Analysis of Trends in Orthopedic Knee Surgery—Key Findings on Total and Unicompartmental Knee Arthroplasty from a Leading Journal
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Data Synthesis
3. Results
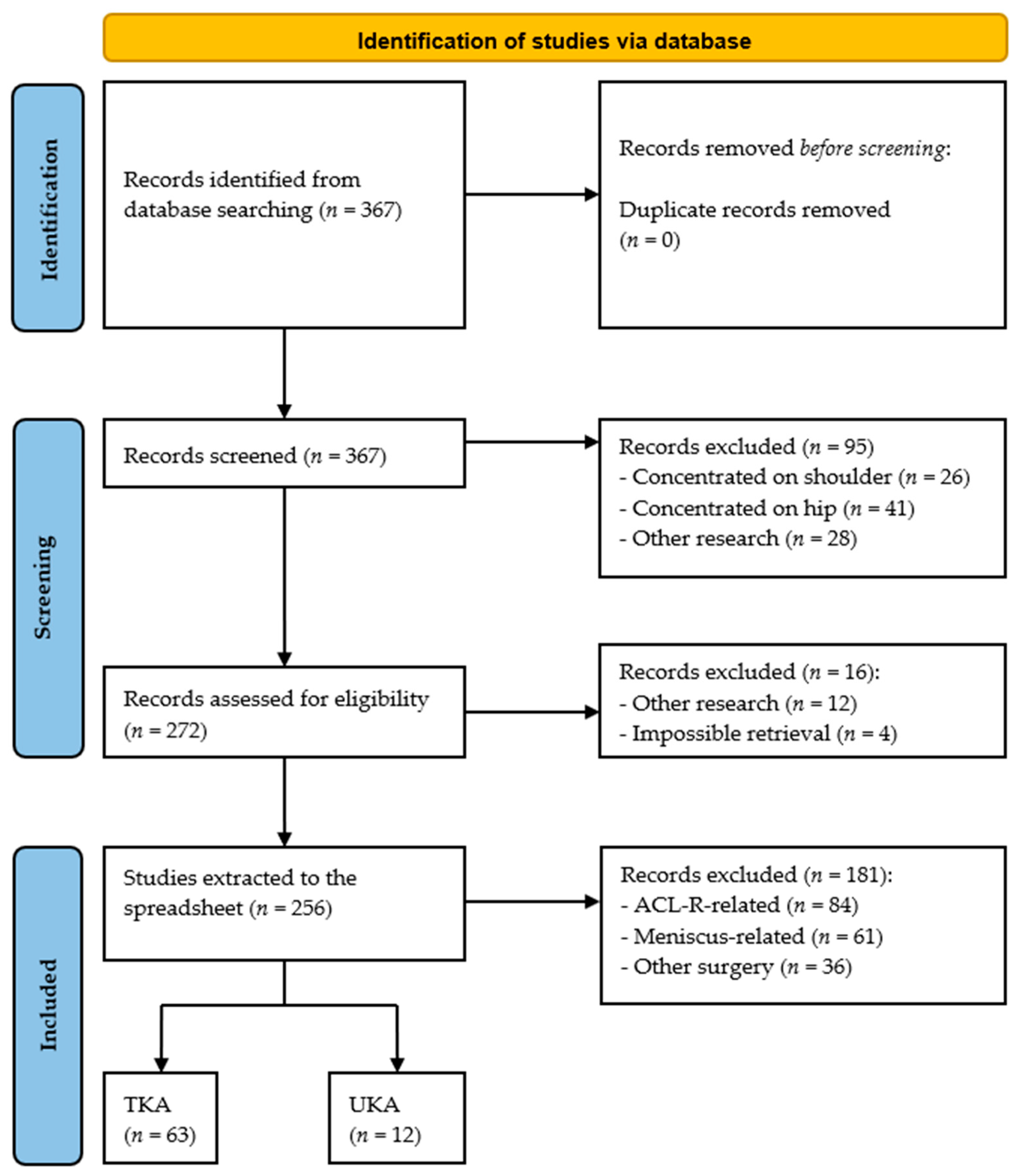
3.1. Results of Study Selection
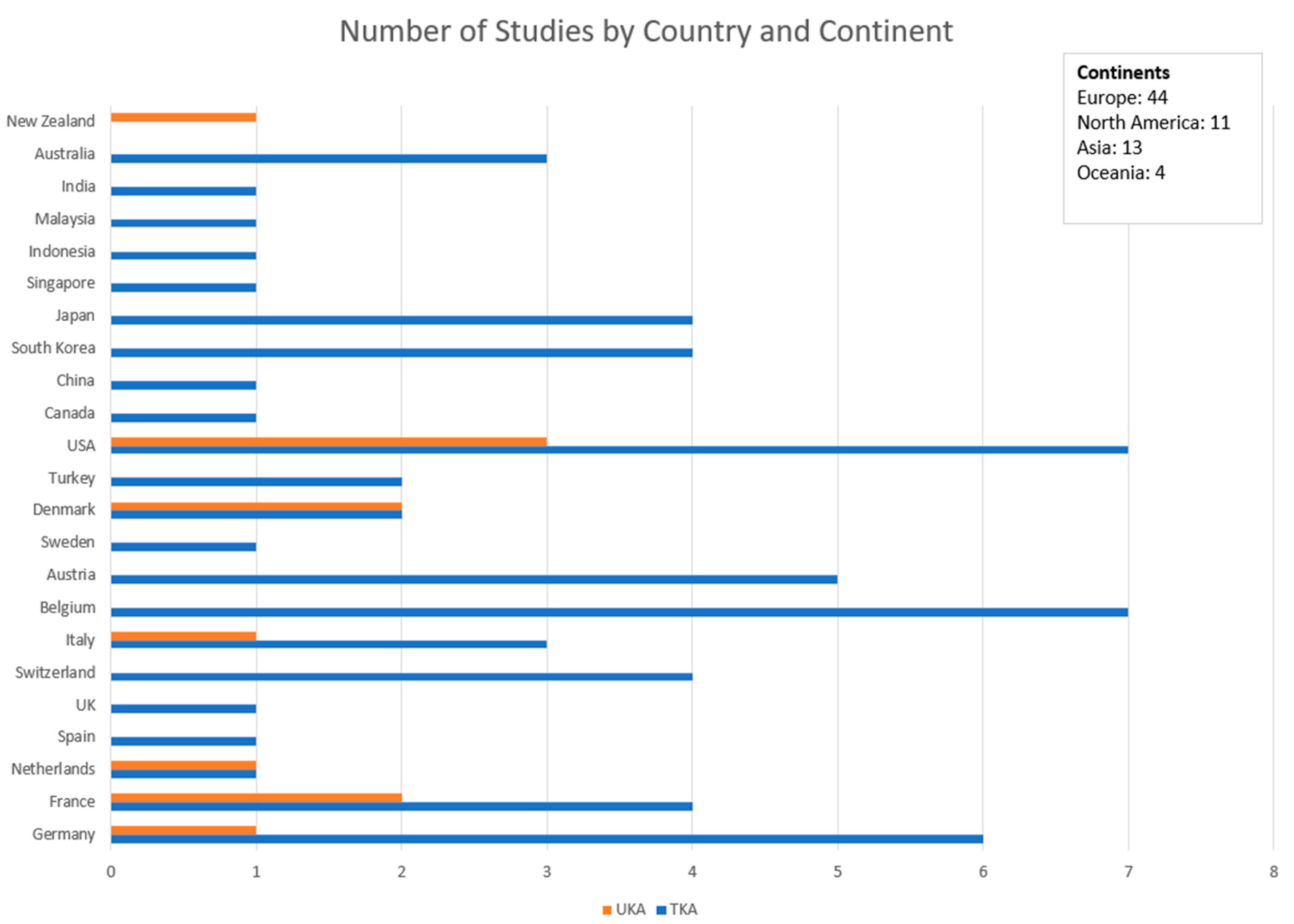
3.2. Distribution of Published Studies
3.3. TKA
3.3.1. Alignment and Gap Balancing
3.3.2. Robotic-Assisted Surgery in Primary TKA
3.3.3. Implant Design
3.3.4. Personalized TKA
3.3.5. Revision TKA
3.3.6. Pre- and Postoperative Care
3.4. Unicondylar Knee Arthropalsty (KA)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AKP | Postoperative anterior knee pain |
| ALBC | Antibiotic-loaded bone cement |
| AMA | Adjusted mechanical alignment |
| BCR | Bicruciate-retaining |
| CAS | Computer-aided surgery |
| CCI | Charlson Comorbidity Index |
| CFS | Clinical Frailty Scale |
| CIM | customized individually made |
| CPAK | coronal plane alignment of the knee |
| CSI | central sensitisation inventory |
| ct | computer tomography |
| ema | extensor mechanism allograft |
| fa | functional alignment |
| fb | fixed-bearing |
| FJS | Forgotten Joint Scores |
| flr | full-leg radiographs |
| hka | hip–knee–ankle |
| hto | high tibial osteotomy |
| ika | inverse kinematic alignment |
| il-6 | interleukin-6 |
| KA | kinematic alignment |
| KOOS | Knee Injury and Osteoarthritis Outcome Score |
| KSSTA | Knee Surgery, Sports Traumatology, Arthroscopy |
| LCL | lateral collateral ligament |
| LDFF | lift–drill–fill–fix |
| MA | mechanical axis |
| MB | mobile-bearing |
| MC-PCLX | medial congruent–posterior cruciate ligament excised |
| MFI | Modified Frailty Index |
| mLDFA | mechanical lateral distal femoral angle |
| MNP | multiple needle puncturing |
| MP | medial-pivot |
| MPTA | medial proximal tibial angle |
| MRI | magnetic resonance imaging |
| OA | osteoarthritis |
| OKS | Oxford Knee Score |
| ots | off-the-shelf |
| pcr | posterior capsular release |
| PCL | posterior cruciate ligament |
| PRISMA | Preferred Reporting Items for Systematic reviews and Meta-Analyses |
| PROMIS | Patient Reported Outcomes Measurement Information System |
| PSI | patient-specific instrumentation |
| PTA | prosthetic trochlear angle |
| PTOA | posttraumatic osteoarthritis |
| QV | quadriceps vector |
| raTKA | robotic-assisted total knee arthroplasty |
| raUKA | robotic-assisted unicompartmental knee arthroplasty |
| rKA | restricted kinematic alignment |
| RHK | rotating hinge knee |
| ROM | range of motion |
| RTKA | revision total knee arthroplasty |
| sMCL | superficial medial collateral ligament |
| TKA | total knee arthroplasty |
| TMC | tantalum metal cones |
| UKA | unicompartmental knee arthroplasty |
| unKA | unrestricted kinematic alignment |
| VEGFA | vascular endothelial growth factor A |
| WOMAC | Western Ontario and McMaster Universities Osteoarthritis Index |
References
- Filip, N.; Radu, I.; Veliceasa, B.; Filip, C.; Pertea, M.; Clim, A.; Pinzariu, A.C.; Drochioi, I.C.; Hilitanu, R.L.; Serban, I.L. Biomaterials in Orthopedic Devices: Current Issues and Future Perspectives. Coatings 2022, 12, 1544. [Google Scholar] [CrossRef]
- Im, G.I. Biomaterials in orthopaedics: The past and future with immune modulation. Biomater. Res. 2020, 24, 7. [Google Scholar] [CrossRef]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Pietrzak, J.R.T.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: A prospective cohort study. Bone Jt. J. 2018, 100-B, 930–937. [Google Scholar] [CrossRef]
- Kizaki, K.; Shanmugaraj, A.; Yamashita, F.; Simunovic, N.; Duong, A.; Khanna, V.; Ayeni, O.R. Total knee arthroplasty using patient-specific instrumentation for osteoarthritis of the knee: A meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 561. [Google Scholar] [CrossRef]
- Tang, J.Z.; Nie, M.J.; Zhao, J.Z.; Zhang, G.C.; Zhang, Q.; Wang, B. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: A meta-analysis. J. Orthop. Surg. Res. 2020, 15, 403. [Google Scholar] [CrossRef]
- Jin, W.S.; Yin, L.X.; Sun, H.Q.; Zhao, Z.; Yan, X.F. Mesenchymal Stem Cells Injection Is More Effective Than Hyaluronic Acid Injection in the Treatment of Knee Osteoarthritis With Similar Safety: A Systematic Review and Meta-Analysis. Arthroscopy 2024, 41, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Prill, R.; Królikowska, A.; Becker, R.; Karlsson, J. Why there is a need to improve evaluation standards for clinical studies in orthopaedic and sports medicine. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4–5. [Google Scholar] [CrossRef]
- Prill, R.; Królikowska, A.; de Girolamo, L.; Becker, R.; Karlsson, J. Checklists, risk of bias tools, and reporting guidelines for research in orthopedics, sports medicine, and rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3029–3033. [Google Scholar] [CrossRef]
- Prill, R.; Mouton, C.; Klugorová, J.; Królikowska, A.; Karlsson, J.; Becker, R. Implementation of evidence-based medicine in everyday clinical practice. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3034–3036. [Google Scholar] [CrossRef]
- Ostojic, M.; Winkler, P.W.; Karlsson, J.; Becker, R.; Prill, R. Minimal Clinically Important Difference: Don’t just look at the “p-value”. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4077–4079. [Google Scholar] [CrossRef] [PubMed]
- Królikowska, A.; Reichert, P.; Karlsson, J.; Mouton, C.; Becker, R.; Prill, R. Improving the reliability of measurements in orthopaedics and sports medicine. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5277–5285. [Google Scholar] [CrossRef]
- Adriani, M.; Becker, R.; Milano, G.; Lachowski, K.; Prill, R. High variation among clinical studies in the assessment of physical function after knee replacement: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3854–3860. [Google Scholar] [CrossRef]
- Sukhera, J. Narrative Reviews in Medical Education: Key Steps for Researchers. J. Grad. Med. Educ. 2022, 14, 418–419. [Google Scholar] [CrossRef] [PubMed]
- Sukhera, J. Narrative Reviews: Flexible, Rigorous, and Practical. J. Grad. Med. Educ. 2022, 14, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Büttner, F.; Andrade, R.; Weir, A.; Ashe, M.C.; Holden, S.; Impellizzeri, F.M.; Delahunt, E.; Dijkstra, H.P.; Mathieson, S.; et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: The PERSiST guidance. Br. J. Sports Med. 2022, 56, 175–195. [Google Scholar] [CrossRef]
- Tuecking, L.R.; Savov, P.; Zander, M.; Jeremic, D.; Windhagen, H.; Ettinger, M. Comparable accuracy of femoral joint line reconstruction in different kinematic and functional alignment techniques. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1795. [Google Scholar] [CrossRef]
- Van de Graaf, V.A.; Chen, D.B.; Allom, R.J.; Wood, J.A.; MacDessi, S.J. Functional alignment in total knee arthroplasty best achieves balanced gaps and minimal bone resections: An analysis comparing mechanical, kinematic and functional alignment strategies. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5118–5127. [Google Scholar] [CrossRef]
- Howell, S.M.; Sappey-Marinier, E.; Niesen, A.E.; Nedopil, A.J.; Hull, M.L. Better forgotten joint scores when the angle of the prosthetic trochlea is lateral to the quadriceps vector in kinematically aligned total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5438–5445. [Google Scholar] [CrossRef] [PubMed]
- Winnock de Grave, P.; Luyckx, T.; Van Criekinge, T.; Müller, J.H.; Ollivier, B.; Van Eecke, E. Inverse kinematic alignment accommodates native coronal knee alignment better in comparison to adjusted mechanical alignment and restricted kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1795. [Google Scholar] [CrossRef]
- Kobayashi, T.; Kawaguchi, K.; Goto, K.; Suzuki, H.; Otsu, M.; Michishita, K. Functional knee phenotypes: A helpful classification tool for visualizing potential femoral varus in restricted kinematic alignment total knee arthroplasty in Japan. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 103–115. [Google Scholar] [CrossRef]
- Rak, D.; Rügamer, T.; Klann, L.; Nedopil, A.J.; Rudert, M. Setting the distal and posterior condyle of the femoral component to restore the medial pre-arthritic femoral articular surface results in better outcomes after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5319–5331. [Google Scholar] [CrossRef]
- Syrikas, I.; Engbäck, C.; Tsikandylakis, G.; Karikis, I.; Desai, N. Increased complication rates and inferior patient-reported outcomes following total knee arthroplasty due to post-traumatic osteoarthritis with previous fracture treatment: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4124–4141. [Google Scholar] [CrossRef]
- Matsumoto, T.; Nakano, N.; Ishida, K.; Maeda, T.; Tachibana, S.; Kuroda, Y.; Hayashi, S.; Matsushita, T.; Kuroda, R. Targeting the neutral hip-to-calcaneus axis in kinematically aligned total knee arthroplasty is feasible with fewer alignment outliers for varus osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1795. [Google Scholar] [CrossRef]
- Winnock de Grave, P.; Van Criekinge, T.; Luyckx, T.; Moreels, R.; Gunst, P.; Claeys, K. Restoration of the native tibial joint line obliquity in total knee arthroplasty with inverse kinematic alignment does not increase knee adduction moments. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4692–4704. [Google Scholar] [CrossRef]
- Van de Kelft, A.S.; De Mulder, K.; De Schepper, J.; Victor, J.; Vundelinckx, B. Balancing the flexion gap first in total knee arthroplasty leads to better preservation of posterior condylar offset resulting in better knee flexion. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1795. [Google Scholar] [CrossRef] [PubMed]
- Wakelin, E.A.; Ponder, C.E.; Randall, A.L.; Koenig, J.A.; Plaskos, C.; DeClaire, J.H.; Lawrence, J.M.; Keggi, J.M. Intra-operative laxity and balance impact 2-year pain outcomes in TKA: A prospective cohort study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5535–5545. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, H.; Saito, R.; Shioda, M.; Jinno, T.; Kaneyama, R.; Watanabe, T. Effect of posteromedial vertical capsulotomy with medial collateral ligament liberation on intraoperative medial component gap mismatch between extension and mid-flexion during total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5603–5610. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, H.; Saito, R.; Shioda, M.; Jinno, T.; Watanabe, T. Limited medial posterior capsular release increases the intraoperative medial component gap while maintaining the joint varus angle at extension in posterior-stabilized total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4187–4194. [Google Scholar] [CrossRef]
- Ho, J.P.Y.; Cho, J.H.; Nam, H.S.; Park, S.Y.; Lee, Y.S. Constitutional alignment predicts medial ligament balancing in mechanically aligned total knee arthroplasty for varus knees. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5940–5949. [Google Scholar] [CrossRef]
- Zou, D.; Ling, Z.; Tan, J.; Zheng, N.; Dimitriou, D.; Chen, Y.; Tsai, T. Medial stability and lateral flexibility of the collateral ligaments during mid-range flexion in medial-pivot total knee arthroplasty patients demonstrates favorable postoperative outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1795. [Google Scholar] [CrossRef]
- Kono, K.; Inui, H.; Tomita, T.; Yamazaki, T.; Konda, S.; Taketomi, S.; Tanaka, S.; D’lIma, D.D. Bicruciate-retaining total knee arthroplasty procedure reduced tensile force in the middle and posterior components of lateral collateral ligament during deep knee flexion activities with no effect on tensile force of the medial collateral ligament. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3889–3897. [Google Scholar] [CrossRef]
- Lee, S.S.; Lee, J.; Alharthi, H.; Moon, Y.W. Effect of mediolateral gap difference on postoperative outcomes in navigation-assisted total knee arthroplasty using an ultracongruent insert and the medial stabilising technique. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3745–3754. [Google Scholar] [CrossRef]
- Schelker, B.L.; Moret, C.S.; Sava, M.P.; von Eisenhart-Rothe, R.; Graichen, H.; Arnold, M.P.; Leclercq, V.; Hirschmann, M.T. The impact of different alignment strategies on bone cuts in total knee arthroplasty for varus knee phenotypes. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1840–1850. [Google Scholar] [CrossRef]
- Bollars, P.; Janssen, D.; De Weerdt, W.; Albelooshi, A.; Meshram, P.; Nguyen, T.D.; Lacour, M.T.; Schotanus, M.G.M. Improved accuracy of implant placement with an imageless handheld robotic system compared to conventional instrumentation in patients undergoing total knee arthroplasty: A prospective randomized controlled trial using CT-based assessment of radiological outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5446–5452. [Google Scholar]
- Shen, T.S.; Uppstrom, T.J.; Walker, P.J.; Yu, J.S.; Cheng, R.; Mayman, D.J.; Jerabek, S.A.; Ast, M.P. High degree of alignment precision associated with total knee arthroplasty performed using a surgical robot or handheld navigation. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4735–4740. [Google Scholar] [CrossRef]
- Glowalla, C.; Langer, S.; Lenze, U.; Lazic, I.; Hirschmann, M.T.; Hinterwimmer, F.; von Eisenhart-Rothe, R.; Pohlig, F. Postoperative full leg radiographs exhibit less residual coronal varus deformity compared to intraoperative measurements in robotic arm-assisted total knee arthroplasty with the MAKOTM system. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3912–3918. [Google Scholar] [CrossRef] [PubMed]
- Kafelov, M.; Batailler, C.; Shatrov, J.; Al-Jufaili, J.; Farhat, J.; Servien, E.; Lustig, S. Functional positioning principles for image-based robotic-assisted TKA achieved a higher Forgotten Joint Score at 1 year compared to conventional TKA with restricted kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5591–5602. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Fontalis, A.; Haddad, I.C.; Donovan, C.; Rajput, V.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with comparable functional outcomes but improved forgotten joint scores compared with conventional manual total knee arthroplasty at five-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5453–5462. [Google Scholar] [CrossRef] [PubMed]
- Turan, K.; Camurcu, Y.; Kezer, M.; Uysal, Y.; Kizilay, Y.O.; Ucpunar, H.; Temiz, A. A comparison of robotic-assisted and manual techniques in restricted kinematically aligned total knee arthroplasty: Coronal alignment improvement with no significant clinical differences. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4673–4679. [Google Scholar] [CrossRef]
- Ollivier, B.; Vandenneucker, H.; Vermue, H.; Luyckx, T. A robotic-assisted simulation of kinematic alignment in TKA leads to excessive valgus and internal rotation in valgus knees. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4747–4754. [Google Scholar] [CrossRef]
- Vandenberk, J.; Mievis, J.; Deferm, J.; Janssen, D.; Bollars, P.; Vandenneucker, H. NAVIO RATKA shows similar rates of hemoglobin-drop, adverse events, readmission and early revision vs conventional TKA: A single centre retrospective cohort study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4798–4808. [Google Scholar] [CrossRef]
- Witvoet, S.; de Massari, D.; Shi, S.; Chen, A.F. Leveraging large, real-world data through machine-learning to increase efficiency in robotic-assisted total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3160–3171. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; von Eisenhart-Rothe, R.; Graichen, H. Any technology assisting total knee arthroplasty (TKA) will fail without the correct 3D alignment and balancing target. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 733–735. [Google Scholar] [CrossRef]
- Hazratwala, K.; Gouk, C.; Wilkinson, M.P.R.; O’Callaghan, W.B. Navigated functional alignment total knee arthroplasty achieves reliable, reproducible and accurate results with high patient satisfaction. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3861–3870. [Google Scholar] [CrossRef]
- Sava, M.P.; Hara, H.; Alexandra, L.; Hügli, R.W.; Hirschmann, M.T. Verasense sensor-assisted total knee arthroplasty showed no difference in range of motion, reoperation rate or functional outcomes when compared to manually balanced total knee arthroplasty: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1851–1858. [Google Scholar] [CrossRef] [PubMed]
- Budhiparama, N.C.; Lumban-Gaol, I.; Novito, K.; Hidayat, H.; De Meo, F.; Cacciola, G.; Cavaliere, P. PCL retained is safe in medial pivot TKA—A prospective randomized trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5856–5863. [Google Scholar] [CrossRef]
- Rajgopal, A.; Kumar, S.; Singh, M.K.; Aggarwal, K. PCL retention demonstrates better functional scores and gait patterns in total knee arthroplasty using a medial congruent insert—A prospective study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4741–4746. [Google Scholar] [CrossRef]
- Favroul, C.; Batailler, C.; Naaim, A.; Foissey, C.; Kafelov, M.; Cheze, L.; Servien, E.; Lustig, S. Cruciate-substituting and posterior-stabilised total knee arthroplasties had similar gait patterns in the short term. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5398–5406. [Google Scholar] [CrossRef] [PubMed]
- Haslhofer, D.J.; Kraml, N.; Winkler, P.W.; Gotterbarm, T.; Klasan, A. Risk for total knee arthroplasty after tibial plateau fractures: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5145–5153. [Google Scholar] [CrossRef]
- Zinno, R.; Alesi, D.; Di Paolo, S.; Pizza, N.; Zaffagnini, S.; Muccioli, G.M.M.; Bragonzoni, L. Wider translations and rotations in posterior-stabilised mobile-bearing total knee arthroplasty compared to fixed-bearing both implanted with mechanical alignment: A dynamic RSA study. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4969–4976. [Google Scholar] [CrossRef]
- Jung, H.J.; Kang, M.W.; Lee, J.H.; Lee, J.K.; Kim, J.I. Preoperative patellar bone marrow lesions with full thickness cartilage defects correlate with residual anterior knee pain in total knee arthroplasty without patellar resurfacing. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5048–5056. [Google Scholar] [CrossRef]
- Nardelli, P.; Neururer, S.; Gruber, K.; Wippel, D.; Kogler, N.; Ender, S.; Leitner, H.; Koller, B.; Fischer, M.; Dammerer, D.; et al. Total knee arthroplasty without patella resurfacing leads to worse results in patients with patellafemoral osteoarthritis Iwano Stages 3–4: A study based on arthroplasty registry data. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3941–3946. [Google Scholar] [CrossRef]
- Goicoechea, N.; Hinarejos, P.; Gasol, B.; Torres-Claramunt, R.; Sánchez-Soler, J.; Perelli, S.; Monllau, J.C. Systematic lateral retinacular release does not reduce anterior knee pain after total knee arthroplasty with patellar resurfacing. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4213–4219. [Google Scholar] [CrossRef]
- Kalaai, S.; Most, J.; van Dun, B.; Kaptein, B.L.; Tilman, P.B.J.; Boonen, B.; Schotanus, M.G.M. Less wear in deep-dished mobile compared to fixed bearing total knee arthroplasty of the same design at 5-year follow-up: A randomised controlled model-based Roentgen stereophotogrammetric analysis trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5137–5144. [Google Scholar] [CrossRef]
- Abdel Khalik, H.; Wood, T.J.; Tushinski, D.M.; Gazendam, A.; Petruccelli, D.T.; Bali, K.; Hamilton Arthroplasty Group; Winemaker, M.; Avram, V.; de Beer, J.; et al. Routine use of antibiotic-laden bone cement in total knee arthroplasty is a cost-effective practice in the single-payer healthcare system. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3847–3853. [Google Scholar] [CrossRef] [PubMed]
- Song, S.J.; Hwang, S.H.; Baek, H.J.; Park, C.H. Aseptic survival of the 1.5-stage exchange arthroplasty for periprosthetic joint infection was acceptable when using an autoclaved femoral component and a new polyethylene insert. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4996–5004. [Google Scholar] [CrossRef] [PubMed]
- Baldini, A.; Lamberti, A.; Balato, G.; Cavallo, G.; Summa, P. Inferior results at long-term follow-up after extensor mechanism allograft reconstruction in septic compared to aseptic revision total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1477–1482. [Google Scholar] [CrossRef] [PubMed]
- Rivière, C.; Villet, L.; Roby, G.B. Anatomical restoration of the anterior femoral compartment when performing KATKA: The end of the flush anterior femoral cut dogma! Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3037–3040. [Google Scholar] [CrossRef]
- Sadoghi, P.; Hirschmann, M.T.; Karlsson, J.; Klasan, A. The neglected factor of constitutional sagittal alignment and its implications for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 10–12. [Google Scholar] [CrossRef]
- Gousopoulos, L.; Dobbelaere, A.; Ratano, S.; Bondoux, L.; ReSurg, J.; Müller, J.H.; Dubreuil, S.; Saffarini, M.; Tibesku, C.O.; Aït-Si-Selmi, T.; et al. Custom total knee arthroplasty combined with personalised alignment grants 94% patient satisfaction at minimum follow-up of 2 years. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1276–1283. [Google Scholar] [CrossRef]
- Vogel, N.; Kaelin, R.; Rychen, T.; Wendelspiess, S.; Müller-Gerbl, M.; Arnold, M.P. Satisfaction after total knee arthroplasty: A prospective matched-pair analysis of patients with customised individually made and off-the-shelf implants. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5873–5884. [Google Scholar] [CrossRef] [PubMed]
- Eer, M.; Flevas, D.A.; Bornes, T.D.; Braun, S.; Meurer, A.; Sculco, P.K.; Quevedo-González, F.J.; Boettner, F. Tibial bone defect prediction based on preoperative artefact-reduced CT imaging is superior to standard radiograph assessment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4842–4850. [Google Scholar]
- Eder-Halbedl, M.; Fink, A.; Pietsch, M.; Djahani, O.; Hofmann, S. Excellent mid- to long-term survival of tantalum metal cones in a case series of revision knee arthroplasty with severe bony defects. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5496–5506. [Google Scholar] [CrossRef]
- Longo, U.G.; De Salvatore, S.; Intermesoli, G.; Pirato, F.; Piergentili, I.; Becker, R.; Denaro, V. Metaphyseal cones and sleeves are similar in improving short- and mid-term outcomes in total knee arthroplasty revisions. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 861–882. [Google Scholar] [CrossRef]
- Rockov, Z.A.; Byrne, C.T.; Rezzadeh, K.T.; Durst, C.R.; Spitzer, A.I.; Paiement, G.D.; Penenberg, B.L.; Rajaee, S.S. Revision total knee arthroplasty for arthrofibrosis improves range of motion. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1859–1864. [Google Scholar] [CrossRef]
- Pearson, Z.C.; Harris, A.B.; Agarwal, A.R.; Kreulen, R.T.; Martin, J.; Ahiarakwe, U.; Golladay, G.J.; Thakkar, S.C. Higher revision rates in patients with preoperative contralateral pes planovalgus deformity following total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4920–4926. [Google Scholar] [CrossRef] [PubMed]
- Mørup-Petersen, A.; Krogsgaard, M.R.; Laursen, M.; Madsen, F.; Winther-Jensen, M.; Odgaard, A. Patients in high- and low-revision hospitals have similar outcomes after primary knee arthroplasty: 1-year postoperative results from the Danish prospective multicenter cohort study, SPARK. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3487–3499. [Google Scholar] [CrossRef]
- Stroobant, L.; de Taeye, T.; Byttebier, P.; Van Onsem, S.; Jacobs, E.; Burssens, A.; Victor, J. Condylar constrained and rotating hinged implants in revision knee arthroplasty show similar survivorship and clinical outcome: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5365–5380. [Google Scholar] [CrossRef]
- Liu, E.X.; Kuhataparuks, P.; Liow, M.H.L.; Pang, H.N.; Tay, D.K.J.; Chia, S.L.; Lo, N.; Yeo, S.; Chen, J.Y. Clinical Frailty Scale is a better predictor for adverse post-operative complications and functional outcomes than Modified Frailty Index and Charlson Comorbidity Index after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3186–3195. [Google Scholar] [CrossRef]
- Lützner, C.; Beyer, F.; David, L.; Lützner, J. Fulfilment of patients’ mandatory expectations are crucial for satisfaction: A study amongst 352 patients after total knee arthroplasty (TKA). Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3755–3764. [Google Scholar] [CrossRef]
- Nam, H.S.; Yoo, H.J.; Ho, J.P.Y.; Kim, Y.B.; Lee, Y.S. Preoperative education on realistic expectations improves the satisfaction of patients with central sensitization after total knee arthroplasty: A randomized-controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4705–4715. [Google Scholar] [CrossRef]
- Wunderlich, F.; Ghaemi Kerahrodi, J.; Kuchen, R.; Klonschinski, T.; Afghanyar, Y.; Wegner, E.; Drees, P.; Eckhard, L. Optimism and pessimism are antithetically associated with post-operative knee function in patients’ undergoing total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3971–3980. [Google Scholar] [CrossRef]
- Marinova, M.; Sundaram, A.; Holtham, K.; Ebert, J.R.; Wysocki, D.; Meyerkort, D.; Radic, R. The role of a cryocompression device following total knee arthroplasty to assist in recovery: A randomised controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4422–4429. [Google Scholar] [CrossRef]
- Za, P.; Papalia, G.F.; Franceschetti, E.; Rizzello, G.; Adravanti, P.; Papalia, R. Aspirin is a safe and effective thromboembolic prophylaxis after total knee arthroplasty: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4407–4421. [Google Scholar] [CrossRef]
- Bayoumi, T.; Burger, J.A.; Ruderman, L.V.; van der List, J.P.; Zuiderbaan, H.A.; Kerkhoffs, G.M.M.J.; Pearle, A.D. Restoration or relative overcorrection of pre-arthritic coronal alignment leads to improved results following medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3981–3991. [Google Scholar] [CrossRef]
- Douiri, A.; Bouguennec, N.; Biset, A.; Colombet, P.; Laboudie, P.; Graveleau, N. Functional scores and prosthetic implant placement are different for navigated medial UKA left in varus alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3919–3926. [Google Scholar] [CrossRef]
- Hariri, M.; Zahn, N.; Mick, P.; Jaber, A.; Reiner, T.; Renkawitz, T.; Innmann, M.; Walker, T. Fixed-bearing is superior to mobile-bearing in lateral unicompartmental knee replacement: A retrospective matched-pairs analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3947–3955. [Google Scholar] [CrossRef]
- Zambianchi, F.; Seracchioli, S.; Franceschi, G.; Cuoghi Costantini, R.; Malatesta, A.; Barbo, G.; Catani, F. Image-based robotic-arm assisted unicompartmental knee arthroplasty provides high survival and good-to-excellent clinical outcomes at minimum 10 years follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5477–5484. [Google Scholar] [CrossRef]
- Micicoi, L.; Machado, A.; Ernat, J.; Schippers, P.; Bernard de Dompsure, R.; Bronsard, N.; Gonzalez, J.; Micicoi, G. Restoration of preoperative tibial alignment improves functional results after medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5171–5179. [Google Scholar] [CrossRef]
- Ruderman, L.V.; Bayoumi, T.; Burger, J.A.; Zuiderbaan, H.A.; Pearle, A.D. Higher incidence of patellar incongruence after under correction of pre-arthritic coronal alignment following medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5773–5782. [Google Scholar] [CrossRef]
- Tay, M.L.; Bolam, S.M.; Monk, A.P.; McGlashan, S.R.; Young, S.W.; Matthews, B.G. Better post-operative outcomes at 1-year follow-up are associated with lower levels of pre-operative synovitis and higher levels of IL-6 and VEGFA in unicompartmental knee arthroplasty patients. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4109–4116. [Google Scholar] [CrossRef]
- ten Noever de Brauw, G.V.; Bayoumi, T.; Ruderman, L.V.; Kerkhoffs, G.M.M.J.; Pearle, A.D.; Zuiderbaan, H.A. Knees with anteromedial osteoarthritis show a substantial phenotypic variation prior and following medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5579–5590. [Google Scholar] [CrossRef]
- Arndt, K.B.; Schrøder, H.M.; Troelsen, A.; Lindberg-Larsen, M. Patient-reported outcomes and satisfaction after revisions of medial unicompartmental knee arthroplasties for unexplained pain vs aseptic loosening. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4766–4772. [Google Scholar] [CrossRef]
- Hoorntje, A.; Pronk, Y.; Brinkman, J.M.; van Geenen, R.C.I.; van Heerwaarden, R.J. High tibial osteotomy versus unicompartmental knee arthroplasty for Kellgren–Lawrence grade 3–4 knee osteoarthritis in younger patients: Comparable improvements in patient-reported outcomes, adjusted for osteoarthritis grade and sex. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4861–4870. [Google Scholar] [CrossRef]
- Mørup-Petersen, A.; Krogsgaard, M.R.; Laursen, M.; Madsen, F.; Mongelard, K.B.G.; Rømer, L.; Winther-Jensen, M.; Odgaard, A. Hospital variation in revision rates after primary knee arthroplasty was not explained by patient selection: Baseline data from 1452 patients in the Danish prospective multicenter cohort study, SPARK. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3474–3486. [Google Scholar] [CrossRef]
- Nguyen, A.; Quan, T.; Wei, C.; Wei, C.; Malahias, M.A. Analysis of Eastern Asia’s Contributions to Major Orthopaedic Journals in the Past 21 Years. Cureus 2022, 14, e21075. [Google Scholar] [CrossRef]
- Van de Graaf, V.A.; Clark, G.W.; Collopy, D.; Wood, J.A.; Chen, D.B.; MacDessi, S.J. Functional alignment minimizes changes to joint line obliquity in robotic-assisted total knee arthroplasty: A CT analysis of functional versus kinematic alignment in 2116 knees using the Coronal Plane Alignment of the Knee (CPAK) classification. Bone Jt. Open 2024, 5, 1081–1091. [Google Scholar] [CrossRef]
- Young, S.W.; Tay, M.L.; Kawaguchi, K.; van Rooyen, R.; Walker, M.L.; Farrington, W.J.; Bayan, A. The John N. Insall Award: Functional Versus Mechanical Alignment in Total Knee Arthroplasty: A Randomized Controlled Trial. J. Arthroplast. 2025, 40, S20–S30.E2. [Google Scholar] [CrossRef]
- Sun, C.; Ma, Q.; Zhang, X.; Li, H.; Yang, X.; Cai, X. Improved alignment accuracy but similar early clinical outcomes with NAVIO imageless robotic-assisted vs. conventional total knee arthroplasty: A meta-analysis. J. Orthop. Surg. Res. 2025, 20, 619. [Google Scholar] [CrossRef]
- Maman, D.; Laver, L.; Becker, R.; Mahamid, A.; Berkovich, Y. Robotic-assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: A national analysis. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 336–342. [Google Scholar] [CrossRef]
- Vermue, H.; Batailler, C.; Budhiparama, N.; Lustig, S. Posterior Cruciate Ligament Retention Does Not Influence Clinical Outcomes in Medial Pivot Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplasty, 2025; in press. [Google Scholar] [CrossRef]
- Vogel, N.; Kaelin, R.; Arnold, M.P. Custom total knee arthroplasty with personalised alignment showed better 2-year functional outcome compared to off-the-shelf arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3220–3229. [Google Scholar] [CrossRef]
- Brenneis, M.; Flevas, D.A.; Braun, S.; Sculco, P.K.; Boettner, F. Imaging in revision total knee arthroplasty: A novel 3D classification system for tibial bone defects. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 323–333. [Google Scholar] [CrossRef]
- Zitsch, B.P.; Salaymeh, J.K.; Burdyny, M.R.; Buckner, B.C.; Lyden, E.R.; Konigsberg, B.S.; Garvin, K.L.; Hartman, C.W. Metaphyseal Fixation Using Cones and Sleeves for Severe Proximal Tibial Bone Loss. J. Arthroplast. 2024, 39, S256–S262. [Google Scholar] [CrossRef]
- Walker, T.; Freericks, J.; Mick, P.; Trefzer, R.; Lunz, A.; Koch, K.A.; Renkawitz, T.; Hariri, M. Long-term results of lateral unicompartmental knee arthroplasty with a mobile-bearing device. Bone Jt. J. 2025, 107-B, 322–328. [Google Scholar] [CrossRef]
- Lee, S.H.; Yoo, H.J.; Nam, H.S.; Ho, J.P.Y.; Lee, Y.S. The preoperative education on realistic expectations does not continually improve patients’ satisfaction after total knee arthroplasty? A randomized controlled trial with serial assessment. Knee Surg. Sports Traumatol. Arthrosc. 2025, 1–13. [Google Scholar] [CrossRef]
- Ruderman, L.V.; Bayoumi, T.; Ten Noever de Brauw, G.V.; Lan, R.; Nguyen, J.T.; Pearle, A.D. Robotic-arm-assisted lateral unicompartmental knee arthroplasty leads to high implant survival and patient satisfaction at mean 10-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2297–2308. [Google Scholar] [CrossRef]
- Bayoumi, T.; Ten Noever de Brauw, G.V.; Ruderman, L.V.; van der List, J.P.; Kerkhoffs, G.M.M.J.; Pearle, A.D.; Zuiderbaan, H.A. The phenotypic diversity of anteromedial osteoarthritis before and after treatment with medial unicompartmental knee arthroplasty: A radiographic analysis of 1000 knees. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 274–286. [Google Scholar] [CrossRef]
- Debopadhaya, S.; Acosta, E.; Ortiz, D. 3rd. Trends and outcomes in the surgical management of young adults with knee osteoarthritis using high tibial osteotomy and unicompartmental knee arthroplasty. Arch. Orthop. Trauma Surg. 2024, 144, 3995–4002. [Google Scholar] [CrossRef] [PubMed]
- Copp, E.H.; Gale, T.H.; Byrapogu, V.K.C.; Urish, K.L.; Anderst, W.J. Unicompartmental knee arthroplasty approximates healthy knee kinematics more closely than total knee arthroplasty. J. Orthop. Res. 2024, 42, 2514–2524. [Google Scholar] [CrossRef]
- Stoddart, J.C.; Garner, A.; Tuncer, M.; Amis, A.A.; Cobb, J.; van Arkel, R.J. Load transfer in bone after partial, multi-compartmental, and total knee arthroplasty. Front. Bioeng. Biotechnol. 2024, 12, 1274496. [Google Scholar] [CrossRef]
- Liu, Z.; Wen, L.; Zhou, L.; Liu, Z.; Chen, Y.; Geng, B.; Xia, Y. Comparison of Cemented and Cementless Fixation in Total Knee Arthroplasty: A Meta-Analysis and Systematic Review of RCTs. J. Orthop. Surg. 2024, 32, 10225536241267270. [Google Scholar] [CrossRef]
- Zhao, E.; Zhu, X.; Tang, H.; Luo, Z.; Zeng, W.; Zhou, Z. Randomized Controlled Trial of a Novel Cementless vs. Cemented Total Knee Arthroplasty: Early Clinical and Radiographic Outcomes. Orthop. Surg. 2024, 16, 2671–2679. [Google Scholar] [CrossRef]
- Za, P.; Papalia, G.F.; Cardile, U.; Gregori, P.; Vasta, S.; Franceschetti, E.; Campi, S.; Papalia, R. Cementless unicompartmental knee arthroplasty is safe and effective at a minimum follow-up of 4.2 years: A systematic review. J. Exp. Orthop. 2025, 12, e70253. [Google Scholar] [CrossRef]
- Rahman, A.; Omoregie, G.; Mellon, S.; Murray, D.W. Microporous titanium and hydroxyapatite improve fixation of the tibial wall in unicompartmental knee replacement. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 704–712. [Google Scholar] [CrossRef]
- Fricka, K.B.; Wilson, E.J.; Strait, A.V.; Ho, H.; Hopper, R.H., Jr.; Hamilton, W.G.; Sershon, R.A. Outcomes of fixed versus mobile-bearing medial unicompartmental knee arthroplasty. Bone Jt. J. 2024, 106-B, 916–923. [Google Scholar] [CrossRef]
- Apostolopoulos, V.; Boháč, P.; Marcián, P.; Nachtnebl, L.; Mahdal, M.; Pazourek, L.; Tomáš, T. Biomechanical comparison of all-polyethylene total knee replacement and its metal-backed equivalent on periprosthetic tibia using the finite element method. J. Orthop. Surg. Res. 2024, 19, 153. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lettner, J.; Prill, R.; Ramadanov, N.; Salzmann, M.; Królikowska, A.; Tandogan, R.N.; Violante, B.; Becker, R. Analysis of Trends in Orthopedic Knee Surgery—Key Findings on Total and Unicompartmental Knee Arthroplasty from a Leading Journal. Surgeries 2025, 6, 76. https://doi.org/10.3390/surgeries6030076
Lettner J, Prill R, Ramadanov N, Salzmann M, Królikowska A, Tandogan RN, Violante B, Becker R. Analysis of Trends in Orthopedic Knee Surgery—Key Findings on Total and Unicompartmental Knee Arthroplasty from a Leading Journal. Surgeries. 2025; 6(3):76. https://doi.org/10.3390/surgeries6030076
Chicago/Turabian StyleLettner, Jonathan, Robert Prill, Nikolai Ramadanov, Mikail Salzmann, Aleksandra Królikowska, Reha Nevzat Tandogan, Bruno Violante, and Roland Becker. 2025. "Analysis of Trends in Orthopedic Knee Surgery—Key Findings on Total and Unicompartmental Knee Arthroplasty from a Leading Journal" Surgeries 6, no. 3: 76. https://doi.org/10.3390/surgeries6030076
APA StyleLettner, J., Prill, R., Ramadanov, N., Salzmann, M., Królikowska, A., Tandogan, R. N., Violante, B., & Becker, R. (2025). Analysis of Trends in Orthopedic Knee Surgery—Key Findings on Total and Unicompartmental Knee Arthroplasty from a Leading Journal. Surgeries, 6(3), 76. https://doi.org/10.3390/surgeries6030076








