1. Introduction
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy of the upper limb, with an estimated prevalence of 3–5% in the general population and accounting for most peripheral nerve compression syndromes [
1].
Open carpal tunnel release (OCTR), which involves division of the transverse carpal ligament to decompress the median nerve, remains the standard surgical approach for CTS. Long-term follow-up studies have confirmed its efficacy: 88% of patients reported being completely or very satisfied, and 74% stated that their symptoms were completely resolved more than a decade postoperatively [
2].
However, the open approach is associated with several drawbacks, including scar tenderness, reduced grip strength, pillar pain, and a relatively longer recovery time, despite its overall effectiveness and a complication rate below 3% [
3].
In recent years, minimally invasive surgical alternatives have been developed, including endoscopic carpal tunnel release (ECTR) and, more recently, ultrasound-guided carpal tunnel release (UGCTR). UGCTR allows visualization and division of the transverse carpal ligament through a minimal incision under real-time sonographic guidance, minimizing trauma to surrounding tissues. Preliminary studies indicate that UGCTR leads to significant improvements in pain and function within the first postoperative week, suggesting faster recovery with efficacy comparable to open release [
4].
Recent economic evaluations have highlighted the cost-effectiveness of UGCTR compared with traditional surgical methods. For example, White et al. [
5] demonstrated that performing carpal tunnel release in a clinic setting under local anesthesia significantly reduced costs without compromising outcomes. Similarly, Ekhtiari et al. [
6] found that UGCTR had the lowest total costs and the highest quality-adjusted life years among the main surgical options. These findings suggest that UGCTR may provide not only clinical but also economic advantages.
Despite these promising results, the current literature on UGCTR remains limited, with most available studies consisting of small, single-center cohorts or non-comparative case series. Therefore, a more rigorous evaluation is warranted to assess the comparative safety and efficacy of UGCTR versus traditional open techniques in a broader clinical context.
This retrospective multicenter study aims to describe the clinical and functional outcomes of patients undergoing UGCTR. By collecting and analyzing real-world data across multiple centers, the study seeks to evaluate the feasibility, safety, and effectiveness of this minimally invasive technique in the routine management of carpal tunnel syndrome.
The primary objective was to evaluate each outcome measure and its change across the prespecified follow-up visits after UGCTR. As an exploratory aim, we assessed associations between clinical variables and recovery endpoints and we reported those associations that reached statistical significance.
2. Materials and Methods
2.1. Study Design and Setting
This was a retrospective, observational, multicenter study involving hand surgeons across multiple Italian centers. Data were collected from patients who underwent ultrasound-guided carpal tunnel release (UGCTR) between January 2012 and April 2025.
2.2. Inclusion and Exclusion Criteria
Patients were included if they met all of the following criteria: (1) clinical history and physical examination findings consistent with carpal tunnel syndrome (CTS); (2) positive electrodiagnostic testing confirming median nerve entrapment at the wrist; (3) persistent neurological symptoms lasting more than three months despite conservative treatment (e.g., nonsteroidal anti-inflammatory drugs, night-time wrist splinting, stretching exercises, and/or corticosteroid injections); and (4) adherence to scheduled postoperative follow-up visits at 1, 4, and 12 weeks. Patients who failed to attend the complete follow-up were excluded from the analysis.
Exclusion criteria were as follows: (1) recurrent CTS in patients with a history of prior surgical decompression; and (2) CTS secondary to non-idiopathic causes, such as post-traumatic deformities of the wrist or distal radius, or space-occupying lesions within the carpal tunnel (e.g., ganglion cysts, lipomas, or other masses).
2.3. Surgical Technique
All UGCTR procedures were performed in an outpatient setting. Each procedure was conducted by a single operator without assistance from nursing or anesthesiology staff. Local anesthesia was administered using the WALANT (Wide-Awake Local Anesthesia No Tourniquet) technique, typically involving lidocaine or mepivacaine combined with epinephrine at a 1:100,000 concentration.
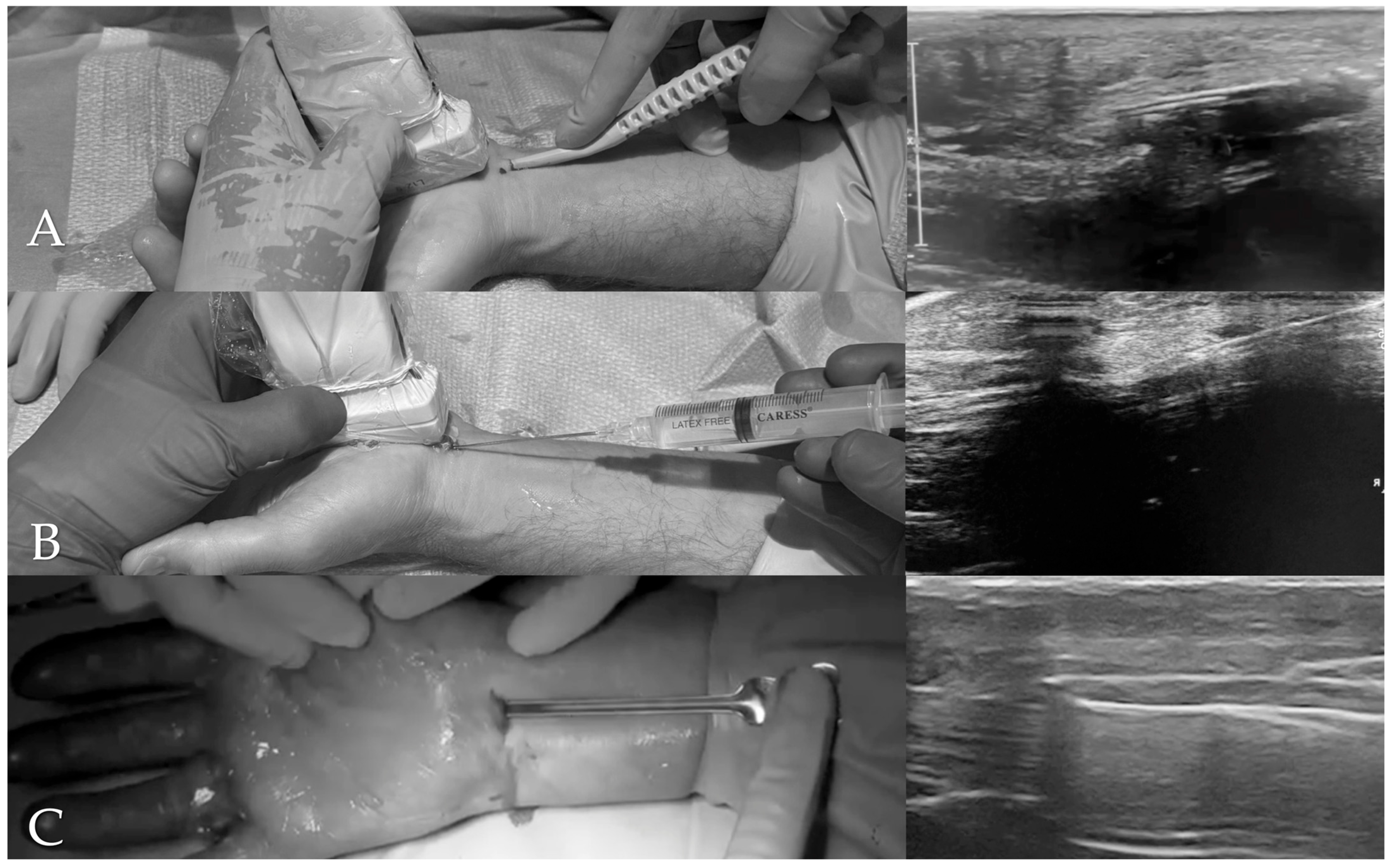
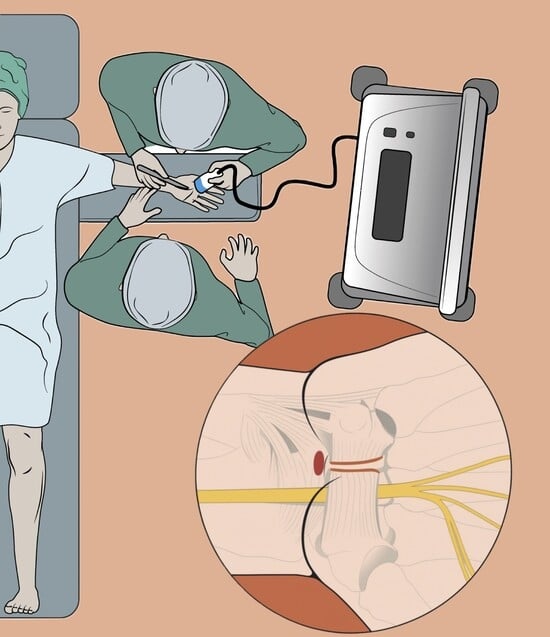
The procedures were performed using three ultrasound-guided techniques (
Figure 1): (1) a method employing the single-use Kemis
® H3 knife (Newclip Technics, Nantes, France); (2) the percutaneous needle release technique described by McShane et al. [
7]; and (3) the technique introduced by Dr. Brando and presented at the 2023 Congress of the Italian Society for Surgery of the Hand (SICM). Sterile draping consisted of a two-component system: a small drape placed between the arm table and the hand, and a large fenestrated drape secured to the forearm with adhesive to separate the surgical field from the patient.
In the Kemis® H3 knife technique, after identifying on ultrasound the median nerve, ulnar artery, and the distal landmarks of the transverse carpal ligament (TCL), a small incision was made proximal to the wrist crease. A mosquito forceps was first introduced above and below the TCL to define the plane, and the Kemis® H3 was then advanced under continuous ultrasound guidance, ensuring that the blade encompassed the entire ligament. The TCL was divided from proximal to distal, using Doppler to avoid vascular injury, and completeness of the release was confirmed on ultrasound.
In the McShane percutaneous needle release technique, through a single entry point at the proximal wrist crease, an 18-gauge spinal needle was introduced under continuous ultrasound control. The needle was advanced parallel to the median nerve, kept superficial and slightly ulnar to it, and repeatedly passed through the TCL to fenestrate the structure until the needle could pass freely, while carefully avoiding nerve and vascular injury.
In the Brando technique, a transverse entry point just ulnar to the palmaris longus tendon at the proximal wrist crease was used to access the carpal tunnel within the ultrasound-defined safe zone. A button-tipped probe was advanced beneath the TCL, confirming that it lay ulnar to the median nerve and superficial to the flexor tendons, and excluding superficial palmar arch involvement on power Doppler. A grooved director (slotted guide) was then advanced over the probe; the probe was removed, and a round-tipped microblade, oriented upward, was introduced. Advancing the blade from proximal to distal along the guide completed the release of the TCL, which was confirmed by supraretinacular migration of the guide.
Despite the technical differences, all approaches share the same principles: continuous ultrasound visualization to protect adjacent structures and confirmation of complete TCL release.
Wound closure varied by operator: one surgeon used a single absorbable suture (Vicryl Rapid®, Ethicon, Somerville, NJ, USA), while the other six applied adhesive skin-closure strips. After surgery, patients were observed for 30 min before discharge and were instructed to perform self-managed wound care, refrain from heavy manual activities for one week, and use over-the-counter analgesics (e.g., acetaminophen and/or ibuprofen) as needed.
2.4. Follow-Up and Outcome Measures
Postoperative follow-up visits were scheduled at 1, 4, and 12 weeks after the procedure. The following outcome measures were recorded:
Pain intensity, assessed using the Visual Analog Scale (VAS), ranging from 0 (no pain) to 10 (worst imaginable pain).
Functional and symptomatic status preoperatively and at 1 week postoperatively, assessed using the Boston Carpal Tunnel Questionnaire (BCTQ), which includes the Symptom Severity Scale (BCTQ-SS) and the Functional Status Scale (BCTQ-FS) [
8]. The Symptom Severity Scale comprises 11 items scored from 1 (no symptoms) to 5 (most severe), while the Functional Status Scale consists of 8 items scored from 1 (no difficulty) to 5 (unable to perform the activity). Higher scores indicate greater symptom severity and functional impairment.
Incidence of postoperative complications, defined as any surgery-related adverse event, including wound-related problems (infection, hematoma, delayed healing), neurological deficits (nerve injury, hypoesthesia), local tenderness or pillar pain, tendon-related issues, and recurrence or persistence of symptoms.
Time to return to daily activities (RDA).
Time to return to work (RTW).
Cross-sectional area (CSA) of the median nerve, measured by ultrasound at the carpal tunnel inlet (pisiform level) using the direct tracing method, assessed preoperatively and at 4 weeks postoperatively.
Since preoperative electrodiagnostic testing was conducted in multiple laboratories using heterogeneous reporting standards, the resulting values were not directly comparable across centers and were therefore excluded from the analysis.
Demographic variables collected included age, sex, and occupational status. Occupations were classified as white-collar (WC; low-load, predominantly non-manual roles such as office, administrative, or managerial work), blue-collar (BC; high-load manual jobs with repetitive or forceful hand use, e.g., construction, manufacturing, cleaning), and medium-duty (MD; intermediate profiles such as healthcare aides, retail workers, or cooks). Retired (R) patients were reported separately, and cases with insufficient information were coded as missing or ambiguous.
Clinical data encompassed comorbidities (diabetes, smoking, rheumatoid arthritis, previous distal radius fracture). Physical examination systematically included the assessment of thenar muscle atrophy and weakness of the muscles innervated by the median nerve, which were recorded at all centers for inclusion in the study. Additional clinical tests (e.g., Phalen and Tinel tests) were performed at the discretion of the treating physician according to the clinical context but were not analyzed because they were not part of the predefined shared dataset.
2.5. Statistical Analysis
Continuous data are reported as mean ± SD or median (IQR/range), and categorical data as n (%). Longitudinal pain (preoperative, 1, 4, 12 weeks) was tested using the Friedman test; paired pre–post outcomes (BCTQ-SS/FS at baseline vs. 1 week; CSA at baseline vs. 4 weeks) with the Wilcoxon signed-rank test; between-group comparisons (e.g., RDA with vs. without week-1 complications) with the Mann–Whitney U test; and associations (e.g., RDA–RTW; BCTQ-FS–complications) with Spearman’s ρ.
Two-sided p-values < 0.05 were considered statistically significant.
3. Results
A total of 735 patients underwent ultrasound-guided carpal tunnel release (UGCTR). The cohort included 562 females (76.5%) and 173 males (23.5%). The mean age was 59.0 years (SD: 16.7; range: 23–90), with a median of 62 years (IQR: 48–70).
Regarding employment status, 275 patients (37.4%) were retired (R), 211 (28.7%) were employed in white-collar (WC; low-load) roles, 183 (24.9%) in blue-collar (BC; high-load) occupations, and 13 (1.8%) in medium-duty (MD) occupations. Fifty patients (6.8%) had missing or ambiguous occupational classification.
Comorbidities were absent in 629 patients (85.6%). The most common comorbidity was diabetes mellitus (DM), observed in 84 patients (11.4%), followed by smoking (S) declared in 14 cases (1.9%), rheumatoid arthritis (AR) in 6 (0.8%), and previous distal radius fracture without residual deformity (PDRF) in 2 patients (0.3%).
Thenar muscle atrophy was observed in 152 patients (20.7%), while 583 patients (79.3%) showed no signs of thenar wasting. Weakness in muscles innervated by the median nerve was detected in 181 patients (24.6%) and was absent in 554 patients (75.4%).
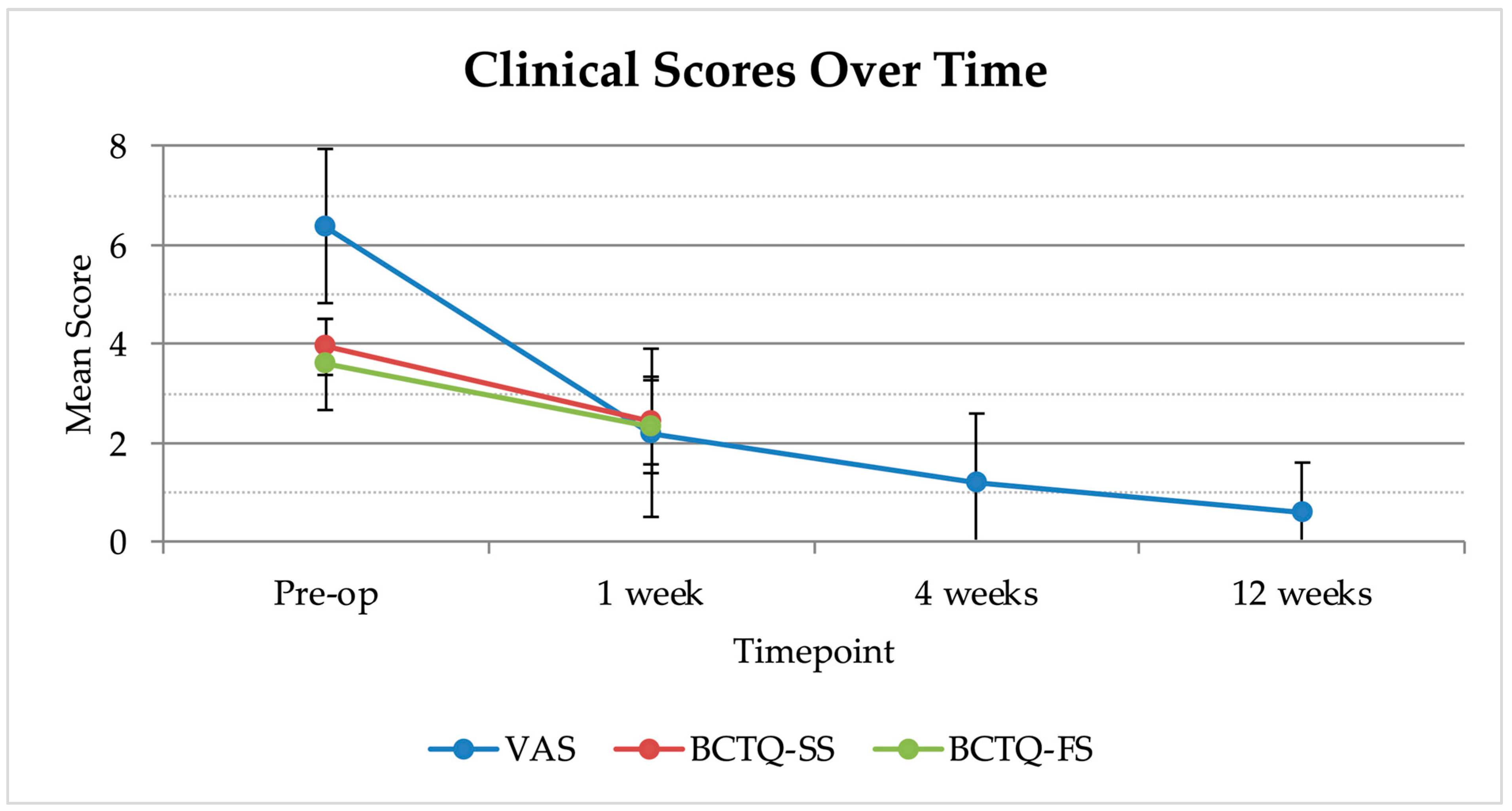
Preoperative pain intensity was assessed using the VAS, with a mean score of 6.37 (SD: 1.56; range: 1–10). The BCTQ showed a mean score of 3.95 (SD: 0.56; range: 2–5) for the BCTQ-SS and 3.59 (SD: 0.91; range: 0–5) for the BCTQ-FS (
Figure 2).
At 1 week following surgery, the mean VAS score was 2.20 (SD: 1.70; range: 0–9). The mean BCTQ-SS score was 2.45 (SD: 0.90; range: 1–5), while the BCTQ-FS score averaged 2.32 (SD: 0.93; range: 0–5). Both BCTQ subscales showed significant reductions from baseline (Wilcoxon W = 1094.5, p < 0.0001; and 1851.5, p < 0.0001, respectively).
At 4 weeks postoperatively, the mean VAS score further declined to 1.20 (SD: 1.40; range: 0–7). At 12 weeks, the VAS score continued to improve, reaching a mean of 0.58 (SD: 1.01; range: 0–8). The Friedman test for repeated measures confirmed that these reductions in VAS score were statistically significant (χ2 = 1827.04, p < 0.001).
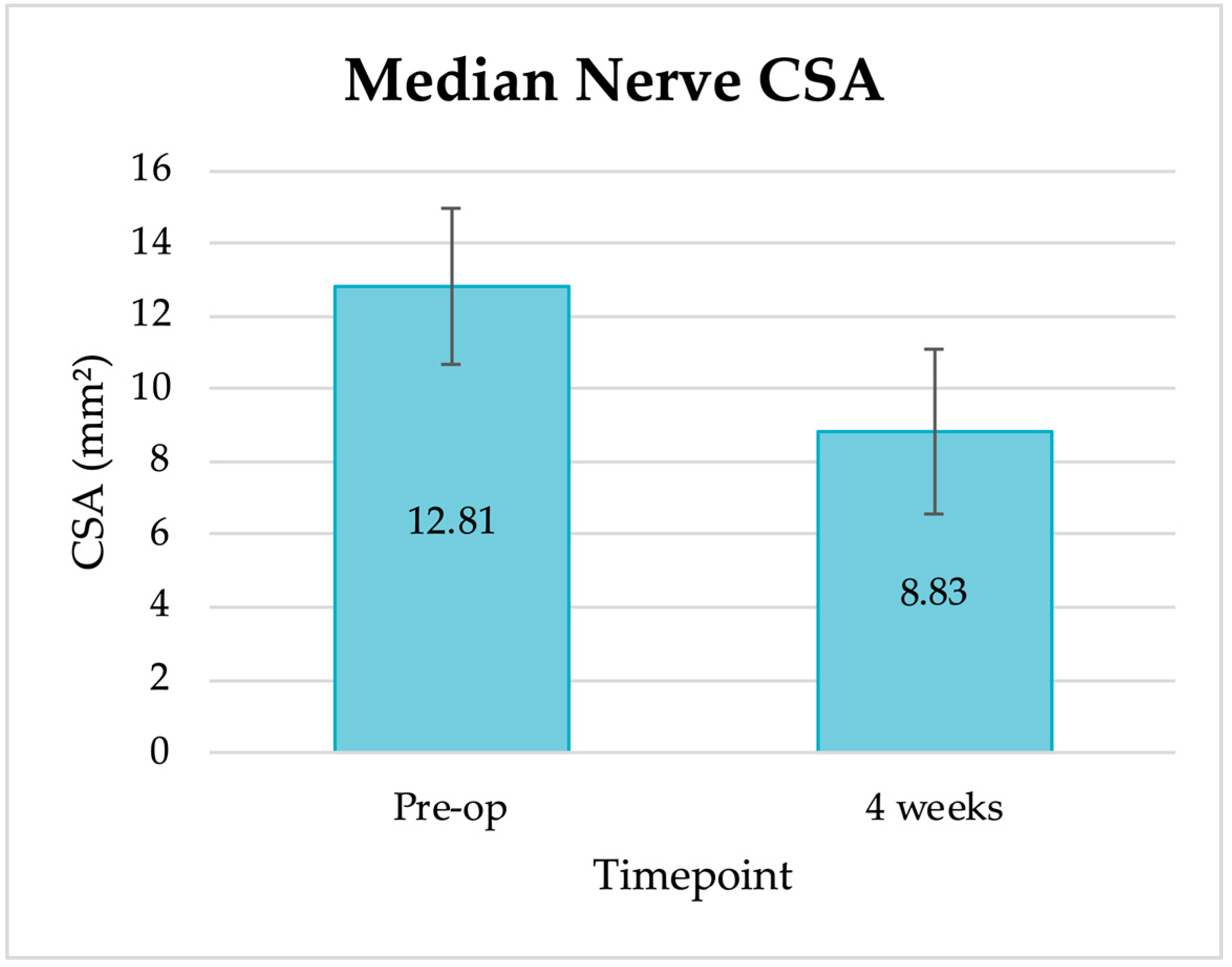
Preoperative ultrasound evaluation showed a mean CSA of the median nerve of 12.81 mm
2 (SD: 2.16; range: 6.2–29.2 mm
2). At 4 weeks postoperatively, the CSA had decreased to a mean of 8.83 mm
2 (SD: 2.24; range: 5.3–26.9 mm
2;
Figure 3). This change was statistically significant (Wilcoxon signed-rank test W = 3340.0,
p < 0.0001).
The average time to return to daily activities (RDA) was 5.7 days (SD: 2.6; range: 0–20), based on data from 690 patients. Data on return to work (RTW) were available for 555 patients. The average time to resume occupational activity was 14.5 days (SD: 4.1; range: 2–35).
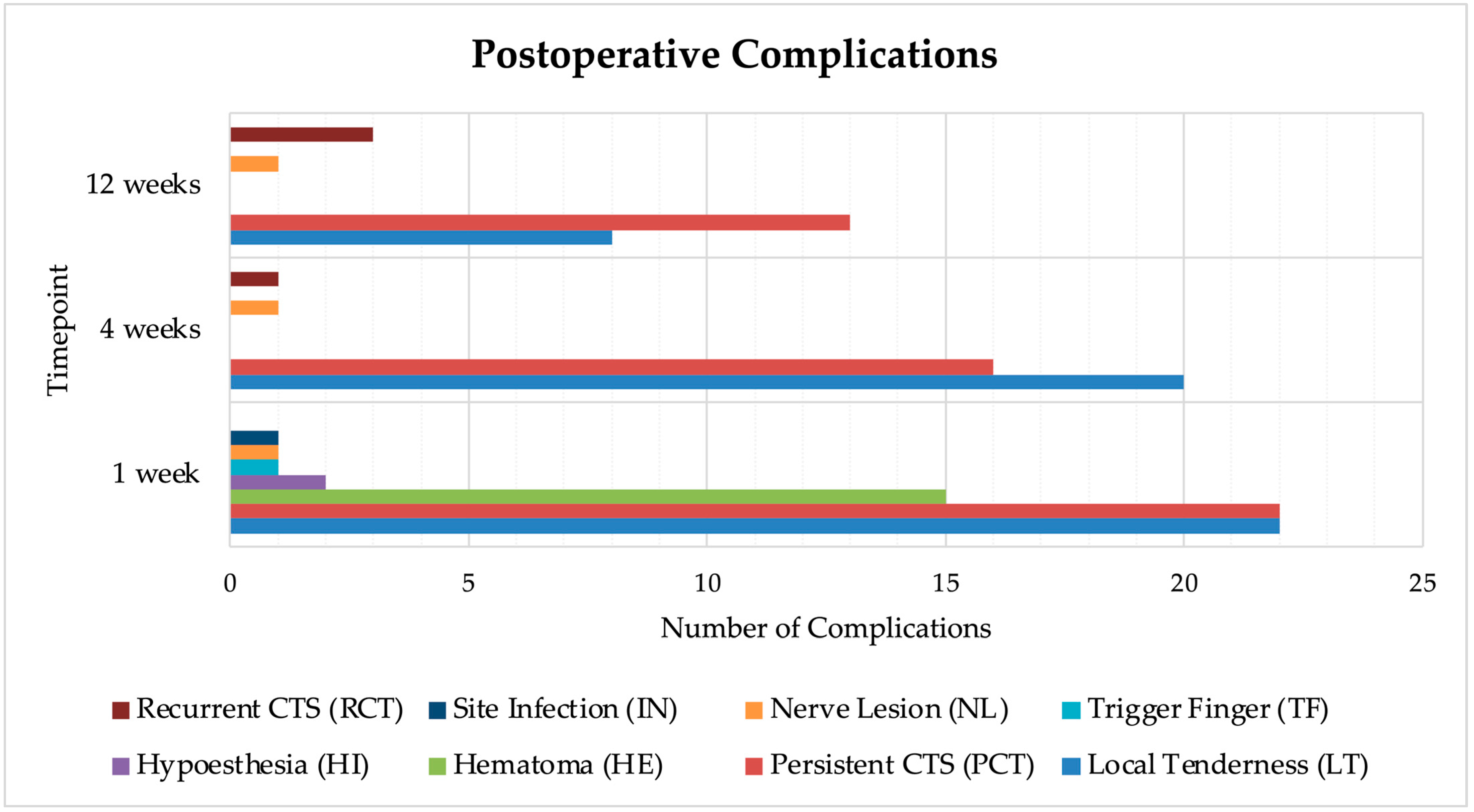
During the early postoperative period, a total of 64 patients (8.7%) experienced at least one complication at the 1-week follow-up (
Figure 4). The most frequently reported event was local tenderness (LT) along the trajectory of the surgical device, corresponding to the subcutaneous access path used during ultrasound guidance, observed in 22 cases (3.0%). This was followed by persistent carpal tunnel symptoms (PCT) in 22 patients (3.0%). Hematoma (HE) occurred in 15 cases (2.0%), while hypoesthesia (HI) and thumb trigger finger (TF) were reported in 2 patients (0.3%) and 1 patient (0.1%), respectively. One patient (0.1%) developed a nerve lesion (NL) involving the recurrent motor branch of the median nerve, and another (0.1%) was diagnosed with a superficial surgical site infection (IN). Overall, 640 patients (91.3%) showed no complications at this time point.
By 4 weeks, the complication rate decreased to 5.2%, with 38 patients reporting adverse events. LT remained the most common (20 cases, 2.7%), followed by PCT (16 cases, 2.2%). One case of recurrent carpal tunnel symptoms (RCT) and the nerve lesion was recorded. 671 patients (94.8%) were free from complications at this point.
At the 12-week follow-up, complications were reported in 25 patients (3.4%). PCT was still present in 13 cases (1.8%), LT in 8 (1.1%), and RCT in 3 cases (0.4%). The previously reported nerve lesion persisted in the patient. Overall, 710 patients (96.6%) showed no complications at the final follow-up.
We evaluated associations between clinical variables and recovery endpoints: statistically significant results are summarized here. RDA correlated strongly with RTW (Spearman’s ρ = 0.85, p < 0.0001). Patients with ≥1 complication at 1 week had longer RDA than those without (Mann–Whitney U = 7626.5, p = 0.048); the difference in RTW was not significant (U = 3962.0, p = 0.522). The presence of a complication at 1 week was associated with BCTQ-FS at baseline (ρ = −0.198, p < 0.0001) and at 1 week (ρ = −0.143, p < 0.001).
4. Discussion
The Results detail consistent improvements across patient-reported and sonographic outcomes after ultrasound-guided carpal tunnel release; below we interpret their clinical meaning, potential mechanisms, and limitations.
4.1. Cohort Description
The demographic profile of the patient cohort in this study aligns with the established epidemiology of carpal tunnel syndrome (CTS). Of the 735 patients who underwent ultrasound-guided carpal tunnel release (UGCTR), 562 were female (76.5%), a distribution consistent with previous epidemiological reports showing a higher prevalence of CTS among women [
1,
9]. This predominance has been attributed to narrower carpal tunnel dimensions and hormonal factors such as pregnancy and menopause, reinforcing the representativeness of the present sample.
The mean age of the cohort was 59.0 years (SD: 16.7), with a median of 62 years, consistent with large epidemiological studies reporting peak CTS incidence between the fifth and sixth decades of life. This distribution supports the degenerative and cumulative nature of the condition, which tends to become more symptomatic with advancing age [
9,
10].
Regarding employment status, at the time of surgery, 410 patients reported being actively employed, of whom 226 (55.1%) were engaged in physically demanding occupations. This finding supports existing literature linking CTS to occupational exposure to repetitive wrist movements, forceful gripping, and vibration, particularly in blue-collar and manual labor roles [
11,
12].
Overall, the demographic and occupational characteristics of this cohort are representative of the broader population undergoing surgical treatment for CTS, thus supporting the external validity and generalizability of the study findings.
4.2. Visual Analog Scale for Pain
A progressive reduction in pain intensity, as measured by the Visual Analog Scale (VAS), was observed across all postoperative time points. The mean preoperative VAS score was 6.37, which decreased significantly to 2.20 at 1 week, 1.20 at 4 weeks, and 0.58 at 12 weeks postoperatively, indicating a consistent and clinically meaningful improvement in pain following UGCTR.
Comparable postoperative reductions in VAS have been reported with both open and endoscopic techniques, with no significant differences between approaches at midterm follow-up [
13,
14]. However, the present study shows that UGCTR achieves similarly effective pain relief more rapidly, with a substantial reduction already evident at the first postoperative week.
4.3. Cross-Sectional Area of the Median Nerve
A significant reduction in the cross-sectional area (CSA) of the median nerve was observed following UGCTR, reflecting the structural efficacy of the procedure: the mean reduction in CSA at 4 weeks was 3.98 mm2, indicating an early and consistent decrease in median nerve swelling after decompression.
These findings are consistent with those reported by Saglam et al., who observed a significant decrease in median nerve CSA following surgical release, using ultrasonography to monitor structural recovery [
15].
The reduction in CSA provides an anatomical indicator of successful decompression; however, as current literature has not demonstrated a strong correlation between post-surgical nerve size and clinical symptoms, CSA should not be considered an isolated outcome measure but interpreted together with clinical outcomes.
4.4. Return to Daily Activities and Work
The present study found an average time to return to daily activities (RDA) of 5.7 days and an average return to work (RTW) of 14.5 days following UGCTR. These results are consistent with previous literature, including a study by Asserson et al. [
16] in which patients treated with ultrasound-guided thread carpal tunnel release (TCTR) resumed work after an average of 12 days, compared with 33 days in the open carpal tunnel release (OCTR) group. In published OCTR series, the time to return to daily activities is longer than in our cohort: Acharya et al. [
17] reported a mean of 13 days, and Gürpınar et al. [
18] reported a mean of 14.1 days.
These findings highlight the advantage of ultrasound-guided techniques in facilitating a quicker functional recovery, with potential benefits for individual patients’ quality of life as well as for reducing overall healthcare resource utilization and work absenteeism.
4.5. Boston Carpal Tunnel Questionnaire
Significant improvements were observed in both symptom severity and functional status within the first postoperative week, as measured by the Boston Carpal Tunnel Questionnaire (BCTQ). These changes were both statistically significant and clinically meaningful, confirming the efficacy of UGCTR in rapidly improving patient-reported symptoms and functional capacity. The observed improvements were consistent with parallel reductions in VAS scores and median nerve CSA, further reinforcing the overall effectiveness of the procedure.
4.6. Complication
The overall complication rate following UGCTR was low and decreased progressively over time. At 1 week postoperatively, 64 patients (8.7%) experienced at least one complication: local tenderness (LT) (3.0%) and persistent carpal tunnel symptoms (PCT) (3.0%) were the most frequent, followed by hematoma (HE) (2.0%), hypoesthesia (HI) (0.3%), trigger finger (TF) (0.1%), infection (IN) (0.1%), and nerve lesion (NL) (0.1%).
By 4 weeks, the complication rate had decreased to 5.2%, and by 12 weeks to 3.4%, with most residual symptoms involving PCT and LT. This trend suggests that most complications were mild and self-limiting, though rare serious events such as NL were observed.
Compared to this, in a recent comprehensive review, Sprangers et al. [
19] reported higher and more variable complication rates following traditional open or endoscopic carpal tunnel release. Scar tenderness was reported in up to 81% during the same period, with some patients still symptomatic after 6 months. Infections occurred in up to 8% of cases, and permanent nerve injury, although rare, was documented. These findings suggest that UGCTR may offer a more favorable complication profile, particularly regarding wound-related and persistent pain outcomes.
In this study, one case of recurrent motor branch nerve injury was documented among 735 patients who underwent UGCTR, corresponding to an incidence of 0.1%. This rate is higher than the estimated 0.03% incidence of motor branch injuries reported by Sprangers et al., based on large cohort studies of carpal tunnel release.
Given that UGCTR is a relatively recent technique, the presence of a single nerve lesion in a large cohort may reflect the early phase of the learning curve. With increased procedural experience and consistent application of high-resolution sonographic techniques, the risk of NL may be further reduced.
4.7. Further Analyses
Additional analyses of the dataset revealed several significant associations between clinical variables, providing further insight into the recovery process following UGCTR.
As expected, a strong positive correlation was found between time to return to daily activities and return to work, indicating that earlier functional recovery in daily life strongly predicts a faster return to professional duties.
Patients who experienced at least one complication at 1 week postoperatively took significantly longer to resume daily activities compared with those without complications. However, the difference in time to return to work between the two groups did not reach statistical significance.
Complications at 1 week were also associated with worse functional outcomes. Patients who experienced postoperative complications tended to report higher BCTQ-FS scores both preoperatively and at 1 week postoperatively, suggesting that these individuals may have had a more functionally limiting presentation and a slower early recovery trajectory.
The ultrasound-guided carpal tunnel release performed in this study exemplifies the growing paradigm of musculoskeletal “echosurgery,” in which imaging and intervention are integrated in real time. This approach enables great procedural precision, minimal invasiveness, and the potential to safely operate outside traditional surgical suites.
4.8. Limitations
This study has several limitations that should be acknowledged.
The multicenter design, while increasing the generalizability of the findings, also introduces heterogeneity in terms of surgical experience, equipment, and perioperative protocols among centers. Although all surgeons followed a shared procedural framework, subtle differences in technique or follow-up assessment may have influenced patient-reported outcomes.
The study lacked a control group treated with OCTR, which prevents direct comparison between techniques. While comparisons with historical data from the literature were included in the discussion, a randomized controlled trial would be necessary to draw definitive conclusions regarding the superiority or equivalence of UGCTR.
While follow-up duration was sufficient to capture early and intermediate outcomes, longer-term follow-up would be required to evaluate recurrence rates, late complications, and the durability of symptom relief beyond 12 weeks. The BCTQ was administered only at baseline and at 1 week; the absence of BCTQ data at 4 and 12 weeks limits the assessment of longer-term patient-reported outcomes.
Additionally, incomplete data availability for certain outcome measures represents a further limitation. In particular, RDA was recorded in 690 patients, whereas RTW data were available for only 555 patients. This partial data capture may reduce the statistical power of subgroup analyses and limit the generalizability of those specific findings.
Lastly, although outcome assessments included both subjective and objective measures, reliance on patient self-reporting for certain metrics (e.g., RTW, RDA, VAS) may introduce recall or reporting bias.
5. Conclusions
This multicenter study demonstrates that ultrasound-guided carpal tunnel release (UGCTR) is a safe, effective, and efficient treatment for carpal tunnel syndrome. Patients experienced rapid postoperative recovery, with significant improvements in pain, symptom severity, and hand function already evident at 1 week and further sustained through subsequent follow-ups. Complication rates were low, and the vast majority of adverse events were mild and transient.
UGCTR enabled a streamlined surgical workflow in outpatient settings, without the need for an operating room or general anesthesia, and showed potential advantages in terms of both recovery time and procedural accessibility. These findings support the growing role of UGCTR not only as a technically sound alternative to open surgery, but also as a model of “echosurgical” intervention, combining imaging and treatment in a minimally invasive, resource-conscious format.
Further prospective studies with long-term follow-up and direct comparison to open or endoscopic techniques will be important to confirm the durability of outcomes and better define optimal patient selection criteria for this evolving technique.