Abstract
Access to quality care before, during, and after childbirth remains an effective means of reducing maternal and neonatal mortality. Therefore, the study identified factors influencing the utilization of prenatal care services among women of childbearing age in South Africa. This is a retrospective study based on secondary data from the South African Demographic Health Survey (DHS) conducted from 1998 to 2016. In South Africa, 21.0% of mothers had used ANC services. Higher odds of seeking prenatal care were found in women aged 35 years and older (cOR = 1.26, 95% CI; 1.08–1.47, p = 0.003), married or cohabiting (cOR = 1.13, 95% CI; 1.004–1.27) observed, p = 0.043), higher level of education (tertiary education: cOR = 0.55, p = 0.001), female residents in urban areas (cOR = 1.35, 95% CI; 1.20–1.52, p = 0.001), higher wealth index (cOR = 1.32, 95% CI; 1.15–1.51, p = 0.001), employed (cOR = 1.48, 95% CI; 1.29–1.70, p = 0.001) and media exposure (cOR = 1.27, 95% CI; 1.12–1.44), p = 0.001). The findings of this study provide insight into the need to make maternal health services more accessible, more widely used, and of a higher quality. This requires effective strategic policies that promote patronage to reduce maternal mortality and improve newborn outcomes in South Africa.
1. Introduction
Antenatal care (ANC) is an important factor in reducing maternal morbidity and mortality in pregnant women and in achieving a positive pregnancy experience [1,2,3]. The essence of this care pathway is to make sure that the health of both the unborn child and the pregnant mother is safe by monitoring the progress of the pregnancy vis-a-vis expected indicators for a normal pregnancy. Access to ANC gives a pregnant woman the opportunity to benefit from care services including health promotion, screening and diagnosis, and disease prevention, required to maintain normalcy and for timely identification of abnormalities that can pose a risk to the life of her unborn child and herself. Unfortunately, many women in developing countries do not have access to such services [1,4].
According to the South African Demographic Health Survey [5], there are approximately 536 prenatal deaths per 100,000 in South Africa. It shows that for every 1000 live births, five (5) women died during pregnancy. A higher proportion of women in South Africa receive prenatal care, also known as antenatal care (ANC) from healthcare professionals; doctors (18%), nurses or midwives (70%). Only a small fraction (2%) are cared for by traditional birth attendants, while 10% receive no prenatal care [5]. The benefits of ANC cannot be overstated, particularly when it comes to reducing maternal and prenatal morbidity and mortality. Maternal morbidity refers to any health condition attributed to, or aggravated by, pregnancy and childbirth that negatively affects the woman’s well-being [6,7].
WHO recommendations prior to 2016 call for at least four ANC visits [8] where a pregnant woman receives focused ANC, if eligible. Currently, a pregnant woman needs at least eight visits [9] to receive any significant evidence-based interventions. The South African Department of Health has classified the appropriate ANC based on the WHO criteria above. If a pregnant woman made at least four and eight visits between April 2006 and April 2017, she was considered booked or received an appropriate ANC. A 2.4% increase in the percentage of South African women who participated in at least four ANC visits from 1998 to 2016 was documented by Global Health data [10,11].
During this period, South Africa recorded 150 maternal deaths per 100,000 live births in 1998 [12] and 119 deaths in 2017 [13]. Despite the observed improvement, the country is far below the required 70 deaths per 100,000 live births to meet the Sustainable Development Goals (SDG) 3.1 [14]. Moreover, the rate of skilled delivery use, a predictor of Maternal Mortality Rate (MMR) in the country increased from 84% in 1998 to 97% in 2016 [15]; although, Bobo et al. [16] reported a higher rate of 96.7 percent. When it comes to pregnant women’s health, adequate ANC services are essential.
It has been observed that increasing access to skilled attendants, which has a close link to ANC, emergency obstetric care, and family planning services can significantly reduce maternal mortality in low-income settings such as South Africa [17,18,19]. Despite the obvious importance of maternity care, including ANC, poor access to and utilization of such services remains an important determinant of maternal mortality and morbidity worldwide [11,17].
Previous research has shown a link between ANC utilization and accessibility, socio-demographic factors, knowledge, and the quality of care provided [20,21,22], but the extent to which these factors influence ANC utilization has not been adequately documented in the region of South Africa. Consequently, this study investigated the critical factors that influence the utilization of ANC and other maternal health services between the years 1998 and 2016 among women of reproductive age in South Africa. The insights provided by this study will further help to shape the strategic policy that South Africa will use to reduce the number of maternal deaths and improve neonatal outcomes.
2. Results
2.1. Characteristics of Maternal Household Factors of Women within Reproductive Age in South Africa
As shown in Table 1, of the 67,645 women included in the analysis, 77.5% were para 1–2, 12% were equally nulliparous, and para ≥3. Timing of ANC (in months) was more among those that have attended between 3–6 months (72.2%), followed by <3 months (17.4%). Almost three-quarters (72.2%) had their first ANC visit between 3–6 months of pregnancy, and slightly above one-sixth (17.4%) attended before three months. More participants resided in the urban area (56.6%), compared to rural (43.4%). The provinces with the most participants were Gauteng (23.5%), Kwazulu-Natal (19.7%), Limpopo (12.6%), and Eastern Cape (12.5%).

Table 1.
Characteristics of women within reproductive age in South Africa and factors influencing the use of antenatal care among them (n = 67,645).
2.2. Characteristics of Women within Reproductive Age in South Africa and Factors Influencing the Use of Antenatal Care among Them
The study analyzed the DHS data of 67,645 women, across South Africa. The majority of the participants (46.6%) were within the age 25–34; 30.9% were within 15–24 years; and 22.4% were 35 years and above. Almost half of the participants (49.8%) were married, and 50.2% were single. Those who have completed secondary education were more with 67.4%, followed by those who have completed primary education (18.5%). Black/African descent was the majority with 86.3%, followed by those of Colored descent (8.4%), White (3.3%), and Indian/Asian (1.9%). Among the women included in the analysis, 77.5% had 1 or 2 parities, 11.6% were nulliparous, and those with 3 or more parities were 11.5%. Almost three-quarters (72.2%) had their first ANC visit between 3 and 6 months of pregnancy while slightly above one-sixth (17.4%) attended before three months. More participants resided in the urban area (56.6%), compared to rural (43.4%) and the provinces with the most participants were Gauteng (23.5%), Kwazulu-Natal (19.7%), Limpopo (12.6%), and Eastern Cape (12.5%) as shown in Table 1.
As shown in Figure 1, the overall prevalence of Utilization of Antenatal care services among women of reproductive age in SA was 79%.
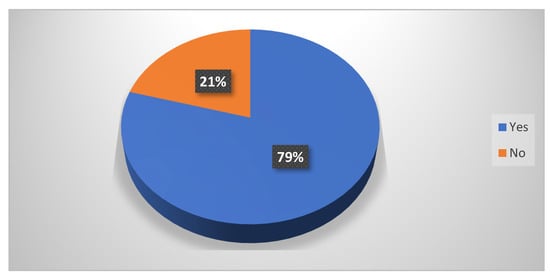
Figure 1.
Utilization of Antenatal care services among women of reproductive age in South Africa.
As shown in Figure 2, the prevalence of Utilization of Antenatal care services among women of reproductive age in SA was statistically significantly highest in the province of Western Cape (88.6%), followed by Kwazulu-Natal (82.8%), Northern Cape (81.6%) and Northwest (80.5%) (χ2=81.47, p = 0.001).
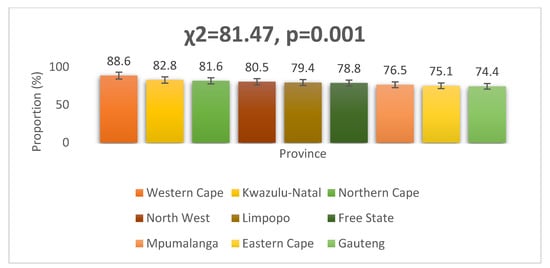
Figure 2.
Utilization of Antenatal care by women of reproductive age in SA stratified by province.
Women in the poverty band of the wealth index were the majority (41.3%), those in the middle wealth index were 22.8% and barely one-third belonged to the rich band (35.9%). The majority were not employed (69.4%), and 77.1% neither owned a car, a motorcycle/scooter (98.4%), nor a bicycle (85.8%). A little over half owned a refrigerator (58.93%), and most had electricity (71.6%). Barely two-thirds owned a television (68.89%), a radio (65.29%), watched TV every day/week (63.6%), and listened to the radio every day/week (61.4%) and 36.9% read newspapers regularly. The overwhelming majority of the women had no problem getting permission (86.9%) and money (72.2%) to visit the health facility for treatment; had no problem with the distance to the health facility (77.6%); and had no problem going to the health facility alone (88.0%), as seen in Table 1.
As shown in Figure 1, the overall prevalence of the Utilization of Antenatal care services among women of reproductive age in SA was 79%.
As shown in Figure 2, the prevalence of the Utilization of Antenatal care services among women of reproductive age in SA was statistically significantly highest in the province of Western Cape (88.6%), followed by Kwazulu-Natal (82.8%), Northern Cape (81.6%) and North West (80.5%) (χ2 = 81.47, p = 0.001).
As shown in Table 2, the utilization of antenatal care varied across socio-demographic variables. Statistically significant higher prevalence of utilization of antenatal care was observed among those between 25 and 34 years in age (p = 0.038); married or cohabiting (p = 0.001); had a tertiary level of education (p = 0.001), and of the Indian/Asian race (p = 0.001). For obstetric and household factors, a significantly higher prevalence of utilization of antenatal care was observed among para 1–2 (p = 0.001), attended antenatal <3 months (p = 0.001), reside in the urban (p = 0.004), and the Western Cape Province (p = 0.001). Considering economic status, utilization of antenatal care has statistical significance for those in the richest wealth index (p = 0.003), are employed (p = 0.001), own a car (p = 0.004), own a motorcycle/scooter (p = 0.001), own a bicycle (p = 0.032), own a refrigerator (p = 0.001) and have electricity (p = 0.001). Moreover, there was statistically significant higher prevalence of utilization of antenatal care among those who own a television (p = 0.001), own a radio (p = 0.001), watches television every day/week (p = 0.001), listens to the radio every day/week (p = 0.038) and reads newspaper regularly (p = 0.039) under the media exposure factor. However, no statistically significant association was observed between health institutional factors and the utilization of antenatal care (p > 0.05).

Table 2.
Associated factors for utilization of antenatal care services.
2.3. Multilevel Multivariate Logistic Regression Results
As shown in Table 3, statistically significant explanatory variables in the Chi-Square test of association were included for the multilevel multivariate logistic regression.

Table 3.
Multilevel Multivariable Logistic Regression Results for Factors Associated with the Utilization of Antenatal Care Services among Women of Reproductive Age in South Africa (n = 67,645).
Model I: Non-adjusted (crude) aggregate model comprising all explanatory variable categories associated with the utilization of Antenatal care services
2.3.1. Socio-Demographic Factors
The study shows higher odds for the utilization of antenatal care among women aged 35 years and older than those 15–24 years (cOR = 1.26, 95% CI; 1.08–1.47, p = 0.003). Moreover, being married or cohabiting had higher odds for utilizing antenatal care than singles (cOR = 1.13, 95% CI; 1.004–1.27, p = 0.043). The odds for the utilization of antenatal care among women improved from primary to tertiary compared to those with no education (primary: cOR = 0.38, secondary: cOR = 0.45 and tertiary: cOR = 0.55, p = 0.001). White or Indian/Asian descent showed lower odds for the utilization of antenatal care compared to black/African (White: cOR = 0.25, Indian/Asian: cOR = 0.35, p = 0.001).
2.3.2. Obstetric and Household Factors
Women with Para 1–2 and Para ≥3 showed increased odds for the utilization of antenatal care compared to those that are nulliparous, with an increased odds in Para ≥3 compared to Para 1–2 (Para 1–2: cOR = 1.33, Para ≥3: OR = 1.63, p < 0.05). Women with the timing of ANC at 3 or more months of pregnancy showed increased odds for the utilization of antenatal care compared to those with the timing of ANC less than 3 months (3–6 months: cOR = 41.91, 6+ months: OR = 9.73, p = 0.001). Women residing in the urban area showed increased odds for the utilization of antenatal care compared to those in the rural area (cOR = 1.35, 95% CI; 1.20–1.52, p = 0.001). Only those residing in Eastern Cape showed increased odds for the utilization of antenatal care compared to Western Cape (cOR = 1.54, 95% CI; 1.09–2.18, p = 0.014). The other provinces, Northern Cape (cOR = 0.56, p = 0.001), Mpumalanga (cOR = 0.63, p = 0.001), Limpopo (cOR = 0.70, 0.001) and Gauteng (cOR = 0.93, p = 0.001) showed lower odds for the utilization of antenatal care compared to Western Cape.
2.3.3. Economic Status Factors
The study shows higher odds for the utilization of antenatal care among women in the middle wealth index compared to those in the poorest/poorer wealth index (cOR = 1.32, 95% CI; 1.15–1.51, p = 0.001). Higher odds for the utilization of antenatal care were observed among women who are employed (cOR = 1.48, 95% CI; 1.29–1.70, p = 0.001), own a car (cOR = 1.44, 95% CI; 1.23–1.69, p = 0.001), own a Motorcycle/Scooter (cOR = 2.97, 95% CI; 1.37–6.44, p = 0.006), own a refrigerator (cOR = 1.58, 95% CI; 1.40–1.79, p = 0.001), and have electricity (cOR = 1.62, 95% CI; 1.43–1.84, p = 0.001).
2.3.4. Media Exposure Factors
Higher odds for the utilization of antenatal care was observed among women who own a television (cOR = 1.27, 95% CI; 1.12–1.44, p = 0.001), own a radio (cOR = 1.50, 95% CI; 1.33–1.69, p = 0.001), watch television everyday/week (cOR = 1.68, 95% CI; 1.49–1.89, p = 0.001), listen to radio every day or week (cOR = 1.21, 95% CI; 1.07–1.36, p = 0.002), and read newspaper regularly (cOR = 1.47, 95% CI; 1.29–1.68, p = 0.001).
2.4. Model II: Household Factors, Economic Factors, and Media Exposure Factors Associated with Utilization of Antenatal Care Services, While Controlling for Their Socio-Emographic/Individual Factors
2.4.1. Obstetric and Household Factor
Women with Para ≥3 showed increased odds for the utilization of antenatal care compared to those who are nulliparous after adjusting for socio-demographic characteristics (aOR = 1.29, 95% CI; 1.03–1.68, p = 0.029). Women with the timing of ANC 3 or more months showed reduced odds for the utilization of antenatal care compared to those with the timing of ANC less than 3 months (3–6 months: aOR = 0.029, 6+ months: aOR = 0.29, p = 0.001). Women residing in the urban still showed increased odds for the utilization of antenatal care compared to those in rural areas after adjusting for confounding variables (aOR = 1.24, 95% CI; 1.04–1.49, p = 0.016).
All provinces showed lower odds for the utilization of antenatal care compared to Western Cape (p < 0.05).
2.4.2. Economic Status Factors
After controlling for socio-demographic characteristics, the study showed no statistically significant association between wealth index and the utilization of antenatal care (p > 0.05). Higher odds for the utilization of antenatal care were now observed among women for only those who were employed (aOR = 1.27, 95% CI; 1.10–1.49, p = 0.001), own a refrigerator (aOR = 1.20, 95% CI; 1.01–1.41, p = 0.036) and have electricity (aOR = 1.27, 95% CI; 1.07–1.50, p = 0.006). The variables own a car or own a Motorcycle/Scooter were no longer statistically significant.
2.4.3. Media Exposure Factors
After controlling for socio-demographic characteristics, higher odds for the utilization of antenatal care were still observed among women who own a television (aOR = 1.16, 95% CI; 1.0–1.35, p = 0.049) and watch TV every day/week (aOR = 1.44, 95% CI; 1.21–1.72, p = 0.001). The variables own a radio, listen to the radio every day or week, and read the newspaper regularly were no longer statistically significant (p > 0.05).
2.5. Model III: Economic Factors and Media Exposure Factors Associated with Utilization of Antenatal Care Services, While Controlling for Obstetric and Household Factors
2.5.1. Economic Status Factors
After controlling for obstetric and household factors, the study showed a statistically significant association between the wealth index and the utilization of antenatal care. Higher odds for the utilization of antenatal care among women were observed in those in the middle wealth index (aOR = 1.21, 95% CI; 1.0–1.47, p = 0.047) and richer/richest wealth index (aOR = 1.23, 95% CI; 1.007–1.51, p = 0.043). Higher odds for the utilization of antenatal care were observed among employed women (aOR = 1.20, 95% CI; 1.004–1.44, p = 0.046), own a refrigerator (aOR = 1.20, 95% CI; 1.01–1.41, p = 0.036) and have electricity (aOR = 1.27, 95% CI; 1.07–1.50, p = 0.006). The variables own a car, own a Motorcycle/Scooter, own a refrigerator, and have electricity were no longer statistically significant (p > 0.05).
2.5.2. Media Exposure Factors
Only the variable, watches TV every day/week, was statistically significantly associated with the utilization of antenatal care. Those watching TV every day/week showed increased odds for the utilization of antenatal care services (aOR = 1.39, 95% CI; 1.12–1.73, p = 0.02).
2.6. Model IV: Media Exposure Factors Associated with Utilization of Antenatal Care Services, While Controlling for Economic Status Factors
Media Exposure Factors
After controlling for economic status factors, higher odds for the utilization of antenatal were was still observed among women who own a television (aOR = 1.18, 95% CI; 1.02–1.38, p = 0.030) and watch TV every day/week (aOR = 1.37, 95% CI; 1.15–1.62, p = 0.001). The variables, own a radio, listen to radio every day or week, and read the newspaper regularly, were no longer statistically significant (p > 0.05), similar to the findings when controlling for maternal household factors.
3. Discussion
Using nationally representative 1998 to 2016 SADHS data, the goal of this study was to assess factors associated with the utilization of ANC services in South Africa. The cluster sampling methodology used ensured sample representativeness and the reliability of the study results. The study included 67,645 mothers of child-bearing age in nine provinces of South Africa whose complete information was available in the survey. In South Africa, 21.0% of mothers had utilized ANC services. There were variations in all the provinces. The highest provinces with the most prevalence were Western Cape and KwaZulu-Natal. The lowest are Eastern Cape and Gauteng, which could be as a result of the demographic and socioeconomic factors associated with both provinces. According to the findings of this study, women in South Africa’s rural areas were less likely than women in the country’s urban areas to use ANC services. This could be due to the disparities in the availability and accessibility of healthcare facilities, and women’s awareness of ANC services in urban and rural areas. This finding was consistent with the findings of other studies conducted in Pakistan and Vietnam where ANC uptake was lower in rural areas [23,24]. This implies that more attention to health awareness, education, and promotion activities in rural areas is needed to improve ANC uptake. According to Rustagi et al. [25], the higher ANC coverage observed in the urban setting may likely be due to ANC accessibility at primary care facilities in these areas, highlighting the need for policy efforts to strengthen primary healthcare. ANC coverage has been found to be linked to primary healthcare availability in similar studies [26,27].
The present study observed a statistically significant relationship between a woman’s age and adequate antenatal care utilization. The older the woman (35 years and older), the more likely she will use antenatal care appropriately. This suggests that young women have less experience with pregnancy care than older women. This is similar to findings to research by Adedokun and Yaya [21], who analyzed information obtained from the Demographic and Health Surveys (DHS) carried out in 31 different countries and involving 235,207 women aged 15–49 years old who had given birth to children within 5 years of the surveys. Similar findings were obtained by Joshi et al. [28] in Nepal, Dairo and Owoyokun [29] in Nigeria, Denny et al. [30] in Indonesia, and Ebonwu et al. [31] in South Africa. This may be due to older women placing more value on ANC, as a lack of knowledge about the benefits of ANC or the pregnancy being unwanted, which are common among adolescents, leads to seeking ANC care less frequently among younger women (including teenagers). Another study in Nigeria discovered that being 35 or older consistently increased the odds of using ANC by more than 200 percent [32]. Therefore, it is imperative for the South African Government to formulate policies that will protect adolescent pregnant women and provide for a tailored ANC to ensure utilization and a favorable pregnancy outcome for them. However, studies investigating the association between a woman’s age and the use of ANC have not always reached consistent conclusions; as one study observed, the younger age utilization of ANC was found to be adequate because working women tend to postpone their first pregnancy and are more mature in terms of age during pregnancy than unemployed women [33].
The odds for the utilization of antenatal care among women improved from secondary to tertiary compared to those with no education. The findings indicated that women with higher levels of education have a greater likelihood of making appropriate use of antenatal care than women with lower levels of education. This suggests that a woman’s likelihood of utilizing antenatal care increases in proportion to the level of education she possesses, which is similar to findings from previous studies [21,34,35]. A plausible explanation is that education fosters better enlightenment on issues, particularly health-related issues. This finding corroborated a study that alluded to increased utilization of maternal healthcare and women’s empowerment through education, wealth, and decision making [36]. The girl child education policy needs to be strengthened, ensuring that no girl child is missed, thus improving their educational status and ANC utilization.
In addition, married or cohabiting had higher odds for utilizing antenatal care than singles. Rurangirwa et al. [33] in their study conducted in Rwanda, observed that the risk of poor utilization of ANC services was higher among single women. This may be due to the support that married and cohabitating women receive from their husbands or partners as a result of the ANC attendance sensitization campaign, which equally targets men and encourages them to follow their wife or partner to the clinic [37]. This is also consistent with the data from similar studies [38,39].
This study observed that women with a better economic status (wealth index) and who are employed had more antenatal care utilization than those with lower wealth indexes. Higher odds for the utilization of antenatal care among women were observed in those in the middle wealth index and richer/richest wealth index. When it comes to prenatal care, women from low-income families may not have the financial means to register at clinics or pay for their services. Studies conducted in Ethiopia and Gabon, and evidence from the Demographic Health Surveys data of 31 countries across sub-Saharan Africa corroborated this finding [21,40,41].
Women living in houses equipped with electricity were found to be utilizers of ANC services. It is possible that the presence of electricity in a household may be an indirect measure of accessibility to media services and may be a sign of a better or higher social class [23].
This study found that women exposed to mass media (own a television and watch TV every day/week, or listen to the radio) had a higher chance of ANC utilization than women who were not, as seen in some similar studies, with the propensity to enjoy essential obstetric care from skilled birth attendants [22,42,43]. This may be due to the fact that mass media can reach a large number of people at once, thereby increasing awareness of the benefits of maternal health services and influencing family behavior.
Limitations and Strengths of the Study
A limitation of this study is that the use of secondary data. One of the strengths of the study is that the DHIS survey is national data with geographical representation; hence, the study results are a true representation of the national data.
4. Materials and Methods
4.1. Research Design
This is a retrospective study based on secondary data obtained from the South African Demographic Health Survey (DHS), which was carried out between the years 1998 and 2016.
4.2. Population
Administratively, South Africa is divided into nine provinces. In 2020, the middle-year population estimated by Statistics South Africa was 59.62 million, of which approximately 51.1% are females. The infant mortality rate for 2020 was estimated at 23.6 per 1000 live births.
4.3. Sample Size and Sampling Frame
A curated and concatenated dataset on ANC utilization was obtained from demographic and health surveys conducted in South Africa from 1998 to 2016 The targeted study population was women of reproductive age (15–49 years).
The survey involved a two-stage cluster stratified sampling method. In the first stage, the country was divided into clusters, using the enumeration areas (EA); clusters for the study were selected using simple random sampling and the households within each cluster were line listed. Women between 15 and 49 years of age who were citizens or permanent residents were randomly selected from the listed households and enrolled in the study in the second stage [44].
4.4. Instruments
Data for the DHS were collected through interviewer-administered semi-structured validated questionnaires. Information obtained with this questionnaire includes socioeconomic characteristics, reproductive history, antenatal, delivery, post-natal care, and breastfeeding.
4.5. Validity and Reliability of the Data Collection Instrument
DHS questionnaire is a validated tool that has been used for many decades. The DHS survey data collection tool’s reliability has been tested and established through repeated use by DHS and other experienced research investigators [44].
4.6. Variables of Interest
The independent variables: These include, sociodemographic characteristics such as age, marital status, education, and race; household factors such as parity (zero, one and two, three or more), the timing of ANC, place of residence, and region; economic status factors such as wealth index, employment, own a car/truck, own a motorcycle/scooter, own a bicycle, own a refrigerator, and electricity; media exposure factors such as own a television, own a radio, watch television regularly, listen to the radio regularly and read newspapers regularly; institutional factors such as access to a health facility and distance to a health facility.
The dependent (outcome) variable: ANC utilization during the women’s pregnancy period was the outcome variable. This was categorized as ‘not utilized—women who did not attend ANC’, and ‘utilized’—women who utilized. ANC not utilized was defined by <4 clinic visits and ANC utilized by ≥4 clinic visits across the study years.
4.7. Data Analysis
The data were analyzed using the SPSS package for data analysis. Descriptive analyses such as count, frequencies, and percentages are presented using a frequency table and bar/pie charts where appropriate. Pearson chi-square test was used to establish relationships between the independent and outcome variables, using a statistical significance of p-value less than or equal to 0.05 (p ≤ 0.05).
Bivariate and multivariate logistic regression analyses were used to measure the associations between the independent and outcome variables.
The study further used a regression model expression to simulate a nested approach in which a non-adjusted aggregate model comprising all explanatory variable categories and utilization of Antenatal care services would be iterated to generate Model 1. Model 2 was simulated using obstetric and household factors; economic factors; and media exposure factors while controlling for their socio-demographic/individual factors. Simulation using economic factors and media exposure factors while controlling for household factors was for Model 3 and lastly, Model 4 was simulated using only media exposure factors and controlling for economic status factors. The primary benefit of the model selected is avoiding confounding effects by analyzing the association between all variables simultaneously. Confounding effects were tested in the four models among different factors. After defining the technique, the fundamental interpretation of the results was emphasized. A p-value set at 0.05 was considered statistically significant.
5. Conclusions
The study uncovered factors that influence women’s use of antenatal care in South Africa. Age, marital status, having a tertiary education, living in an urban area, and socioeconomic factors, such as being in the richest wealth index and employed, having electricity, and media exposure, all influenced antenatal care utilization. Antenatal care enables the early detection and treatment of diseases that may affect both the mother and the child. It also allows a pregnant woman to be cared for during prenatal, antenatal, childbirth, and post-natal periods, reducing the chances of complications leading to maternal and neonatal death. Introducing targeted health promotion and education programs in communities would empower young and illiterate rural women to use available ANC services more often during pregnancy. Strengthening antenatal care visits becomes critical to the government in promoting and improving the health of the mother and child. This will lead to improved maternal and neonatal outcomes and minimize rural–urban reproductive health indices in South Africa. Maternal health services need to be accessible, used more frequently, and of higher quality. In addition, strengthening girl child education is paramount, not only to improve women’s empowerment, but also to improve ANC utilization among those who are pregnant. Further, health promotion in the primary and secondary levels of education needs to be intensified to change the narrative of poor ANC utilization among these categories of people.
Author Contributions
Conceptualization, O.O. and P.Z.N.; methodology, O.O.; validation, O.O., K.E.O. and L.B.; formal analysis, O.O. and F.E.A.; resources, O.O.; writing—original draft preparation, O.O.; writing—review and editing, O.O. and K.E.O.; visualization, M.N.; F.L.M.H., T.R.A. and J.A.M.; Supervision, O.O.; funding acquisition, O.O. All authors have read and agreed to the published version of the manuscript.
Funding
Financial support for OO from the Fogarty International Center and National Institute of Mental Health, National Institutes of Health Award (D43 TW010543), National Research Foundation Grant (132385) to Incentive Funding for Rated Researchers (IPRR), and The APC was funded by the Walter Sisulu Seed Funding. The content is solely the responsibility of the authors and does not necessarily reflect the opinion(s) of the sponsors and affiliated institutions.
Institutional Review Board Statement
The DHS team ensured that ethical approvals were obtained from the national department’s health ethics committee before the surveys were conducted. Ethical approval was obtained from the WSU IRB (033/2021) before the secondary data were obtained from the DHS for retrospective analysis. Respondents in the DHS data were informed that participation in this study is voluntary and they were asked to sign a voluntary consent form prior to enrollment in the study. Confidentiality and privacy were respected.
Data Availability Statement
The datasets analyzed for this study are available at https://dhsprogram.com (accessed on 15 June 2021).
Conflicts of Interest
The authors declare no conflict of interest.
References and Note
- Konje, E.T.; Magoma, M.T.N.; Hatfield, J.; Kuhn, S.; Sauve, R.S.; Dewey, D.M. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Pregnancy Childbirth 2018, 18, 394. [Google Scholar] [CrossRef]
- Arunda, M.; Emmelin, A.; Asamoah, B.O. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: Analysis of national survey data. Glob. Health Action 2017, 10, 1328796. [Google Scholar] [CrossRef] [PubMed]
- Bolarinwa, O.A.; Sakyi, B.; Ahinkorah, B.O.; Ajayi, K.V.; Seidu, A.A.; Hagan, J.E., Jr.; Tessema, Z.T. Spatial patterns and multilevel analysis of factors associated with antenatal care visits in nigeria: Insight from the 2018 nigeria demographic health survey. Healthcare 2021, 9, 1389. [Google Scholar] [CrossRef] [PubMed]
- Mutowo, J.; Yazbek, M.; van der Wath, A.; Maree, C. Barriers to using antenatal care services in a rural district in Zimbabwe. Int. J. Afr. Nurs. Sci. 2021, 15, 100319. [Google Scholar] [CrossRef]
- NDoH SS, SAMRC I. South Africa Demographic and Health Survey 2016. Pretoria, South Africa, and Rockville, Maryland, USA: National Department of Health (NDoH). Statistics South Africa (Stats SA), South African Medical Research Council (SAMRC), ICF. 2019
- WHO. Maternal Health. World Health Organization. 2022, p. 1. Available online: https://www.who.int/health-topics/maternal-health#tab=tab_1 (accessed on 13 May 2022).
- Lange, I.L.; Gherissi, A.; Chou, D.; Say, L.; Filippi, V. What maternal morbidities are and what they mean for women: A thematic analysis of twenty years of qualitative research in low and lower-middle income countries. PLoS ONE 2019, 14, e0214199. [Google Scholar] [CrossRef]
- Fife, J.G. Antenatal Care. Br. Med. J. 1948, 2, 227. [Google Scholar] [CrossRef]
- World Health Organization. WHO recommendations on antenatal Care for a Positive Pregnancy Experience. World Heal Organ. 2018, pp. 1–172. Available online: https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1 (accessed on 13 May 2022).
- WHO. Global Health Observatory Data Repository: Antenatal Care Coverage Data by Country. World Health Organization. 2021, p. 1. Available online: https://apps.who.int/gho/data/view.main.ANTENATALCARECOVERAGE4v (accessed on 13 May 2022).
- Olaitan, T.; Okafor, I.P.; Onajole, A.T.; Abosede, O.A. Ending preventable maternal and child deaths in western Nigeria: Do women utilize the life lines? PLoS ONE 2017, 12, e0176195. [Google Scholar] [CrossRef]
- Odhiambo, A. “Stop Making Excuses”: Accountability for Maternal Health Care in South Africa. Human Rights Watch, 8 August 2011. [Google Scholar]
- World Health Organization. Trends in Maternal Mortality: 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Beitzel, M. Sustainable Development Goal# 3 Good Health and Well-Being: Maternal and Child Health. Available online: https://summit.plymouth.edu/handle/20.500.12774/168 (accessed on 25 August 2022).
- SSA Statistics South Africa. Maternal Health Indicators: Further Analysis of the 1998 and 2016 South Africa Demographic and Health Surveys; Statistics South Africa: Pretoria, South Africa, 2020. [Google Scholar]
- Bobo, F.T.; Asante, A.; Woldie, M.; Dawson, A.; Hayen, A. Spatial patterns and inequalities in skilled birth attendance and caesarean delivery in sub-Saharan Africa. BMJ Glob. Health 2021, 6, e007074. [Google Scholar] [CrossRef]
- Nuamah, G.B.; Agyei-Baffour, P.; Mensah, K.A.; Boateng, D.; Quansah, D.Y.; Dobin, D.; Addai-Donkor, K. Access and utilization of maternal healthcare in a rural district in the forest belt of Ghana. BMC Pregnancy Childbirth 2019, 19, 6. [Google Scholar] [CrossRef]
- Geleto, A.; Chojenta, C.; Musa, A.; Loxton, D. Barriers to access and utilization of emergency obstetric care at health facilities in sub-Saharan Africa: A systematic review of literature 11 Medical and Health Sciences 1117 Public Health and Health Services. Syst. Rev. 2018, 7, 183. [Google Scholar] [CrossRef] [PubMed]
- Wabiri, N.; Chersich, M.; Shisana, O.; Blaauw, D.; Rees, H.; Dwane, N. Growing inequities in maternal health in South Africa: A comparison of serial national household surveys. BMC Pregnancy Childbirth 2016, 16, 256. [Google Scholar] [CrossRef] [PubMed]
- Morón-Duarte, L.S.; Varela, A.R.; Bertoldi, A.D.; Domingues, M.R.; Wehrmeister, F.C.; Silveira, M.F. Quality of antenatal care and its sociodemographic determinants: Results of the 2015 Pelotas birth cohort, Brazil. BMC Health Serv. Res. 2021, 21, 1070. [Google Scholar] [CrossRef] [PubMed]
- Adedokun, S.T.; Yaya, S. Correlates of antenatal care utilization among women of reproductive age in sub-Saharan Africa: Evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Arch. Public Health 2020, 78, 134. [Google Scholar] [CrossRef]
- Okedo-Alex, I.N.; Akamike, I.C.; Ezeanosike, O.B.; Uneke, C.J. Determinants of antenatal care utilisation in sub-Saharan Africa: A systematic review. BMJ Open 2019, 9, e031890. [Google Scholar] [CrossRef]
- Aziz Ali, S.; Aziz Ali, S.; Feroz, A.; Saleem, S.; Fatmai, Z.; Kadir, M.M. Factors affecting the utilization of antenatal care among married women of reproductive age in the rural Thatta, Pakistan: Findings from a community-based case-control study. BMC Pregnancy Childbirth 2020, 20, 355. [Google Scholar] [CrossRef]
- Tran, T.K.; Nguyen, C.T.; Nguyen, H.D.; Eriksson, B.; Bondjers, G.; Gottvall, K.; Ascher, H.; Petzold, M. Urban-Rural disparities in antenatal care utilization: A study of two cohorts of pregnant women in Vietnam. BMC Health Serv. Res. 2011, 11, 120. [Google Scholar] [CrossRef] [PubMed]
- Rustagi, R.; Basu, S.; Garg, S.; Singh, M.M.; Mala, Y.M. Utilization of antenatal care services and its sociodemographic correlates in urban and rural areas in Delhi, India. Eur. J. Midwifery 2021, 5, 40. [Google Scholar] [CrossRef]
- Venkateswaran, M.; Bogale, B.; Abu Khader, K.; Awwad, T.; Friberg, I.K.; Ghanem, B.; Hijaz, T.; Mørkrid, K.; Frøen, J.F. Effective coverage of essential antenatal care interventions: A cross-sectional study of public primary healthcare clinics in the West Bank. PLoS ONE 2019, 14, e0212635. [Google Scholar] [CrossRef]
- Ogbo, F.A.; Dhami, M.V.; Ude, E.M.; Senanayake, P.; Osuagwu, U.L.; Awosemo, A.O.; Ogeleka, P.; Akombi, B.J.; Ezeh, O.K.; Agho, K.E. Enablers and barriers to the utilization of antenatal care services in India. Int. J. Environ. Res. Public Health 2019, 16, 3152. [Google Scholar] [CrossRef]
- Joshi, C.; Torvaldsen, S.; Hodgson, R.; Hayen, A. Factors associated with the use and quality of antenatal care in Nepal: A population-based study using the demographic and health survey data. BMC Pregnancy Childbirth 2014, 14, 94. [Google Scholar] [CrossRef] [PubMed]
- Dairo, M.D.; Owoyokun, K. Factors affecting the utilization of antenatal care services in Ibadan, Nigeria. Benin J. Postgrad. Med. 2011, 12, 1–11. [Google Scholar] [CrossRef]
- Denny, H.M.; Laksono, A.D.; Matahari, R.; Kurniawan, B. The Determinants of Four or More Antenatal Care Visits Among Working Women in Indonesia. Asia Pac. J. Public Health 2022, 34, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Ebonwu, J.; Mumbauer, A.; Uys, M.; Wainberg, M.L.; Medina-Marino, A. Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa: A cross-sectional study. PLoS ONE 2018, 13, e0191903. [Google Scholar] [CrossRef]
- Dahiru, T.; Oche, O.M. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr. Med. J. 2015, 21, 1–17. [Google Scholar] [CrossRef]
- Rurangirwa, A.A.; Mogren, I.; Nyirazinyoye, L.; Ntaganira, J.; Krantz, G. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregnancy Childbirth 2017, 17, 142. [Google Scholar] [CrossRef]
- Basha, G.W. Factors Affecting the Utilization of a Minimum of Four Antenatal Care Services in Ethiopia. Obstet. Gynecol. Int. 2019, 2019, 5036783. [Google Scholar] [CrossRef]
- Tessema, Z.T.; Teshale, A.B.; Tesema, G.A.; Tamirat, K.S. Determinants of completing recommended antenatal care utilization in sub-Saharan from 2006 to 2018: Evidence from 36 countries using Demographic and Health Surveys. BMC Pregnancy Childbirth 2021, 21, 192. [Google Scholar] [CrossRef]
- Chopra, I.; Juneja, S.K.; Sharma, S. Effect of maternal education on antenatal care utilization, maternal and perinatal outcome in a tertiary care hospital. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 8, 247. [Google Scholar] [CrossRef]
- Teklesilasie, W.; Deressa, W. Husbands’ involvement in antenatal care and its association with women’s utilization of skilled birth attendants in Sidama zone, Ethiopia: A prospective cohort study. BMC Pregnancy Childbirth 2018, 18, 315. [Google Scholar] [CrossRef] [PubMed]
- Alenoghena, I.O.; Isah, E.C.; Isara, A.R. Maternal health services uptake and its determinants in public primary health care facilities in edo state, Nigeria. Niger. Postgrad. Med. J. 2015, 22, 25–31. [Google Scholar] [PubMed]
- Maduka, O.; Ogu, R. Non-Utilization of antenatal care services among women of reproductive age in the Niger delta region of Nigeria: Findings from 2595 women. Clin. Obstet. Gynecol. Reprod. Med. 2018, 4, 1–5. [Google Scholar] [CrossRef]
- Yaya, S.; Bishwajit, G.; Ekholuenetale, M.; Shah, V.; Kadio, B.; Udenigwe, O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS ONE 2017, 12, e0184934. [Google Scholar] [CrossRef] [PubMed]
- Sanogo, N.A.; Yaya, S. Wealth Status, Health Insurance, and Maternal Health Care Utilization in Africa: Evidence from Gabon. BioMed Res. Int. 2020, 2020, 4036830. [Google Scholar] [CrossRef] [PubMed]
- Acharya, D.; Khanal, V.; Singh, J.K.; Adhikari, M.; Gautam, S. Impact of mass media on the utilization of antenatal care services among women of rural community in Nepal. BMC Res. Notes 2015, 8, 345. [Google Scholar] [CrossRef]
- Fatema, K.; Lariscy, J.T. Mass media exposure and maternal healthcare utilization in South Asia. SSM-Popul. Health 2020, 11, 100614. [Google Scholar] [CrossRef]
- Login, S. The DHS Program. DHS 2016:1–2. Available online: https://dhsprogram.com/What-We-Do/Survey-Types/DHS-Questionnaires.cfm (accessed on 25 August 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).