Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Group-Based Score Changes
3.2. Directionality in the S-Reg↔S-Eff Change Relationships
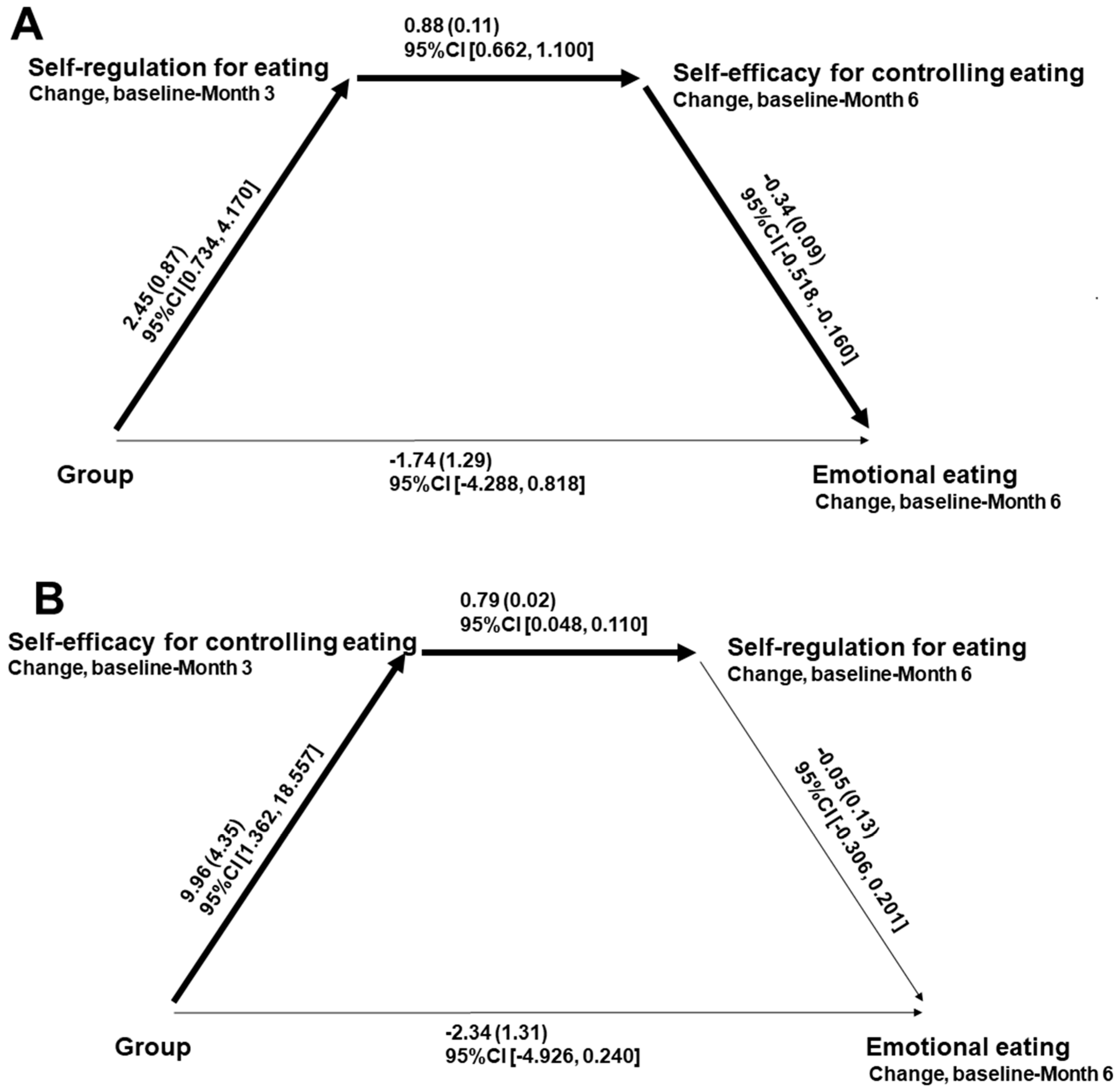
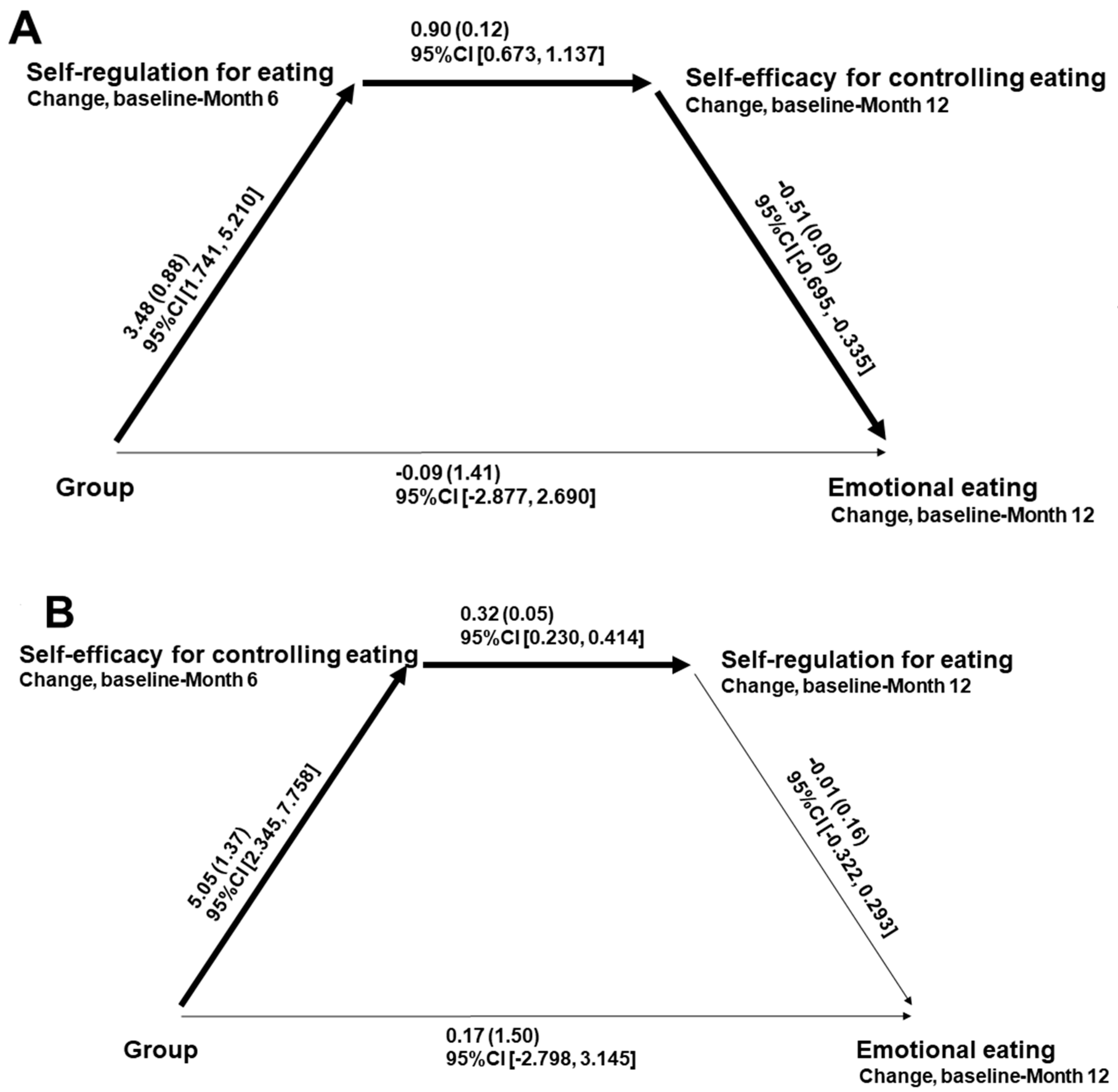
3.3. Contrasting Directionality Across Proposed Paths
3.4. Association of Reduced EmE with Weight/Waist Circumference Reductions
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2021 US Obesity Forecasting Collaborators. National-level and state-level prevalence of overweight and obesity among children, adolescents, and adults in the USA, 1990–2021, and forecasts up to 2050. Lancet 2024, 404, 2278–2298. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Kim, K.K.; Wilding, J.P.H.; World Obesity Federation. Obesity: A chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 2017, 18, 715–723. [Google Scholar] [CrossRef]
- Dombrowski, S.U.; Knittle, K.; Avenell, A.; Araújo-Soares, V.; Sniehotta, F.F. Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ 2014, 348, g2646. [Google Scholar] [CrossRef]
- MacLean, P.S.; Wing, R.R.; Davidson, T.; Epstein, L.; Goodpaster, B.; Hall, K.D.; Levin, B.E.; Perri, M.G.; Rolls, B.J.; Rosenbaum, M.; et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity 2015, 23, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Koenders, P.G.; van Strien, T. Emotional eating, rather than lifestyle behavior, drives weight gain in a prospective study in 1562 employees. J. Occup. Environ. Med. 2011, 53, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Vasileiou, V.; Abbott, S. Emotional eating among adults with healthy weight, overweight and obesity: A systematic review and meta-analysis. J. Hum. Nutr. Diet. 2023, 36, 1922–1930. [Google Scholar] [CrossRef] [PubMed]
- Péneau, S.; Ménard, E.; Méjean, C.; Bellisle, F.; Hercberg, S. Sex and dieting modify the association between emotional eating and weight status. Am. J. Clin. Nutr. 2013, 97, 1307–1313. [Google Scholar] [CrossRef]
- Smith, J.M.; Serier, K.N.; Belon, K.E.; Sebastian, R.M.; Smith, J.E. Evaluation of the relationships between dietary restraint, emotional eating, and intuitive eating moderated by sex. Appetite 2020, 155, 104817. [Google Scholar] [CrossRef]
- Mata, J.; Silva, M.N.; Vieira, P.N.; Carraça, E.V.; Andrade, A.M.; Coutinho, S.R.; Sardinha, L.B.; Teixeira, P.J. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009, 28, 709–716. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Silva, M.N.; Coutinho, S.R.; Palmeira, A.L.; Mata, J.; Vieira, P.N.; Carraça, E.V.; Santos, T.C.; Sardinha, L.B. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity 2010, 18, 725–735. [Google Scholar] [CrossRef]
- Annesi, J.J. Behavioral weight loss and maintenance: A 25-year research program informing innovative programming. Perm. J. 2022, 26, 98–117. [Google Scholar] [CrossRef]
- Cooper, Z.; Doll, H.A.; Hawker, D.M.; Byrne, S.; Bonner, G.; Eeley, E.; O’connor, M.E.; Fairburn, C.G. Testing a new cognitive behavioural treatment for obesity: A randomized controlled trial with three-year follow-up. Behav. Res. Ther. 2010, 48, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Altieri, M.S.; Irish, W.; Pories, W.J.; Shah, A.; DeMaria, E.J. Examining the rates of obesity and bariatric surgery in the United States. Obes. Surg. 2021, 31, 4754–4760. [Google Scholar] [CrossRef] [PubMed]
- Berning, P.; Adhikari, R.; Schroer, A.E.; Jelwan, Y.A.; Razavi, A.C.; Blaha, M.J.; Dzaye, O. Longitudinal analysis of obesity drug use and public awareness. JAMA Netw. Open 2025, 8, e2457232. [Google Scholar] [CrossRef]
- Himmerich, H.; Lewis, Y.D.; Conti, C.; Mutwalli, H.; Karwautz, A.; Sjögren, J.M.; Isaza, M.M.U.; Tyszkiewicz-Nwafor, M.; Aigner, M.; McElroy, S.L.; et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines update 2023 on the pharmacological treatment of eating disorders. World J. Biol. Psychiatry 2023, 24, 643–706. [Google Scholar] [CrossRef]
- Jastreboff, A.M.; Aronne, L.J.; Ahmad, N.N.; Wharton, S.; Connery, L.; Alves, B.; Kiyosue, A.; Zhang, S.; Liu, B.; Bunck, M.C.; et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 2022, 387, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Harding, S. Mental health implications of weight loss medications: A narrative review. J. Nurse Pract. 2024, 20, 105207. [Google Scholar] [CrossRef]
- Radkhah, H.; Anaraki, S.R.; Roudsari, P.P.; Bahri, R.A.; Zooravar, D.; Asgarian, S.; Dolama, R.H.; Alirezaei, A.; Khalooeifard, R. The impact of glucagon-like peptide-1 (GLP-1) agonists in the treatment of eating disorders: A systematic review and meta-analysis. Eat. Weight Disord. 2025, 30, 10. [Google Scholar] [CrossRef]
- Jeffery, R.W.; Drewnowski, A.; Epstein, L.H.; Wilson, G.T.; Stunkard, A.J.; Wing, R.R. Long-term maintenance of weight loss: Current status. Health Psychol. 2000, 19, 5–16. [Google Scholar] [CrossRef]
- Mann, T.; Tomiyama, A.J.; Westling, E.; Lew, A.M.; Samuels, B.; Chatman, J. Medicare’s search for effective obesity treatments: Diets are not the answer. Am. Psychol. 2007, 62, 220–233. [Google Scholar] [CrossRef]
- Spieker, E.A.; Pyzocha, N. Economic impact of obesity. Prim. Care 2016, 43, 83–95. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Vohs, K.D.; Baumeister, R.F. (Eds.) Handbook of Self-Regulation: Research, Theory, and Application, 3rd ed.; Guilford: New York, NY, USA, 2017. [Google Scholar]
- Carraça, E.V.; Silva, M.N.; Coutinho, S.R.; Vieira, P.N.; Minderico, C.S.; Sardinha, L.B.; Teixeira, P.J. The association between physical activity and eating self-regulation in overweight and obese women. Obes. Facts 2013, 6, 493–506. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Marques, M.M.; Rutter, H.; Oppert, J.-M.; De Bourdeaudhuij, I.; Lakerveld, J.; Brug, J. Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Med. 2015, 13, 84. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J. Supported exercise improves controlled eating and weight through its effects on psychosocial factors: Extending a systematic research program toward treatment development. Perm. J. 2012, 16, 7–18. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Clark, M.M.; Abrams, D.B.; Niaura, R.S.; Eaton, C.A.; Rossi, J.S. Self-efficacy in weight management. J. Consult. Clin. Psychol. 1991, 59, 739–744. [Google Scholar] [CrossRef]
- Lombardo, C.; Cerolini, S.; Alivernini, F.; Ballesio, A.; Violani, C.; Fernandes, M.; Lucidi, F. Eating self-efficacy: Validation of a new brief scale. Eat. Weight Disord. 2021, 26, 295–303. [Google Scholar] [CrossRef]
- Nezami, B.T.; Lang, W.; Jakicic, J.M.; Davis, K.K.; Polzien, K.; Rickman, A.D.; Hatley, K.E.; Tate, D.F. The effect of self-efficacy on behavior and weight in a behavioral weight-loss intervention. Health Psychol. 2016, 35, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. The primacy of self-regulation in health promotion. Appl. Psychol. 2005, 54, 245–254. [Google Scholar] [CrossRef]
- Conn, V.S. Older women: Social cognitive theory correlates of health behavior. Women Health 1997, 26, 71–85. [Google Scholar] [CrossRef]
- Kitsantas, A. The role of self-regulation strategies and self-efficacy perceptions in successful weight loss maintenance. Psychol. Health 2000, 15, 811–820. [Google Scholar] [CrossRef]
- Zimmerman, B.J.; Schunk, D.H.; DiBenedetto, M.K. The Role of Self-Efficacy and Related Beliefs in Self-Regulation of Learning and Performance. In Handbook of Competence and Motivation: Theory and Application, 2nd ed.; Elliot, A.J., Dweck, C.S., Yeager, D.S., Eds.; Guilford: New York, NY, USA, 2017; pp. 313–333. [Google Scholar]
- Blaxall, M.; Richardson, R.; Schoonees, A.; Metzendorf, M.; Durão, S.; Naude, C.; Bero, L.; Farquhar, C. Obesity intervention evidence synthesis: Where are the gaps and which should we address first? Obes. Rev. 2024, 25, e13685. [Google Scholar] [CrossRef]
- Byrne, M. Gaps and priorities in advancing methods for health behaviour change research. Health Psychol. Rev. 2020, 14, 165–175. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Annesi, J.J.; Marti, C.N. Path analysis of exercise treatment-induced changes in psychological factors leading to weight loss. Psychol. Health 2011, 26, 1081–1098. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef]
- Ames, G.E.; Heckman, M.G.; Grothe, K.B.; Clark, M.M. Eating self-efficacy: Development of a short-form WEL. Eat. Behav. 2012, 13, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Warziski, M.; Sereika, S.M.; Styn, M.A.; Music, E.; Burke, L.E. Changes in self-efficacy and dietary adherence: The impact on weight loss in the PREFER study. J. Behav. Med. 2008, 31, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Arnow, B.; Kenardy, J.; Agras, W.S. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 1995, 18, 79–90. [Google Scholar] [CrossRef]
- Ricca, V.; Castellini, G.; Lo Sauro, C.; Ravaldi, C.; Lapi, F.; Mannucci, E.; Rotella, C.M.; Faravelli, C. Correlations between binge eating and emotional eating in a sample of overweight subjects. Appetite 2009, 53, 418–421. [Google Scholar] [CrossRef]
- National Institutes of Health/National Cancer Institute. Evidence-Based Cancer Control Program: Obesity. Available online: https://ebccp.cancercontrol.cancer.gov/topicPrograms.do?topicId=1592287&choice=default (accessed on 13 November 2025).
- Champion, V.L.; Skinner, C.S. The Health Belief Model. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K.V., Eds.; Jossey-Bass/Wiley: Hoboken, NJ, USA, 2015; pp. 45–65. [Google Scholar]
- Kaiser Permanente Health Education Services. Cultivating Health Weight Management Kit, 9th ed.; Kaiser Foundation Health Plan of the Northwest: Portland, OR, USA, 2009. [Google Scholar]
- White, I.R.; Horton, N.J.; Carpenter, J.; Pocock, S.J. Strategy for intention to treat data in randomized trials with missing outcome data. BMJ 2011, 342, d40. [Google Scholar] [CrossRef]
- Ding, W.; Song, P.X.-K. EM algorithm in Gaussian copula with missing data. Comput. Stat. Data Anal. 2016, 101, 1–11. [Google Scholar] [CrossRef]
- Little, R.J.; Rubin, D.B. Statistical Analysis with Missing Data, 2nd ed.; Wiley: Hoboken, NJ, USA, 2014. [Google Scholar]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Lawrence Erlbaum: Mahwah, NJ, USA, 2003. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Guilford: New York, NY, USA, 2022. [Google Scholar]
- Armstrong, R.A. When to use the Bonferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Perneger, T.V. What’s wrong with Bonferroni adjustments. BMJ 1998, 316, 1236–1238. [Google Scholar] [CrossRef]
- Barak, R.E.; Shuval, K.; Li, Q.; Oetjen, R.; Drope, J.; Yaroch, A.L.; Fennis, B.M.; Harding, M. Emotional eating in adults: The role of sociodemographics, lifestyle behaviors, and self-regulation-findings from a U.S. national study. Int. J. Environ. Res. Public Health 2021, 18, 1744. [Google Scholar] [CrossRef]
- Jones, C.J.; Smith, H.; Llewellyn, C. Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Health Psychol. Rev. 2014, 8, 253–269. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.; Moullec, G.; Lavoie, K.L.; Laurin, C.; Cowan, T.; Tisshaw, C.; Kazazian, C.; Raddatz, C.; Bacon, S.L. Impact of cognitive-behavioral interventions on weight loss and psychological outcomes: A meta-analysis. Health Psychol. 2018, 37, 417–432. [Google Scholar] [CrossRef]
- Armitage, C.J. Randomized test of a brief psychological intervention to reduce and prevent emotional eating in a community sample. J. Public Health 2015, 37, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Frayn, M.; Knäuper, B. Emotional eating and weight in adults: A review. Curr. Psychol. 2018, 37, 924–933. [Google Scholar] [CrossRef]
- van Strien, T. Causes of emotional eating and matched treatment of obesity. Curr. Diab. Rep. 2018, 18, 35. [Google Scholar] [CrossRef]
- Carillo, K.D. Social Cognitive Theory in IS Research—Literature Review, Criticism, and Research Agenda. In Information Systems, Technology and Management: Communications in Computer and Information Science; Prasad, S.K., Vin, H.M., Sahni, S., Jaiswal, M.P., Thipakorn, B., Eds.; Springer: New York, NY, USA, 2010; Volume 54. [Google Scholar]
- Comșa, L.; David, O.; David, D. Outcomes and mechanisms of change in cognitive-behavioral interventions for weight loss: A meta-analysis of randomized clinical trials. Behav. Res. Ther. 2020, 132, 103654. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Tice, D.M.; Vohs, K.D. The strength model of self-regulation: Conclusions from the second decade of willpower research. Perspect. Psychol. Sci. 2018, 13, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Brownell, K.D. The humbling experience of treating obesity: Should we persist or desist? Behav. Res. Ther. 2010, 48, 717–719. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Bray, G.A.; Ryan, D.H. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity 2015, 23, 2319–2320. [Google Scholar] [CrossRef] [PubMed]
| Measure | Effect for Time | Time × Group Effect | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment Group | F(1, 144) | p | η2p | M | SD | M | SD | M | SD | F(1, 144) | p | η2p |
| Baseline | Month 3 | Baseline-Month 3 change | ||||||||||
| Self-regulation for eating | 122.43 | <0.001 | 0.46 | 8.34 | <0.001 | 0.06 | ||||||
| Cognitive–behavioral methods | 23.51 | 5.15 | 30.98 | 4.55 | 7.47 | 6.60 | ||||||
| Weight loss education methods | 22.50 | 5.64 | 26.88 | 5.38 | 4.38 | 5.13 | ||||||
| Aggregated data | 23.16 | 5.32 | 29.58 | 5.21 | 6.41 | 6.30 | ||||||
| Self-efficacy for controlling eating | 1605.03 | <0.001 | 0.92 | 4.87 | 0.029 | 0.03 | ||||||
| Cognitive–behavioral methods | 22.25 | 6.38 | 113.09 | 27.24 | 90.84 | 24.87 | ||||||
| Weight loss education methods | 22.25 | 7.87 | 103.60 | 27.73 | 81.36 | 24.21 | ||||||
| Aggregated data | 22.25 | 6.90 | 109.84 | 27.68 | 87.59 | 24.97 | ||||||
| Baseline | Month 6 | Baseline–Month 6 change | ||||||||||
| Self-regulation for eating | 131.11 | <0.001 | 0.53 | 20.30 | <0.001 | 0.12 | ||||||
| Cognitive–behavioral methods | 23.51 | 5.15 | 32.42 | 3.77 | 8.91 | 6.35 | ||||||
| Weight loss education methods | 22.50 | 5.64 | 26.72 | 5.44 | 4.38 | 5.13 | ||||||
| Aggregated data | 23.16 | 5.32 | 30.47 | 5.17 | 7.30 | 6.32 | ||||||
| Self-efficacy for controlling eating | 98.45 | <0.001 | 0.41 | 15.53 | <0.001 | 0.10 | ||||||
| Cognitive–behavioral methods | 22.25 | 6.38 | 31.70 | 7.20 | 9.44 | 7.94 | ||||||
| Weight loss education methods | 22.25 | 7.87 | 26.32 | 8.00 | 4.08 | 7.57 | ||||||
| Aggregated data | 22.25 | 6.90 | 29.86 | 7.88 | 7.61 | 8.19 | ||||||
| Emotional eating | 102.79 | <0.001 | 0.42 | 10.14 | 0.002 | 0.07 | ||||||
| Cognitive–behavioral methods | 27.71 | 7.99 | 17.94 | 8.28 | −9.77 | 9.70 | ||||||
| Weight loss education methods | 25.10 | 9.66 | 20.00 | 9.69 | −5.10 | 5.05 | ||||||
| Aggregated data | 26.82 | 8.65 | 18.64 | 8.81 | −8.17 | 8.67 | ||||||
| Weight (kg) | 165.75 | <0.001 | 0.54 | 50.57 | <0.001 | 0.26 | ||||||
| Cognitive–behavioral methods | 95.16 | 11.86 | 89.44 | 11.70 | −5.72 | 3.59 | ||||||
| Weight loss education methods | 96.21 | 10.02 | 94.56 | 9.61 | −1.65 | 2.58 | ||||||
| Aggregated data | 95.52 | 11.24 | 91.19 | 11.26 | −4.33 | 3.80 | ||||||
| Waist circumference (cm) | 75.91 | <0.001 | 0.35 | 52.67 | <0.001 | 0.27 | ||||||
| Cognitive–behavioral methods | 106.38 | 9.27 | 100.30 | 9.76 | −6.07 | 4.57 | ||||||
| Weight loss education methods | 105.55 | 7.86 | 105.00 | 8.09 | −0.55 | 3.91 | ||||||
| Aggregated data | 106.09 | 8.79 | 101.91 | 9.46 | −4.18 | 5.08 | ||||||
| Baseline | Month 12 | Baseline–Month 12 change | ||||||||||
| Emotional eating | 76.39 | <0.001 | 0.35 | 2.55 | 0.113 | 0.02 | ||||||
| Cognitive–behavioral methods | 27.71 | 7.99 | 18.71 | 9.09 | −9.00 | 10.54 | ||||||
| Weight loss education methods | 25.10 | 9.66 | 18.88 | 9.97 | −6.22 | 8.81 | ||||||
| Aggregated data | 26.82 | 8.65 | 18.77 | 9.37 | −8.05 | 10.04 | ||||||
| Weight (kg) | 81.89 | <0.001 | 0.36 | 31.43 | <0.001 | 0.18 | ||||||
| Cognitive–behavioral methods | 95.16 | 11.86 | 89.63 | 11.96 | −5.53 | 4.35 | ||||||
| Weight loss education methods | 96.21 | 10.02 | 94.91 | 10.34 | −1.30 | 4.28 | ||||||
| Aggregated data | 95.52 | 11.24 | 91.44 | 11.67 | −4.08 | 4.76 | ||||||
| Waist circumference (cm) | 52.24 | <0.001 | 0.27 | 30.39 | <0.001 | 0.17 | ||||||
| Cognitive–behavioral methods | 106.38 | 9.27 | 100.71 | 10.32 | −5.66 | 5.42 | ||||||
| Weight loss education methods | 105.55 | 7.86 | 104.79 | 8.33 | −0.76 | 4.41 | ||||||
| Aggregated data | 106.09 | 8.79 | 102.11 | 9.85 | −3.98 | 5.59 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Annesi, J.J.; Machek, S.B. Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy. Obesities 2025, 5, 83. https://doi.org/10.3390/obesities5040083
Annesi JJ, Machek SB. Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy. Obesities. 2025; 5(4):83. https://doi.org/10.3390/obesities5040083
Chicago/Turabian StyleAnnesi, James J., and Steven B. Machek. 2025. "Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy" Obesities 5, no. 4: 83. https://doi.org/10.3390/obesities5040083
APA StyleAnnesi, J. J., & Machek, S. B. (2025). Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy. Obesities, 5(4), 83. https://doi.org/10.3390/obesities5040083






