022, 84, 22m14534. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef]
- Peralta, V.; Cuesta, M.J. Psychometric properties of the positive and negative syndrome scale (PANSS) in schizophrenia. Psychiatry Res. 1994, 53, 31–40. [Google Scholar] [CrossRef]
- Apiquian, R.; Elena Ulloa, R.; Herrera-Estrella, M.; Moreno-Gómez, A.; Erosa, S.; Contreras, V.; Nicolini, H. Validity of the Spanish version of the Personal and Social Performance scale in schizophrenia. Schizophr. Res. 2009, 112, 181–186. [Google Scholar] [CrossRef]
- Garcia-Portilla, M.P.; Saiz, P.A.; Bousoño, M.; Bascaran, M.T.; Guzmán-Quilo, C.; Bobes, J.; en nombre del grupo de validación de la versión española de la escala de Funcionamiento Personal y Social (PSP). Validation of the Spanish Personal and Social Performance scale (PSP) in outpatients with stable and unstable schizophrenia. Rev. Psiquiatr. Salud Ment. 2011, 4, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Endicott, J.; Spitzer, R.L.; Fleiss, J.L.; Cohen, J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch. Gen. Psychiatry 1976, 33, 766–771. [Google Scholar] [CrossRef]
- Haro, J.M.; Kamath, S.A.; Ochoa, S.; Novick, D.; Rele, K.; Fargas, A.; Rodríguez, M.J.; Rele, R.; Orta, J.; Kharbeng, A.; et al. The Clinical Global Impression—Schizophrenia scale: A simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatr. Scand. Suppl. 2003, 416, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Speak, B.L.; Hay, P.; Muncer, S.J. HoNOS—Their utility for payment by results in mental Health. Int. J. Health Care Qual. Assur. 2015, 28, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Orrell, M.; Yard, P.; Handysides, J.; Schapira, R. Validity and reliability of the Health of the Nation Outcome Scales in psychiatric patients in the community. Br. J. Psychiatry 1999, 174, 409–412. [Google Scholar] [CrossRef]
- Vázquez, F.L.; Torres, A.; Otero, P.; Blanco, V.; Attkisson, C.C. Psychometric properties of the Castilian Spanish Version of the Client Satisfaction Questionnaire (CSQ-8). Curr. Psychol. 2019, 38, 829–835. [Google Scholar] [CrossRef]
- Pedersen, H.; Havnen, A.; Brattmyr, M.; Attkisson, C.C.; Lara-Cabrera, M.L. A digital Norwegian version of the client satisfaction questionnaire. 8: Factor validity and internal reliability in outpatient mental health care. BMC Psychiatry 2022, 22, 671. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).