Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity
Abstract
1. Introduction
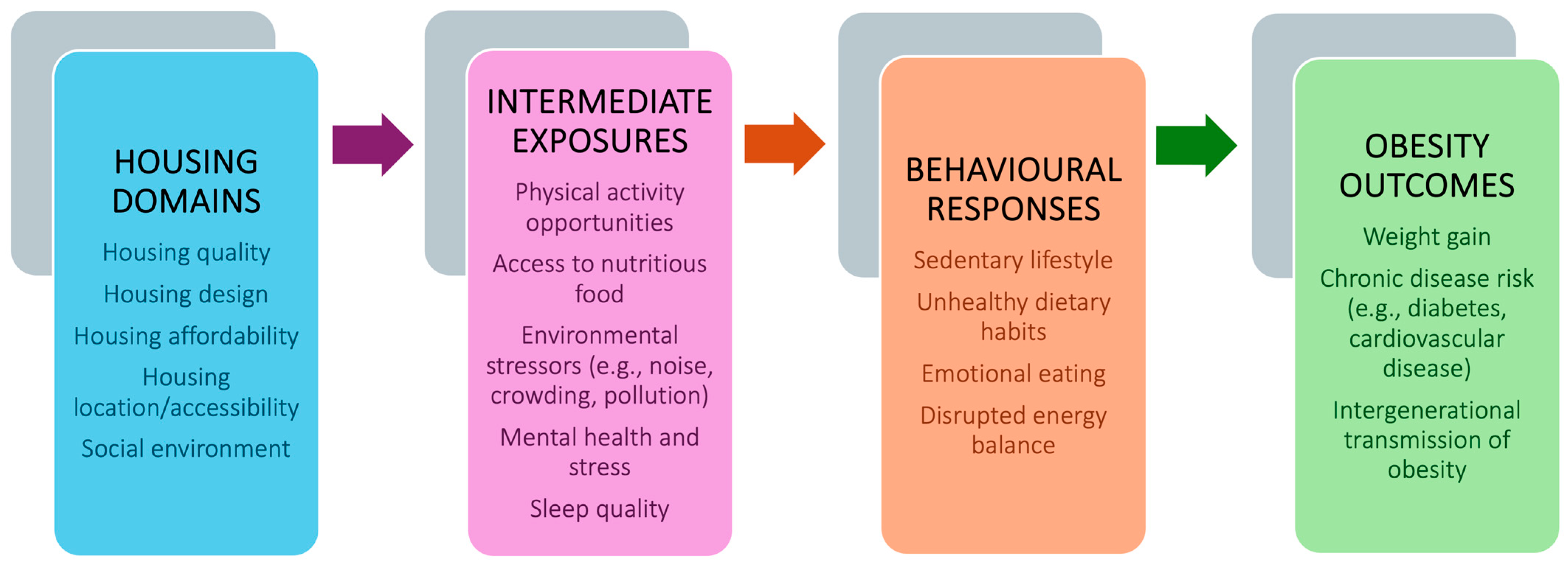
2. Definition and Conceptualization of “Obesity–Housing Nexus”
3. Methods
4. The Gap in the Relative Importance of Individual Versus Environmental Factors
5. Obesity–Housing Nexus
5.1. Housing Quality and Obesity
5.2. Housing Design and Physical Activity
5.3. Housing Location and Access to Amenities
5.4. Neighborhood Walkability and Obesity
5.5. Housing Affordability and Obesity
5.6. Social Environment and Obesity
6. Policy Implications and Future Directions
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The Lancet Gastroenterology & Hepatology. Obesity: Another Ongoing Pandemic. Lancet Gastroenterol. Hepatol. 2021, 6, 411. [Google Scholar] [CrossRef]
- WHO. Obesity. Available online: https://www.who.int/news-room/facts-in-pictures/detail/6-facts-on-obesity#:~:text=More%20than%201.9%20billion%20adults,%2D%20and%20middle%2Dincome%20countries (accessed on 28 June 2025).
- Chimoriya, R.; Rana, K.; Adhikari, J.; Aitken, S.J.; Poudel, P.; Baral, A.; Rawal, L.; Piya, M.K. The Association of Physical Activity with Overweight/Obesity and Type 2 Diabetes in Nepalese Adults: Evidence from a Nationwide Non-Communicable Disease Risk Factor Survey. Obes. Sci. Pract. 2025, 11, e70046. [Google Scholar] [CrossRef]
- Rana, K.; Ghimire, P.; Chimoriya, R.; Chimoriya, R. Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors Among Women in Nepal: Findings from the Nepal Demographic and Health Surveys. Obesities 2021, 1, 113–135. [Google Scholar] [CrossRef]
- Rana, K.; Chimoriya, R.; Haque, N.B.; Piya, M.K.; Chimoriya, R.; Ekholuenetale, M.; Arora, A. Prevalence and Correlates of Underweight Among Women of Reproductive Age in Nepal: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 11737. [Google Scholar] [CrossRef]
- Jin, X.; Qiu, T.; Li, L.; Yu, R.; Chen, X.; Li, C.; Proud, C.G.; Jiang, T. Pathophysiology of obesity and its associated diseases. Acta Pharm. Sin. B 2023, 13, 2403–2424. [Google Scholar] [CrossRef]
- Martin-Rodriguez, E.; Guillen-Grima, F.; Martí, A.; Brugos-Larumbe, A. Comorbidity associated with obesity in a large population: The APNA study. Obes. Res. Clin. Pract. 2015, 9, 435–447. [Google Scholar] [CrossRef]
- Chimoriya, R.; Ho, V.; Wang, Z.V.; Chang, R.; Boumelhem, B.B.; Simmons, D.; Kormas, N.; Gorrell, M.D.; Piya, M.K. Application and Diagnostic Performance of Two-Dimensional Shear Wave Elastography and Liver Fibrosis Scores in Adults with Class 3 Obesity. Nutrients 2024, 16, 74. [Google Scholar] [CrossRef]
- Chimoriya, R.; Naylor, J.; Mitlehner, K.; Adie, S.; Harris, I.; Bell-Higgs, A.; Brosnahan, N.; Piya, M.K. Remote Delivery of Partial Meal Replacement for Weight Loss in People Awaiting Arthroplasty. J. Clin. Med. 2024, 13, 3227. [Google Scholar] [CrossRef]
- Chimoriya, R.; Mitlehner, K.; Khoo, C.L.; Osuagwu, U.L.; Thomson, R.; Si, L.; Lean, M.; Simmons, D.; Piya, M.K. Translation of a Diabetes Remission Service into Australian Primary Care: Findings from the Evaluation of DiRECT-Australia. J. Diabetes Res. 2024, 2024, 2350551. [Google Scholar] [CrossRef]
- Khoo, C.L.; Chimoriya, R.; Simmons, D.; Piya, M.K. Partial Meal Replacement for People with Type 2 Diabetes: 2-Year Outcomes from an Australian General Practice. Aust. J. Prim. Health 2022, 29, 74–80. [Google Scholar] [CrossRef]
- Goodman, C.C.; Fuller, K.S.; Pribyl, M.M.; Gorman, I. Epigenetics: Behavioral, Social, and Environmental Factors. In Goodman and Fuller’s Pathology: Implications for the Physical Therapist; Elsevier: Amsterdam, The Netherlands, 2020; Volume 13. [Google Scholar]
- Jennings, V.; Browning, M.H.; Rigolon, A. Urban Green Spaces: Public Health and Sustainability in the United States; Springer: Cham, Switzerland, 2019; Volume 8. [Google Scholar]
- Elinder, L.S.; Jansson, M. Obesogenic environments–aspects on measurement and indicators. Public Health Nutr. 2009, 12, 307–315. [Google Scholar] [CrossRef]
- Papas, M.A.; Alberg, A.J.; Ewing, R.; Helzlsouer, K.J.; Gary, T.L.; Klassen, A.C. The built environment and obesity. Epidemiol. Rev. 2007, 29, 129–143. [Google Scholar] [CrossRef]
- Rana, K.; Page, A.; Kent, J.L.; Arora, A. Pathways Linking Housing Inequalities and Health Outcomes Among Migrant and Refugee Populations in High-Income Countries: A Protocol for a Mixed-Methods Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16627. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, F. Built environment and obesity by urbanicity in the US. Health Place 2015, 34, 19–29. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological Models of Health Behavior. In Health Behavior: Theory, Research, and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2015; Volume 5. [Google Scholar]
- Rother, E.T. Systematic literature review X narrative review. Acta Paul. Enferm. 2007, 20, v–vi. [Google Scholar] [CrossRef]
- Qasim, A.; Turcotte, M.; de Souza, R.J.; Samaan, M.C.; Champredon, D.; Dushoff, J.; Speakman, J.R.; Meyre, D. On the origin of obesity: Identifying the biological, environmental and cultural drivers of genetic risk among human populations. Obes. Rev. 2018, 19, 121–149. [Google Scholar] [CrossRef]
- Ohri-Vachaspati, P.; DeLia, D.; DeWeese, R.S.; Crespo, N.C.; Todd, M.; Yedidia, M.J. The Relative Contribution of Layers of the Social Ecological Model to Childhood Obesity. Public Health Nutr. 2015, 18, 2055–2066. [Google Scholar] [CrossRef]
- Lee, B.Y.; Bartsch, S.M.; Mui, Y.; Haidari, L.A.; Spiker, M.L.; Gittelsohn, J. A systems approach to obesity. Nutr. Rev. 2017, 75, 94–106. [Google Scholar] [CrossRef]
- Serrano-Fuentes, N.; Rogers, A.; Portillo, M.C. Beyond individual responsibility: Exploring lay understandings of the contribution of environments on personal trajectories of obesity. PLoS ONE 2024, 19, e0302927. [Google Scholar] [CrossRef]
- Martín Moya, R.; Ruiz Montero, P.J.; Rivera García, E. Personal barriers to physical practice by older adults in different socio-economic locations: A qualitative study. J. Gerontol. Geriatr. 2022, 70, 244–252. [Google Scholar] [CrossRef]
- Eime, R.M.; Charity, M.J.; Harvey, J.T.; Payne, W.R. Participation in sport and physical activity: Associations with socio-economic status and geographical remoteness. BMC Public Health 2015, 15, 434. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L. Physical activity in relation to urban environments in 14 cities worldwide: A cross-sectional study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.D.; Donley, A.M.; Gualtieri, M.C.; Strickhouser, S.M. Food Deserts: What is the Problem? What is the Solution? Society 2016, 53, 171–181. [Google Scholar] [CrossRef]
- Shannon, J. Beyond the supermarket solution: Linking food deserts, neighborhood context, and everyday mobility. Ann. Am. Assoc. Geogr. 2016, 106, 186–202. [Google Scholar] [CrossRef]
- Giskes, K.; Kamphuis, C.B.M.; van Lenthe, F.J.; Kremers, S.; Droomers, M.; Brug, J. A systematic review of associations between environmental factors, energy and fat intakes among adults: Is there evidence for environments that encourage obesogenic dietary intakes? Public Health Nutr. 2007, 10, 1005–1017. [Google Scholar] [CrossRef]
- Zhang, H.; Yin, L. A meta-analysis of the literature on the association of the social and built environment with obesity: Identifying factors in need of more in-depth research. Am. J. Health Promot. 2019, 33, 792–805. [Google Scholar] [CrossRef]
- Baobeid, A.; Koç, M.; Al-Ghamdi, S.G. Walkability and its relationships with health, sustainability, and livability: Elements of physical environment and evaluation frameworks. Front. Built Environ. 2021, 7, 721218. [Google Scholar] [CrossRef]
- Sallis, J.; Bauman, A.; Pratt, M. Environmental and policy interventions to promote physical activity. Am. J. Prev. Med. 1998, 15, 379–397. [Google Scholar] [CrossRef]
- Rana, K.; Pandey, S.R.; Chimoriya, R. The Influence of Greenspace on Obesity: An Umbrella Systematic Review. Obes. Res. Clin. Pract. 2024, 18, S48. [Google Scholar] [CrossRef]
- Sallis, J.F.; Floyd, M.F.; Rodríguez, D.A.; Saelens, B.E. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012, 125, 729–737. [Google Scholar] [CrossRef]
- Huang, T.T.; Drewnosksi, A.; Kumanyika, S.; Glass, T.A. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev. Chronic. Dis. 2009, 6, A82. [Google Scholar]
- Cohen, D.A.; Han, B.; Isacoff, J.; Shulaker, B.; Williamson, S.; Marsh, T.; McKenzie, T.L.; Weir, M.; Bhatia, R. Impact of park renovations on park use and park-based physical activity. J. Phys. Act. Health 2015, 12, 289–295. [Google Scholar] [CrossRef]
- Cummins, S.; Flint, E.; Matthews, S.A. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014, 33, 283–291. [Google Scholar] [CrossRef]
- Odoms-Young, A.; Brown, A.G.M.; Agurs-Collins, T.; Glanz, K. Food Insecurity, Neighborhood Food Environment, and Health Disparities: State of the Science, Research Gaps and Opportunities. Am. J. Clin. Nutr. 2024, 119, 850–861. [Google Scholar] [CrossRef]
- Lovasi, G.S.; Hutson, M.A.; Guerra, M.; Neckerman, K.M. Built Environments and Obesity in Disadvantaged Populations. Epidemiol. Rev. 2009, 31, 7–20. [Google Scholar] [CrossRef]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place 2010, 16, 876–884. [Google Scholar] [CrossRef]
- North American Association for the Study of Obesity; National Heart, Lung, and Blood Institute; National Institutes of Health (USA); NHLBI Obesity Education Initiative. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; University of Michigan Library: Ann Arbor, MI, USA, 2002. [Google Scholar]
- Minkler, M. Linking science and policy through community-based participatory research to study and address health disparities. Am. J. Public Health 2010, 100 (Suppl. S1), S81–S87. [Google Scholar] [CrossRef]
- Rigolon, A. A complex landscape of inequity in access to urban parks: A literature review. Landsc. Urban Plan. 2016, 153, 160–169. [Google Scholar] [CrossRef]
- Evans, G.W. The built environment and mental health. J. Urban Health 2003, 80, 536–555. [Google Scholar] [CrossRef]
- Frank, L.D.; Sallis, J.F.; Conway, T.L.; Chapman, J.E.; Saelens, B.E.; Bachman, W. Many Pathways from Land Use to Health: Associations between Neighborhood Walkability and Active Transportation, Body Mass Index, and Air Quality. J. Am. Plan. Assoc. 2006, 72, 75–87. [Google Scholar] [CrossRef]
- Swinburn, B.; Egger, G.; Raza, F. Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity. Prev. Med. 1999, 29, 563–570. [Google Scholar] [CrossRef]
- Rana, K.; Shrestha, V.; Chimoriya, R. The effect of housing on health and challenges of demographic changes. Glob. J. Sci. Front. Res. 2020, 20, 75–82. [Google Scholar]
- Rana, K.; Kent, J.L.; Page, A. Housing inequalities and health outcomes among migrant and refugee populations in high-income countries: A mixed-methods systematic review. BMC Public Health 2025, 25, 1098. [Google Scholar] [CrossRef]
- Garg, R.; McQueen, A.; Wolff, J.M.; Skinner, K.E.; Kegler, M.C.; Kreuter, M.W. Low housing quality, unmet social needs, stress and depression among low-income smokers. Prev. Med. Rep. 2022, 27, 101767. [Google Scholar] [CrossRef]
- Bowen, D.J.; Quintiliani, L.M.; Bhosrekar, S.G.; Goodman, R.; Smith, E. Changing the housing environment to reduce obesity in public housing residents: A cluster randomized trial. BMC Public Health 2018, 18, 883. [Google Scholar] [CrossRef]
- Hope, J. A Review of the Mechanism of Injury and Treatment Approaches for Illness Resulting from Exposure to Water—Damaged Buildings, Mold, and Mycotoxins. Sci. World J. 2013, 2013, 767482. [Google Scholar] [CrossRef]
- Pasquali, R. The hypothalamic–pituitary–adrenal axis and sex hormones in chronic stress and obesity: Pathophysiological and clinical aspects. Ann. N. Y. Acad. Sci. 2012, 1264, 20–35. [Google Scholar] [CrossRef]
- Lucassen, E.A.; Cizza, G. The hypothalamic-pituitary-adrenal axis, obesity, and chronic stress exposure: Sleep and the HPA axis in obesity. Curr. Obes. Rep. 2012, 1, 208–215. [Google Scholar] [CrossRef]
- Münzel, T.; Sørensen, M.; Gori, T.; Schmidt, F.P.; Rao, X.; Brook, J.; Chen, L.C.; Brook, R.D.; Rajagopalan, S. Environmental Stressors and Cardio-Metabolic Disease: Part I—Epidemiologic Evidence Supporting a Role for Noise and Air Pollution and Effects of Mitigation Strategies. Eur. Heart J. 2017, 38, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Chimed-Ochir, O.; Ikaga, T.; Ando, S.; Ishimaru, T.; Kubo, T.; Murakami, S.; Fujino, Y. Effect of housing condition on quality of life. Indoor Air 2021, 31, 1029–1037. [Google Scholar] [CrossRef]
- Schmid, S.M.; Hallschmid, M.; Jauch-Chara, K.; Born, J.; Schultes, B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J. Sleep. Res. 2008, 17, 331–334. [Google Scholar] [CrossRef]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Zhang, Y.; van Dijk, T.; Wagenaar, C. How the Built Environment Promotes Residents’ Physical Activity: The Importance of a Holistic People-Centered Perspective. Int. J. Environ. Res. Public Health 2022, 19, 5595. [Google Scholar] [CrossRef]
- Hume, C.; Grieger, J.A.; Kalamkarian, A.; D’Onise, K.; Smithers, L.G. Community gardens and their effects on diet, health, psychosocial and community outcomes: A systematic review. BMC Public Health 2022, 22, 1247. [Google Scholar] [CrossRef]
- Rana, K. Towards passive design strategies for improving thermal comfort performance in a naturally ventilated residence. J. Sustain. Archit. Civ. Eng. 2021, 29, 150–174. [Google Scholar] [CrossRef]
- Evans, G.W.; Wells, N.M.; Moch, A. Housing and mental health: A review of the evidence and a methodological and conceptual critique. J. Soc. Issues 2003, 59, 475–500. [Google Scholar] [CrossRef]
- Singh, A.; Daniel, L.; Baker, E.; Bentley, R. Housing disadvantage and poor mental health: A systematic review. Am. J. Prev. Med. 2019, 57, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Baum, A.; Davis, G.E. Reducing the stress of high-density living: An architectural intervention. J. Personal. Soc. Psychol. 1980, 38, 471. [Google Scholar] [CrossRef] [PubMed]
- Saelens, B.E.; Handy, S.L. Built environment correlates of walking: A review. Med. Sci. Sports Exerc. 2008, 40, S550–S566. [Google Scholar] [CrossRef] [PubMed]
- Devarajan, R.; Prabhakaran, D.; Goenka, S. Built environment for physical activity—An urban barometer, surveillance, and monitoring. Obes. Rev. 2020, 21, e12938. [Google Scholar] [CrossRef]
- Herrington, S.; Brussoni, M. Beyond physical activity: The importance of play and nature-based play spaces for children’s health and development. Curr. Obes. Rep. 2015, 4, 477–483. [Google Scholar] [CrossRef]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef]
- Raman, S. Designing a liveable compact city: Physical forms of city and social life in urban neighbourhoods. Built Environ. 2010, 36, 63–80. [Google Scholar] [CrossRef]
- Nuworsoo, C.; Cooper, E.; Cushing, K.; Jud, E. Integration of Bicycling and Walking Facilities into the Infrastructure of Urban Communities. In Mineta Transportation Institute Report 11-05; Mineta Transportation Institute: San José, CA, USA, 2012. [Google Scholar]
- Durand, C.P.; Andalib, M.; Dunton, G.F.; Wolch, J.; Pentz, M.A. A systematic review of built environment factors related to physical activity and obesity risk: Implications for smart growth urban planning. Obes. Rev. 2011, 12, e173–e182. [Google Scholar] [CrossRef]
- Sallis, J.F.; Glanz, K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006, 16, 89–108. [Google Scholar] [CrossRef] [PubMed]
- Bancroft, C.; Joshi, S.; Rundle, A.; Hutson, M.; Chong, C.; Weiss, C.C.; Genkinger, J.; Neckerman, K.; Lovasi, G. Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Soc. Sci. Med. 2015, 138, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Chimoriya, R.; MacMillan, F.; Lean, M.; Simmons, D.; Piya, M.K. A qualitative study of the perceptions and experiences of participants and healthcare professionals in the DiRECT-Australia type 2 diabetes remission service. Diabet. Med. 2024, 41, e15301. [Google Scholar] [CrossRef] [PubMed]
- Arora, A.; Rana, K.; Manohar, N.; Li, L.; Bhole, S.; Chimoriya, R. Perceptions and Practices of Oral Health Care Professionals in Preventing and Managing Childhood Obesity. Nutrients 2022, 14, 1809. [Google Scholar] [CrossRef]
- Atlantis, E.; Chimoriya, R.; Seifu, C.N.; Peters, K.; Murphy, G.; Carr, B.; Lim, D.; Fahey, P. Enablers and barriers to implementing obesity assessments in clinical practice: A rapid mixed-methods systematic review. BMJ Open 2022, 12, e063659. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Bartlett, S.J. Access and Use of Medical Care Among Obese Persons. Obes. Res. 2000, 8, 403–406. [Google Scholar] [CrossRef]
- Wiig Dammann, K.; Smith, C. Factors Affecting Low-income Women’s Food Choices and the Perceived Impact of Dietary Intake and Socioeconomic Status on Their Health and Weight. J. Nutr. Educ. Behav. 2009, 41, 242–253. [Google Scholar] [CrossRef]
- Ravikumar, D.; Spyreli, E.; Woodside, J.; McKinley, M.; Kelly, C. Parental perceptions of the food environment and their influence on food decisions among low-income families: A rapid review of qualitative evidence. BMC Public Health 2022, 22, 9. [Google Scholar] [CrossRef]
- Hesketh, K.R.; Lakshman, R.; van Sluijs, E.M.F. Barriers and facilitators to young children’s physical activity and sedentary behaviour: A systematic review and synthesis of qualitative literature. Obes. Rev. 2017, 18, 987–1017. [Google Scholar] [CrossRef] [PubMed]
- Tam-Seto, L.; Weir, P.; Dogra, S. Factors Influencing Sedentary Behaviour in Older Adults: An Ecological Approach. AIMS Public Health 2016, 3, 555–572. [Google Scholar] [CrossRef] [PubMed]
- Chrisinger, B.W. Taking Stock of New Supermarkets in Food Deserts: Patterns in Development, Financing, and Health Promotion. Work. Pap. 2016, 2016, 4. [Google Scholar]
- Hunter, R.F.; Christian, H.; Veitch, J.; Astell-Burt, T.; Hipp, J.A.; Schipperijn, J. The impact of interventions to promote physical activity in urban green space: A systematic review and recommendations for future research. Soc. Sci. Med. 2015, 124, 246–256. [Google Scholar] [CrossRef]
- Lee, R.J.; Sener, I.N.; Jones, S.N. Understanding the role of equity in active transportation planning in the United States. Transp. Rev. 2017, 37, 211–226. [Google Scholar] [CrossRef]
- Nwana, N.; Javed, Z.; Jones, S.L.; Lee, C.; Maddock, J.E.; Al-Kindi, S.; Nasir, K. Green Streets, Healthy Hearts: Exploring the Roles of Urban Nature and Walkability in Cardiovascular Health. Methodist Debakey Cardiovasc. J. 2024, 20, 37–46. [Google Scholar] [CrossRef]
- Brown, B.B.; Yamada, I.; Smith, K.R.; Zick, C.D.; Kowaleski-Jones, L.; Fan, J.X. Mixed land use and walkability: Variations in land use measures and relationships with BMI, overweight, and obesity. Health Place 2009, 15, 1130–1141. [Google Scholar] [CrossRef]
- Besser, L.M.; Dannenberg, A.L. Walking to Public Transit: Steps to Help Meet Physical Activity Recommendations. Am. J. Prev. Med. 2005, 29, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Creatore, M.I.; Glazier, R.H.; Moineddin, R.; Fazli, G.S.; Johns, A.; Gozdyra, P.; Matheson, F.I.; Kaufman-Shriqui, V.; Rosella, L.C.; Manuel, D.G.; et al. Association of Neighborhood Walkability with Change in Overweight, Obesity, and Diabetes. JAMA 2016, 315, 2211–2220. [Google Scholar] [CrossRef]
- Stangierska, D.; Fornal-Pieniak, B.; Szumigała, P.; Widera, K.; Żarska, B.; Szumigała, K. Green Physical Activity Indicator: Health, Physical Activity and Spending Time Outdoors Related to Residents Preference for Greenery. Int. J. Environ. Res. Public Health 2023, 20, 1242. [Google Scholar] [CrossRef]
- Deka, D.; Brown, C.T.; Sinclair, J. Exploration of the effect of violent crime on recreational and transportation walking by path and structural equation models. Health Place 2018, 52, 34–45. [Google Scholar] [CrossRef]
- Nobari, T.Z.; Whaley, S.E.; Blumenberg, E.; Prelip, M.L.; Wang, M.C. Severe housing-cost burden and obesity among preschool-aged low-income children in Los Angeles County. Prev. Med. Rep. 2019, 13, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.L.; Miake-Lye, I.M.; Begashaw, M.M.; Zimmerman, F.J.; Larkin, J.; McGrath, E.L.; Shekelle, P.G. Association of Promoting Housing Affordability and Stability with Improved Health Outcomes: A Systematic Review. JAMA Netw. Open 2022, 5, e2239860. [Google Scholar] [CrossRef]
- Schuler, B.R.; Shipe, S.L.; O’Reilly, N.; Uhl, A.; Vazquez, C.E.; Tripicchio, G.L.; Hernandez, D.C. Balancing Nutrition and Budgets: Socio-Ecological Impacts on Nutritional Environments of Families with Low Incomes. Appetite 2024, 203, 107706. [Google Scholar] [CrossRef]
- Glover, T.D.; Todd, J.; Moyer, L. Neighborhood Walking and Social Connectedness. Front. Sports Act Living 2022, 4, 825224. [Google Scholar] [CrossRef]
- Henderson, H.; Child, S.; Moore, S.; Moore, J.B.; Kaczynski, A.T. The Influence of Neighborhood Aesthetics, Safety, and Social Cohesion on Perceived Stress in Disadvantaged Communities. Am. J. Community Psychol. 2016, 58, 80–88. [Google Scholar] [CrossRef]
- Wang, S.-C.; Fowler, P.J. Social Cohesion, Neighborhood Collective Efficacy, and Adolescent Subjective Well-Being in Urban and Rural Taiwan. Am. J. Community Psychol. 2019, 63, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. AN ECOLOGICAL APPROACH TO CREATING ACTIVE LIVING COMMUNITIES. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; O’Fallon, L.R.; Dearry, A. Creating Healthy Communities, Healthy Homes, Healthy People: Initiating a Research Agenda on the Built Environment and Public Health. Am. J. Public Health 2003, 93, 1446–1450. [Google Scholar] [CrossRef]
- Rana, K.; Aitken, S.J.; Chimoriya, R. Interdisciplinary Approaches in Doctoral and Higher Research Education: An Integrative Scoping Review. Educ. Sci. 2025, 15, 72. [Google Scholar] [CrossRef]
- Nesshöver, C.; Assmuth, T.; Irvine, K.N.; Rusch, G.M.; Waylen, K.A.; Delbaere, B.; Haase, D.; Jones-Walters, L.; Keune, H.; Kovacs, E.; et al. The science, policy and practice of nature-based solutions: An interdisciplinary perspective. Sci. Total Environ. 2017, 579, 1215–1227. [Google Scholar] [CrossRef]
- Bibri, S.E. The core academic and scientific disciplines underlying data-driven smart sustainable urbanism: An interdisciplinary and transdisciplinary framework. Comput. Urban Sci. 2021, 1, 1. [Google Scholar] [CrossRef]
- Gates, S.G. The Limits of Conditionality: An Examination of Individual Incentives and Structural Constraints. Ph.D. Thesis, University of Michigan, Ann Arbor, MI, USA, 1989. [Google Scholar]
- Kraak, V.; Englund, T.; Misyak, S.; Serrano, E.L. A novel marketing mix and choice architecture framework to nudge restaurant customers toward healthy food environments to reduce obesity in the United States. Obes. Rev. 2017, 18, 852–868. [Google Scholar] [CrossRef]
- Kaiser, L.; Martinez, J.; Horowitz, M.; Lamp, C.; Johns, M.; Espinoza, D.; Byrnes, M.; Gomez, M.M.; Aguilera, A.; de la Torre, A. Adaptation of a culturally relevant nutrition and physical activity program for low-income, Mexican-origin parents with young children. Prev. Chronic Dis. 2015, 12, E72. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, D.; Janke, R.; Barry, J.; Cloherty, A.; Shahram, S.Z.; Jones, C.A. Learning from “our relations” indigenous peoples of Australia, Canada, New Zealand, and United States: A review of culturally relevant diabetes and obesity interventions for health. Int. Indig. Policy J. 2022, 13, 1–35. [Google Scholar] [CrossRef]
- Gomes, S.M. Using Community-Engaged Research to Increase Food Literacy and Food Security in Local Communities. Ph.D. Thesis, University of Cincinnati, Cincinnati, OH, USA, 2024. [Google Scholar]
- Kumanyika, S.K. A framework for increasing equity impact in obesity prevention. Am. J. Public Health 2019, 109, 1350–1357. [Google Scholar] [CrossRef]
- Kumanyika, S.K. Advancing health equity efforts to reduce obesity: Changing the course. Annu. Rev. Nutr. 2022, 42, 453–480. [Google Scholar] [CrossRef] [PubMed]
- Bombak, A. Obesity, health at every size, and public health policy. Am. J. Public Health 2014, 104, e60–e67. [Google Scholar] [CrossRef]
- Rana, K.; Chimoriya, R. A Guide to a Mixed-Methods Approach to Healthcare Research. Encyclopedia 2025, 5, 51. [Google Scholar] [CrossRef]
- Elgaard Jensen, T.; Kleberg Hansen, A.K.; Ulijaszek, S.; Munk, A.K.; Madsen, A.K.; Hillersdal, L.; Jespersen, A.P. Identifying notions of environment in obesity research using a mixed-methods approach. Obes. Rev. 2019, 20, 621–630. [Google Scholar] [CrossRef] [PubMed]
| Housing Domains | Mechanisms Influencing Obesity | Key Risk Factors |
|---|---|---|
| Housing Quality | Poor insulation, dampness, pests, crowding lead to stress, disrupted sleep, and reduced physical activity | Chronic stress, poor sleep, mental health problems, sedentary lifestyle |
| Housing Design | Lack of outdoor space, poorly lit or cramped interiors limit physical activity | Low physical activity, sedentary behavior |
| Housing Location | Location affects access to parks, healthy food, and exposure to pollution | Food deserts, activity deserts, air/noise pollution |
| Neighborhood Walkability | Pedestrian infrastructure, mixed-use design influences active transport and recreation | Reliance on cars, lack of daily walking |
| Housing Affordability | High costs limit spending on healthy food and exercise; financial stress drives emotional eating | Unhealthy diets, emotional eating, lack of recreation |
| Social Environment | Strong social networks encourage activity and healthy eating; disorganized areas discourage participation | Isolation, low trust, crime exposure, reduced motivation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rana, K.; Chimoriya, R. Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity. Obesities 2025, 5, 64. https://doi.org/10.3390/obesities5030064
Rana K, Chimoriya R. Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity. Obesities. 2025; 5(3):64. https://doi.org/10.3390/obesities5030064
Chicago/Turabian StyleRana, Kritika, and Ritesh Chimoriya. 2025. "Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity" Obesities 5, no. 3: 64. https://doi.org/10.3390/obesities5030064
APA StyleRana, K., & Chimoriya, R. (2025). Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity. Obesities, 5(3), 64. https://doi.org/10.3390/obesities5030064







