Support Needs for Anxiety among Pregnant Women in Japan: A Qualitative Pilot Study
Abstract
:1. Introduction
2. Results
2.1. Participants’ Characteristics
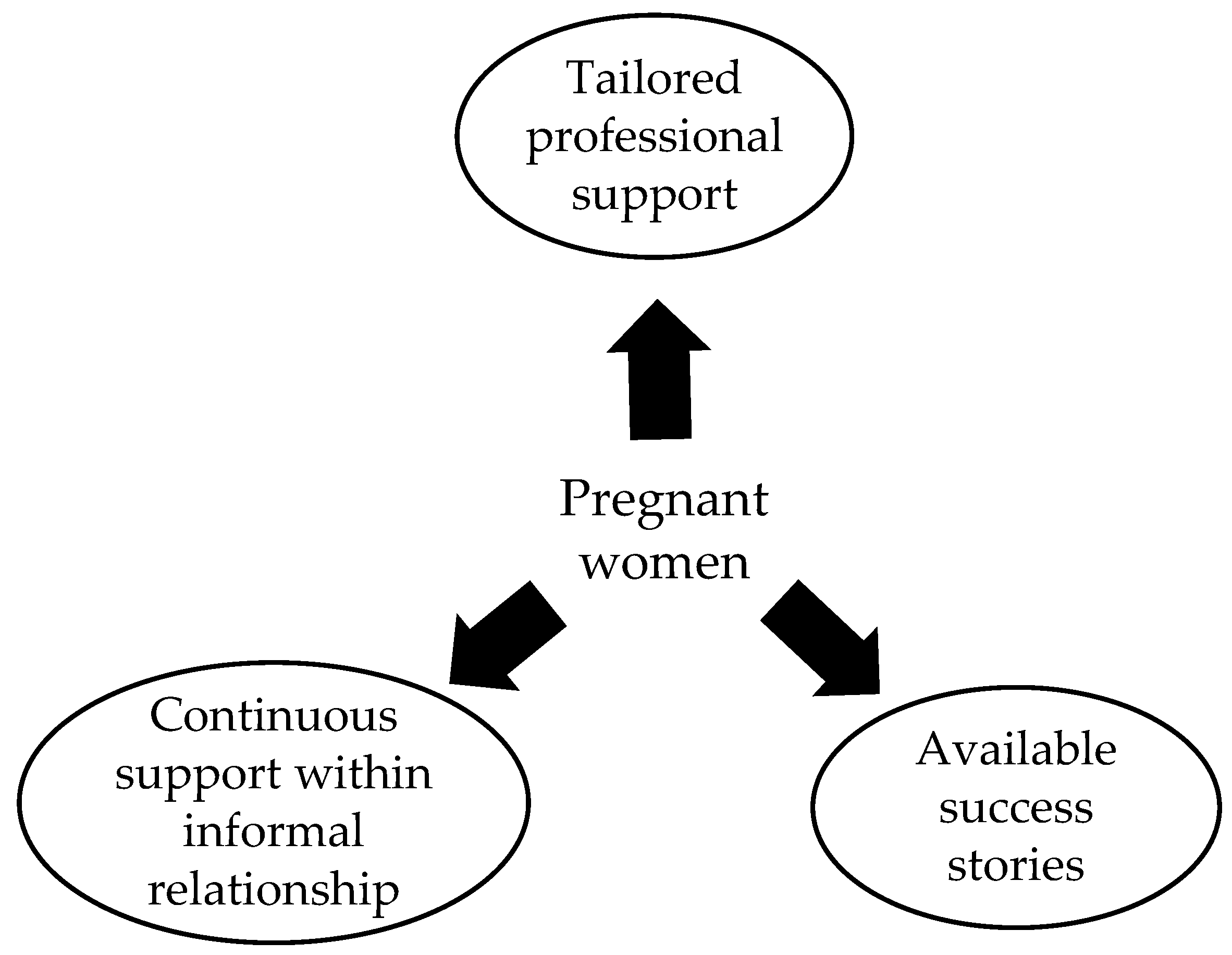
2.2. Support Needs
- Seeking tailored professional support;
- Seeking continuous support within informal relationships;
- Seeking others’ success stories in the same situation.
2.2.1. Theme 1: Seeking Tailored Professional Support
In fact, it’s like…when I gave birth, the people around me were…well…only the midwives and the doctors, so I felt very reassured, and the doctors and midwives who were there and kept calling out to me were of course much more powerful than the stories I had heard. That’s right. It was very reassuring. (Participant D)
I tried to talk to a nurse or a doctor at the hospital about such things [partner’s smoking], but all they said was that I should definitely stop him from smoking… (Participant E)
2.2.2. Theme 2: Seeking Continuous Support within Informal Relationships
I don’t have any friends who are pregnant or have children, so I don’t really have anyone to talk to about something…like events during pregnancy, I guess I’m a little nervous about it. (Participant B)
When I’m in the hospital, I feel a bit rushed and I don’t feel like I can take my time to talk to the doctor, so I tend to ask [another] mother who is ahead of me such things about the pain of childbirth and daily life after childbirth. (Participant C)
My number of gestational weeks is now 33, so I can’t run any more tests of a definitive diagnosis at this week, well, like NIPT (noninvasive prenatal genetic testing). I’ll tell you what…oh, I guess I should have taken it, although I can’t take it anymore, when I’ve heard that my friend who is also pregnant got it, I was a little worried that maybe I should have taken the test, well, I made my own decision, but I think I [will] have anxiety about whether my decision was right all the way until my baby is born. (Participant C)
My husband is a smoker, and we’ve talked about it, but the results haven’t been to my satisfaction… (Participant E)
2.2.3. Theme 3: Seeking Others’ Success Stories in the Same Situation
Well, I’m not sure if I can really take care of my children properly…of course my niece and nephew are cute but…yes, this is my first baby so I guess I’m a little nervous about having to raise my baby day in and day out by myself, so…although I think the only way to solve it is to have a baby and raise it, I’ve been looking at pictures of cute babies on the Internet, or been reading blogs, by those things I can think babies are pretty cute, and it’s kind of comforting. (Participant E)
(By reading information about non-evidence-based treatments on the Internet) Well, that’s the emotional part, the bleeding may not be treatable, but if I receive some kind of treatment, and it might be good for my baby…that would make me feel like I’m doing my best, it’s better than doing nothing…on the contrary, I was doing nothing and just waiting to see what happens…oh, well, I think I was more worried. (Participant B)
2.3. Proposed Model
When it comes to normal checkups, I don’t really have that much to talk about… In other words, I thought that it would be easier to ask someone closer to me. (Participant D)
At first, I was very shocked, it is my first pregnancy, and no way, I was told that there was a possibility of a miscarriage. After that, I talked to the doctor about various things, let me see, like how likely it was, I asked a lot of questions about such things, but I was said the doctor didn’t know…After I went home, I did a Google search and then it said that in my case, almost 100% my baby was going to be miscarried, so my shock got worse. (Participant B)
3. Materials and Methods
3.1. Participant Recruitment
3.2. Interview Procedure
3.3. Data Analysis
4. Discussion
4.1. Theoretical Implications
4.2. Practice Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Anxiety Codes | Supporting Quotes 1 |
|---|---|
| Anxiety from Pregnancy Itself | |
| From confirmation of pregnancy to feeling fetal movement | Before I felt…the fetal movement, I was very anxious if my baby would be okay after I lost my morning sickness and entered the stable period, conversely. (Participant D) |
| Prenatal testing | I made my own decision (not to take prenatal testing), but I think I [will] have anxiety about whether my decision was right all the way until my baby is born. (Participant C) |
| Childbirth | As for my next concern, it is the first time I have given birth, so I am starting to feel a little scared about…childbirth. (Participant A) |
| Lack of preparation for childbirth and postpartum | The new anxiety that emerged was, as (Ms. G.) said, about what preparations I should make, whether there is anything I am missing or not, what and what timing I should prepare for the birth…I was starting to feel anxious about the birth?…little by little…(Participant C) |
| Postpartum attachment formation | Well, I’m not sure if I can really take care of my children properly…of course my niece and nephew are cute but…yes, this is my first baby so I guess I’m a little nervous about having to raise my baby day in and day out by myself… (Participant E) |
| Personal characteristics | |
| After miscarriage experience | My first child is four years old now, well, I’m four years away (before this pregnancy) and I had three miscarriages during that time…well…I was not anxious at all when I had my first child, but now that I experienced those miscarriages…I am always wondering…if my baby will be really okay. (Participant D) |
| Whether the pregnancy after infertility treatment can continue | (Like Ms. A,) I too had gone through infertility treatment, and since I had already gone through the full course of treatment, I was finally able to conceive on my third IVF cycle, so to be honest, I was more worried about whether this pregnancy would actually be successful than I was worried about the corona (COVID-19) disaster… (Participant C) |
| Complications during pregnancy | At first, well, I was in great shock…it was my first pregnancy, and I was told that I might have a miscarriage, which I didn’t expect… (Participant B) |
| Environment surrounding individuals | |
| Facilities and medical staffs | I was a little young when I had my first miscarriage, and I felt like a tragic heroine when I had a miscarriage…the doctor’s response was not very good, and I blamed it on the doctor and became displeased with the clinic…I had such experience of being tossed around by the hospital…so I am wondering what kind of criteria people use to choose a clinic, not just the proximity to their homes. (Participant C) |
| Home environment | If I impose it (the smoking cessation) [on my husband], it will make my family unhappy, and so on… (Participant E) |
| Workplace | Well, I couldn’t tell people at work (about my pregnancy) because of that (anxiety about miscarriage), and I finally reported it…recently. (Participant D) |
| Outbreak of COVID-19 | Of course, the world is getting so bad right now with corona (COVID-19) infections and things like that, so I was afraid of that… (Participant B) |
References
- Hahn-Holbrook, J.; Cornwell-Hinrichs, T.; Anaya, I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-analysis, and Meta-Regression of 291 Studies from 56 Countries. Front. Psychiatry 2018, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.-L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Grigoriadis, S.; Graves, L.; Peer, M.; Mamisashvili, L.; Tomlinson, G.; Vigod, S.N.; Dennis, C.-L.; Steiner, M.; Brown, C.; Cheung, A.; et al. A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Arch. Women’s Ment. Health 2019, 22, 543–556. [Google Scholar] [CrossRef] [PubMed]
- Pregnancy Health Examination; No. 0227001; Notice by Director, Maternal and Child Health Division, Equal Employment and Child Family Bureau; Ministry of Health, Labor and Welfare: Tokyo, Japan, 27 February 2009.
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice Hall: Hoboken, NJ, USA, 1986. [Google Scholar]
- Chen, H.-H.; Hwang, F.-M.; Tai, C.-J.; Chien, L.-Y. The Interrelationships among Acculturation, Social Support, and Postpartum Depression Symptoms among Marriage-Based Immigrant Women in Taiwan: A Cohort Study. J. Immigr. Minor. Health 2013, 15, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Escribà-Agüir, V.; Royo-Marqués, M.; Artazcoz, L.; Romito, P.; Ruiz-Pérez, I. Longitudinal study of depression and health status in pregnant women: Incidence, course and predictive factors. Eur. Arch. Psychiatry Clin. Neurosci. 2013, 263, 143–151. [Google Scholar] [CrossRef]
- Kritsotakis, G.; Vassilaki, M.; Melaki, V.; Georgiou, V.; Philalithis, A.E.; Bitsios, P.; Kogevinas, M.; Chatzi, L.; Koutis, A. Social capital in pregnancy and postpartum depressive symptoms: A prospective mother–child cohort study (the Rhea study). Int. J. Nurs. Stud. 2013, 50, 63–72. [Google Scholar] [CrossRef]
- Leung, B.M.; Kaplan, B.J.; Field, C.J.; Tough, S.; Eliasziw, M.; Gomez, M.F.; McCargar, L.J.; Gagnon, L.; the APrON Study Team. Prenatal micronutrient supplementation and postpartum depressive symptoms in a pregnancy cohort. BMC Pregnancy Childbirth 2013, 13, 2. [Google Scholar] [CrossRef]
- Bedaso, A.; Adams, J.; Peng, W.; Sibbritt, D. The relationship between social support and mental health problems during pregnancy: A systematic review and meta-analysis. Reprod. Health 2021, 18, 162. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Fathi, F.; Mohammad-Alizadeh-Charandabi, S.; Mirghafourvand, M. Maternal self-efficacy, postpartum depression, and their relationship with functional status in Iranian mothers. Women Health 2018, 58, 188–203. [Google Scholar] [CrossRef]
- Mohammad, K.I.; Sabbah, H.; Aldalaykeh, M.; Albashtawy, M.; Abuobead, K.Z.; Creedy, D.; Gamble, J. Informative title: Effects of social support, parenting stress and self-efficacy on postpartum depression among adolescent mothers in Jordan. J. Clin. Nurs. 2021, 30, 3456–3465. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Zhang, J.; Yang, J.; Yang, X.; Bai, H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr. Dis. Treat. 2022, 18, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Gremigni, P.; Mariani, L.; Marracino, V.; Tranquilli, A.L.; Turi, A. Partner support and postpartum depressive symptoms. J. Psychosom. Obstet. Gynecol. 2011, 32, 135–140. [Google Scholar] [CrossRef]
- Downe, S.; Finlayson, K.; Tunçalp, Ö.; Gülmezoglu, A.M. What matters to women: A systematic scoping review to identify the processes and outcomes of antenatal care provision that are important to healthy pregnant women. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 529–539. [Google Scholar] [CrossRef]
- Riessman, C.K. Narrative Methods for the Human Sciences; Sage Publications: Thousands Oaks, CA, USA, 2008. [Google Scholar]
- Liamputtong, P. Qualitative Research Methods, 5th ed.; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Sofaer, S. Qualitative research methods. Int. J. Qual. Health Care 2002, 14, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, S.; Schumm, J.S.; Sinagub, J.M. Focus Group Interviews in Education and Psychology; Sage Publications: Thousands Oaks, CA, USA, 1996. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage Publications: Thousands Oaks, CA, USA, 1998. [Google Scholar]
- Bandura, A. Self-Efficacy: The Exercise of Control; W H Freeman & Co.: New York, NY, USA, 1999. [Google Scholar]
- Ashford, S.; Edmunds, J.; French, D. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br. J. Health Psychol. 2010, 15, 265–288. [Google Scholar] [CrossRef]
- Kelder, S.H.; Hoelscher, D.; Perry, C.L. How Individuals, Environments, and Health Behaviors Interact. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2015; pp. 159–182. [Google Scholar]
- Gagnon, A.J.; Sandall, J. Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Syst. Rev. 2007, 2007, CD002869. [Google Scholar] [CrossRef]
- Brugha, T.S.; Sharp, H.M.; Cooper, S.-A.; Weisender, C.; Britto, D.; Shinkwin, R.; Sherrif, T.; Kirwan, P.H. The Leicester 500 Project. Social support and the development of postnatal depressive symptoms, a prospective cohort survey. Psychol. Med. 1998, 28, 63–79. [Google Scholar] [CrossRef]
- Kenyon, S.; Jolly, K.; Hemming, K.; Hope, L.; Blissett, J.; Dann, S.-A.; Lilford, R.; MacArthur, C. Lay support for pregnant women with social risk: A randomised controlled trial. BMJ Open 2016, 6, e009203. [Google Scholar] [CrossRef]
- Yim, I.S.; Stapleton, L.R.T.; Guardino, C.M.; Hahn-Holbrook, J.; Schetter, C.D. Biological and Psychosocial Predictors of Postpartum Depression: Systematic Review and Call for Integration. Annu. Rev. Clin. Psychol. 2015, 11, 99–137. [Google Scholar] [CrossRef] [PubMed]
- Prescott, J.; Mackie, L. “You Sort of Go Down a Rabbit Hole…You’re Just Going to Keep on Searching”: A Qualitative Study of Searching Online for Pregnancy-Related Information During Pregnancy. J. Med. Internet Res. 2017, 19, e194. [Google Scholar] [CrossRef] [PubMed]
- Bjelke, M.; Martinsson, A.-K.; Lendahls, L.; Oscarsson, M. Using the Internet as a source of information during pregnancy—A descriptive cross-sectional study in Sweden. Midwifery 2016, 40, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Elder, N.; Miller, W.L. Reading and evaluating qualitative research studies. J. Fam. Pract. 1995, 41, 279–285. [Google Scholar]
| Participant | Age (Years) | GA (Weeks) | Facility | Number of Deliveries | Number of Abortions | IVF | Job | Education | Economic Comfort | Prenatal Class | Deliver at Same Facility | Risk |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 34 | 31 | Hospital | 0 | 0 | Yes | Full-time worker | University | Some | Yes | Yes | NA |
| B | 29 | 24 | University hospital | 0 | 0 | No | Full-time worker | University | Not much | No | Yes | Been abused |
| C | 33 | 33 | Clinic | 0 | 2 | Yes | Contract worker | University | Not much | Yes | No | Fibroid |
| D | 36 | 23 | Hospital | 1 | 3 | No | Full-time worker | University | Not much | No | Yes | NA |
| E | 27 | 31 | Clinic | 0 | 0 | No | Full-time worker | University | Not much | Yes | No | NA |
| Themes | Affect | Supporting Quotes 1 |
|---|---|---|
| Seeking tailored professional support | Positive | Well… the doctor at the clinic, and also the nurses and the receptionists, I like the way they behave towards myself, and I go to the checkups every time with a good feeling, well, I think I feel this way maybe because there is nothing wrong with my baby now, but I am very thankful that I can go to the checkups with a happy feeling. (Participant C) |
| Negative | Well, as it turned out, it was okay, but should I search on Google? I didn’t get much guidance on what and how much I should do in detail…so I was a bit confused. (Participant B) | |
| Seeking continuous support within informal relationships | Positive | Well, now that I’m on maternity leave, I have more time to spare, so I’ve been going to see my friends around me…well, just going to see friends like who have children or who have recently born babies, well…listening their opinions or…I wonder…just by talking with them, yes, I think I was able to relieve a lot of my worries. (Participant A) |
| Negative | Well…when I was pregnant with my first child, my husband always said something like that it would be fine if the baby was born healthy and without a physical defect, but that made me feel really anxious, and I thought “Please don’t say things like that anymore.” (Participant D) | |
| Seeking others’ success stories in the same situation | Positive | Let me see…I did a lot of research on the Internet in English and so on, to find people who experienced bleeding, and when…I read the stories of people who had done well, I was a little relieved… (Participant B) |
| Negative | There’s a lot of information on the Internet that says [your partner] should quit smoking, but if I force him to do so, it might cause discord in my family, that’s one of the things that happens…so, in that respect, I recently would like to know positive feedback like what measures are taken by those who have husbands who smoke, or how their children grew up well even though they could only get this level of cooperation. (Participant E) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shirabe, R.; Okuhara, T.; Okada, H.; Goto, E.; Kiuchi, T. Support Needs for Anxiety among Pregnant Women in Japan: A Qualitative Pilot Study. Women 2023, 3, 95-106. https://doi.org/10.3390/women3010008
Shirabe R, Okuhara T, Okada H, Goto E, Kiuchi T. Support Needs for Anxiety among Pregnant Women in Japan: A Qualitative Pilot Study. Women. 2023; 3(1):95-106. https://doi.org/10.3390/women3010008
Chicago/Turabian StyleShirabe, Ritsuko, Tsuyoshi Okuhara, Hiroko Okada, Eiko Goto, and Takahiro Kiuchi. 2023. "Support Needs for Anxiety among Pregnant Women in Japan: A Qualitative Pilot Study" Women 3, no. 1: 95-106. https://doi.org/10.3390/women3010008
APA StyleShirabe, R., Okuhara, T., Okada, H., Goto, E., & Kiuchi, T. (2023). Support Needs for Anxiety among Pregnant Women in Japan: A Qualitative Pilot Study. Women, 3(1), 95-106. https://doi.org/10.3390/women3010008







