Abstract
Non-traditional settings, such as schools, early childhood education programs, and healthcare clinics, can play a critical role in preventing obesity by providing free and nutritious food outside of food pantries to households that are experiencing low or very low food security, particularly during emergency situations. This evaluation study describes a low-income population that attended free food and produce distribution events during the COVID-19 pandemic. In 2021, a cross-sectional survey was administered to this group (n = 1498) to assess their food security status, fruit and vegetable (F+V) consumption, and prevalence of chronic disease condition(s). Program and event assessments were carried out using descriptive, bivariate, and multivariable logistic regression analyses. More than a quarter (26%) of the participants attended the free food events for the first time. Approximately 70% reported some level of low food security, 57% to 64% did not meet F+V intake recommendations, and 37% had a diet-related chronic disease condition. In the adjusted models, households with very low food security had lower odds of meeting F+V recommendations (aOR, 0.41, 95% CI, 0.28, 0.58 and aOR, 0.27, 95% CI, 0.19, 0.39, respectively) and higher odds of having a chronic condition (aOR, 3.49, 95% CI, 2.34, 5.20) than those with high or marginal food security. Given these experiences, future research should examine how safety net food assistance programs can incorporate alternative service/distribution models to improve the nutritional value of the foods they offer.
1. Introduction
Among the more pronounced socioeconomic and health impacts of the coronavirus disease 2019 (COVID-19) pandemic has been the disruption of the United States (US) food system, which has, in turn, contributed to decreased availability of affordable foods and limited access to healthy food [1]. All of which contributes to heightened experiences of food insecurity for low-income people and those with chronic conditions such as diabetes, high blood pressure, and obesity. According to the United States Department of Agriculture (USDA), food insecurity is a “household-level economic and social condition of limited or uncertain access to adequate food” [2]. About 13.8 million or 10.5% of US households experienced this condition at some point in 2020—this was unchanged from 2019 [3]. Recent projections by organizations such as Feeding America suggest a similar pattern for 2021, with this prevalence not likely to decline in 2022 or beyond, even as the pandemic gradually transitions to endemicity [4].
Federal nutrition assistance programs and local programmatic efforts have worked to address food insecurity primarily as it relates to hunger and to ensuring populations have access to sufficient calories. Charitable, emergency-based approaches have been a critical element in providing an immediate solution for emergency food needs, as seen throughout the COVID-19 pandemic. However, alternative food program strategies, such as community gardens, farmer’s markets, food procurement policies, and/or redistribution of surplus food to households in need, especially at free food events, have evolved into a practical intervention for providing healthier food options that are nutritionally and ecologically sustainable [5,6]. This evolution in strategy is in part driven by a growing recognition that preventing obesity and related chronic conditions requires addressing these conditions as well as food insecurity/hunger at more upstream levels [5,6,7,8]. In recent years, national investments in these alternative program strategies, which includes policy, systems, and environmental change interventions (PSEs), have increased and have become a larger part of several federal agencies’ portfolios, including for the USDA [9] and the Centers for Disease Control and Prevention [10].
An alternative program strategy that has garnered increased attention recently has been the coupling of nutrition education to food distribution of food (e.g., fresh produce) to food insecure households at free food events at community sites [11]. This approach is best exemplified by a growing network of partnerships that the Los Angeles County Department of Public Health (DPH) has built to work with various sectors outside of the emergency food system to redistribute free food and surplus produce to households with low income in Los Angeles County (LAC). The effort is supported in part by the region’s Supplemental Nutrition Assistance Program Education (SNAP-Ed) program, which focuses on increasing fruit and vegetable (F+V) intake among underserved communities as part of a broader effort to improve food and nutrition security in the region.
The first goal of this strategy is based on established evidence that F+V intake is an important component of a balanced diet, a critical behavioral action that drives good health; i.e., higher intake of F+V is associated with favorable outcomes in obesity and chronic disease prevention [12]. In the US, increasing F+V intake has been a difficult undertaking for public health. For example, while 1 in 10 US adults met the current F+V recommendations in 2019, as outlined in the 2020–2025 Dietary Guidelines for Americans (DGA), only 6.8% with a lower income met the vegetable recommendation [13,14]. Locally in LAC, low-income households fared no better: 28% frequently were unable to find affordable, fresh F+V [15], and a large percentage of them had a concomitant cardiometabolic condition that puts them at risk of poor health outcomes—17.0% had diabetes, 30.4% had hypertension, and 30.4% had high cholesterol [16].
The second goal of the strategy is grounded in the growing acceptance that the quality of food matters to health maintenance and to the prevention of chronic conditions such as prediabetes, diabetes, high blood pressure, and obesity. One possible way to achieve this goal is to provide or expand services in a manner so that services are tailored to meet the nutritional needs of clients (e.g., providing nutrient-dense items when the situation calls for it, offering culturally appropriate options when requested, or making age and health appropriate foods more available) [17]. This approach is not necessarily novel per se, as other innovative programs (e.g., produce prescription projects, healthy retail initiatives) have utilized a similar game plan to achieve the working concept of ‘nutrition security’ [18,19]. In the literature, ‘nutrition security’ is defined as “consistent access, availability, and affordability of foods and beverages that promote well-being and prevent (and if needed, treat) disease” [20,21].
The present study addresses these gaps in health promotion practice by describing a county-level nutrition education program in LAC that partnered with food pantries and community-based organizations to deliver food and free recovered produce to households with a lower income at selected community sites. The level of food security, F+V intake, and type(s) of chronic condition(s) were assessed using a cross-sectional 2021 survey administered to the food distribution program’s participants.
2. Methods
2.1. Context
In LAC, the USDA’s SNAP-Ed program, known in California as CalFresh Healthy Living, works to increase access to healthy foods for eligible populations who are at or below 185% of the Federal Poverty Level by hosting free food and produce distribution events (hereafter free food events) at their partner community sites several times per month. Beginning in 2020, DPH partnered with 18 community-based agencies to deliver nutrition education and implement various PSE strategies. Nine partner agencies, including two food banks/pantries, three public school districts, one early childhood education center, and three healthcare systems, distributed free food to families and patients at various locations throughout the county.
Using a network of community-based organizations and food rescue organizations, community sites regularly distributed recovered, edible produce (>1 time per month). During February to June 2021, the local SNAP-Ed program hosted 290 events, served 92,190 people, and distributed 1,377,395 pounds of recovered produce. Due to the COVID-19 pandemic, all food that was distributed was pre-boxed or pre-bagged to limit contact among participants. The number of bags or boxes distributed to each participant were often based on household size (e.g., larger households could receive more produce). An estimated 46 varieties of fruits and 72 varieties of vegetables were distributed at the events. During these events, nutrition education and messaging were also made available to participants, including but not limited to distributing cookbooks on how to utilize the items in the box or bag, suggesting ways to reduce sugar consumption, and having pop-up banners to reinforce health messaging. Participants were also given the opportunity to attend virtual nutrition education classes that were designed to increase knowledge and awareness of healthy eating and active living. Figure 1 shows a photo of an event during one of these food distribution efforts.

Figure 1.
Health educators participating in an event providing bilingual cookbooks, recipe cards, and informational nutrition handouts to accompany fresh produce distribution.
2.2. Data Collection
Survey participants were adults ages 18 years and older who attended a LAC SNAP-Ed food distribution event at 1 of the 46 sites across the nine partner agencies between February and June 2021. Sites included traditional food distribution locations, such as food pantries, and non-traditional food distribution sites, such as elementary and middle schools, early childhood education programs, and healthcare clinics. A pilot of the survey was completed in December 2020 at an elementary school site with 30 participants completing the survey online. The pilot helped confirm that the population in the lowest income bracket was being reached at an event, and since the survey needed to be completed online, that the intended participant pool had the required technology to complete the survey (e.g., cellphones, tablets).
Initially, participant recruitment for the survey was to be conducted on site and in person. However, due to the limitations posed by COVID-19, including the need to adhere to health and safety standards, this process was converted to a web-based approach using an online survey. Recruitment responsibilities were shifted to staff members at each site and recruitment strategies were tailored based on the site’s capacity for staffing, physical layout, and expected volume of clients. Among the methods employed for recruiting these participants included (a) a survey link and quick response (QR) code for the participants to scan using their own electronic device; and (b) placing promotional flyers into the free produce bags and/or sharing the flyer information verbally with people attending the free food events hosted by the nine partner agency sites. The flyers were also posted on school websites, via social media, and on A-Frame signs. They contained contact information comprising an email address and telephone number where prospective participants could request technical assistance to help complete the survey. For two of the clinic agencies, clinic staff were able to send text messages to promote the survey. All participants received a USD 5 gift card after completing the online questionnaire.
The survey inclusion criteria were (a) a resident of LAC; (b) age 18 years and older; and (c) willing and able to complete the survey in one of the offered languages (English, Spanish, Chinese, Korean). The survey questionnaire was self-administered via Qualtrics, an online survey platform; this platform yielded a completion rate of 91.7%. A paper version was also available if the participant did not have access to an electronic device (completion rate was 8.0% for this format). Informed consent was obtained from all participants prior to survey administration. The survey questionnaire consisted of 45 questions that were compiled by Harder and Company Community Research; the group also consulted with and obtained input from DPH’s Nutrition and Physical Activity Program. Questions were based on previously validated and published scales. They included assessments of household food security status, the number and type(s) of chronic disease condition(s), history or current participation in public nutrition assistance programs, their satisfaction with the services they have received, and individual/household demographic information. In addition, there were three questions pertaining to study eligibility and one question about participation in a follow-up study.
Data collection was tracked in real time to ensure precision and fidelity. For example, several weeks into this process, a large and significant increase in survey completion was observed. Over several weeks, 30,746 surveys were noted to have been completed, but upon checking 29,248 of them were determined to be “invalid”. Another 132 participants who completed the surveys were also discovered to not meet the inclusion criteria based on the results of the eligibility screener. A participant’s survey was determined to be invalid if the IP address, email address, phone number, duplicate and fraud score, ReCaptcha score, and/or the agency name could not be verified or was found to be missing. All invalid surveys were subsequently excluded from the survey analyses. The final number of valid surveys was 1498. For the present evaluation study, only surveys from participants for which there were no missing values on any of the variables were used. In total, there were three survey samples based on the number of complete cases for each of the three dependent variables (fruit intake, n = 1086; vegetable intake, n = 1062; chronic condition, n = 1085).
2.3. Variables
The three dependent variables used in the study were constructed in the following manner. First, participants were asked to indicate how often “in the past 7 days including today, did you eat 2 cups of fruit a day?” Responses were categorized as meeting the adequate fruit intake recommendation if the participant ate 2 cups of fruit often (4–6 days) or every day. Second, a question on vegetable intake asked participants to indicate how often “in the past 7 days including today, did you eat 2 ½ cups of vegetable a day?” Responses were categorized as meeting the adequate vegetable intake recommendation if the participant consumed 2 ½ cups of vegetable often (4–6 days) or every day. The F+V intake recommendations were based on the 2020–2025 DGA for an adult with a 2000 average calorie diet [13]. Lastly, a question on diet-related chronic disease conditions asked participants, “Have you ever been diagnosed with any of the following? (select all that apply).” Participants were categorized as having a chronic condition if they marked yes to having any one of the following: high cholesterol, prediabetes or diabetes, high blood pressure, or heart disease; they were categorized as not having a chronic condition if they did not mark any of these conditions. The survey also collected participant responses on height and weight, which were used to calculate body mass index (BMI). Reported ranges of the BMI were then classified as underweight, normal weight, overweight, or obese, based on the Centers for Disease Control and Prevention’s cut-points [22].
The main independent variable used in the modeling analyses was household food security status, based on the short-form 6-item food security scale [23]. Items were summed and scored, and participating households were categorized as high or marginal food security, low food security, and very low food security. Study covariates included age (continuous variable), gender, race/ethnicity, educational attainment, SNAP participation, household size, site type where the survey was completed (traditional, non-traditional), and frequency of attending free food events.
2.4. Data Analysis
Bivariate analyses examined the relationships between household food security status and meeting the fruit intake recommendation, meeting the vegetable intake recommendation, and having any diet-related chronic condition. Multivariable logistic regression models were constructed to examine the associations between household food security status and the three dependent variables, controlling for age, gender, race/ethnicity, educational attainment, SNAP participation, household size, site type, frequency of attending free food events, and BMI. All statistical analyses were performed using Statistical Analysis Software (SAS, version 9.4) and Stata version 14. All program materials were reviewed and approved by the DPH Institutional Review Board prior to field implementation.
3. Results
The survey participant characteristics are shown in Table 1. Approximately two-thirds of the sample identified as female (59.4%), 30.3% as White, 33.8% as Hispanic/Latino, 15.4% had less than a high school diploma, and 30.7% participated in SNAP; 45.6% of the participants were overweight or obese. Among the participants, 64.2% did not meet the fruit intake recommendation and 56.9% did not meet the vegetable intake recommendation. Over a third of the sample (37.0%) had at least one of the listed chronic conditions (high cholesterol, prediabetes/diabetes, high blood pressure, or heart disease). Nearly 69.4% reported their household as having experienced some level of low or very low food security during the past 12 months.

Table 1.
Survey participant demographics and health-related characteristics, Los Angeles County, California, 2021 (n = 1498).
Across the 46 sites included in the sample, there was an even distribution of participants completing the survey at traditional and non-traditional sites (51.7% and 48.3%, respectively). When asked how often they attended free food events, 34.4% indicated they attended frequently (twice a month or weekly), while 26.3% indicated it was their first time attending this type of event.
Results of the bivariate analyses (Figure 2) showed that lower levels of household food security (higher food insecurity) were associated with lower levels of F+V intake and higher levels of any chronic condition. Among participants reporting very low food security, only 26.4% and 31.9% had an adequate F+V intake, respectively, and 47.1% had a chronic condition.
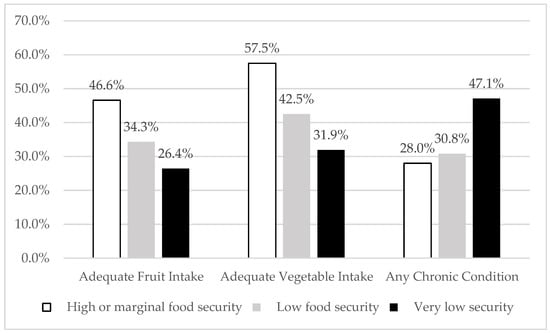
Figure 2.
Adequate fruit and vegetable intake and any chronic condition by food security status among participants who attended free food and produce distribution events in Los Angeles County, California, 2021.
After adjusting for covariates (Table 2), participants in households with very low food security had lower odds of meeting the fruit intake recommendation (adjusted Odds Ratio (aOR), 0.41, 95% confidence interval (CI), 0.28, 0.58, Model 1) and meeting the vegetable intake recommendation (aOR, 0.27, 95% CI, 0.19, 0.39, Model 2) as compared to participants in households with high or marginal food security. Participants in households with very low food security had higher odds of having a chronic condition than those with high or marginal food security (aOR, 3.49, 95% CI, 2.34, 5.20, Model 3) (Table 2).

Table 2.
Associations between food security and adequate fruit and vegetable intake and any chronic condition among participants who attended free food and produce distribution events in Los Angeles County, California, 2021.
Participants who identified as Hispanic/Latino, Black, and Asian all had lower odds of meeting adequate vegetable intake when compared to those who identified as White (Table 2). Participants who lived in households with five or more people had higher odds of both F+V intake relative to participants in households with 1–2 people. Participants who obtained food at non-traditional sites, including schools, early childhood education program sites, and healthcare clinics, had lower odds of meeting the fruit intake recommendation when compared to participants who obtained food at a traditional site (food pantry). Participants who were overweight or obese had higher odds of having any chronic condition (aOR 2.49, 95% CI, 1.82–3.40) compared to participants with a normal BMI.
4. Discussion
This study describes a sample of adults who attended free food events at food pantries, K-8 schools, early childhood education program sites, and healthcare clinics throughout LAC during the COVID-19 pandemic. During the time of the survey, nearly 300 free food events were held and 100,000 people received boxes or bags of food and produce. Across these sites, approximately 1.3 million pounds of free, recovered produce were distributed.
More than a quarter of the survey participants reported that at the time of the survey this was the first time they had attended a free food event. This suggests that the survey may have captured data on a group of people who could be accessing food due to the COVID-19 pandemic; i.e., as a result of the unforeseen economic need and the uncertainty that determined what food stores were actually open at the time [24]. Even prior to the pandemic, new and alternative food program strategies, such as the one described here, coexisted alongside charitable, emergency-based approaches [5,6]. However, many of these strategies presented unique barriers for low-income populations, including the perception that, at farmer’s markets, food assistance benefits are not accepted or that prices are too expensive [25].
This evaluation study is among the first to show that even in emergency situations, food pantries and community-based settings can and should play a critical role in providing free and nutritious food to households that are or have become food insecure due to a public health crisis. A unique aspect of the local SNAP-Ed program was that DPH facilitated partnerships between community-based organizations and community-based settings (K-8, early childhood education programs, and healthcare clinics) to distribute recovered surplus food and produce. Nutrition education and health messaging were also offered at these events—the education included distributing cookbooks and disseminating health messages using pop-up banners. Recognizing that F+V are perishable, and if such a choice/selection is made available at events, nutrition education can additionally help participants with their choices, potentially increasing their likelihood of purchasing and consuming more fresh produce. Another important dimension of the LAC effort is the distribution of food with staff and at sites that the program participants were familiar with and had interacted with on a regular basis. The addition of non-traditional sites complemented the work of the food pantries; they provided unique roles within the community relative to other food initiatives [26].
Approximately 70% of survey participants lived in households experiencing some level of low food security, and being food insecure was associated with not meeting F+V intake recommendations and having a diet-related chronic condition. Government programs such as SNAP, the National School Lunch Program, and the Special Supplemental Nutrition Program for Women, Infants, and Children have been critically important for reducing hunger and ensuring eligible population groups have access to food and adequate caloric intake. However, gaps remain in food access and availability of foods of higher nutritional value. A relatively recent study showed that SNAP participants experienced disparities in most components of a healthy diet and that these disparities have persisted over time when compared to income-eligible nonparticipants and higher income adults [27]. Other studies suggest that, in addition to food insecurity, more should be done to better identify and track the nutrition security of vulnerable populations, and the quality and nutrition of foods accessible to them [20,21]. SNAP-Ed and public health nutrition programs can play this important role by shaping local food environments so that nutrition security can be achieved equitably and effectively. The value of nutrition security could not be overstated, as microsimulation research has shown that interventions (most of them involving a nutrition focus) that can reduce a BMI by 0.5 could decrease the prevalence of diabetes and heart disease by 5.34% and 0.66%, respectively, in the population [28].
The present survey results also highlight the importance of offering nutritious food for groups at free food events, as 57% to 64% of participants did not meet F+V intake recommendations. About 37% had a diet-related chronic disease condition at the time of the survey: 14% with high cholesterol, 15% with prediabetes or diabetes, 15% with high blood pressure, and 6% with heart disease (also see Table 1). In 2018, the Los Angeles County Health Survey found that nearly a quarter of low-income adults from households experiencing food insecurity had hypertension and high cholesterol, and nearly 20% had diabetes [16]. This finding on chronic conditions is alarming, as chronic disease is strongly associated with severe COVID-19 illness, hospitalization, and death [29]. Frequently, as a household’s income declines, healthier items such as whole grains, fruits, and vegetables are replaced by lower cost and less healthy alternatives such as starch-heavy foods or items containing higher contents of vegetable fats and added sugars [30]. The high prevalence of participants with any chronic condition in the survey sample suggests that accessing free food events—an emerging area of nutrition and edible food recovery work—could become a scalable strategy for sourcing and distributing foods with higher nutritional value. Increasing access to these healthy foods can help make lifestyle changes much easier for those with existing chronic conditions such as obesity or diabetes. For example, in patients with type 2 diabetes, foods with a low glycemic index (such as lentils, legumes, and oats) and low carbohydrate diets have been shown to be effective for improving glycemic control [31]. Similarly, unsaturated fatty acids, vitamins, and bioactive compounds are increasingly being considered as adjunctive regimens for managing chronic disease [31].
Limitations and Strengths
The present survey (evaluation study) has several limitations and strengths. For instance, the data is cross-sectional; i.e., the survey was not able to capture data on whether or not F+V intake increased as a result of the free food events themselves. In addition, during data collection, the COVID-19 pandemic posed several challenges that altered the design; among them was the conversion of a planned in-person survey to a survey that utilized an online format. This conversion led to unexpected issues, including a very high volume of invalid completions, likely as a result of bots proliferating the survey responses. An online format may have also led to a decrease in the response and completion rates by expanding the pool of potential participants (i.e., a larger denominator relative to the numerator). Like most surveys, recall and social desirability biases were likely present in the data, which also may have affected data interpretation. Lastly, while the survey provided key insights into the benefits of having free food events to increase food access, it was not designed to demonstrate their impacts on health outcomes or behavioral change.
A significant strength of the study has been the data collected from non-traditional community sites that were delivering recovered produce (i.e., versus data only from traditional food pantry sites). In focusing on non-traditional sites, the study may have captured data on a group that were new to having this public health problem of low or very low food security, an emergency situation largely created by the COVID-19 pandemic. Moving forward, additional research using longitudinal data should be conducted to better assess and understand the health and social impacts of alternative food strategy programs such as the one described in this article.
5. Conclusions
At free food events held during the height of the COVID-19 pandemic, data showed that program participants experiencing low or very low food security struggled to meet F+V intake recommendations and generally had higher odds of having a diet-related chronic condition. As such, traditional and non-traditional agencies or other community organizations that distribute free food should consider adopting healthy nutrition standards to guide their offerings, providing food options that are of high nutritional quality that can help the recipients maintain their health and avoid chronic conditions such as obesity, prediabetes/diabetes, and high blood pressure. In LAC, the local public health department facilitated partnerships with food pantries and community-based organizations to increase access to F+Vs. Further research is needed to better understand how utilization of community-based organizations and sites that households are familiar with and that interact with regularly could become a model of practice on how best to increase people’s access to healthy and nutritious food in the community. This alternative program strategy to traditional nutrition education, or as a complement to it, could be leveraged to more efficiently promote well-being and to prevent obesity and related chronic conditions in the US.
Author Contributions
Conceptualization, J.C., D.S. and T.K.; methodology, A.R. and D.F.; formal analysis, P.S. and J.C.; writing—original draft preparation, P.S. and J.C.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This project was supported in part by a contract from the California Department of Public Health to the Los Angeles County Department of Public Health (#19-10328) for work related to the United States Department of Agriculture’s Supplemental Nutrition Assistance Program Education.
Institutional Review Board Statement
All program materials were reviewed and approved by the DPH Institutional Review Board (#2014-09-535) prior to field implementation.
Informed Consent Statement
Informed consent was obtained from all subjects who participated in the survey.
Data Availability Statement
The data presented in this article are not publicly accessible but are available on request from and with approval from the corresponding author.
Acknowledgments
The authors thank Lana Skylar and Bernadet Garcia-Silva from the Los Angeles County Department of Public Health, and Eva Maria Chavez, Veronica Awan, Carolina Mantilla, Diana McDonnell, Elizabeth Lev, and Joelle Greene from Harder and Company Community Research for their technical support of the project. The authors also thank the participating community-based organizations for their assistance with the survey data collection. The content and any views expressed in this article are those of the authors and do not represent the position(s) or viewpoint(s) of the affiliated agencies or organizations mentioned in the text.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Davis, K.; Downs, S.; Gephart, J. Towards food supply chain resilience to environmental shocks. Nat. Food 2021, 2, 54–65. [Google Scholar] [CrossRef]
- United States Department of Agriculture Economic Research Service. Definitions of Food Security. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/ (accessed on 4 May 2022).
- United States Department of Agriculture Economic Research Service. Food Security in the United States. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/key-statistics-graphics/ (accessed on 4 May 2022).
- Feeding America. The Impact of Coronavirus on Food Insecurity. Available online: https://www.feedingamerica.org/research/coronavirus-hunger-research (accessed on 4 May 2022).
- Duncan, J.; Claeys, P. Politicizing food security governance through participation: Opportunities and opposition. Food Secur. 2018, 10, 1411–1424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, S.B.; Edge, S.S.; Beatty, J.; Leatherdale, S.; Perlman, C.; Dean, J.; Ward, P.R.; Kirkpatrick, S.I. Challenges to evidence-based health promotion: A case study of a food security coalition in Ontario, Canada. Health Promot. Int. 2018, 33, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Kaphingst, K.M.; Robinson-O’Brien, R.; Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 2008, 29, 253–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuo, T. The varying effects of the food, built, and socioeconomic environment on BMI. Obesity 2020, 28, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Backman, D.; Kizer, K.W. Restructuring a state nutrition education and obesity prevention program: Implications of a local health department model for SNAP-Ed. J. Public Health Manag. Pract. 2017, 23, e28–e36. [Google Scholar] [CrossRef]
- Bunnell, R.; O’Neil, D.; Soler, R.; Payne, R.; Giles, W.H.; Collins, J.; Bauer, U.; Communities Putting Prevention to Work Program Group. Fifty communities putting prevention to work: Accelerating chronic disease prevention through policy, systems, and environmental change. J. Community Health 2012, 37, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- United Stated Department of Agriculture. “SNAP-Ed Evaluation Framework,” Food and Nutrition Services. 2016. Available online: https://snapedtoolkit.org/app/uploads/SNAP-EdEvaluationFramework.pdf (accessed on 3 August 2021).
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.-Y.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United States Department of Agriculture. Dietary Guidelines for Americans. Available online: https://www.dietaryguidelines.gov/ (accessed on 4 May 2022).
- Lee, S.; Moore, L.; Harris, D.; Blanck, H. Adults meeting fruit and vegetable intake recommendations—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cantor, J.; Cohen, D.A.; Caldwell, J.; Kuo, T. Neighborhood environments, SNAP-Ed eligibility, and health behaviors: An analysis of the California Health Interview Survey (CHIS). J. Urban Health 2020, 97, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Los Angeles County Department of Public Health. Food Insecurity in Los Angeles County before and During the COVID-19 Pandemic. Available online: http://ph.lacounty.gov/nut/media/nutrition-physical-activity-resources/LA_County_Food_Insecurity_Report_2021_508Compliant.pdf (accessed on 4 May 2022).
- Bazerghi, C.; McKay, F.; Dunn, M. The role of food banks in addressing food insecurity: A systematic review. J. Community Health 2016, 41, 732–740. [Google Scholar] [CrossRef] [PubMed]
- U.S. Centers for Disease Control and Prevention. Healthier Food Retail (HFR) Action Guide. Available online: https://www.cdc.gov/nccdphp/dnpao/state-local-programs/pdf/Healthier-Food-Retail-guide-full.pdf (accessed on 4 May 2022).
- GUSNIP NTAE Center. Nutrition Incentive Hub. Available online: https://www.nutritionincentivehub.org/ (accessed on 4 August 2022).
- Mozaffarian, D.; Fleischhacker, S.; Andres, J. Prioritizing nutrition security in the US. J. Am. Med. Assoc. 2021, 325, 1605. [Google Scholar] [CrossRef] [PubMed]
- Ingram, J. Nutrition security is more than food security. Nat. Food 2020, 1, 2. [Google Scholar] [CrossRef] [Green Version]
- United States Centers for Disease Control and Prevention. Defining Adult Overweight & Obesity. Available online: https://www.cdc.gov/obesity/basics/adult-defining.html#:~:text=If%20your%20BMI%20is%20less,%20falls%20within%20the%20obesity%20range (accessed on 4 May 2022).
- United States Department of Agriculture. Six-Item Short Form of the Food Security Survey Module. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/#six (accessed on 4 May 2022).
- Public Exchange, University of South California. Enough to Eat: The Impact of COVID-19 on Food Insecurity and the Food Environment in L.A. County April 2020–September 2021. Available online: https://publicexchange.usc.edu/wp-content/uploads/2021/10/Enough-to-Eat.pdf (accessed on 4 May 2022).
- Freedman, D.; Vaudrin, N.; Schneider, C.; Trapl, E.; Ohri-Vachaspati, P.; Taggart, M.; Cascio, A.; Walsh, C.; Floke, S. Systematic Review of Factors Influencing Farmers’ Market Use Overall and among Low-Income Populations. J. Acad. Nutr. Diet. 2016, 116, 1136–1155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edge, S.; Meyer, S. Pursuing dignified food security through novel collaborative governance initiatives: Perceived benefits, tensions and lessons learned. Soc. Sci. Med. 2019, 232, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Liu, J.; Rehm, C.; Wilde, P.; Mande, J.; Mozaffarian, D. Trends and disparities in diet quality among US adults by Supplemental Nutrition Assistance Program participation status. JAMA Netw. Open 2018, 1, e180237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell-Fritch, J.; Cohen, D.; Caldwell, J.; Kuo, T. Simulating the impact of health behavior interventions in the SNAP-Ed population. Prev. Med. Rep. 2020, 20, 101257. [Google Scholar] [CrossRef] [PubMed]
- Kompaniyets, L.; Pennington, A.F.; Goodman, A.B.; Rosenblum, H.G.; Belay, B.; Ko, J.Y.; Chevinsky, J.R.; Schieber, L.Z.; Summers, A.D.; Lavery, A.M.; et al. Underlying medical conditions and severe illness among 540,667 adults hospitalized with COVID-19, March 2020–March 2021. Prev. Chronic Dis. 2021, 18, 210123. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Eichelsdoerfer, P. Can low-income Americans afford a healthy diet? Nutr. Today 2009, 44, 246–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ojo, O. Nutrition and chronic conditions. Nutrients 2019, 11, 459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).