Short-Term Outcomes of a Novel Fascio-Aponeurotic Flap Technique for Ulnar Nerve Instability at the Elbow
Abstract
1. Introduction
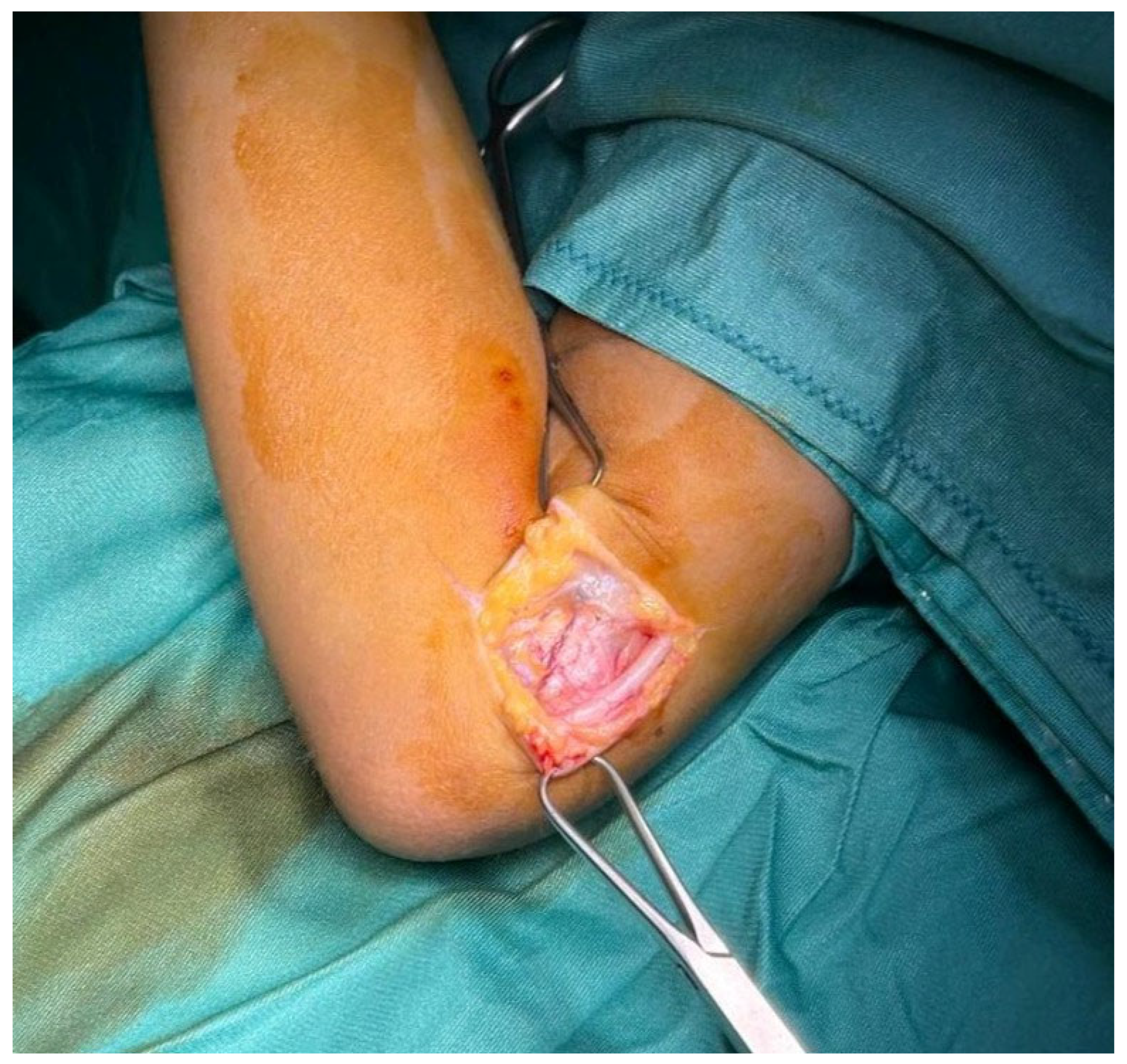
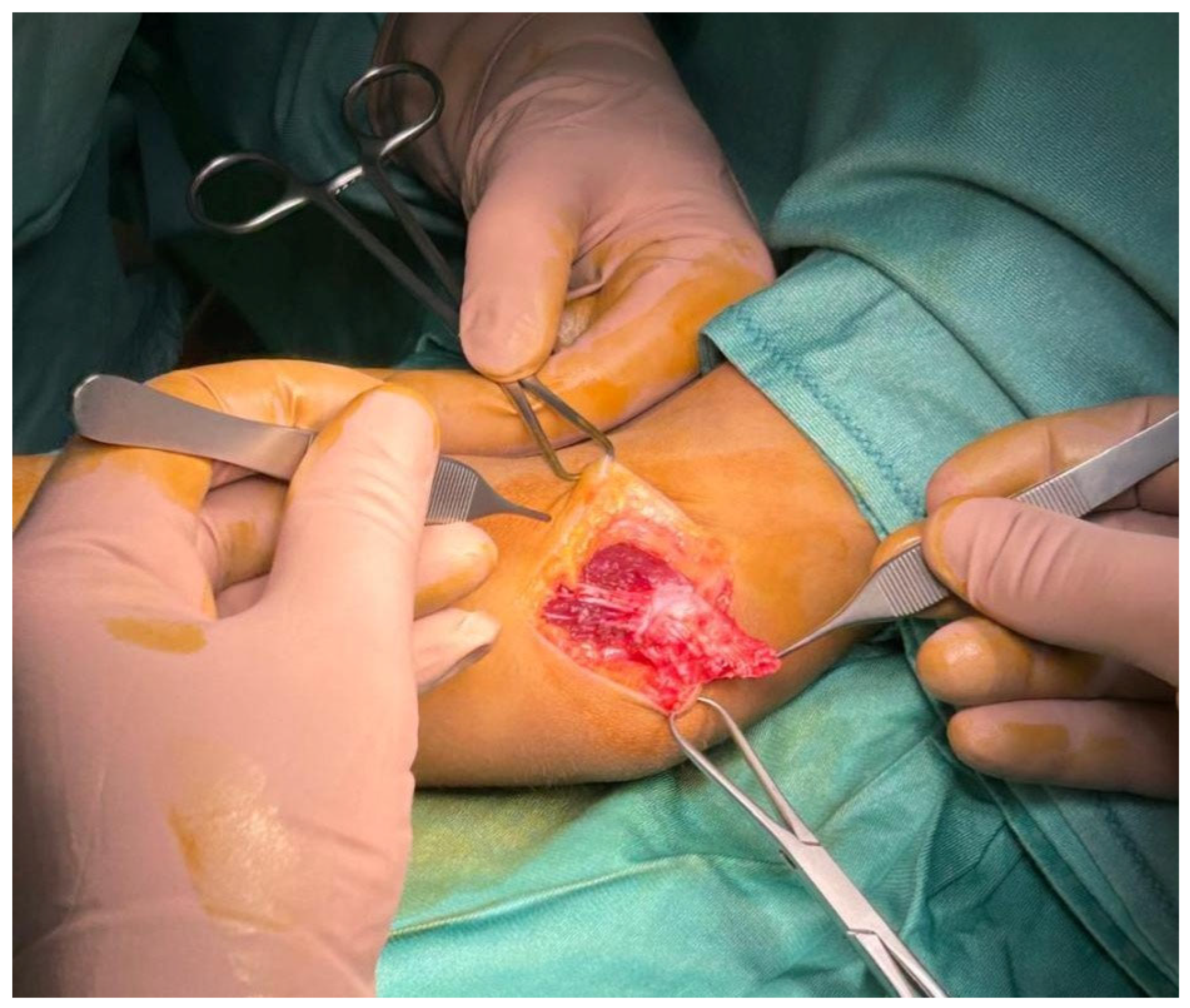
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Han, H.H.; Kang, H.W.; Lee, J.Y.; Jung, S.N. Fascia wrapping technique: A modified method for the treatment of cubital tunnel syndrome. Sci. World J. 2014, 2014, 482702. [Google Scholar] [CrossRef] [PubMed]
- Caliandro, P.; La Torre, G.; Padua, R.; Giannini, F.; Padua, L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst. Rev. 2016, 11, CD006839. [Google Scholar] [CrossRef]
- Vij, N.; Traube, B.; Bisht, R.; Singleton, I.; Cornett, E.M.; Kaye, A.D.; Imani, F.; Mohammadian Erdi, A.; Varrassi, G.; Viswanath, O.; et al. An Update on Treatment Modalities for Ulnar Nerve Entrapment: A Literature Review. Anesthesiol. Pain Med. 2020, 10, e112070. [Google Scholar] [CrossRef] [PubMed]
- Staples, J.R.; Calfee, R. Cubital Tunnel Syndrome: Current Concepts. J. Am. Acad. Orthop. Surg. 2017, 25, e215–e224. [Google Scholar] [CrossRef]
- Childress, H.M. Recurrent Ulnar-Nerve Dislocation at the Elbow. Clin. Orthop. Relat. Res. 1975, 108, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Lavyne, M.H.; Bell, W.O. Simple decompression and occasional microsurgical epineurolysis under local anesthesia as treatment for ulnar neuropathy at the elbow. Neurosurgery 1982, 11, 6–11. [Google Scholar] [CrossRef]
- Wilson, D.H.; Krout, R. Surgery of ulnar neuropathy at the elbow: 16 cases treated by decompression without transposition. J. Neurosurg. 1973, 38, 780–785. [Google Scholar] [CrossRef]
- Andrews, K.; Rowland, A.; Pranjal, A.; Ebraheim, N. Cubital tunnel syndrome: Anatomy, clinical presentation, and management. J. Orthop. 2018, 15, 832–836, Erratum in J. Orthop. 2020, 23, 275. [Google Scholar] [CrossRef]
- Eaton, R.G.; Crowe, J.F.; Parkes, J.C., 3rd. Anterior transposition of the ulnar nerve using a Non-Compressing fasciodermal sling. J. Bone Jt. Surg. Am. 1980, 62, 820–825. [Google Scholar] [CrossRef]
- O’Grady, E.E.; Vanat, Q.; Power, D.M.; Tan, S. A systematic review of medial epicondylectomy as a surgical treatment for cubital tunnel syndrome. J. Hand Surg. (Eur. Vol.) 2017, 42, 941–945. [Google Scholar] [CrossRef]
- Richmond, J.C.; Southmayd, W.W. Superficial anterior transposition of the ulnar nerve at the elbow for ulnar neuritis. Clin. Orthop. Relat. Res. 1982, 164, 42–44. [Google Scholar] [CrossRef]
- D’Orio, M.; Fulchignoni, C.; De Vitis, R.; Passiatore, M.; Taccardo, G.; Marzella, L.; Lazzerini, A. Feasibility of a fascial flap to avoid anterior transposition of unstable Ulnar nerve: A cadaver study. J. Clin. Orthop. Trauma 2023, 42, 102202. [Google Scholar] [CrossRef]
- Passiatore, M.; De Vitis, R.; Cilli, V.; Milano, G.; Saccomanno, M.F.; Cotroneo, C.; Brozzini, E.; Vigliarolo, D.; Taccardo, G. The Italian Version of the Michigan Hand Outcomes Questionnaire (MHQ): Translation, Cross-Cultural Adaptation and Validation. J. Hand Surg. (Asian-Pac. Vol.) 2021, 26, 666–683. [Google Scholar] [CrossRef]
- Padua, R.; Padua, L.; Ceccarelli, E.; Romanini, E.; Zanoli, G.; Amadio, P.C.; Campi, A. Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-Cultural adaptation and validation. J. Hand Surg. Br. 2003, 28, 179–186. [Google Scholar] [CrossRef]
- Pratt, N. Anatomy of nerve entrapment sites in the upper quarter. J. Hand Ther. 2005, 18, 216–229. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L.; Hament, W.; Gittelshon, A. Nonoperative management of cubital tunnel syndrome: An 8-year prospective study. Neurology 1993, 43, 1673–1677. [Google Scholar] [CrossRef] [PubMed]
- D’Orio, M.; De Vitis, R.; Taccardo, G.; Rocchi, L.; Ferrari, F.; Perna, A.; Passiatore, M. Clinical usefulness of nutraceutics with acetyl-L-carnitine, α-lipoic acid, phosphatidylserine, curcumin, C, E and B-group vitamins in patients awaiting for carpal tunnel release during COVID-19 pandemic: A randomized controlled open label prospective study. Acta Biomed. 2023, 94, e2023050. [Google Scholar]
- Passiatore, M.; Perna, A.; De-Vitis, R.; Taccardo, G. The Use of Alfa-Lipoic Acid-R (ALA-R) in Patients with Mild-Moderate Carpal Tunnel Syndrome: A Randomised Controlled Open Label Prospective Study. Malays. Orthop. J. 2020, 14, 1–6. [Google Scholar]
- Evangelista, M.; Cilli De Vitis, R.; Militerno, A.; Fanfani, F. Ultra-Micronized Palmitoylethanolamide Effects on Sleep-Wake Rhythm and Neuropathic Pain Phenotypes in Patients with Carpal Tunnel Syndrome: An Open-Label, Randomized Controlled Study. CNS Neurol. Disord. Drug Targets 2018, 17, 291–298. [Google Scholar] [CrossRef]
- Elhassan, B.; Steinmann, S.P. Entrapment neuropathy of the ulnar nerve. J. Am. Acad. Orthop. Surg. 2007, 15, 672–681. [Google Scholar] [CrossRef]
- Deer, T.R.; Jain, S.; Hunter, C.; Chakravarthy, K. Neurostimulation for Intractable Chronic Pain. Brain Sci. 2019, 9, 23. [Google Scholar] [CrossRef]
- Dellon, A.L. Review of treatment results for ulnar nerve entrapment at the elbow. J. Hand Surg. Am. 1989, 14, 688–700. [Google Scholar] [CrossRef]
- Arle, J.E.; Zager, E.L. Surgical treatment of common entrapment neuropathies in the upper limbs. Muscle Nerve 2000, 23, 1160–1174. [Google Scholar] [CrossRef] [PubMed]
- Filippi, R.; Farag, S.; Reisch, R.; Grunert, P.; Böcher-Schwarz, H. Cubital tunnel syndrome. Treatment by decompression without transposition of ulnar nerve. Minim. Invasive Neurosurg. 2002, 45, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.H.; Samadani, U.; Zager, E.L. Ulnar nerve entrapment neuropathy at the elbow: Simple decompression. Neurosurgery 2004, 55, 1150–1153. [Google Scholar] [CrossRef] [PubMed]
- Mirza, A.; Reinhart, M.K.; Bove, J.; Litwa, J. Scope-Assisted release of the cubital tunnel. J. Hand Surg. Am. 2011, 36, 147–151. [Google Scholar] [CrossRef]
- Zhang, X.; Dhawan, V.; Yu, Y.; Zhang, G.; Shao, X. A minimally invasive approach for cubital tunnel release and ulnar nerve transposition. Phys. Sportsmed. 2017, 45, 110–113. [Google Scholar] [CrossRef]
- Nabhan, A.; Ahlhelm, F.; Kelm, J.; Reith, W.; Schwerdtfeger, K.; Steudel, W.I. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J. Hand Surg. Br. 2005, 30, 521–524. [Google Scholar] [CrossRef]
- Ahcan, U.; Zorman, P. Endoscopic decompression of the ulnar nerve at the elbow. J. Hand Surg. Am. 2007, 32, 1171–1176. [Google Scholar] [CrossRef]
- Baek, G.H.; Kwon, B.C.; Chung, M.S. Comparative study between minimal medial epicondylectomy and anterior subcutaneous transposition of the ulnar nerve for cubital tunnel syndrome. J. Shoulder Elb. Surg. 2006, 15, 609–613. [Google Scholar] [CrossRef]
- Amako, M.; Nemoto, K.; Kawaguchi, M.; Kato, N.; Arino, H.; Fujikawa, K. Comparison between partial and minimal medial epicondylectomy combined with decompression for the treatment of cubital tunnel syndrome. J. Hand Surg. Am. 2000, 25, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Porcellini, G.; Paladini, P.; Campi, F.; Merolla, G. Arthroscopic neurolysis of the ulnar nerve at the elbow. Chir. Organi Mov. 2005, 90, 191–200. [Google Scholar] [PubMed]
- Lucchina, S.; Fusetti, C.; Guidi, M. Sonographic Follow-Up of Patients with Cubital Tunnel Syndrome Undergoing In Situ Open Neurolysis or Endoscopic Release: The SPECTRE Study. Hand 2021, 16, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Chuang, D.C.; Treciak, M.A. Subfascial anterior transposition: A modified method for the treatment of cubital tunnel syndrome (CuTS). Tech. Hand Up. Extrem. Surg. 1998, 2, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.M.; Piscoya, A.S.; Dunn, J.C.; Nesti, L.J. The impact of Pre-Existing ulnar nerve instability on the surgical treatment of cubital tunnel syndrome: A systematic review. J. Shoulder Elb. Surg. 2020, 29, 2339–2346. [Google Scholar] [CrossRef]
- Ruettermann, M. Challenging the dogma: Anterior transposition of the ulnar nerve is indicated in recurrent cubital tunnel syndrome. J. Hand Surg. (Eur. Vol.) 2021, 46, 45–449. [Google Scholar] [CrossRef]

| Patients | Sex | Preoperative Condition | Age | Pre-op VAS | Post-op VAS | Pre-op qDash | Post-op qDash | Pre-op MHQ | Post-op MHQ |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | Dislocation by tumor | 10 | 9.00 | 0.00 | 95.25 | 12.50 | 23.1% | 98.4% |
| 2 | M | Type B instability | 33 | 10.00 | 3.00 | 96.50 | 29.50 | 22.2% | 89.3% |
| 3 | F | Previous surgical anterior transposition | 26 | 10.00 | 1.00 | 92.00 | 14.50 | 21.6% | 96.4% |
| 4 | F | Type A instability | 30 | 8.00 | 1.00 | 85.25 | 23.50 | 39.0% | 91.6% |
| 5 | F | Type A instability | 38 | 8.00 | 2.00 | 79.50 | 21.25 | 34.7% | 94.3% |
| 6 | M | Type A instability | 21 | 9.00 | 1.00 | 98.25 | 13.75 | 28.3% | 95.7% |
| 7 | F | Previous surgical anterior transposition | 90 | 9.00 | 4.00 | 90.75 | 35.25 | 41.8% | 86.9% |
| 8 | F | Type A instability | 46 | 8.00 | 1.00 | 85.25 | 19.25 | 46.8% | 97.6% |
| 9 | M | Type B instability | 55 | 8.00 | 1.00 | 90.75 | 17.75 | 34.7% | 98.1% |
| 10 | F | Type A instability | 63 | 8.00 | 2.00 | 80.25 | 16.50 | 22.5% | 94.2% |
| Mean | 6/4 | 41.2 | 8.70 | 1.60 | 89.37 | 20.38 | 31.47% | 94.25% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Vitis, R.; D’Orio, M.; Cannella, A.; Michel Gabriel, E.; Taccardo, G.; Marzella, L.; Cilli, V.; Sassara, G.M.; Passiatore, M. Short-Term Outcomes of a Novel Fascio-Aponeurotic Flap Technique for Ulnar Nerve Instability at the Elbow. Surgeries 2025, 6, 49. https://doi.org/10.3390/surgeries6030049
De Vitis R, D’Orio M, Cannella A, Michel Gabriel E, Taccardo G, Marzella L, Cilli V, Sassara GM, Passiatore M. Short-Term Outcomes of a Novel Fascio-Aponeurotic Flap Technique for Ulnar Nerve Instability at the Elbow. Surgeries. 2025; 6(3):49. https://doi.org/10.3390/surgeries6030049
Chicago/Turabian StyleDe Vitis, Rocco, Marco D’Orio, Adriano Cannella, Eve Michel Gabriel, Giuseppe Taccardo, Luciana Marzella, Vitale Cilli, Giulia Maria Sassara, and Marco Passiatore. 2025. "Short-Term Outcomes of a Novel Fascio-Aponeurotic Flap Technique for Ulnar Nerve Instability at the Elbow" Surgeries 6, no. 3: 49. https://doi.org/10.3390/surgeries6030049
APA StyleDe Vitis, R., D’Orio, M., Cannella, A., Michel Gabriel, E., Taccardo, G., Marzella, L., Cilli, V., Sassara, G. M., & Passiatore, M. (2025). Short-Term Outcomes of a Novel Fascio-Aponeurotic Flap Technique for Ulnar Nerve Instability at the Elbow. Surgeries, 6(3), 49. https://doi.org/10.3390/surgeries6030049





