Determinants of Depression, Anxiety, and Stress among Pregnant Women Attending Tertiary Hospitals in Urban Centers, Nigeria
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Data Collection Instruments and Procedures
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
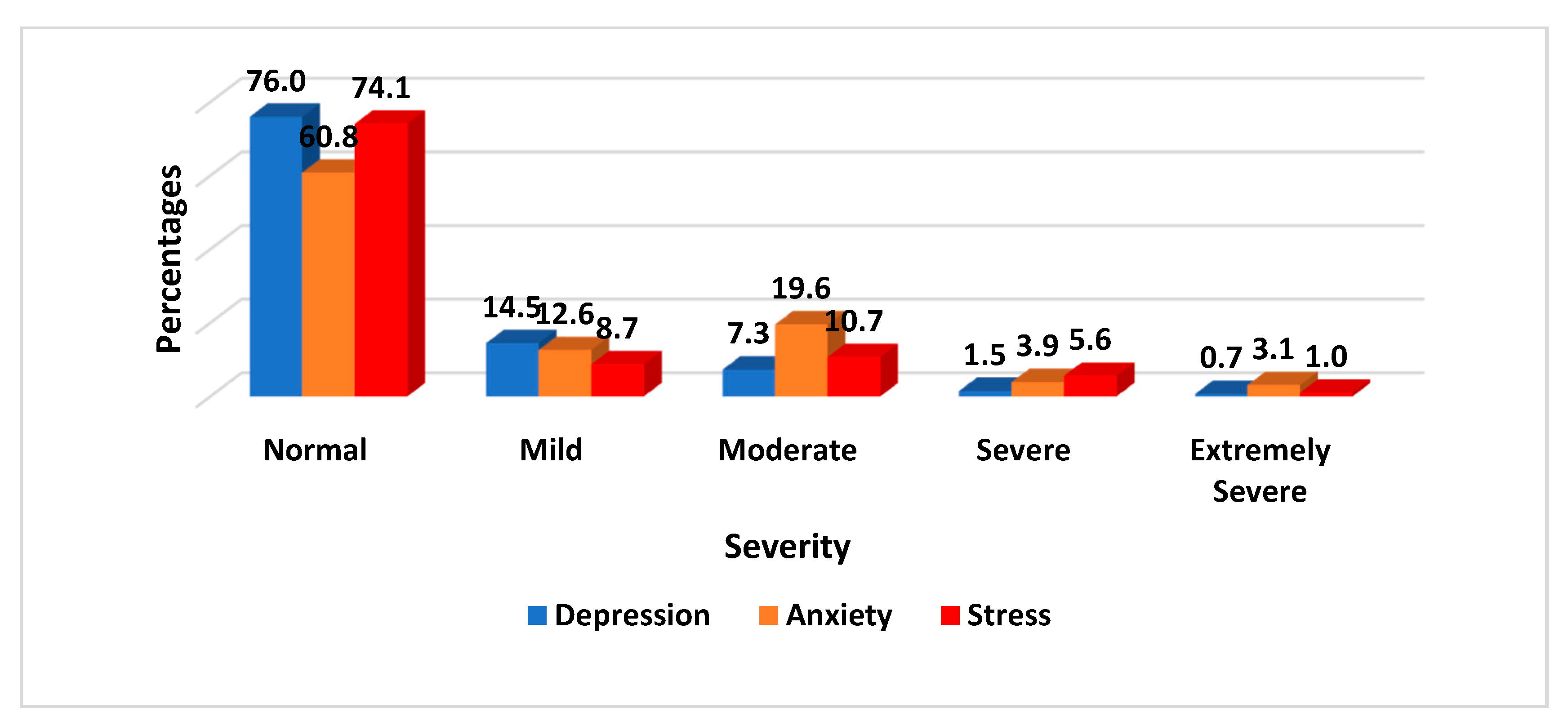
3.2. Severity of Depression, Anxiety, and Stress among Pregnant Women
3.3. Determinants of Depression, Anxiety, and Stress among Pregnant Women
4. Discussion
Study Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McMahon, C.A.; Boivin, J.; Gibson, F.L.; Hammarberg, K.; Wynter, K.; Fisher, J.R.W. Older maternal age, and major depressive episodes in the first two years after birth: Findings from the Parental Age and Transition to Parenthood Australia (PATPA) study. J. Afect. Disord. 2015, 175, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.V.; Shao, L.; Howell, H.; Lin, H.; Yonkers, K.A. Perinatal depression and birth outcomes in a healthy start project. Matern. Child Health J. 2011, 15, 401–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gadanya, M.A.; Abulfathi, A.A.; Ahmad, F.A. Anxiety and depression in pregnancy: Prevalence and associated risk factors among pregnant women attending antenatal clinic in Aminu Kano Teaching Hospital Kano, Nigeria. Ann. Afr. Med. Res. 2018, 1, 1–15. [Google Scholar] [CrossRef]
- Signal, T.L.; Paine, S.J.; Sweeney, B. The prevalence of symptoms of depression and anxiety, and the level of life stress and worry in New Zealand Māori and non-Māori women in late pregnancy. Aust. N. Z. J. Psychiatry 2017, 51, 168–176. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Mental Health Determinants and Populations. Department of mental Health and Substance Dependence. Maternal and Child Mental Health Program. 2016. Available online: http://www.who.int/mental_health/maternal-child/maternal_mental_health/en/ (accessed on 23 August 2022).
- Rallis, S.; Skouteris, H.; McCabe, M.; Milgrom, J. A prospective examination of depression, anxiety, and stress throughout pregnancy. Women Birth 2014, 27, e36–e42. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- The American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-V, 5th ed.; The American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Effati-Daryani, F.; Zarei, S.; Mohammadi, A.; Hemmati, E.; Yngyknd, S.G.; Mojgan Mirghafourvand, M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020, 8, 1–10. [Google Scholar] [CrossRef]
- Busari, A.O. Prevalence and associated factors of anxiety and depression among pregnant women attending antenatal care at state hospital Moniya, Ibadan, Oyo state, Nigeria. Gend. Behavour 2018, 16, 11938–11953. [Google Scholar]
- Grote, N.K.; Bridge, J.A.; Gavin, A.R.; Melville, J.L.; Iyengar, S.; Katon, W.J. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch. Gen. Psychiatry 2010, 67, 1012–1024. [Google Scholar] [CrossRef]
- Fisher, J.; Cabral de Mello, M.; Patel, V.; Rahman, A.; Tran, T.; Holton, S. prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012, 90, 139–149. [Google Scholar] [CrossRef]
- Abdelhai, R.; Mosleh, H. Screening for antepartum anxiety and depression and their association with domestic violence among Egyptian pregnant women. J. Egypt. Public Health Assoc. 2015, 90, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Assefa, G.W. Prevalence and factors associated with antenatal depression among women following antenatal care at Shashemane health facilities, South Ethiopia. Ann. Glob. Health 2015, 81, 90. [Google Scholar]
- Adewuya, A.O.; Ola, B.A.; Aloba, O.O.; Dada, A.O.; Fasoto, O.O. Prevalence and correlates of depression in late pregnancy among Nigerian women. Depress. Anxiety 2007, 24, 15–21. [Google Scholar] [CrossRef]
- Deecher, D.; Andree, T.H.; Sloan, D.; Schechter, L.E. From menarche to menopause: Exploring the underlying biology of depression in women experiencing hormonal changes. Psychoneuroendocrinology 2008, 33, 3–17. [Google Scholar] [CrossRef]
- Gelaye, B.; Rondon, M.; Araya, R. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiat. 2016, 10, 973–982. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5155709/pdf/nihms820433.pdf (accessed on 23 August 2022). [CrossRef] [PubMed] [Green Version]
- Dadi, A.F.; Akalu, T.Y.; Baraki, A.G.; Wolde, H.F. Epidemiology of postnatal depression and its associated factors in Africa: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0231940. [Google Scholar] [CrossRef] [PubMed]
- Umuziga, M.P.; Adejumo, O.; Hynie, M. A cross-sectional study of the prevalence and factors associated with symptoms of perinatal depression and anxiety in Rwanda. BMC Pregnancy Childbirth 2020, 20, 68. [Google Scholar] [CrossRef] [Green Version]
- Míguez, M.C.; Vázquez, M.B. Prevalence of depression during pregnancy in Spanish women: Trajectory and risk factors in each trimester. Int. J. Environ. Res. Public Health 2021, 18, 6789. [Google Scholar] [CrossRef]
- Bante, A.; Mersha, A.; Zerdo, Z.; Wassihun, B.; Yeheyis, T. Comorbid anxiety and depression: Prevalence and associated factors among pregnant women in Arba Minch zuria district, Gamo zone, southern Ethiopia. PLoS ONE 2021, 16, e0248331. [Google Scholar] [CrossRef] [PubMed]
- Roy-Byrne, P. Treatmentment-refractory anxiety; definition, risk factors, and treatment challenges. Dialogues Clin. Neurosci. 2015, 17, 1–16. [Google Scholar] [CrossRef]
- O‘Connor, T.G.; Heron, J.; Glover, V. Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 1470–1477. [Google Scholar] [CrossRef] [PubMed]
- Jonsdottir, S.S.; Thome, M.; Steingrimsdottir, T.; Lydsdottir, L.B.; Sigurdsson, J.F.; Olafsdottir, H.; Swahnberg, K. Partner relationship, social support and perinatal distress among pregnant Icelandic women. Women Birth 2017, 30, e46–e55. [Google Scholar] [CrossRef]
- Priya, A.; Chaturvedi, S.; Bhasin, S.K.; Bhatia, M.S.; Gita Radhakrishan, G. Depression, Anxiety and Stress among pregnant women: A community—Based study. Indian J. Psychiatry 2018, 60, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Fairbrother, N.; Janssen, P.; Antony, M.M.; Tucker, E.; Young, A.H. Perinatal anxiety disorder prevalence and incidence. J. Affect. Disord. 2016, 200, 148–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, Y.T.; Yao, Y.; Dou, J. Prevalence and risk factors of maternal anxiety in late pregnancy in China. Int. J. Environ. Res. Public Health 2016, 13, 468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Britton, J.R. Maternal anxiety: Course and antecedents during the early postpartum period. Depress. Anxiety 2008, 25, 793–800. [Google Scholar] [CrossRef]
- Nwafor, J.I.; Okedo-Alex, I.N.; Ikeotuonye, A.C. Prevalence and predictors of depression, anxiety, and stress symptoms among pregnant women during COVID-19-related lockdown in Abakaliki, Nigeria. Malawi Med. J. 2021, 33, 54–58. [Google Scholar]
- Keramat, A.; Malary, M.; Moosazadeh, M.; Bagherian, N.; Rajabi-Shakib, M.-R. Factors influencing stress, anxiety, and depression among Iranian pregnant women: The role of sexual distress and genital self-image. BMC Pregnancy Childbirth 2021, 21, 87. [Google Scholar] [CrossRef]
- Khouj, M.A.; Albasri, S.; Albishri, A.A.; Softa, S.M.; Almaslamani, A.S.; Ahmad, H.M. Prevalence of Stress, Anxiety, and Depression Among Pregnant Women in Jeddah. Cureus 2022, 14, 1–9. [Google Scholar] [CrossRef]
- Chorwe-Sungani, G.; Chipps, J. A cross-sectional study of depression among women attending antenatal clinics in Blantyre district. Malawi S. Afr. J. Psychiatry 2018, 24, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woldetensay, Y.K.; Belachew, T.; Biesalski, H.K.; Ghosh, S.; Lacruz, M.E.; Scherbaum, V. The role of nutrition, intimate partner violence and social support in prenatal depressive symptoms in rural Ethiopia: Community based birth cohort study 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Pregnancy Childbirth 2018, 18, 1–10. [Google Scholar]
- Baron, E.; Hanlon, C.; Mall, S.; Honikman, S.; Breuer, E.; Kathree, T. Mental health in primary care in five low- and middle-income countries: A situtational analysis. BMC Health Serv. Res. 2016, 16, 53. [Google Scholar] [CrossRef] [Green Version]
- Thompson, O.; Ajayi, I. Prevalence of antenatal depression and associated risk factors among pregnant women attending antenatal clinics in Abeokuta North Local Government Area Nigeria. Depress. Res. Treat. 2016, 2016, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Alqahtani, A.H.; Al-Khedair, K.; Al-Jeheiman, R.; Al-Turki, H.A.; Al-Qahtani, N.H. Anxiety and depression during pregnancy in women attending clinics in a University Hospital in Eastern province of Saudi Arabia: Prevalence and associated factors. Int. J. Womens Health 2018, 10, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Ramohlola, M. Prevalence and Factors Associated with Depression amongst Pregnant Women at Helene Franz Hospital of the Limpopo Province, South Africa. Available online: http://hdl.handle.net/10386/3612 (accessed on 24 August 2022).
- Shrestha, S.; Pun, K.D. Anxiety on primigravid women attending antenatal care: A hospital based cross-sectional study. Kathmandu Univ. Med. J. (KUMJ) 2018, 16, 23–27. [Google Scholar]
- Akinsulore, A.; Temidayo, A.M.; Oloniniyi, I.O.; Olalekan, B.O.; Yetunde, O.B. Pregnancy-related anxiety symptoms and associated factors amongst pregnant women attending a tertiary hospital in south-west Nigeria. S. Afr. J. Psychiatr. 2021, 27, 1616. [Google Scholar] [CrossRef]
- Zhang, Y.; Muyiduli, X.; Wang, S. Prevalence and relevant factors of anxiety and depression among pregnant women in a cohort study from south-east China. J. Reprod. Infant Psychol. 2018, 36, 519–529. [Google Scholar] [CrossRef]
- Figueiredo, B.; Conde, A. Anxiety and depression in women and men from early pregnancy to 3-months postpartum. Arch. Women’s Ment. Health 2011, 14, 247–255. [Google Scholar] [CrossRef]
- Çolak, S.; Gürlek, B.; Önal, Ö.; Yılmaz, B.; Hocaoglu, C. The level of depression, anxiety, and sleep quality in pregnancy during coronavirus disease 2019 pandemic. J. Obstet. Gynaecol. Res. 2021, 47, 2666–2676. [Google Scholar] [CrossRef]
- Tang, X.; Lu, Z.; Hu, D.; Zhong, X. Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J. Affect. Disord. 2019, 253, 292–302. [Google Scholar] [CrossRef]
- Lilliecreutz, C.; Larén, J.; Sydsjö, G.; Josefsson, A. Effect of maternal stress during pregnancy on the risk for preterm birth. BMC Pregnancy Childbirth 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.Y.; Qiu, T.; Huang, H.; Tian, F.Q.; Wu, H. Factors associated with anxiety symptoms of women in early pregnancy in Shenyang. J. Environ. Occupat. Med. 2019, 36, 63–67. [Google Scholar] [CrossRef]
- Răchită, A.I.C.; Strete, G.E.; Suciu, L.M.; Ghiga, D.V.; Sălcudean, A.; Mărginean, C. Psychological Stress Perceived by Pregnant Women in the Last Trimester of Pregnancy. Int. J. Environ. Res. Public Health 2022, 19, 8315. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.M.; Melville, J.L.; Guo, Y.; Fan, M.-Y.; Gavin, A. Psychosocial stress during pregnancy. Am. J. Obs. Gynecol. 2010, 202, 61.e1–61.e7. [Google Scholar] [CrossRef] [Green Version]
- Weng, S.C.; Huang, J.P.; Huang, Y.L.; Lee, T.S.; Chen, Y. Effects of tobacco exposure on perinatal suicidal ideation, depression, and anxiety. BMC Public Health 2016, 16, 623. [Google Scholar] [CrossRef]
- Glover, V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract. Res. Clin. Obs. Gynaecol. 2014, 28, 25–35. [Google Scholar] [CrossRef]
| Level | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0–9 | 0–7 | 0–14 |
| Mild | 10–13 | 8–9 | 15–18 |
| Moderate | 14–20 | 10–14 | 19–25 |
| Severe | 21–27 | 15–19 | 26–33 |
| Extremely Severe | 28+ | 20+ | 34+ |
| Characteristics | n (%) |
|---|---|
| Facility | |
| UPTH | 220 (53.3) |
| RSUTH | 193 (46.3) |
| Age (years) | |
| <25 | 65 (16.2) |
| 25–34 | 264 (65.7) |
| ≥35 | 73 (18.2) |
| Mean (SD) | 29.7 (5.6) |
| Marital Status | |
| Not Married | 43 (10.4) |
| Married | 370 (89.6) |
| Educational Level | |
| ≤Secondary | 137 (33.2) |
| >Secondary | 276 (66.8) |
| Employment Status | |
| Unemployed | 118 (28.9) |
| Employed | 291 (71.1) |
| Religion | |
| Christianity | 399 (96.6) |
| Islam | 14 (3.4) |
| Income (Dollars) per month | |
| <100 | 219 (58.4) |
| 100–200 | 75 (20.0) |
| >200 | 81 (21.6) |
| Gravidity | |
| First Timer | 196 (47.5) |
| 2–4 | 185 (44.8) |
| ≥5 | 32 (7.7) |
| Trimester | |
| First Trimester | 42 (10.4) |
| Second Trimester | 160 (39.5) |
| Third Trimester | 203 (50.1) |
| Previous Abortion/Miscarriage | |
| No | 310 (76.9) |
| Yes | 93 (23.1) |
| Variables | Severity of Depression | |||
|---|---|---|---|---|
| Normal | Mild | ≥Moderate | p-Value | |
| n (%) | n (%) | n (%) | ||
| Age (years) | 0.000 | |||
| <25 | 38 (58.5) | 10 (15.4) | 17 (26.2) | |
| 25–34 | 208 (78.8) | 40 (15.2) | 16 (6.1) | |
| ≥35 | 59 (80.8) | 9 (12.3) | 5 (6.8) | |
| Mean (SD) | ||||
| Marital Status | 0.000 | |||
| Not Married | 17 (39.5) | 9 (20.9) | 17 (39.5) | |
| Married | 297 (80.3) | 51 (13.8) | 22 (5.9) | |
| Educational Level | 0.002 | |||
| ≤Secondary | 92 (67.2) | 23 (16.8) | 22 (16.1) | |
| >Secondary | 222 (80.4) | 37 (13.4) | 17 (6.2) | |
| Employment Status | 0.016 | |||
| Unemployed | 83 (70.3) | 16 (13.6) | 19 (16.1) | |
| Employed | 228 (78.4) | 43 (14.8) | 20 (6.9) | |
| Religion | 0.186 | |||
| Christianity | 306 (76.7) | 57 (14.3) | 36 (9.0) | |
| Islam | 8 (57.1) | 3 (21.4) | 3 (21.4) | |
| Income (Dollars) per month | 0.722 | |||
| <100 | 171 (78.1) | 32 (14.6) | 16 (7.3) | |
| 100–200 | 61 (81.3) | 10 (13.3) | 4 (5.3) | |
| >200 | 61 (75.3) | 11 (13.6) | 9 (11.1) | |
| Gravidity | 0.197 | |||
| First Timer | 141 (71.9) | 35 (17.9) | 20 (10.2) | |
| 2–4 | 145 (78.4) | 24 (13.0) | 16 (8.6) | |
| ≥5 | 28 (87.5) | 1 (3.1) | 3 (9.4) | |
| Trimester | 0.912 | |||
| First Trimester | 30 (71.4) | 7 (16.7) | 5 (11.9) | |
| Second Trimester | 124 (77.5) | 20 (12.5) | 16 (10.0) | |
| Third Trimester | 157 (77.3) | 28 (13.8) | 18 (8.9) | |
| Previous Abortion/Miscarriage | 0.596 | |||
| No | 236 (76.1) | 46 (14.8) | 28 (9.0) | |
| Yes | 71 (76.3) | 11 (11.8) | 11 (11.8) | |
| Variables | Level of Anxiety | |||
|---|---|---|---|---|
| Normal | Mild | ≥Moderate | p-Value | |
| n (%) | n (%) | n (%) | ||
| Age (years) | 0.273 | |||
| <25 | 35 (53.8) | 9 (13.8) | 21 (32.3) | |
| 25–34 | 169 (64.0) | 28 (10.6) | 67 (25.4) | |
| ≥35 | 39 (53.4) | 13 (17.8) | 21 (28.8) | |
| Mean (SD) | ||||
| Marital Status | 0.001 | |||
| Not Married | 15 (34.9) | 9 (20.9) | 19 (44.2) | |
| Married | 236 (63.8) | 43 (11.6) | 91 (24.6) | |
| Educational Level | 0.127 | |||
| ≤Secondary | 74 (54.0) | 19 (13.9) | 44 (32.1) | |
| >Secondary | 177 (64.1) | 33 (12.0) | 66 (23.9) | |
| Employment Status | 0.139 | |||
| Unemployed | 63 (53.4) | 17 (14.4) | 38 (32.2) | |
| Employed | 186 (63.9) | 34 (11.7) | 71 (24.4) | |
| Religion | 0.032 | |||
| Christianity | 246 (61.7) | 51 (12.8) | 102 (25.6) | |
| Islam | 5 (35.7) | 1 (7.1) | 8 (57.1) | |
| Income (Dollars) per month | 0.973 | |||
| <100 | 136 (62.1) | 27 (12.3) | 56 (25.6) | |
| 100–200 | 48 (64.0) | 9 (12.0) | 18 (24.0) | |
| >200 | 50 (61.7) | 12 (14.8) | 19 (23.5) | |
| Gravidity | 0.725 | |||
| First Timer | 119 (60.7) | 28 (14.3) | 49 (25.0) | |
| 2–4 | 111 (60.0) | 11.9 | 52 (28.1) | |
| ≥5 | 21 (65.6) | 2 (6.3) | 9 (28.1) | |
| Trimester | 0.006 | |||
| First Trimester | 31 (73.8) | 3 (7.1) | 8 (19.0) | |
| Second Trimester | 109 (68.1) | 22 (13.8) | 29 (18.1) | |
| Third Trimester | 109 (53.7) | 26 (12.8) | 68 (33.5) | |
| Previous Abortion/Miscarriage | 0.107 | |||
| No | 189 (61.0) | 44 (14.2) | 77 (24.8) | |
| Yes | 55 (59.1) | 7 (7.5) | 31 (33.3) | |
| Variables | Level of Stress | |||
|---|---|---|---|---|
| Normal | Mild | ≥Moderate | p-Value | |
| n (%) | n (%) | n (%) | ||
| Age (years) | 0.001 | |||
| <25 | 36 (55.4) | 11 (16.9) | 18 (27.7) | |
| 25–34 | 211 (79.9) | 16 (6.1) | 37 (14.0) | |
| ≥35 | 49 (67.1) | 9 (12.3) | 15 (20.5) | |
| Mean (SD) | ||||
| Marital Status | 0.001 | |||
| Not Married | 22 (51.2) | 5 (11.6) | 16 (37.2) | |
| Married | 284 (76.8) | 31 (8.4) | 55 (14.9) | |
| Educational Level | 0.000 | |||
| ≤Secondary | 78 (56.9) | 19 (13.9) | 40 (29.2) | |
| >Secondary | 228 (82.6) | 17 (6.2) | 31 (11.2) | |
| Employment Status | 0.588 | |||
| Unemployed | 83 (70.3) | 12 (10.2) | 23 (19.5) | |
| Employed | 219 (75.3) | 24 (8.2) | 48 (16.5) | |
| Religion | 0.020 | |||
| Christianity | 299 (74.9) | 32 (8.0) | 68 (17.0) | |
| Islam | 7 (50.0) | 4 (28.6) | 3 (21.4) | |
| Income (Dollars) per month | 0.001 | |||
| <100 | 151 (68.9) | 22 (10.0) | 46 (21.0) | |
| 100–200 | 67 (89.3) | 3 (4.0) | 5 (6.7) | |
| >200 | 70 (86.4) | 4 (4.9) | 7 (8.6) | |
| Gravidity | 0.233 | |||
| First Timer | 139 (70.9) | 19 (9.7) | 38 (19.4) | |
| 2–4 | 142 (76.8) | 17 (9.2) | 26 (14.1) | |
| ≥5 | 25 (78.1) | 0 (0.0) | 7 (21.9) | |
| Trimester | 0.000 | |||
| First Trimester | 37 (88.1) | 1 (2.4) | 4 (9.5) | |
| Second Trimester | 137 (85.6) | 7 (4.4) | 16 (10.0) | |
| Third Trimester | 127 (62.6) | 25 (12.3) | 51 (25.1) | |
| Previous Abortion/Miscarriage | 0.045 | |||
| No | 228 (73.5) | 22 (7.1) | 60 (19.4) | |
| Yes | 69 (74.2) | 13 (14.0) | 11 (11.8) | |
| Variable | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
| POR (95% CI) | p-Value | POR (95% CI) | p-Value | POR (95% CI) | p-Value | |
| Age (years) | ||||||
| <25 | Ref | - | - | Ref | ||
| 25–34 | 0.60 (0.30–1.17) | 0.135 | - | - | 0.51 (0.23–1.10) | 0.085 |
| ≥35 | 0.54 (0.23–1.26) | 0.157 | - | - | 0.81 (0.32–2.01) | 0.646 |
| Marital Status | ||||||
| Not Married | Ref | Ref | Ref | |||
| Married | 0.20 (0.10–0.41) | 0.000 | 0.35 (0.19–0.64) | 0.001 | 0.35 (0.14–0.84) | 0.020 |
| Educational Level | ||||||
| ≤Secondary | Ref | Ref | ||||
| >Secondary | 0.68 (0.41–1.14) | 0.15 | - | - | 0.56 (0.31–0.93) | 0.054 |
| Employment Status | ||||||
| Unemployed | Ref | - | - | |||
| Employed | 0.95 (0.55–1.66) | - | - | - | - | |
| Religion | ||||||
| Christianity | - | - | Ref | Ref | ||
| Islam | - | - | 3.02 (1.01–9.04) | 0.048 | 1.38 (0.33–5.73) | 0.543 |
| Income (Dollars) per month | ||||||
| <100 | - | - | - | Ref | ||
| 100–200 | - | - | - | 0.40 (0.17–0.93) | 0.034 | |
| >200 | - | - | - | 0.41 (0.18–0.89) | 0.026 | |
| Trimester | ||||||
| First Trimester | - | - | Ref | Ref | ||
| Second Trimester | - | - | 1.31 (0.61–2.83) | 0.490 | 1.63 (0.49–5.44) | 0.428 |
| Third Trimester | - | - | 2.53 (1.20–5.33) | 0.015 | 5.46 (1.68–17.77) | 0.005 |
| Previous Abortion/Miscarriage | ||||||
| No | - | - | - | - | Ref | |
| Yes | - | - | - | - | 1.16 (0.62–2.16) | 0.636 |
| Overall p-value from Brant test (testing POM assumption) | 0.398 | 0.411 | 0.509 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wegbom, A.I.; Edet, C.K.; Ogba, A.A.; Osaro, B.O.; Harry, A.M.; Pepple, B.G.; Fagbamigbe, A.F. Determinants of Depression, Anxiety, and Stress among Pregnant Women Attending Tertiary Hospitals in Urban Centers, Nigeria. Women 2023, 3, 41-52. https://doi.org/10.3390/women3010003
Wegbom AI, Edet CK, Ogba AA, Osaro BO, Harry AM, Pepple BG, Fagbamigbe AF. Determinants of Depression, Anxiety, and Stress among Pregnant Women Attending Tertiary Hospitals in Urban Centers, Nigeria. Women. 2023; 3(1):41-52. https://doi.org/10.3390/women3010003
Chicago/Turabian StyleWegbom, Anthony Ike, Clement Kevin Edet, Amaka Azubuike Ogba, Benjamin Osarolaka Osaro, Agiriye M. Harry, Biteegeregha Godfrey Pepple, and Adeniyi Francis Fagbamigbe. 2023. "Determinants of Depression, Anxiety, and Stress among Pregnant Women Attending Tertiary Hospitals in Urban Centers, Nigeria" Women 3, no. 1: 41-52. https://doi.org/10.3390/women3010003
APA StyleWegbom, A. I., Edet, C. K., Ogba, A. A., Osaro, B. O., Harry, A. M., Pepple, B. G., & Fagbamigbe, A. F. (2023). Determinants of Depression, Anxiety, and Stress among Pregnant Women Attending Tertiary Hospitals in Urban Centers, Nigeria. Women, 3(1), 41-52. https://doi.org/10.3390/women3010003






