Abstract
Contraceptive use is deemed one of the 10 greatest public health achievements of the 20th century because its benefits are universally acknowledged as a cornerstone for reducing global maternal morbidity and mortality. However, although the adoption of the Affordable Care Act in the United States (US) enhanced access to preventive health services, as well as increased contraceptive use, a considerable proportion of reproductive-aged women still have unmet reproductive health needs. Current data indicates gaps in contraceptive use patterns in the US, particularly among low-income women and those from racial/ethnic and gender minority subgroups, necessitating further investigation using an ecological approach. This narrative literature review aims to investigate the current perspective of contraceptive use in the US using the social-ecological model (SEM). Based on SEM levels, barriers to contraceptive use entail the following levels: individual (e.g., misbelief about the side effects of contraceptives), interpersonal (e.g., influence of family and friends), institutional (e.g., lack of training on how to use different types of contraceptives), community (e.g., societal stigma and shame), and policy (e.g., restrictive federal and states policies). Access to contraceptives for women is a system-level issue that necessitates consideration for multilevel strategies by key stakeholders to improve contraceptive uptake among vulnerable populations.
1. Introduction
Contraceptive use is deemed one of the 10 greatest public health achievements of the 20th century by the United States (US) Centers for Disease Control and Prevention [1]. This is because its benefits are universally acknowledged as a cornerstone for reducing global maternal morbidity and mortality, improving knowledge about health benefits of pregnancy spacing for maternal and child outcomes, mitigating unintended pregnancy, preventing risky sexual behaviors, and reducing the risk of contracting sexually transmitted infections. Contraceptive use also encourages workforce participation and economic and social self-sufficiency for women [2].
Contraception is a vital dimension of women’s health. Decisions regarding contraceptives have important implications on human rights, including a woman’s right to life and liberty, freedom of opinion and expression, right to work and education, and other benefits [3]. To fulfill these rights, women must have full access to their contraceptive choices. Because women spend most of their adult lives trying to prevent pregnancy, protecting their reproductive healthcare rights must be upheld. For example, in the US, women spend almost three decades of their life trying to avoid becoming pregnant, in contrast to only about 3 years of their adult life trying to be pregnant, being pregnant, or postpartum [4]. Thus, access to contraceptive methods is integral in a woman’s life.
The prevalence of using at least one form of contraception method has remained steady in the US. National survey data reveal that between 2008 to 2016, about 60–62% of reproductive age women (15–44) used one method of contraception. However, recent reports indicate a slight increase of 65.3% between 2017 to 2019 [5,6,7,8]. While the increase seems promising, disparities exist in contraceptive use, type, and access across socioeconomic strata.
From 2017 to 2019, the most common form of contraception among reproductive-aged women was female sterilization (18.1%), oral contraceptive pills (14.0%), long-acting reversible contraceptives (LARCs) (10.4%), and male condoms (8.4%). Contraceptive use varies by age and socioeconomic status [7]. For example, while LARC use is higher among women aged 20–29 (13.7%) and 30–39 (12.7%), those between 15–19 (5.8%) and 40–49 (6.6%) were least likely to use LARCs [7]. In addition, teenagers tend to favor short-acting reversible contraception over LARCs. Data indicate that roughly 75% of sexually experienced teenage females have used the male condom at least once, 60% have used the withdrawal method, followed by the pill (56%) [9]. Simultaneously, current condom use was greatest among non-Hispanic Black women (11.0%) and Hispanic women (10.5%) compared to their White counterparts (7.0%) [7]. Additionally, being a college graduate increases the use of LARCs such as intrauterine devices [5].
Although the adoption of the Affordable Care Act (ACA) increased access to preventive health services, including pills, IUDs, and female sterilization, which has increased contraceptive use in the US, the percentage of reproductive-aged women in need of contraceptive services has increased, suggesting unmet reproductive healthcare needs [10,11]. In 2014 alone, more than 38.3 million (representing a 10% increase between 2000 and 2010) needed contraceptive services and supplies [11]. In addition, in 2014, the need for contraceptive use was more prevalent among poor women with family income under 100% of the federal poverty line (11%), low-income women with family income between 100% and 250% of the federal poverty line (7%), being Hispanic (8%), and non-Hispanic Black (4%) women. Interestingly, the need for contraceptive services decreased for non-Hispanic White women (1%) [11]. Overall, however, over 14% of women were uninsured in 2014. Without adequate insurance coverage and access, women lose their ability to prevent unintended pregnancy through contraceptive use and, thereby, reduce abortion rates.
Moreover, unintended pregnancy and abortion rates are higher in the US than in most developed nations. More so, the burden of these conditions disproportionately affects low-income women [12,13]. Without a doubt, publicly funded family planning services are the lifeline for optimal reproductive health outcomes. For example, in 2014, the proportions of unintended pregnancy, resulting births, and abortions would have been 68% higher without publicly funded family planning services [11]. Taken together, the data indicate gaps in contraceptive use patterns in the US, necessitating further investigation using an ecological approach.
Therefore, this narrative literature review aims to investigate the current perspective of contraceptive use in the US using the social-ecological model (SEM). Articles were extracted unsystematically from PubMed and Google Scholar using key terms specific to each section. Notably, we used the “OR” and “AND” Boolean combinations iteratively to search for relevant articles published between 2010 and 2021. Keywords used central to each section included but were not limited to “sexual health,” “reproductive health,” “contracept,” “barriers,” and “facilitators.”
Rationale for Using the Social-Ecological Model
The social-ecological model (SEM) of health promotion by McLeroy and colleagues states that health behavior and promotion are interrelated and occur around multiple levels in the individual, interpersonal, institutional, community, and policy levels [14]. SEM has been used across various health topics to identify, understand, and explain complex health issues and patterns [15,16]. This multifaceted perspective is important to understand and explicate factors that influence women’s contraceptive use (see Figure 1). Using the SEM will help identify leverage areas for targeted public health efforts to increase and sustain contraceptive use, particularly among low-income women.
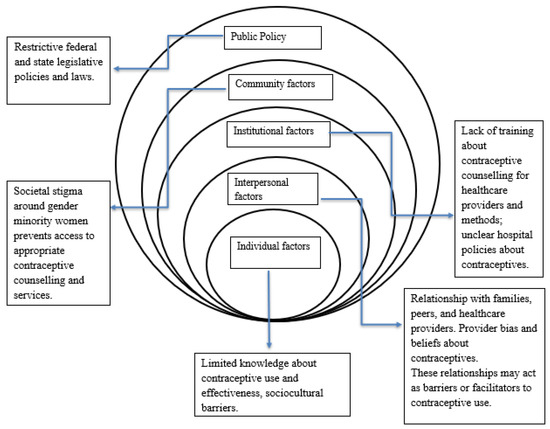
Figure 1.
Conceptual framework showing the factors that influence contraceptive use in the United States.
2. Literature Review
Contraception Mechanisms
There are several contraceptive methods with varying degrees of effectiveness in preventing pregnancy. These methods are broadly categorized as female and male sterilization, LARC methods, short-acting hormonal methods, barrier methods, and natural rhythm methods. Contraceptive efficacy relates to the correct use and consistency of using a particular type of contraceptive. The World Health Organization measures contraceptive methods effectiveness by the number of pregnancies per 100 women using the method per year [3]. However, the effectiveness differs by type of contraceptive. Table 1 below shows the global estimates of contraceptive methods and their effectiveness.

Table 1.
Global estimates of contraceptive mechanisms and effectiveness.
3. Barriers to Contraceptive Use
3.1. Individual-Level Factors
These factors are situated within the intrapersonal dimensions. Lack of knowledge, misaligned concerns, religious beliefs, and misconceptions about contraceptive safety and effectiveness are major barriers to the under-utilization or ineffectiveness of contraceptives [17,18,19]. The focus of abstinence-only education plays a role in the poor knowledge and misconception of contraceptive methods, effectiveness, and safety. In addition, it is possible that having a positive perception about contraceptives can improve understanding of and awareness of contraceptives. There are also myths surrounding the health consequences or side effects of contraceptives. For example, many women believe that IUDs or LARCs increase the risk of infection [18]. In addition to these issues, low-income women, particularly those with no or inconsistent health insurance coverage, may still experience financial burdens when removing IUDs or implants. This is because hospitals bill the removal of IUDs or implants separately from their placement despite the ACA’s provision [20].
3.2. Interpersonal-Level Factors
Interpersonal level factors refer to interactions with others in formal and informal social network and social support systems. Contraceptive use is influenced by the patient’s interaction with their healthcare providers. However, provider bias determines which method of contraceptives they discuss, particularly among younger females. For example, one study found that up to 50% of pediatricians prefer an abstinence-only form of contraception for adolescents, with fewer than 20% discussing any type of IUD [21]. Moreover, the propensity of discussing IUD is higher among female and younger pediatricians [21,22]. In addition, family and friends’ perspectives of contraception may influence contraceptive selection and continuation. A recent review of the impact of social networks on contraceptive use found that families were more likely to disseminate inaccurate or negative information about LARC [23]. This highlights the importance for healthcare providers to identify strategies to dispel negative information consistently. In the same vein, cultural barriers may affect contraceptive uptake. The deviation from receiving accurate medical information and counseling about family planning may affect the effectiveness of a method. One study reported that among 321 postpartum women of Mexican origin, LARC use was predominantly low in Austin, Texas, USA (9%) and El Paso, Texas, USA (7%) [24]. This study also showed an overwhelmingly low use between intended and actual LARC use as only 8% used a LARC method compared to 52% who intended to use the same [24]. This disparate utilization supports the revelation that language barriers hinder access to immediate postpartum LARC among non-English speaking patients [25]. Moreover, healthcare providers’ unfounded belief and poor knowledge about some methods of family planning services such as the IUD limit their provision of appropriate contraceptive counseling for their patients.
3.3. Institutional-Level Factors
Institutional-level factors comprise aspects and activities within the healthcare system that influence contraceptive use. Provider schedule and limited training about contraceptive counseling often act as barriers to contraceptive use. A study of 167 pediatricians from the Massachusetts Pediatric Society revealed that 53% of pediatricians did not have the time to counsel teenagers about contraceptives. Another 27% reported receiving no formal training on contraceptive counseling [21]. However, concerning IUD counseling, an overwhelming 117% of pediatricians said they had no formal training on how to do so [21]. Unfortunately, these issues are not unique to teenagers. Among certified midwives and nurse-midwives from the American College of Nurse-Midwives, 63.5% said they desired additional training for inserting immediate postpartum IUD, and 22.8% reported the same sentiments for implant insertion [26]. Indeed, the lack of formal training implies structural barriers suggesting that medical training programs and hospitals do not provide the requisite training needed for providers to enable them to discuss family planning options with patients. Other structural barriers related to contraceptive use include the lack or unavailability of standardized procedures, cost-related challenges, low reimbursement from health insurers, restrictive religious institutional policies, parental consent, or regulatory pharmacy prescription only-model that hinders offering contraceptive counseling and services [20,26,27,28].
Simultaneously, barriers such as issues with confidentiality and privacy, perceived judgment or stigma, lack of clinical space, costs, inadequate health insurance, and limited information about how to access contraceptive services are persistent institutional barriers to contraceptive use [15].
3.4. Community-Level Factors
Community-level factors comprise interactions between and within healthcare organizations, community organizations, and other informal networks that influence contraceptives. Shame and stigma related to sexuality, particularly among sexual minorities, impede contraceptive counseling and use. One study found that queer women have complicated relationships with their healthcare providers because medical professionals often assume they do not need contraceptives [29]. This coincides with results from a national survey showing that lesbians were significantly less likely than heterosexual women to receive contraceptive counseling or prescriptions [30].
3.5. Policy-Level Factors
Policy-level factors are characterized by federal and state policies. Despite the ACA, restrictive state policies can impede access to contraceptive care. Some states declined to expand or ended their state-federal Medicaid family planning expansion programs in favor of a solely state-funded program. However, the state-funded programs exclude, for instance, abortion services. For example, 18 states have abortion-related limitations on the allocation of public funds, 15 states restrict the provision of state family planning funds, 13 states restrict the allotment of some federal and state funds on services such as STI testing and treatment and sex education, and 8 states explicitly limit the allocation of federal Title X family planning to exclude some types of providers, among other forms of restrictions [31].
4. Facilitators of Contraceptive Use
In addition to the barriers discussed above, few studies reported facilitators supporting women’s contraceptive uptake. These themes are displayed in Table 2 and are structured by the social-ecological level, with most facilitators identified at the individual level. Cited examples of facilitators for contraceptive use include peace of mind knowing that there is a minimal risk for pregnancy, trust in providers’ suggestions on the best contraception methods, and same-day LARC insertions to minimize transportation and convenience barriers. Social stigma related to getting pregnant also served as a way to promote contraceptive use, especially among younger populations. Finally, laws that support pharmacists’ and other providers’ ability to prescribe hormonal contraception also minimize barriers for women when obtaining contraceptives. These providers provide a safe, convenient access point for women seeking contraception, and in most cases, provide greater levels of knowledge about contraception than physicians.

Table 2.
Facilitators of Contraceptive Use by Social-Ecological Level.
5. Recommendations to Increase Contraceptive Use
In synthesizing the barriers and facilitators outlined, we developed a set of recommendations to increase access to and uptake for women’s contraceptive use. While not an exhaustive list, these recommendations could help alleviate some of the barriers cited and reduce unplanned pregnancy’s negative consequences.
At the most basic level, steps to increase knowledge and confidence in contraceptive use are critical. Barriers related to lack of knowledge are extensively cited in the literature. Among studies that discussed facilitators to contraceptive use, women who knew the benefits of contraception were more likely to utilize it. An increase in knowledge can be accomplished by incorporating contraceptive counseling into well-woman exams and moving from abstinence education programs to more holistic sexual education programs that discuss all methods to prevent pregnancy.
Provider communication is key to disseminating information on contraceptives to women. Providers serve as trusted sources of information; however, many lack the knowledge to make informed recommendations for contraceptive selection based on a woman’s needs. Therefore, more extensive training for family practitioners, midwives, and nurses could prove useful in serving as a resource to support women’s uptake of contraceptives. Furthermore, younger providers and females were also more likely to discuss contraception with their patients. Continuing education for existing providers and targeted training for male providers could support their confidence and ability to carry out contraceptive counseling.
Community movements supporting contraceptive use and removing the social stigma related to contraception are also ways to support women’s contraceptive uptake. While in theory, this can prove challenging, community initiatives that bring together multiple stakeholders, such as nonprofit, community, and medical organizations, are becoming more and more prevalent in public health. These movements create a shared plan and approach to improving health within a community and focus on supplying trusted information and resources through multiple initiatives to result in community change.
Policy-level initiatives that expand the ability of healthcare providers to recommend and prescribe contraception can help minimize access barriers to contraceptive use. These policies support providers’ training in contraceptive counseling and increase the chances for a woman to receive trusted information from multiple sources. Additionally, government-mandated insurance coverage for all forms of contraceptives is essential to removing financial barriers faced by women.
6. Policy Implications
Contraceptive use is not only beneficial for women, but it also has implications for public spending and society at large. Studies show that increases in contraceptive use, facilitated by Medicaid expansion, reduced infant mortality rates, especially among subpopulations (e.g., African Americans) [36]. Furthermore, the provision of postpartum IUD placement for low-income and underinsured women was found to significantly reduce state expenditures related to subsequent unintended pregnancies [37]. As a result, public policies that increase the accessibility and affordability of contraceptives, as well as the availability of providers to serve as sources of information, could pave the way for reducing unintended pregnancies, decreasing negative health and economic outcomes for a woman and her child, and improving population-level outcomes for future generations. In addition, policies aimed at providing comprehensive sexual education within the school setting should be encouraged and adopted. This is because our review indicates that abstinence-only sexual education limits knowledge and accurate use of contraceptives.
Our review also suggests that contraceptive use has political and societal ramifications. Hence, legislation should account for these variables while ensuring that women’s autonomy is not diminished.
7. Limitations
Although this study contributes comprehensively to the literature, there are some limitations. First, we conducted a nonsystematic literature search with only two electronic databases, leading to potential article selection bias. Even so, we did not assess the quality of the literature reviewed. Second, we focused on contraceptives and did not stratify them by contraceptive types, which might have facilitated in-depth knowledge in those aspects. Given these limitations, future studies should adopt a more rigorous systematic approach to better inform public health policies and efforts.
8. Conclusions
Although, on the surface, it seems as though there is universal access to contraceptive use in the US, an in-depth analysis demonstrates persistent gaps exist in contraceptive access, particularly among vulnerable women. This study calls for strategies to address contraceptive use from a multidimensional apparatus to ensure equitable access to contraception.
Author Contributions
K.V.A. and S.P. conceptualized the idea, writing—writing and editing. W.R.G. and K.W., writing—editing and supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Department of Health and Human Services, Office of the Assistant Secretary for Health, Office of Population Affairs under grant number [AH-TP2-20-002]—Tier 2 Innovation and Impact Network Grants: Achieving Optimal Health and Preventing Teen Pregnancy in Key Priority Areas. Its contents are solely the authors’ responsibility and do not necessarily represent the official views of the Department of Health and Human Services or the Office of Population Affairs.
Institutional Review Board Statement
Not applicable as this study did not involve humans or animals.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ten Great Public Health Achievements–United States, 1900–1999. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm (accessed on 28 September 2021).
- The Social and Economic Benefits of Women’s Ability to Determine Whether and When to Have Children|Guttmacher Institute. Available online: https://www.guttmacher.org/report/social-and-economic-benefits-womens-ability-determine-whether-and-when-have-children (accessed on 28 September 2021).
- Family Planning/Contraception Methods. Available online: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception (accessed on 28 September 2021).
- Moving Forward: Family Planning in the Era of Health Reform|Guttmacher Institute. Available online: https://www.guttmacher.org/report/moving-forward-family-planning-era-health-reform (accessed on 28 September 2021).
- Kavanaugh, M.L.; Pliskin, E. Use of Contraception among Reproductive-Aged Women in the United States, 2014 and 2016. F&S Rep. 2020, 1, 83. [Google Scholar] [CrossRef]
- Kavanaugh, M.L.; Jerman, J. Contraceptive Method Use in the United States: Trends and Characteristics between 2008, 2012 and 2014. Contraception 2018, 97, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Products-Data Briefs-Number 388-October 2020. Available online: https://www.cdc.gov/nchs/products/databriefs/db388.htm (accessed on 28 September 2021).
- Daniels, K.; Daugherty, J.; Jones, J. Current contraceptive status among women aged 15-44: United States, 2011–2013. NCHS Data Brief 2014, 173, 1–8. [Google Scholar]
- Abma, J.C.; Martinez, G.M. Sexual Activity and Contraceptive Use among Teenagers in the United States, 2011–2015. Natl. Health Stat. 2017, 104, 1–23. [Google Scholar]
- Birth control methods | Office on Women’s Health. Available online: https://www.womenshealth.gov/a-z-topics/birth-control-methods (accessed on 28 September 2021).
- Contraceptive Needs and Services, 2014 Update | Guttmacher Institute. Available online: https://www.guttmacher.org/report/contraceptive-needs-and-services-2014-update (accessed on 28 September 2021).
- Finer, L.B.; Zolna, M.R. Unintended Pregnancy in the United States: Incidence and Disparities, 2006. Contraception 2011, 84, 478–485. [Google Scholar] [CrossRef] [Green Version]
- Unintended Pregnancy In the United States | Guttmacher Institute. Available online: https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states (accessed on 28 September 2021).
- Mcleroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Behav. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Garney, W.; Wilson, K.; Ajayi, K.V.; Panjwani, S.; Love, S.M.; Flores, S.; Garcia, K.; Esquivel, C. Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 4138. [Google Scholar] [CrossRef]
- Aura, A.; Sormunen, M.; Tossavainen, K. The Relation of Socio-Ecological Factors to Adolescents’ Health-Related Behaviour: A Literature Review. Health Educ. 2016, 2016, 177–201. [Google Scholar] [CrossRef]
- Guiahi, M. Religious Refusals to Long-Acting Reversible Contraceptives in Catholic Settings: A Call for Evidence. Am. J. Obstet. Gynecol. 2020, 222, S869.e1–S869.e5. [Google Scholar] [CrossRef]
- Hall, K.S.; Ela, E.; Zochowski, M.K.; Caldwell, A.; Moniz, M.; McAndrew, L.; Steel, M.; Challa, S.; Dalton, V.K.; Ernst, S. “I Don’t Know Enough to Feel Comfortable Using Them:” Women’s Knowledge of and Perceived Barriers to Long-Acting Reversible Contraceptives on a College Campus. Contraception 2016, 93, 556–564. [Google Scholar] [CrossRef] [Green Version]
- Raidoo, S.; Kaneshiro, B. Contraception Counseling for Adolescents. Curr. Opin. Obstet. Gynecol. 2017, 29, 310–315. [Google Scholar] [CrossRef]
- Gomez, A.M.; Fuentes, L.; Allina, A. Women or LARC First? Reproductive Autonomy and the Promotion of Long-Acting Contraceptive Methods. Perspect. Sex. Reprod. Health 2014, 46, 171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, S.F.; Strohsnitter, W.; Baecher-Lind, L. Practices and Perceptions among Pediatricians Regarding Adolescent Contraception with Emphasis on Intrauterine Contraception. J. Pediatr. Adolesc. Gynecol. 2013, 26, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Akers, A.Y.; Gold, M.A.; Borrero, S.; Santucci, A.; Schwarz, E.B. Providers’ Perspectives on Challenges to Contraceptive Counseling in Primary Care Settings. J. Women’s Health 2010, 19, 1163–1170. [Google Scholar] [CrossRef]
- Mahony, H.; Spinner, C.; Vamos, C.A.; Daley, E.M. Social Network Influences on Young Women’s Choice to Use Long-Acting Reversible Contraception: A Systematic Review. J. Midwifery Women’s Health 2021, 7. [Google Scholar] [CrossRef]
- Potter, J.E.; Hubert, C.; White, K. The Availability and Use of Postpartum LARC in Mexico and Among Hispanics in the United States. Matern. Child Health J. 2016, 21, 1744–1752. [Google Scholar] [CrossRef] [PubMed]
- Wallace Huff, C.; Potter, J.E.; Hopkins, K. Patients’ Experiences with an Immediate Postpartum Long-Acting Reversible Contraception Program. Women’s Health Issues 2021, 31, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Moniz, M.H.; Roosevelt, L.; Crissman, H.P.; Kobernik, E.K.; Dalton, V.K.; Heisler, M.H.; Low, L.K. Immediate Postpartum Contraception: A Survey Needs Assessment of a National Sample of Midwives. J. Midwifery Women’s Health 2017, 62, 538–544. [Google Scholar] [CrossRef]
- Moniz, M.H.; McEvoy, A.K.; Hofmeister, M.; Plegue, M.; Chang, T. Family Physicians and Provision of Immediate Postpartum Contraception: A Cera Study. Fam. Med. 2017, 49, 600–606. [Google Scholar]
- Rafie, S.; Haycock, M.; Rafie, S.; Yen, S.; Harper, C.C. Direct Pharmacy Access to Hormonal Contraception: California Physician and Advanced Practice Clinician Views. Contraception 2012, 86, 687–693. [Google Scholar] [CrossRef]
- HHiggins, J.A.; Carpenter, E.; Everett, B.G.; Greene, M.Z.; Haider, S.; Hendrick, C.E. Sexual Minority Women and Contraceptive Use: Complex Pathways Between Sexual Orientation and Health Outcomes. Am. J. Public Health 2019, 109, 1680–1686. [Google Scholar] [CrossRef]
- Everett, B.G.; Higgins, J.A.; Haider, S.; Carpenter, E. Do Sexual Minorities Receive Appropriate Sexual and Reproductive Health Care and Counseling? J. Women’s Health 2019, 28, 53–62. [Google Scholar] [CrossRef]
- State Family Planning Funding Restrictions | Guttmacher Institute. Available online: https://www.guttmacher.org/state-policy/explore/state-family-planning-funding-restrictions (accessed on 28 September 2021).
- FFree, C.; Ogden, J.; Lee, R. Young women’s contraception use as a contextual and dynamic behaviour: A qualitative study. Psychol. Health 2005, 20, 673–690. [Google Scholar] [CrossRef]
- Campo, S.; Askelson, N.M.; Spies, E.L.; Losch, M. Preventing Unintended Pregnancies and Improving Contraceptive Use among Young Adult Women in a Rural, Midwestern State: Health Promotion Implications. Women Health 2010, 50, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Politi, M.C.; Estlund, A.; Milne, A.; Buckel, C.M.; Peipert, J.F.; Madden, T. Barriers and Facilitators to Implementing a Patient-Centered Model of Contraceptive Provision in Community Health Centers. Contracept. Reprod. Med. 2016, 1, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez, A.M.; McCullough, C.; Fadda, R.; Ganguly, B.; Gustafson, E.; Severson, N.; Tomlitz, J. Facilitators and barriers to implementing pharmacist-prescribed hormonal contraception in California independent pharmacies. Women Health 2019, 60, 249–259. [Google Scholar] [CrossRef]
- Bhatt, C.B.; Beck-Sague, C.M. Medicaid Expansion and Infant Mortality in the United States. Am. J. Public Health 2018, 108, 565–567. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.I.; Caughey, A.B.; Edelman, A.; Darney, P.D.; Foster, D.G. Cost–benefit analysis of state- and hospital-funded postpartum intrauterine contraception at a university hospital for recent immigrants to the United States. Contraception 2010, 81, 304–308. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).